Abstract
Socially and culturally embedded norms regarding smoking may be one pathway by which individuals adopt smoking behaviors. However, few studies have examined if social norms operate in young adults, a population at high risk of becoming regular smokers. There is also little research examining correlates of social norms in populations with a large immigrant segment, where social norms are likely to differ from the receiving country and could contribute to a better understanding of previously reported acculturation-health associations. Using data from a nationally representative sample of young adults in the United States reached via a novel cell-phone sampling design, we explored the relationships between acculturation proxies (nativity, language spoken and generational status), socioeconomic position (SEP), smoking social norms and current smoking status among Latinos 18–34 years of age (n=873). Specifically, we examined if a measure of injunctive norms assessed by asking participants about the acceptability of smoking among Latino co-ethnic peers was associated with acculturation proxies and SEP. Results showed a strong gradient in smoking social norms by acculturation proxies, with significantly less acceptance of smoking reported among the foreign-born and increasing acceptance among those speaking only/ mostly English at home and third-generation individuals. No consistent and significant pattern in smoking social norms was observed by education, income or employment status, possibly due to the age of the study population. Lastly, those who reported that their Latino peers do not find smoking acceptable were significantly less likely to be current smokers compared to those who said their Latino peers were ambivalent about smoking (do not care either way) in crude models, and in models that adjusted for age, sex, generational status, language spoken, and SEP. This study provides new evidence regarding the role of social norms in shaping smoking behaviors among Latino young adults and suggests distinct influences of acculturation proxies and socioeconomic condition on smoking social norms in this population.
Keywords: Latinos, smoking, social norms, young adults, acculturation
Background
Smoking remains a significant public health problem among Latinos in the United States (US). Smoking prevalence among Latino adults can range from 12.5–18% depending on the data source1–3 and tobacco use is implicated in the top 3 leading causes of death in this population (i.e., cancer, stroke and heart disease).4 Similar to other racial/ ethnic groups, recent data also suggest a stagnation in the decline of smoking prevalence over the last few years among Latinos.2 While overall smoking prevalence among Latinos is generally lower than in the general US population (12.5% vs. 18.1%),1 notable differences exist by nativity status. For example, foreign-born Latinos living in the United States less than ten years are less likely to be current smokers than their US-born peers (9.6% vs. 16.2%), but longer duration of stay in the US is associated with increasing smoking prevalence, particularly among women.5–8
One explanation proposed for this nativity-smoking association is that acculturation processes influence the adoption of smoking behaviors among Latinos. Acculturation is generally defined as the ideological and behavioral exchange that takes place as individuals from one cultural group interact with those of another and can involve both the retention or loss of cultural norms, views, and practices.9 Commonly used acculturation proxies include nativity status, length of stay in the US, generational status (i.e., whether person and parents are US or foreign-born) and language-based items. While studies have consistently shown that acculturation is associated with health generally, and smoking behaviors including quit attempts,10 little is known about the underlying mechanisms explaining these associations. 11–14 Specifically, there has been a growing interest in recent years to broaden the scope of acculturation research to consider, for example, how immigration policies and structural disadvantage influence health among Latinos,15,16 or how distinct forms of social disadvantage interact to influence the adoption of health-damaging behaviors,17 to explicitly measuring the social and cultural factors that are hypothesized to underlie acculturation.18 In the context of smoking behaviors, social norms regarding smoking may represent one pathway underlying acculturation-health associations.
