Abstract
Taenia solium was declared potentially eradicable by the International Task Force for Disease Eradication in 1992. Yet, very few well-designed community-based randomized controlled trials have been conducted to measure the effectiveness of alternative control strategies. Most strategies have been tested in pre-post intervention designs in very few communities, often without a control group. The only two community-based randomized controlled trials suggest that an educational program alone or a combination of human and porcine mass treatment reduce porcine cysticercosis in the short term. A transmission dynamics model suggests that improved sanitation and pig management are more effective and sustainable than pig vaccination, human or porcine mass treatment. Current evidence does not support the eradication of Taenia solium in the foreseeable future. Investigators should follow international recommendations on the conduct of community-based randomized control trials to provide more valid estimates of the effect and cost-effectiveness of alternative control strategies for cysticercosis.
Keywords: Taenia solium, cysticercosis, neurocysticercosis, intervention trials, community-based trials, porcine, human, review
Introduction
The International Task Force on Disease Eradication (ITFDE) of the World Health Organization declared Taenia solium as being potentially eradicable in 1992 [1]. In 2013, the ITFDE re-emphasized their opinion that T. solium should be considered eradicable, with the most effective method to interrupt the life cycle being improvement of human sanitation and hygiene, combined with surveillance of porcine infection through tongue inspection [**2]. Many others have made recommendations on the best approaches to control cysticercosis [3-6], but these are not based on evidence arising from well-designed community-randomized controlled trials, despite the call for such studies by the ITFDE [**2]. In addition, no cost-effectiveness or cost-benefit analyses have been conducted to compare alternative control strategies for the simultaneous control of porcine and human cysticercosis [**2]. This article is a review of evidence from published community-based trials which used at least a pre-post intervention design to estimate the effect of at least one control strategy on the community-level frequency of porcine or human cysticercosis, neurocysticercosis or human taeniasis.
How to break Taenia solium life cycle
When discussing alternative control measures for cysticercosis, it is essential to understand the life cycle of T. solium and how different types of interventions may break that cycle (Figure 1). Briefly, humans serve as the definitive host usually harboring one adult hermaphrodite parasite in their intestine, a condition called taeniasis. When humans with taeniasis defecate in the environment, they may shed up to five parasite segments per day, each containing tens of thousands of eggs [7,8]). Interventions that stop the eggs from reaching the environment include the use and proper maintenance of latrines or treatment of taeniasis cases with praziquantel or niclosamide, followed by safe disposal of feces after treatment. Very little is known about factors that affect the survival of the eggs in the environment. In one experimental study, exposure to very high temperatures achieved 100% inactivation of T. solium eggs, and acid pH combined with dryer environments increased inactivation [9]. This suggests that eggs are likely to survive for months in an alkaline soil in humid environments. Pigs are the only intermediate hosts for T. solium. In areas where they are traditionally raised and left roaming, they eat human feces or food contaminated with T. solium eggs. Even penned pigs may have access to infectious eggs, when fed with contaminated food or when directly fed human feces, as reported in some endemic communities [10, 11, 12] (Flisser, 1988; Pouedet et al., 2002; Shey-Njila et al., 2003). Interventions focusing on improved pig management practices aim at reducing access of human feces to pigs. Vaccines aim at protecting pigs from acquiring the infection when exposed to the eggs. Once ingested, the egg releases an embryo or oncosphere, which migrate primarily to the muscles where they mature into a larval stage named metacestode (commonly referred to as cysticercus). Cysticerci establish as cysts 10-12 weeks after ingestion. When humans consume undercooked infected pork meat, they develop taeniasis, and after about two months, worms produce eggs that are passed with feces, thus completing the cycle. Treatment of pigs, appropriate meat inspection and sufficient cooking of pork meat are alternative strategies to stop humans from consuming contaminated meat. The public health burden of T. solium lies in the infection of humans with the larval stages, a condition called cysticercosis. Humans may develop cysticercosis when eating food contaminated with the eggs present in the environment, through auto-infection if they have taeniasis, or through direct contact with a carrier. In addition to proper use of latrines and treatment of human taeniasis carriers mentioned above, proper hand washing and food hygiene can prevent humans from acquiring cysticercosis. When the larva(e) lodge in the central nervous systems (CNS), neurocysticercosis develops. Neurocysticercosis is very pleomorphic in its manifestations but seizures and epilepsy, severe chronic headaches and focal deficits have been shown to be the most common among symptomatic cases [13].
Figure 1.
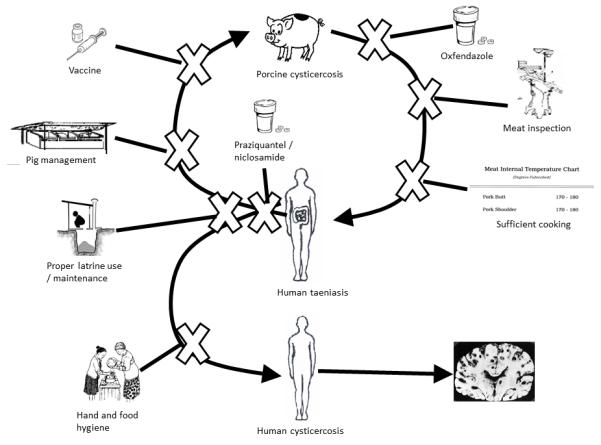
Life cycle of Taenia solium cysticercosis and possible interventions for control Legend: the “X” denotes areas where the life cycle may be interrupted.
Literature search method and findings
A search in Medline using Mesh terms “taenia solium” or “cysticercosis” and publication type “randomized controlled trial” returned 48 hits. The search did not restrict for date or language.. When the keyword “community” was added, only three articles remained, among which only one was a community-based randomized controlled trial conducted in Tanzania [14]. Given these search results, we kept the mesh terms and combined them with the keywords (control OR intervention OR treatment OR vaccination OR trial) AND (community OR village* OR municipality OR household OR farm). This resulted in 163 articles, of which 10 reported on original studies assessing the effect of some intervention implemented at the community level on the frequency of porcine or human cysticercosis, neurocysticercosis or human taeniasis [14, 15-23]. We also identified several documents on cysticercosis control, including guidelines [3-4], book chapters [6], and review or opinion papers [5, 24]. The review of these resulted in identifying two additional articles [25, 26]. We also found a review paper on control strategies reported in the Chinese literature [28], but it included too few details regarding methods to be included in this review. Finally, a Mexican study published after we had conducted our literature search was also included ([27])
The sections below review and critique these studies according to the interventions being evaluated. Tables 1 and 2 describe and provide a summary of biases of studies focusing on a human outcome (Tables 1a and 2a) and a pig outcome (Tables 1b and 2b), respectively, to assess the effect of the intervention. None of the interventions solely targeting pigs (treatment or vaccine) assessed the effectiveness of the control strategy on human outcomes.
Table 1a.