Theoretical perspectives on how social norms influence smoking behaviors
Social norm theory has received relatively little empirical examination in population health research despite the long history of scholarship on this topic.19,20 Social norms can be defined as the rules of acceptable behavior that operate within a group that dictate the boundaries of permissible behavior and promote or deter the adoption of health behaviors.21–23 In the now classic paper by Christakis and Fowler,24 the authors showed that similar to contagion processes typically characteristic of infectious diseases, smoking and smoking cessation were spread through social ties maintained in the offspring of the Framingham Cohort followed over 32 years. Results indicated that that the patterning of smoking behaviors occurred through group processes, whereby groups of individuals started smoking together and groups also quit together. The authors speculated, but were not able to test, that socially or culturally shared norms explained the clustering of smoking and quitting behaviors observed. It stands to reason that membership in socially defined groups such as Latinos may also be associated with social norms that can shape the adoption of smoking behaviors and that immigration or acculturation-related processes may differentially pattern smoking social norms for native and foreign-born groups.
Identifying the specific ways in which social norms influence human behaviors is complex because several different types of normative influences are hypothesized to exist and norms can influence individuals across multiple levels of organization (e.g., as a group-level vs. individual-level phenomenon). Nonetheless, at least two types of social norms dominate the psychological and public health literature.22,25,26 The first of these is defined as descriptive norms and describes what individuals perceive others actually do in a given context.21 For example, questions on descriptive norms among teenagers would ask about the extent to which teens perceive that peers in their schools, neighborhoods or other social groups actually smoke and then determine if a teenager’s perception of the prevalence of smoking is associated with their own current smoking status. The second type of norm, injunctive norms, assesses if individuals perceive a referent group to approve or disapprove of a behavior and how much they are willing to comply with this behavior expectation.21 In this scenario, questions center on determining if perceptions of disapproval of a particular behavior among a referent social group is associated with a person’s engagement in that behavior. Of these two types of norms, injunctive norms may be particularly salient to consider in Latino health research as they are rooted in normative beliefs about acceptable behaviors (rather than what others actually do) and thus would point to belief systems that may promote the adoption of smoking behaviors in Latino populations. Further, the study of normative beliefs allows for the empirical examination of whether belief systems appear to differ between US vs. foreign-born Latinos (an underlying assumption in acculturation research) and thus contribute to ‘unpacking’ aspects of acculturation that may matter for health. Lastly, another theoretical contribution of norms research is that if associations between smoking norms and smoking status hold, it would suggest the need to address culturally-defined norms and belief systems and the multi-level social factors that shape these norms in the design and implementation of health interventions.27–29
Surprisingly, little research has been conducted to examine the influence of social norms on smoking status among Latinos generally, and more specifically among young Latino adults. Young adulthood, an age period typically defined from 18–34 years of age, represents a critical life-course stage during which individuals are at significant risk of developing and maintaining life-long smoking habits and are targets of tobacco marketing. Current evidence suggests that adolescents who initiated and became daily smokers during adolescence became addicted to nicotine by the time they entered young adulthood.30 Surveys that include a racially/ ethnically diverse sample further indicate that anywhere from 17–36% of US-born 18–34 year olds reported being current smokers,31 representing the highest prevalence of smoking by age group. Prior research on social norms has largely focused on adolescent or college-based populations and shown that adolescents who perceive that their friends or acquaintances have acceptable views on smoking are more likely to smoke themselves and have more difficulty quitting smoking.32–35 One study involving racially/ ethnically diverse youth found that social norms regarding the acceptability of smoking among Asian American adolescents was significantly associated with having smoked in the past 30 days.36 Other studies have extended the notion of social norms to characterize it as a group-level phenomenon and shown that school-level and neighborhood-level social norms, for example, are associated with smoking and smoking cessation.25,37 However, to the best of our knowledge, no study has examined the role of social norms shaping smoking status among young Latino adults.
Study Objectives
Our goal in the present study was to contribute to the literature in two ways. First, we examined how acculturation proxies such as nativity, language use and generational status, and measures of socioeconomic position such as education, income and employment, were associated with smoking social norms assessed among young Latino adults participating in a novel study design using cell-phone sampling.38 We hypothesized that the foreign-born, first-generation and Latinos who only or mostly spoke Spanish would have more restrictive norms surrounding smoking, and thus would be more likely to report that smoking is not acceptable in their group of origin when compared to the US-born. For measures of SEP, we hypothesized less acceptance of smoking in higher income, highly educated, and currently employed young adults. Second, we examined if smoking norms were associated with current smoking status among young Latino adults, hypothesizing that those who report that smoking is not acceptable among their Latino peers would have a lower probability of smoking than those who report that smoking is acceptable.
Methods
Data for this study are drawn from the 2011 and 2013 National Young Adult Health Survey (NYAHS). Details on the NYAHS method can be found elsewhere as well as the feasibility of cell-phone sampling for reaching young adults in the U.S. 38 In brief, NYAHS is a stratified random-digit-dial (RDD) cell phone survey of 18- to 34-year young adults. The survey was designed as a nationally representative sample of the young adult population that reached all of the major racial/ ethnic groups in the United States (i.e., African-American, Asian, Latino and non-Latino White) and produced equal sample quality to the Behavioral Risk Factor Surveillance System (BRFSS), an RDD survey of both landline and cell phones38. The participation rate of the young adult population in national health surveys has declined quite drastically over time.39 One proposed explanation for this decline is that young adults have foregone landline telephones in favor of only owning a cell phone at a much higher rate than the general population.40 Additionally, a large share of this population lives in group quarters (e.g. college dormitories or military barracks) and are thus not reachable via typical household based sampling strategies. In fact, about 48% of those 18–24 years of age are enrolled in college and a non-negligible share of them live in dormitories.41 Thus, our sampling approach is novel in that it is an RDD sample of only cell phones and does not include landline phones. This overcomes the challenge of reaching the young adult population as over 95% of them have a cellular phone and the ownership and use of a cell phone is not tied to a specific domicile.42
In the present study, we use the Latino subsample (873 out of a total of 5,966 participants) representing an average of 14% of the total sampled population and constituting a nationally representative sample of young Latino adults in the US. The NYAHS questionnaire was translated into Spanish using back translation techniques and administered in English or Spanish depending on participant request. Participants were asked questions on tobacco use and perceptions, Internet and social media use, obesity and physical activity, and socioeconomic and demographic characteristics. Items about tobacco use were adapted from existing surveillance system to ensure comparability with existing national surveys. All new items, including social norms, were pretested using cognitive interviewing. Cognitive interview participants were racially/ethnically diverse young adults, including Latino individuals, and included college and non–college students. The study was approved by the investigators’ Institutional Review Board.
Outcome Variables
The present study involves two stages of analysis. The first analytic stage examines factors that contribute to smoking social norms (as an outcome) among Latinos. In the second stage of the analysis, we examine if smoking social norms among Latinos is associated with current smoking status. To fill gaps in the literature, we modified previously used questions on injunctive norms that ask respondents their views on the acceptability of smoking in certain groups or settings25 but made the question specific to Latinos. Participants were first asked to identify their origin or ancestry (e.g., Mexican, Puerto Rican, Dominican, South American, etc). Their Latino group of origin was then piped into the question, ‘In general, what do you think [Latino group of origin.] feel about smoking cigarettes?” Response options included ‘Acceptable, Not Acceptable, Do Not Care Either Way, and Do Not Know/ Not Sure”. Participants were classified as having views about co-ethnic peers that accepted, did not accept, or did not care about smoking.
Current cigarette smoking status was our second (binary) outcome. Current smokers were defined as respondents who reported smoking at least 100 cigarettes in their lifetime and who also reported that they now smoke every day or some days. Former smokers were individuals who had smoked 100 or more cigarettes during their lifetime but currently did not smoke. Never smokers were those who reported never having smoked or not having smoked at least 100 cigarettes or more during their lifetime. Respondents were additionally asked to report on how often they smoke (regardless of lifetime smoking) and were classified as smoking every day, some days or not all.