Summary of articles published on the effectiveness of community-based control strategies aimed at reducing human cysticercosis, taeniasis or neurocysticercosis or at improving knowledge, attitudes and practices (KAP).
| Country [reference] |
Years of study |
Study design | Duration of follow-up |
Sample sizes (at the unit of the intervention and at the subject level pre and post intervention) |
Control Strategy | Randomization /control group (treatment) |
Measurement of outcome |
|---|---|---|---|---|---|---|---|
| Mexico [10] | 1988-89 | Pre-post prevalence comparison |
12 months | 1 village Stools: Pre: 302; post: 283 Sera: Pre: 335; Post: 278 |
Praziquantel *MDA (10 mg/kg; coverage of 71%) |
No / No | Taeniasis : coproscopy on 3 stools from 3 days with Faust, Ritchie and Martin and Beaner methods. Cysticercosis : §AbELISA |
| Mexico [11] | 1991-96 | Pre-post prevalence comparison |
6 and 42 months |
1 village Stools: pre: 1865; 6 mo: 1311; 42 mo: 605 Sera: Pre: 1603; 6 mo 1360; 42 mo: 272 sera “Individual” analysis with 304 stools and 112 sera with 2 or 3 samples |
Praziquantel MDA (5mg/kg; coverage of 87%) |
No / No | Taeniasis: combined coproantigen- and coproscopy Cysticercosis: ¶EITB assay |
| Guatemala [12] |
1994-96 | Pre-post prevalence comparison |
10 months | 2 villages Stools: pre: 1582; post: 1116 |
Niclosamide MDA (2g for >= 6 years old, 1 g for < 6 years old; coverage 74.9%) |
No / No | Taeniasis: copro-antigen (Allan et al., 1990) and coproscopy |
| Mexico [13] | 1992-93 | Pre-post prevalence comparison |
6 months | 1 village Stools: pre : 1404; post : 792 ¶KAP : pre and post : 146 (out of 200 at pre) |
Education (6 months): (poster, pamphlet, two videos) |
No / No | Taeniasis: copro-antigen ¥ KAP: questionnaires |
| Kenya [14] | 2006-08 | Pre-post prevalence comparison |
3 and 10 months (some at 15 months) |
2 districts and 4 divisions in Western Kenya (number of farmers: Pre: 282, 3 months: 276; 10 months: 236) |
Educational workshops ( 1 day) using a train the trainer approach |
No / No | KAP: questionnaire to farmers |
| Tanzania [9] | 2002- 2004 |
Community- based randomized controlled trial |
10 to 12 months |
42 villages in one district (21 intervention and 21 control villages) |
PRECEDE-PROCEED to develop educational package for farmers |
Yes / Yes(No education) |
KAP: questionnaire to farmers |
| Ecuador [21] | 1986-87 | Pre-post prevalence comparison |
12 months | Part of one canton Stools: pre n=2761; post n=739 (420 with Kato-Katz) |
Education (radio, poster, leaflet) and praziquantel (5 mg/kg; 76% coverage) |
No / No | Taeniasis: Report of expulsion of tapeworm and Kato-Katz at follow-up |
| Honduras [15] |
1997- 2005 |
Pre post proportion comparison |
6 years | Salamá County (18 villages and towns) 1997 : 90 1997-2005 : 36 |
Education and media campaign (1999), training in pig management practices for farmers (1999), construction of water projects and sewage disposal facilities (2001), construction of a child clinic (2002), MDA of albendazole (400 mg) to schoolchildren every 6 months (1999), taeniasis surveillance and treatment of cases with niclosamide (2001) |
No / No | Epilepsy: combination of positive screen to a house-to- house survey (1997 to 2005) and medical records or informant identification. All suspected cases confirmed by an epileptologist Active epilepsy: seizures in the past 5 years Neurocysticercosis (NCC): brain tomography |
MDA: Mass drug administration
AbELISA : Enzyme-linked Immunosorbent assay to detect antibodies to T. solium
EITB: Enzyme linked immunoelectrotransfer blot assay to detect antibodies to T. solium
KAP: Knowledge, attitudes and practices
Table 2a.
Summary of results and potential for bias of articles published on the effectiveness of community-based control strategies aimed at reducing human cysticercosis, taeniasis or neurocysticercosis or at improving knowledge, attitudes and practices (KAP).
| Country [reference] |
Results | Potential for bias | |||||
|---|---|---|---|---|---|---|---|
| Information bias |
Confounding | Selection bias | Clustering/ non independence |
Power/ generalizability |
Other | ||
| Mexico [10] |
Taeniasis Pre: 1.4% (4 cases / 302); Post: 0% *PPR: 0 (95%§CI: undefined) Antibodies to Cysticercosis: Pre: 10.7%; Post: 7.4% PPR: 0.65 (95%CI: 0.39; 1.10) |
High: poor tests |
High: not controlled; no randomization |
Moderate: some losses to follow-up |
Ignored/ ignored |
Poor / poor 25% participation in village |
Clustering of cases noted |
| Mexico [11] |
Taeniasis Pre: 2.0% (matched); 1.1% (unmatched) 6 mo.: 1.0% (matched); 0.5% (unmatched) 42 mo.: 0.7% (matched); 0.5% (unmatched) PPR (6 mo unmatched): 0.47 (95%CI: 0.20-1.11) PPR (42 mo unmatched): 0.44 (95%CI: 0.13-1.47) Seroprevalence (EITB): Pre: 7.1% (matched); 5.7% (unmatched) 6 mo.: 10.7% (matched) 10.1% (unmatched) 42 mo: 1.8% (matched); 2.2% (unmatched) PPR (6 mo unmatched): 1.77 (95%CI: 1.38-2.29) PPR (42 mo unmatched): 0.39 (95%CI: 0.17-0.88) |
Low: valid tests |
High: not controlled; no randomization |
High: many losses to follow- up at 42 months |
Ignored/ Ignored even in “individual” analysis |
Poor / poor | Increase in prevalence of cysticercosis at 6 months (those positive lost to follow-up?); inappropriate statistical analyses |
| Guatemala [12] |
Taeniasis Pre: 3.5%; Post: 1% PPR: 0.28 (95%CI: 0.15-0.53) |
Low: valid test | High: not controlled; no randomization |
Modertae: some losses to follow-up |
Ignored/ ignored |
Poor / poor | Taeniasis incidence rate post treatment: 0.96 / 100 person- years. Side effect of niclosamide not monitored |
| Mexico [13] |
Taeniasis Pre: 0.8%; Post: 0.5%. PPR: 0.64 (95%CI: 0.21-2.02) ¥KAP: improvement of knowledge on life cycle; not defecation or washing hand/food |
Low: valid tests, low |
High: not controlled; no randomization |
High: many losses to follow- up, sampling not described |
Ignored/ ignored |
Poor / poor | Generally well described study |
| Kenya [14] |
KAP General improvement in knowledge on the life cycle and in practices for pig management (tethering) |
Moderate: self-reported questionnaire |
High: not controlled, no randomization |
Moderate: some losses-to- follow-up |
Ignored / well described but unclear if appropriately applied |
Good at the individual level, poor otherwise/ unknown |
Data in Table does not agree with described paired analyses. Losses to- follow-up may bethose with least knowledge |
| Tanzania [9] |
KAP Improvement pre-post in knowledge about porcine cysticercosis and prevention in both groups. Practice of not eating undercooked pork improved in intervention compared to control group. |
Moderate: self-reported questionnaire; |
Low: randomized and paired |
Moderate: losses to- follow-up (not at the village level) |
Group analysis/ paired analysis |
Good / good for Mbulu |
Study well described. Monitoring alone improves knowledge and practices. |
| Ecuador [20] |
Taeniasis Pre: 2.2%; Post: 0% PPR: 0 (95%CI: undefined) |
Very high: Very poor test |
High: not controlled; no randomization |
High: sampling not described |
Ignored/ ignored |
Poor / poor | Poor description of study. Unrealistic cost estimate. |
| Honduras [15] |
% NCC among People With Active Epilepsy: Onset pre 1997: 36.7% (27/74) Onset post 1997: 13.9% (5/36) PPR: 0.38 (95%CI: 0.16-0.89) |
Low: valid tests |
High: not controlled; no randomization |
Moderate:mmi gration of new onset seizures may have occurred |
Ignored / only new cases of epilepsy included in the follow-up |
Poor / Salama county |
Unclear if door-to- door survey done every year. |
PPR: Prevalence Proportion Ratio
CI : Confidence Interval
KAP: Knowledge, attitudes and practices
Table 1b.