Independent Variables
The main independent variables include acculturation proxies and measures of socioeconomic position. One goal of our research is to contribute empirical evidence on the extent to which theoretically-grounded constructs may be associated with acculturation measures, and thus build an evidence base on the relative merits of this concept in health research. In this regard, we follow the select number of studies in recent years that have attempted to empirically test concepts hypothesized to underlie acculturation, such as notions of familism, fatalism, and social ties.43–47 More specifically, we add to this literature by highlighting the importance of culturally-based domains that may explain population health,11 and could help elucidate the patterning of health disparities. As Airhihenbuwa et al. propose, ‘Culture can be thought of as the building blocks that make up institutions, shared normative values, and ways of knowing and relating. Culture shapes how personal understandings of health and illness are constructed and normalized by influencing health perceptions and health seeking practices.’ Moreover, considering culture as one element shaping health patterns in populations does not exclude considering how culture intersects with poverty, or other forms of social location in the US context. In fact, in recent years sociology scholars have questioned the lack of scholarship examining culture and how it operates across broader structural conditions.48 Thus, to build on the literature attempting to identify more specific constructs in acculturation research,49 we used commonly applied acculturation proxies to examine if these measures were associated with social norms and thereby suggest a link to a theoretically-based construct.
The three acculturation proxies examined included nativity status, generational status and language most often used. Participants were asked if they were born in the United States and classified as US-born or foreign-born (nativity status). They were also asked if their mother and father were born in the US in order to determine generational status. First generation individuals include those who were born outside of the US, second generation includes those born in the US of at least one foreign-born parent, and third generation includes those born in the US of US-born parents. The total number of individuals categorized as foreign-born and first-generation slightly differs because two individuals were born outside of the US but their parents were US-born. The language measure was based on language used most often and classified as only/mostly Spanish, Spanish and English about the same, and only/mostly English.
Because socioeconomic position is strongly associated with smoking status and has largely been neglected in acculturation research, we also examined if education, income and employment status were correlates of smoking social norms. Education was classified as less than high school, completed high school (12 years), some college, and college (bachelor’s) degree or higher. Household income was classified as ≤$24,999; $25,000 to $49,999; $50,000 to $74,999; and ≥$75,000. Approximately 17% of observations had missing data on income. We addressed this by creating a ‘missing’ category in the income variable. A sensitivity analysis excluding observations with missing income data yielded virtually identical estimates. As such, the income variable with the missing category was used in the final models in order to include as many of the observations as possible across all models. Employment status was classified according to standard employment categories and included employed for wages, unemployed (includes those looking for work), and other employment status (homemakers, students, retired and those unable to work).
Statistical analysis
The combined 2011 and2013 NYAHS sample included 873 Latino participants. Percent distributions and means were estimated for the total population with sampling weights applied to adjust for nonresponse and the varying probabilities of selection. Rao and Scott 2nd order corrected Chi-square test of independence, which converts the Pearson Chi-square to an F-statistic, were used to determine differences across categories of the acculturation proxies and social norms in categorical form. We subsequently classified the 3-level social norms measure into a binary measure (unacceptable vs. accept/do not care) in order to fit a logistic regression model to estimate age and sex-adjusted predicted probabilities of unacceptable social norms by acculturation and SEP measures. A p-value for trend was obtained by entering the acculturation proxies and SEP measures in ordinal fashion in regression models. We then fit a series of sequential logistic regression models (Table 3) examining the association between social norms (3 categories), acculturation proxies and current smoking status. The first model in our analysis (Model 1, Table 3) examines if social norms, generational status, and language preference are each independently (bivariate association) associated with current smoking status. Nativity status is not included in any of these models as it is embedded within the definition of generational status and because preliminary analyses indicated a high correlation between nativity and generational status (r=0.84). Models 2 includes our main predictor, social norms, and examines if associations with current smoking status remain after adjusting for age, gender, education, annual household income and employment status. Model 3 additionally adjusted for generational status, and model 4 includes all measures plus language most often spoken, which some research suggests captures cultural retention.43 Of note, although our primary interest in these models was to demonstrate the association between smoking social norms and current smoking status, we adjust for acculturation proxies in Models 3–4 to further corroborate if social norms remained independently associated with current smoking status after adjusting for acculturation proxies. We believe this is important to present since our study is one of the few in the literature to attempt to empirically test associations between acculturation proxies, normative beliefs, and smoking status. The number of records retained in these models can vary depending on the covariates included, but deleted observations did not exceed more than 5% across Models 1–5. Lastly, we estimated prevalence ratios as functions of average marginal predictions within a complex survey design setting50 from logistic regression models in an effort to reduce the potential of overestimating associations with odds ratios. All analyses were conducted with SAS-callable SUDAAN (SAS Institute, Cary, NC; Research Triangle Institute, Research Triangle Park, NC).