Summary of articles published on the effectiveness of community-based control strategies aimed at reducing porcine cysticercosis.
| Country [reference] |
Years of study |
Study design | Duration of follow-up |
Sample sizes (at the unit of the intervention and at the subject level pre and post intervention |
Control Strategy | Randomization/ control group |
Measurement of outcome |
|---|---|---|---|---|---|---|---|
| Mexico [11] | 1991-96 | Pre-post prevalence comparison |
6 and 42 months |
1 village Tongue: Pre: 646; 6 mo: 449; 42 mo: 334 Serum: Pre: 269; 6 mo: 448; 42 mo: 326 |
Praziquantel (single dose 5mg/kg) MDA (87% coverage) |
No / No | Tongue examination and ¶EITB |
| Guatemala [12] | 1994-96 | Pre-post prevalence comparison |
10 months | 2 villages Pre : 269 Post : 300 |
Niclosamide MDA (2g for >= 6 years old, 1 g for < 6 years old; coverage 74.9%) |
No / No | EITB |
| Mexico [21] | 2001-2003 | Pre-post prevalence comparison in sentinel pigs during controlled trial with study pigs |
4 to 8 months; 14 and 28 months for sentinel pigs |
One community Sentinel pigs : Pre : 29; 14 mo : 200; 28 mo : 50 |
S3Pvac (1 dose at 2 months in 48 study pigs and 2 doses at 2 and 3 months in 98 study pigs) |
No / No (for the sentinel pigs) |
Tongue examination |
| Mexico [17] | Not specified |
Pre-post prevalence comparison |
12 and 24 months |
6 villages (12 mo) and 4 villages (24 mo) Pre (6 villages): 814 Pre (4 villages) : 508 12 mo (6 villages) : 971 24 mo (4 villages) : 655 |
Vaccine prepared from crude antigens extracts |
No / No | Tongue examination |
| Peru [18] | Not specified |
Pre-post community- based randomized controlled trial (paired?) |
20 months with examinations every 4 months |
12 “treatment units”, 9 villages | One praziquantel MDA in humans (5mg/kg) coverage 75%, two oxfendazole MDA in pigs (30 mg/kg) |
Yes / Yes (one pyrantel pamoate MDA in humans (11 mg/kg) coverage 75%; no control MDA in pigs) |
EITB |
| Mexico [16] | 1986-87 | Pre-post prevalence comparison |
«about» 1 year | 1 village (440 pigs pre and 300? pigs post) |
Education (meetings) * and praziquantel MDA (60% coverage) |
No / No | Tongue examination |
| Tanzania [9] | 2002-2004 | Pre-post community- based randomized controlled trial |
2-9 months | 42 villages in one district 133 pigs in intervention; 128 in control |
PRECEDE-PROCEED to develop educational package for farmers |
Yes / Yes(No education) |
Tongue examination and §AgELISA |
| Mexico [13] | 1992-93 | Pre-post prevalence comparison |
6 months | 1 village Pre: 194; Post: 165 |
Education (6 months): (poster, pamphlet, two videos) |
No / No | Tongue examination and EITB |
| Ecuador [21] | 1986-87 | Pre-post prevalence comparison |
12 months | Part of one canton Pre: 70 pigs; Post: 113 pigs |
Education (radio, poster, leaflet) and praziquantel (5 mg/kg; 76% coverage) |
No / No | “careful” inspection of pigs killed at the local slaughterhouse |
| Mexico [27] | 2009-2012 | Pre-post prevalence comparison |
39 months | 3 municipalities (AgELISA: Pre: 1012; post: 180; Tongue: Pre: 960; post: 396; Ultrasound: Pre: 786; post: 381) |
Education (pamphlets, meetings, videos) and pig vaccination (3 times at 6 months interval) with S3Pvac |
None | AbELISA, tongue inspection and ultrasound. |
MDA: Mass drug administration
AgELISA : Enzyme linked Immunosorbent assay to detect antigens to T. solium
EITB: Enzyme linked immunoelectrotransfer blot assay to detect antibodies to T. solium
Table 2b.
Summary of results and potential for bias of articles published on the effectiveness of community-based control strategies aimed at reducing porcine cysticercosis.
| Country [reference] |
Results | Limitations | |||||
|---|---|---|---|---|---|---|---|
| Information bias | Confounding | Selection bias | Clustering / non independence |
Power/ generalizability |
Other | ||
| Mexico [11] |
Antibodies (EITB): Pre: 4.8%; 6 mo.: 2.2%; 42 mo.: 3.4% PPR (6 mo): 0.46 (95%CI: 0.21-1.04) PPR (42 mo): 0.70 (95%CI : 0.32-1.53) Tongue examination: Pre: 1.2%; 6 mo.: 1.1%; 42 mo.: 0.6% PPR (6 mo): 0.90 (95%CI: 0.30-2.73) PPR (42 mo): 0.48 (95%CI : 0.10-2.26) |
Low: Valid test | High: not controlled, no randomization |
High: Sampling not described |
Ignored / ignored | Poor / poor | More pigs were sampled at 6 mo., followed by 42 months without any explanation. |
| Guatemala [12] |
Antibodies (EITB) : Pre: 55%; Post: 7% PPR: 0.13 (95%CI: 0.09-0.20) |
Low : Valid test | High: not controlled, no randomization |
Low : Pigs randomly sampled |
Ignored / ignored | Poor / poor | Pigs sampled post intervention were younger. |
| Mexico [21] |
Tongue inspection (sentinel pigs) : Pre: 13.8%; 14 mo: 12%; 28 mo: 16% PPR (14 mo): 0.87 (95%CI: 0.33-2.33) PPR (28 mo): 1.16 (95%CI : 0.38-3.52) |
High: Poor test (especially for decreasing number of cysts) |
High: Not controlled, no randomization |
Moderate: Variation in sample size in the 3 examinations unexplained |
Ignored / ignored | Poor / poor | Poorly designed and analyzed study. |
| Mexico [17] |
Tongue inspection Pre (6 villages): 25.8%; (4 villages): 2.0%; 12 mo (6 villages): 12.5%; 24 mo (4 villages): 0.5% PPR (12 mo): 0.48 (95%CI: 0.24-0.98) PPR (24 mo): 0.23 (95% CI: 0.64-0.84) |
High: Poor test | High: Not controlled, no randomization |
High: Choice of villages to follow-up unexplained |
Ignored / ignored | Poor / poor | Poorly designed study |
| Peru [18] |
Antibodies (EITB) using incident cases: ±OR (treatment): 1.28 (0.59; 2.78) OR (post period): 2.84 (0.79; 10.25) OR (treatment and post period): 0.39 (0.18-0.81) |
Moderate: Contamination of intervention, valid test |
Moderate: Randomization broken (imbalance in baseline prevalences) |
Moderate: Census of all pigs; important losses to follow- up |
Unclear (GEE used, but village- effects included)/ only new cases or different pigs included |
Moderate / good for that area |
Inappropriate statistical analysis (logistic regression for common outcome- overestimates magnitude of effect; model mis-specified) |
| Mexico [16] |
Tongue examination: Pre: 6%; Post: 11% *PPR : 1.86 (95%§CI : 1.14-3.05) |
High: poor test | High: not controlled, no randomization |
High: Sampling not described |
Ignored / ignored | Poor / poor | Methods inconsistent with results description. |
| Tanzania [9] |
Antigens (AgELISA): ¶IRR = 0.57 (95%BCI: 0.3-1.0) |
Low; Valid test | Low: randomized and adjusted for baseline prevalence |
Moderate: High losses to follow- up |
Evaluated not needed / only new cases included |
Good / areas similar to Mbulu district |
Short follow-up of 2- 9 months. |
| Mexico [13] |
Antibodies (EITB) : Pre: 5.2%; Post: 1.2% PPR: 0.24 (95% CI : 0.05; 1.06). |
Low: Valid test | High: not controlled, no randomization |
High: Sampling not described |
Ignored / ignored | Poor / poor | |
| Ecuador [20] |
Inspection at Slaughterhouse: Pre : 11.4%; Post : 2.6% PPR : 0.23 (0.06-0.85) |
High: Poorly described method |
High: not controlled, no randomization |
High: Sampling not described |
Ignored / ignored | Poor / poor | Fewer infected pigs may have been sent to the slaughterhouse after education. |
| Mexico [27] |
Antibodies (AgELISA): Pre: 17.7%; Post: 13.3% PPR: 0.75 (0.50-1.11) Tongue inspection: Pre: 7.0%; Post: 0.5% PPR: 0.07 (0.02-0.29) Ultrasound: Pre: 3.6%; Post: 0.3% PPR: 0.07 (0.01-0.54) |
High : Poor tests | High : not controlled, no randomization |
High: large losses to follow-up; sampling not described |
Ignored / Ignored | Poor / poor | Poorly described methods; errors in calculation in the Tables and in p- values reported |
PPR: Prevalence Proportion Ratio
CI : Confidence Interval
IRR: Incidence Rate Ratio
OR: Odds Ratio
GEE: Generalized Estimating Equations
EITB: Enzyme linked immunoelectrotransfer blot assay to detect antibodies to T. solium
AgELISA : Enzyme linked Immunosorbent assay to detect antigens to T. solium
Effectiveness of mass drug administration of antiparasitics to humans as the sole intervention
Both praziquantel and niclosamide are on the WHO essential drugs list [29]. The effect of Mass Drug Administration (MDA) of praziquantel or niclosamide on reducing the prevalence of taeniasis and human or porcine cysticercosis has been evaluated in three community-based studies in Guatemala [17] and Mexico [15, 16]. Yet, no randomized clinical trials estimating the efficacy of these drugs to treat taeniasis could be found in Medline. It may be that the absence of a gold standard to diagnose taeniasis makes it difficult to know who is infected, leading to a challenge in assessing efficacy. An estimated efficacy of 77.9% (95%CI: 66.7%-86.2%) of niclosamide is probably the best available [30]. According to a review [31], the efficacy of praziquantel (5mg/kg) ranges between 67% and 94% while a dose of 10 mg/kg would be 100% efficacious, but the assessment of taeniasis in these studies were problematic. The three reviewed community-based studies used a pre-post intervention prevalence comparison design without a control group or randomization and were conducted in one [15, 16] and two villages [17]. While the authors suggested that MDA could reduce taeniasis and cysticercosis in the short or long term, only one study used a 42 months follow-up [16]. Taeniasis was measured with coproscopy and copro-antigen [32] tests in two studies [16, 17], while only coproscopy, which has low sensitivity to detect T. solium [33], was used in the remaining study [15]. The presence of antibodies to T. solium antigens as suggestive of human cysticercosis was measured by EITB [34] in one study [16] and by ELISA [35], which has poor specificity and mediocre sensitivity [36], in another one [15]. Two studies [16, 17] used EITB [34] to determine antibody seroprevalence for porcine cysticercosis. All studies found a reduction in taeniasis prevalence in the short term, although not always statistically significant, with Prevalence Proportion Ratios (PPR) of 0.47 (95%CI: 0.20-1.11) after 6 months [16], 0.28 (95%CI: 0.15-0.53) after 10 months [17], and 0 (95%CI: undefined) after 12 months [15]. In the longer term, a PPR of 0.44 (95%: 0.13-1.47) after 42 months was obtained, but this study used data with 83% of the study population pre-treatment being lost to follow-up [16]. When only those followed-up for 42 months were included, a reduction in prevalence was observed, but there was insufficient information to estimate a PPR. The PPR of human cysticercosis could be estimated at 1.77 (95%CI: 1.38-2.29) 6 months post MDA and at 0.39 (95%CI: 0.17-0.88) at 42 months using the EITB [16] and at 0.65 (95%CI: 0.39-1.10) at 12 months using the antibody-detecting ELISA test [15]. The authors could not provide a reasonable explanation for the increase in human sero-prevalence after 6 months, which was also observed when only including those followed-up for 42 months [16]. No such increase was observed in the seroprevalence of porcine cysticercosis. Indeed, the PPR of MDA on porcine cysticercosis could be estimated to 0.46 (95%CI: 0.21-1.04) after 6 months, 0.13 (95%CI: 0.09-0.20) after 10 months, and 0.70 (95%CI: 0.32-1.53) after 42 months [16, 17]. One important limitation of [17] is that sampled pigs were considerably younger post-intervention, introducing a considerable confounding bias that could increase the magnitude of the effect.
To summarize, although these studies suggest some effect of MDA on taeniasis and cysticercosis, they all present important biases, most of which are summarized in the last section of this review. Another important limitation is the lack of assessment of the effect of repeated MDA. In conclusion, given the poorly designed nature of the studies, we have very little scientific evidence to support that community-based MDA are sufficient to generate an effective control of T. solium.
Effectiveness of mass drug administration of anti-parasitic treatment to pigs as the sole intervention
We were unable to identify studies where anti-parasitic MDA to pigs was the sole intervention implemented at the community-level. The efficacy and safety of anti-helminthic drugs established in experimental studies were recently reviewed [37], but with little criticism and assessment of biases. The most recent experiment compared the efficacy of nine different regimens [38]. Although they have limitations, these studies suggest oxfendazole (30mg/kg) to be the most effective drug to treat cysts in pig muscles, but less so in pig brains [37, 38]. We could only identify one randomized controlled trial estimating the effectiveness of oxfendazole in field conditions [39]. In this trial, 216 piglets aged 4 months were blocked-randomized (blocked by litter) to receive 1 dose of oxfendazole (30 mg/kg) at 4 months (1 piglet per litter), 2 doses at 4 and 9 months (1 piglet per litter) or serve as controls (2 piglets per litter). Oxfendazole reduced the incidence rate of infection, especially at older ages.