Table 3.
Bivariate and multivariate associations between smoking social norms, acculturation proxies, and current cigarette smoking among Latinos, National Young Adult Health Survey, 2011 and 2013.
| Model 1 (Bivariate Association) |
Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Social Norm | PR (CI) | PR (CI) | PR (CI) | PR (CI) |
| Do not accept | 0.44 (0.24, 0.82) |
0.48 (0.27, 0.87) |
0.61 (0.35,1.05) |
0.64 (0.38, 1.07) |
| Accept | 1.22 (0.80,1.85) |
1.32 (0.93, 1.89) |
1.41 (0.98,2.02) |
1.34 (0.93, 1.94) |
| Do not care either way | 1.0 | 1.0 | 1.0 | 1.0 |
| Generational status | ||||
| 1st generation | 0.28 (0.16,0.50) |
0.26 (0.15, 0.46) |
0.31 (0.16, 0.60) |
|
| 2nd generation | 0.65 (0.44,0.94) |
0.80 (0.58, 1.12) |
0.83 (0.58, 1.19) |
|
| 3rd generation | 1.0 | 1.0 | 1.0 | |
| Language spoken | ||||
| Only/ mostly Spanish | 0.14 (0.07,0.28) |
0.27 (0.10, 0.72) |
||
| English and Spanish about the same |
0.73 (0.48,1.11) |
1.03 (0.69, 1.55) |
||
| Only/ mostly English | 1.0 | 1.0 | ||
| Age, Mean (se) | 1.04 (0.98, 1.10) |
1.06 (1.00,1.13) |
1.07 (1.00, 1.14) |
|
| Gender | ||||
| Male | 1.52 (1.04, 2.21) |
1.63 (1.15, 2.31) |
1.51 (1.08, 2.10) |
|
| Female | 1.0 | 1.0 | 1.0 | |
| Education | ||||
| < High School | 2.51 (1.21, 5.21) |
3.34 (1.68, 6.64) |
4.22 (2.03, 8.75) |
|
| High School | 2.34 (1.15, 4.76) |
2.45 (1.24, 4.87) |
2.63 (1.25, 5.53) |
|
| Some college | 1.99 (1.00,3.96) |
2.06 (1.05, 4.03) |
2.30 (1.13, 4.70) |
|
| College graduate or more | 1.0 | 1.0 | 1.0 | |
| Annual household income, $ | ||||
| Missing | 1.17 (0.46, 2.97) |
1.22 (0.46, 3.25) |
0.92 (0.33, 2.56) |
|
| <$24,999 | 2.40 (1.12, 5.16) |
2.53 (1.19, 5.41) |
2.33 (1.10, 4.91) |
|
| $25,000–49,999 | 1.32 (0.58, 3.01) |
1.60 (0.72, 3.55) |
1.49 (0.68, 3.26) |
|
| $50,000–74,999 | 1.40 (0.55,3.54) |
1.25 (0.51, 3.07) |
1.08 (0.47, 2.49) |
|
| $75,000 or more | 1.0 | 1.0 | 1.0 | |
| Employment | ||||
| Unemployed | 0.73 (0.41, 1.30) |
0.69 (0.39, 1.21) |
0.71 (0.42, 1.22) |
|
| Other work status | 0.59 (0.37, 0.93) |
0.70 (0.44, 1.11) |
0.67 (0.42, 1.05) |
|
| Employed | 1.0 | 1.0 | 1.0 |
First generation includes individuals who were born outside of the US, 2nd generation includes those born in the US with at least one foreign-born parent, and 3rd generation includes those born in the US with US-born parents.