Unfortunately, inappropriate statistical analyses were applied by ignoring the block randomization and clustering and using a logistic regression to analyse a common outcome [40]. This resulted in overestimating the magnitude and precision the treatment effect. In addition, several piglets were lost to follow-up. If the reason for the loss was linked to the outcome in only one group, this could introduce a selection bias, which direction is difficult to predict. Acknowledging these limitations, one can conclude that oxfendazole is likely to reduce porcine cysticercosis, but to a lesser magnitude to what was reported [39].
To summarize, despite abundant literature on the efficacy of anti-parasitic treatments for porcine cysticercosis, we were unable to find studies assessing the effectiveness of community-based delivery of porcine MDA alone on cysticercosis.
Effectiveness of pig vaccination alone
Three major vaccines have been assessed in field studies, namely: 1) a vaccine using crude antigen extracts collected from metacestodes of infected pigs developed by the Molinari group [41], 2) a recombinant oncosphere antigen-based TSOL16 or TSOL18 vaccine developed by the Lightowlers group [42] and 3) a peptide-based S3PVac developed by the Sciutto group [43]. While TSOL18 has been tested for its effectiveness in field-based randomized controlled trials in Peru (with TSOL16) [44] and Cameroon [45], no implementation or measure at the community-level has been assessed. The effect of both S3PVac [26] and the crude extract vaccine [22] have been assessed using community-level outcomes in Mexico, but unfortunately, both used the poorly accurate tongue examination method for diagnosing porcine cysticercosis, making the interpretation of the results extremely difficult. Indeed, considering that tongue inspection has sensitivity and specificity values of around 50% and 80% [46], respectively, the direction of the bias is difficult to predict. This limitation is in addition to the lack randomization, control group, control for confounding, and possible selection bias. We can henceforth conclude that there is insufficient evidence to determine if porcine vaccination impacts the transmission of T. solium at the community level.
Several controlled trials have been conducted in the field with pigs being randomized (usually within a same litter) to receive a vaccine or placebo, and the outcome measured by the number of cysts or viable cysts found at necropsy [43, 44, 45, 47]. Three doses of TSOL18 (at baseline, 4 weeks, and 4 months) in combination with oxfendazole at 4 weeks, compared to a treatment with oxfendazole at 4 weeks, was very effective at eliminating any cysts in the vaccinated group, while 19.6% of the control group had muscle cysts (20 pigs with 3 to 37,080 cysts) [45]. In a similar trial, 137 pairs of piglets aged 2-4 months were randomized to receive either TSOL16-18 at baseline with a booster at 4 weeks combined with a swine classical fever vaccine or to receive a swine classical vaccine only, and then necropsied 7 months later [44]. Of the 100 pairs necropsied, 4 had both piglets infected, 13 had control piglets infected and vaccinated piglets uninfected, and 3 had the vaccinated piglets infected and the control piglets uninfected. Most cysts found in the vaccination group were degenerated, in contrast to the viable cysts found in the control group. Both studies showed TSOL18 and TSOL16-18 to be effective vaccines at the pig level, as long as at least two doses at 4 weeks interval were given. The S3PV vaccine also showed promising results [43, 47]. Muscle cysts were found in 7.5% of piglets vaccinated with 2 doses of S3PV (at 60 and 90 days of age) and in 15.8% of control piglets [43]. Despite this interesting results, the use of inappropriate statistical analyses makes the interpretation of the reduction in cysts number difficult. In another trial where 331 of 1047 pigs randomized were autopsied, the odds of presenting cysts at necropsy was 2.3 (95%CI: 1.2-4.3) times higher in the control group than in the vaccinated group (two doses of S3PV at 3-4 months and at 4-5 months of age), in a model including castration status and weight to adjust for factors associated with losses-to-follow-up. These randomized trials suggest that pig vaccination is effective at preventing infection, with TSOL16-18 appearing to show a higher efficacy than S3PV when two doses are used. However, the magnitude of the efficacy is difficult to assess with the data provided by the authors and the improper statistical analyses used in most cases. In addition, no evidence is available on the community-level effect of vaccinating pigs on human taeniasis and porcine and human cysticercosis. Pig vaccination remains problematic in terms of its sustainability in very poor areas where farmers cannot even afford to feed their pigs.
Effectiveness of a combination of mass drug delivery of anti-parasitic to pigs and humans
One pre-post community-based randomized controlled trial assessed the effectiveness of a program using MDA of oxfendazole (30mg/kg, two rounds at an unspecified interval) to pigs and of praziquantel (5mg/kg, one round, 75% coverage) to humans [24]. The study divided nine endemic villages into 12 “treatment units” to increase sample size, but due to mistakes in implementation, seven units received the intervention, while five served as control, with three villages being “split” into two units. In addition, one split village was missing baseline incidence rate estimates. The break in randomization resulted in an imbalance in the baseline prevalence of porcine cysticercosis, which may lead to AN over-estimation of the intervention effectivenessSimilarly, the “split” strategy will likely result in contamination, leading to under-estimating the effectiveness. The authors used a logistic regression to analyze incidence rate data, included each village as an independent factor, ignored clustering, and did not interpret the interaction term correctly. These improper analyses along with important issues with the study design make it impossible to accurately interpret the results of this study.
Effectiveness of educational programs alone
Education is recognized as an important tool in the control of cysticercosis [2-6, 24]. Three studies have assessed the effectiveness of education programs for pig farmers [14, 19] or the general population [18] on reducing human taeniasis [18], porcine cysticercosis [14, 18] or improving knowledge, attitudes and practices [14, 18, 19]. In a pre-post prevalence comparison study conducted in one Mexican village [18], an education program including the use of pamphlets, posters and two videos designed following in-depth interviews, led to a PPR of 0.64 (95%CI: 0.21-2.02) for taeniasis as measured by a copro-antigen assay 6 months post-intervention. This study suffers from the lack of a control group and randomization as well as a very high proportion of losses to follow-up.
The Mexican group also measured the change in porcine cysticercosis prevalence (194 at baseline and 165 at 6-months post-intervention) using EITB assay and obtained a PPR of 0.24 (95%CI: 0.05-1.06), but pig sampling was not described [18]. A much better designed community-based randomized controlled trial evaluating the effectiveness of a pig management educational program developed following a PRECEDE-PROCEED approach was conducted in 42 villages of northern Tanzania [9]. An incidence rate ratio of 0.57 (95%CI: 0.3-1.0) for porcine cysticercosis (measured with Ag-ELISA [48] adjusted for baseline prevalence of porcine cysticercosis was obtained. Among all the papers reviewed, this is the only paper that followed the CONSORT guidelines to report results of community-based randomized controlled trials [49]. These authors are also the only ones to conduct a cost analysis, demonstrating that the education program was cost beneficial to pig farmers, with a net present value of US$3507 (95%CI: $3421-$3591) [50]. Nonetheless, this study suffers from two important limitations, namely a short median follow-up time (4 months) and a large proportion of losses-to-follow-up (52%) resulting from a severe drought which forced farmers to sell or eat the pigs that they were given. This makes it impossible to assess the long term impact of the intervention. All three studies assessed the impact of their education program on knowledge, attitudes and practices regarding cysticercosis [14, 18, 19]. The study in Kenya interviewed 296 pig farmers before and twice after receiving a workshop and one-to-one training using a train-the-trainer approach, but the number of farmers interviewed at each visit varied [19]. Only the Tanzanian study analyzed the data at the community-level and was designed in such manner that the effect of monitoring alone could be determined [14]. Interestingly, monitoring alone had a strong effect on knowledge, meaning that farmers not living in intervention villages may have heard about it or that being given sentinel pigs made them improve their knowledge about cysticercosis. Since the Kenyan [19] and Mexican [18] studies did not have a control group, it is impossible to determine if the observed improvements in knowledge were due to monitoring alone. In Tanzania and Mexico, the only reported practices improved by the intervention were a reduction in eating contaminated pork and an increased practice of boiling drinking water [14, 18]. In Kenya, there was a tendency for improvement in the proportion of farmers keeping their pigs tethered 100% of the time, but the results among those not lost to follow-up was inconclusive [19]. All of these studies suffer from a possible reporting bias for practices as research participants may report preferred behaviors instead of the truth, as noticed by [18]. To summarize, education alone seems to reduce the level of porcine cysticercosis at least in the short term, but the impact on knowledge and practices is less certain. Endemic areas for cysticercosis are generally very poor, which limits the ability of farmers to restrict pigs from roaming, and also may limit the ability to maintain latrines. Access to water could also limit improvement in handwashing. This probably explains the general lack of improvement in practices. Nonetheless, the presence of a research team appears to improve knowledge, which could in the longer term improve practices, but this will require longer follow-ups to take place.
Effectiveness of programs combining education activities and mass drug administration of anti-parasitic to humans or vaccination of pigs
Two studies combined education with human MDA to control cysticercosis [20, 25] while one combines education to porcine vaccination (27). The first study was a pre-post proportion comparison study conducted in 18 villages in Salamá county (Honduras) involved a very intense, multi-facetted intervention, spanning over several years (see Table 1a) [20]. The intervention was associated with a PPR of 0.38 (95%CI: 0.16-0.89) in the proportion of epilepsy cases showing lesions of neurocysticercosis [20]. In addition to being a non-randomized, not controlled pre-post comparison study, there were only new onset seizure cases included post intervention (from 1997 to 2005), while all cases of active epilepsy were included at baseline. This would lead to a higher prevalence of neurocysticercosis at baseline due to old calcified lesions still causing seizures, over-estimating the effect of the intervention. The second study, undertaken in Ecuador, implemented a shorter but still intense intervention where during door-to-door visits, leaflets on cysticercosis/taeniasis control, verbal health education and an offer for treatment with praziquantel (5mg/kg) were provided to all individuals living in one canton of Ecuador [25]. Taeniasis was measured as self-report of parasite expulsion, an extremely unreliable measurement tool, especially without the use of a purgation agent, in addition to the possible under-reporting at follow-up. This design flaw invalidates the observed reduction in the prevalence of human taeniasis. The effect on porcine cysticercosis was assessed through a vaguely described “careful inspection” of pigs after slaughter at the Canton’s slaughterhouse. Since education may teach farmers to assess infection by looking under pigs’ tongues, owners of infected pigs may have been less inclined to send them to the official slaughterhouse after the intervention, which too invalidates the observed reduction in the prevalence of porcine cysticercosis. The third study, conducted in three municipalities of Mexico, was a pre-post prevalence comparison evaluating the effect of vaccinating all pigs aged more than 2 months with S3Pvac at least three times with an educational program including meetings, distribution of educational pamphlets and videos about T. solium (27). The authors report a reduction in the prevalence using tongue inspection, ultrasound, and to a lower extent, AbELISA, but the study suffers from many biases making it difficult to interpret the results. The poor designs of these three studies make it impossible to draw firm conclusions on the effect of combined interventions on the control of cysticercosis.
Results from theoretical transmission dynamics models
In the absence of convincing evidence from field trials, transmission dynamics models can be helpful in ranking the relative effectiveness of control strategies while taking the dynamics of the infection as well as herd immunity into account. This study modeling the transmission dynamics of T. solium between pigs and humans suggest that the most sustainable intervention remains the improvement of sanitation and pig management practices, but the effect of such improvement would need to be considerable [51]. This model is limited by its lack of age structure, seasonality and possible clustering of infection.
Epidemiological methods limitations of the reviewed studies and conclusion
All the articles reviewed aimed at reducing human cysticercosis or taeniasis [15-18, 20, 26] and all [16-18, 21, 22, 26, 27], except two [14, 23], aimed at reducing porcine cysticercosis, lacked the use of randomization and of a control group, preventing control for confounding factors through study design or statistical methods. Randomization insures that all confounding factors, measured or unmeasured, are well balanced, preventing confounding bias. They are therefore susceptible to confounding bias, whose direction and magnitude is difficult to predict. The use of a control group insures that participation itself is not the cause of the change in the outcome through time. For instance, without a control group, any changes in environmental or behavioral factors through time may distort the true effectiveness of the intervention, leading to an overestimation the effectiveness of the interventions. Indeed, improvement in education levels and pig management practices through time was acknowledged in one study [16] and the impact of monitoring (i.e. time) on knowledge was demonstrated in another [14]. The lack of control group also prevents statistical adjustment for confounding. None of these studies, except for [14, 23], had a sample size large enough to generate statistical power and generalize the results, with one village or community included where very intense interventions were offered. Such approaches are unlikely to be sustainable when used in larger settings with limited resources. The study of a single community also limits the assessment of potential variability in the effectiveness of the intervention. In addition, except for [14, 16, 23], no study acknowledged the non-independence of individuals studied pre and post intervention, leading to the use of improper statistical analyses and biased results. The studies conducted in Tanzania [14] and Peru [23] remain the best available, but unfortunately did not report on the effect of the intervention on human taeniasis or cysticercosis, and also had some limitations.
We can conclude that there is insufficient evidence to suggest any community-based intervention to control human and porcine cysticercosis. Given this lack of evidence, it is very unlikely for the infection to be eradicated from poor endemic areas in the foreseeable future. Future studies should carefully follow recommendations provided in by Thompson and coworkers [52] for the conduct of community-based controlled randomized trials, as well as adhere to the CONSORT guidelines when reporting the results [49]. This will considerably improve the evidence about the effectiveness of alternative control strategies for T. solium at the community level and hopefully lead to the implementation of cost-effective control strategies.
Acknowledgements
This work was conducted with the support of the National Institute of Neurological Disorders and Stroke (NINDS) and of the Forgarty International Center (FIC) of the National Institutes of Health (NIH) under the Brain in the Developing World: Research across the life span program, grant R01NS064901.
Footnotes
Conflict of Interest
Hélène Carabin and Aminata A Traoré declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors
References
Papers of particular interest, published recently, have been highlighted as:
* Of importance
** Of major importance
- 1.Centers for Disease Control and Prevention Recommendations of the International Task Force for Disease Eradication. Mort Morb Week Rep. 1993;42:1–27. [Google Scholar]
- 2**.The Carter Center [Last accessed on August 6, 2014];Summary of the twenty-first meeting of the international task force for disease eradication (II) 2013 Jul 10; Report available from: http://www.cartercenter.org/resources/pdfs/news/health_publications/itfde/ITFDE-summary-071013.pdf. This report is of importance because it emphasizes for the first time the key role of human hygiene and sanitation as promising strategy to control cysticercosis.
- 3.Willingham AL, 3rd, Wu HW, Conlan J, Satrija F. Combatting Taenia solium cysticercosis in Southeast Asian and opportunity for improving human health and livestock production. Adv Parasitol. 2010;72:235–66. doi: 10.1016/S0065-308X(10)72009-1. [DOI] [PubMed] [Google Scholar]
- 4.Murrell KD, editor. WHO/FAO/OIE Guidelines for the Surveillance, Prevention and Control of Taeniosis/Cysticercosis. Office International des Epizooties; Paris: 2005. [Google Scholar]
- 5.O’Neil SE, Winthrop KL, Gonzalez AE. Cysticercosis control: bringing advances to the field. J Glob Infect Dis. 2011;3:156–160. doi: 10.4103/0974-777X.81693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fleury A, Sciutto E, de Aluja AS, et al. Foyaca-Sibat H, editor. [Last accessed on Aug 6, 2014];Control of Taenia solium transmission of taeniosis and cysticercosis in endemic countries: the roles of continental networks of specialists and of local health authorities. Novel Aspects on Cysticercosis and Neurocysticercosis. InTech. 2013 DOI: 10.5772/51286. Available from: http://www.intechopen.com/books/novel-aspects-on-cysticercosis-and-neurocysticercosis/control-of-taenia-solium-transmission-of-taeniosis-and-cysticercosis-in-endemic-countries-the-roles-
- 7.Flisser A. Taeniasis and cysticercosis due to Taenia solium. In: Sun T, editor. Progress in Clinical Parasitology. CRC Press; New York: 1994. pp. 77–116. [PubMed] [Google Scholar]
- 8.Pawlowski Z, Murrell KD. Taeniasis and cysticercosis. In: Hui YH, Sattar SA, Murrell KD, Nip WK, Stanfield PS, editors. Foodborne Disease Handbook (Second Edition) 2000, Volume 2: Viruses, Parasites, Pathogens and HAACP. Marcel Dekker, Inc; New York: pp. 217–227. [Google Scholar]; Maya C, Torner-Morales FJ, Lucario ES, Hernandez E, Jumenez B. Viability of six species of larval and non-larval helminth eggs for different conditions of temperature, pH and dryness. Water Res. 2012;46:4770–4782. doi: 10.1016/j.watres.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 9.Maya C, Torner-Morales FJ, Lucario ES, Hernandez E, Jumenez B. Viability of six species of larval and non-larval helminth eggs for different conditions of temperature, pH and dryness. Water Res. 2012;46:4770–4782. doi: 10.1016/j.watres.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 10.Flisser A. Neurocysticercosis in Mexico. Parasitol Today. 1988;4:131–137. doi: 10.1016/0169-4758(88)90187-1. [DOI] [PubMed] [Google Scholar]
- 11.Pouedet MSR, Zoli AP, Nguekam L, Vondou L, Assana E, Speybroeck N, Berkvens D, Dorny P, Brandt J, Geerts S. Epidemiological survey of swine cisticercosis in two rural communities of West-Cameroon. Vet Parasitol. 2002;106:45–54. doi: 10.1016/s0304-4017(02)00035-3. [DOI] [PubMed] [Google Scholar]
- 12.Shey-Njila O, Zoli PA, Awah-Ndukum J, Nguekam JP, Assana E, Byambas P, Dorny P, Brandt J, Geerts S. Porcine cysticercosis in village pigs of northwest Cameroon. J Helminthol. 2003;77:351–354. doi: 10.1079/joh2003179. [DOI] [PubMed] [Google Scholar]
- 13.Carabin H, Ndimubanzi PC, Budke CM, et al. Clinical manifestations associated with neurocysticercosis: a systematic review. PLoS Neg Trop Dis. 2011;5:e1152. doi: 10.1371/journal.pntd.0001152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ngowi HA, Carabin H, Kassuku AA, et al. A health-education intervention trial to reduce porcine cysticercosis in Mbulu District. Tanzania. Prev Vet Med. 2008;85:52–67. doi: 10.1016/j.prevetmed.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Diaz Camacho SP, Candil Ruiz A, Suate Peraza V, et al. Epidemiologic study and control of Taenia solium infections with praziquantel in a rural village of Mexico. Am J Trop Med Hyg. 1991;45:522–531. doi: 10.4269/ajtmh.1991.45.522. [DOI] [PubMed] [Google Scholar]
- 16.Sarti E, Schantz PM, Avilla G, Ambrosio J, Medina-Santillan R, Flisser A. Mass treatment against human taeniasis for the control of cysticercosis: a population-based intervention study. Trans Roy Soc Trop Med Hyg. 2000;94:85–89. doi: 10.1016/s0035-9203(00)90451-6. [DOI] [PubMed] [Google Scholar]
- 17.Allan JC, Velasquez-Tohom M, Fletes C, et al. Mass chemotherapy for intestinal Taenia solium infection: effect on prevalence in humans and pigs. Trans R Soc Trop Med Hyg. 1997;91:595–598. doi: 10.1016/s0035-9203(97)90042-0. [DOI] [PubMed] [Google Scholar]
- 18.Sarti E, Flisser A, Schantz PM, et al. Development and evaluation of a health education intervention against Taenia solium in a rural community in Mexico. Am J Trop Med Hyg. 1997;56:127–132. doi: 10.4269/ajtmh.1997.56.127. [DOI] [PubMed] [Google Scholar]
- 19.Wohlgemut J, Dewey C, Levy M, Mutua F. Evaluating the efficacy of teaching methods regarding prevention of human epilepsy caused by Taenia solium neurocysticercosis in Western Kenya. Am J Trop Med Hyg. 2010;82:634–642. doi: 10.4269/ajtmh.2010.09-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medina MT, Aguilar-Estrada RL, Alvarez A, et al. Reduction in rate of epilepsy from neurocysticercosis by community interventions: the Salamá, Honduras study. Epilepsia. 2011;52:1177–1185. doi: 10.1111/j.1528-1167.2010.02945.x. [DOI] [PubMed] [Google Scholar]
- 21.Keilbach NM, de Aluja AS, Sarti-Gutierrez E. A programme to control taeniasis-cysticercosis (T. solium): experiences in a Mexican village. Acta Leiden. 1989;57:181–189. [PubMed] [Google Scholar]
- 22.Molinari JL, Rodríguez D, Tato P, et al. Field trial for reducing porcine Taenia solium cysticercosis in Mexico by systematic vaccination of pigs. Vet Parasitol. 1997;69:55–63. doi: 10.1016/s0304-4017(96)01102-8. [DOI] [PubMed] [Google Scholar]
- 23.Garcia HH, Gonzalez AE, Gilman RH, et al. Combined human and porcine mass chemotherapy for the control of T. solium. Am J Trop Med Hyg. 2006;74:850–855. [PubMed] [Google Scholar]
- 24.Garcia HH, Gonzalez AE, Rodriguez S, et al. Epidemiology and control of cysticercosis in Peru [article in Spanish] Rev Peru Med Exp Salud Publica. 2010;27:592–7. doi: 10.1590/s1726-46342010000400016. [DOI] [PubMed] [Google Scholar]
- 25.Cruz M, Davis A, Dixon H, Pawlowski ZS, Proano J. Operational studies on the control of Taenia solium taeniasis/cysticercosis in Ecuador. Bull World Health Organiz. 1989;67:401–407. [PMC free article] [PubMed] [Google Scholar]
- 26.Sciutto E, Morales J, Martinez JJ, et al. Further evaluation of the synthetic peptide vaccine S3Pvac against Taenia solium cysticercosis in pigs in an endemic town of Mexico. Parasitology. 2007;164:124–133. doi: 10.1017/S0031182006001132. [DOI] [PubMed] [Google Scholar]
- 27.De Aluja AD, Suarez-Martin R, Sciutto-Conde E, et al. Evaluacion del impacto de un programa de control de la teniasis-cisticercosis. Salud Pública Méx. 2014;56:259–265. [PubMed] [Google Scholar]
- 28.Wu W, Qian X, Huang Y, Hong Q. A review of the control of Clonorchiasis sinensis and Taenia solium taeniasis/cysticercosis in Chin. Parasitol Red. 2012;111:1879–84. doi: 10.1007/s00436-012-3152-y. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization . Drugs used in parasitic diseases. Second Edition WHO; Geneva: 1995. WHO Model Prescribing Information. [Google Scholar]
- 30.Bustos JA, Rodrigues S, Jimenez JA. Detection of Taenia solium taeniasis coproantigen is an early indicator of treatment failure for taeniasis. Clin Vaccine Immunol. 2012;19:570–573. doi: 10.1128/CVI.05428-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pawlowski ZS. Efficacy of low doses of praziquantel in taeniasis. Acta Trop. 1991;48:83–88. doi: 10.1016/0001-706x(90)90046-3. [DOI] [PubMed] [Google Scholar]
- 32.Allan JC, Avila G, Garcia-Noval J, Flisser A, Craig P. Immunodiagnosis of taeniasis by coproantigen detection. Parasitol. 1990;101:473–7. doi: 10.1017/s0031182000060686. [DOI] [PubMed] [Google Scholar]
- 33.Praet N, Verweii JJ, Meape KE. Bayesian modelling to estimate the test characteristics of coprology, coproantigen ELISA and a novel real-time PCR for the diagnosis of taeniasis. Trop Med Int Health. 2013;18:608–614. doi: 10.1111/tmi.12089. [DOI] [PubMed] [Google Scholar]
- 34.Tsang VC, Brand HA, Boyer AE. An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium) J Infect Dis. 1989;159:50–59. doi: 10.1093/infdis/159.1.50. [DOI] [PubMed] [Google Scholar]
- 35.Larralde C, Lacelette JP, Madrazo I, et al. Reliable serology of Taenia solium cysticercosis with antigens from cyst vesicular fluid: ELISA and hemagglutination tests. Am J Trop Med Hyg. 1986;35:965–973. doi: 10.4269/ajtmh.1986.35.965. [DOI] [PubMed] [Google Scholar]
- 36.Praet N, Rodriguez-Hidalgo R, Speybroeck N, et al. Infection with versus exposure to Taenia solium: what do serological test results tell us? Am J Trop med Hyg. 2010;83:413–415. doi: 10.4269/ajtmh.2010.10-0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mkupasi EM, Sikasunge CS, Ngowi HA, Vang Johansen M. Efficacy and safety of anthelmintics tested against Taenia solium cysticercosis in pigs. PLoS Negl Trop Dis. 2013;7:e2200. doi: 10.1371/journal.pntd.0002200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gonzalez AE, Bustos JA, Jimenez JA, et al. Efficacy of diverse antiparasitic treatments for cysticercosis in the pig model. Am J Trop Med Hyg. 2012;87:292–296. doi: 10.4269/ajtmh.2012.11-0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pondja A, Neves L, Mlangwa J, et al. Use of oxfendazole to control porcine cysticercosis in a high-endemic area of Mozambique. PLoS Negl Trop Dis. 2012;6:e1651. doi: 10.1371/journal.pntd.0001651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 41.Molinari JL, Soto R, Tato P, et al. Immunization against porcine cysticercosis in an endemic area in Mexico: a field and laboratory study. Am J Trop Med Hyg. 1993;49:502–512. doi: 10.4269/ajtmh.1993.49.502. [DOI] [PubMed] [Google Scholar]
- 42.Lightowlers MW. Eradication of Taenia solium cysticercosis: a role for vaccination of pigs. Int J Parasitol. 2010;40:1183–1192. doi: 10.1016/j.ijpara.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 43.Huerta M, de Aluja AS, Fragoso G, et al. Synthetic peptide vaccine against Taenia solium pig cysticercosis: successful vaccination in a controlled field trial in rural Mexico. Vaccine. 2001;20:262–266. doi: 10.1016/s0264-410x(01)00249-3. [DOI] [PubMed] [Google Scholar]
- 44.Jayashi CM, Kyngdon CT, Gauci CG. Successful immunization of naturally reared pigs against porcine cysticercosis with a recombinant oncosphere antigen vaccine. Vet Parasitol. 2012;188:261–267. doi: 10.1016/j.vetpar.2012.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Assana E, Kyngdon CT, Gauci CG. Elimination of Taenia solium transmission to pigs in a field trial of the TSOL18 vaccine in Cameroon. Int J Parasitol. 2010;40:515–519. doi: 10.1016/j.ijpara.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krecek RC, Michael LM, Schantz PM, et al. Prevalence of Taenia solium cysticercosis in swine from a community-based study in 21 villages of the Eastern Cape Province, South Africa. Vet Parasitol. 2008;154:38–47. doi: 10.1016/j.vetpar.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 47.Morales J, Martínez JJ, Manoutcharian K, et al. Inexpensive anti-cysticercosis vaccine: S3Pvac expressed in heat inactivated M13 filamentous phage proves effective against naturally acquired Taenia solium porcine cysticercosis. Vaccine. 2008;26:2899–2905. doi: 10.1016/j.vaccine.2008.03.042. [DOI] [PubMed] [Google Scholar]
- 48.Dorny P, Phiri IK, Vercruysse J, et al. A Bayesian approach for estimating values for prevalence and diagnostic test characteristics of porcine cysticercosis. Int J Parasitol. 2004;34:569–576. doi: 10.1016/j.ijpara.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 49.Campbell MK, Piaggio G, Elbourne, Altman DG, for the CONSORT Group Consort 2010 statement: extension to cluster randomised trials. Brit Med J. 2012;345:e5661. doi: 10.1136/bmj.e5661. [DOI] [PubMed] [Google Scholar]
- 50.Ngowi HA, Mlangwa JED, Carabin H, et al. [last accessed on Aug 20, 2014];Financial efficiency of health and pig management education intervention in controlling porcine cysticercosis in Mbulu District, northern Tanzania. Livestock Res Rural Dev. 2007 :19. Available at URL: http://www.lrrd.org/lrrd19/5/ngow19062.htm.
- 51.Kyvsgaard NC, Johansen MV, Carabin H. Simulating transmission and control of Taenia solium infections using a Reed-Frost stochastic model. Int J Parasitol. 2007;37:547–558. doi: 10.1016/j.ijpara.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 52.Thompson B, Coronado G, Snipes SA, Puschel K. Methodological advances and ongoing challenges in designing community-based health promotion programs. Ann Rev Pub Health. 2003;24:315–340. doi: 10.1146/annurev.publhealth.24.100901.140819. [DOI] [PubMed] [Google Scholar]