Results
The unweighted frequencies and weighted distributions of the study population are shown in Table 1. Participants were on average 25 years of age and 50.7% were female. Twenty-six percent of the young adults sampled had a high school education or less and nearly half earned less than $25,000 per year. While most participants were US-born (67.4%), half (51.6%) reported that they only/mostly spoke English. When asked about smoking norms, 25.6 % of participants reported that their Latino peers do not accept smoking, and an additional 51.3% reported that their Latino peers do not care either way if they smoke. Approximately one in four of the young adults sampled were current cigarette smokers (25.6%), and 68% had either not smoked 100+ cigarettes in their lifetime or never smoked at all.
Table 1.
Sample Characteristics and Weighted Distributions of Latino participants by Smoking Status: National Young Adult Health Survey, 2011 and 2013.
| Unweighted No. |
Total Mean (se) or % |
Smokers Mean (se) or % |
Non-Smokers Mean (se) or % |
|
|---|---|---|---|---|
| Age, Mean (se) | 873 | 25.4 (0.23) | 26.12 (0.48) | 25.20 (0.27) |
| Gender | ||||
| Female | 414 | 50.7 | 34.18 | 56.54 |
| Male | 459 | 49.3 | 65.82 | 43.46 |
| Education | ||||
| < High School | 115 | 26.0 | 33.65 | 23.43 |
| High School | 298 | 26.6 | 28.73 | 25.82 |
| Some college | 267 | 33.4 | 31.61 | 33.99 |
| College graduate or more | 172 | 14.0 | 6.0 | 1.91 |
|
Annual household income, $ |
||||
| <$24,999 | 377 | 50.6 | 72.06 | 56.90 |
| $25,000–49,999 | 183 | 16.9 | 14.88 | 22.22 |
| $50,000–74,999 | 76 | 7.8 | 9.44 | 9.37 |
| $75,000 or more | 83 | 7.7 | 3.61 | 11.52 |
| Missing | 154 | 17.0 | ||
| Employment* | ||||
| Unemployed | 106 | 11.93 | 8.89 | 12.94 |
| Other work status | 274 | 30.92 | 20.46 | 34.72 |
| Employed | 486 | 57.16 | 70.66 | 52.34 |
| Nativity | ||||
| Foreign-born | 255 | 32.6 | 16.41 | 38.22 |
| US-born | 599 | 67.4 | 83.59 | 61.78 |
| Language Use | ||||
| Only Spanish | 115 | 16.4 | 2.9 | 20.88 |
| English and Spanish about the same |
273 | 32.0 | 30.32 | 32.66 |
| Only English | 465 | 51.6 | 66.78 | 46.46 |
| Generational status** | ||||
| 1st generation (Foreign born of foreign-born parents) |
253 | 32.8 | 14.79 | 38.63 |
| 2nd generation (US-born with foreign-born parents) |
342 | 37.6 | 38.37 | 37.27 |
| 3rd generation (US-born with US-born parents) |
244 | 29.7 | 46.84 | 24.10 |
| Smoking social norms | ||||
| Do not accept | 160 | 25.6 | 12.48 | 29.97 |
| Accept | 181 | 23.1 | 30.92 | 20.46 |
| Do not care either way | 409 | 51.3 | 56.49 | 49.58 |
| Current Smoking Status | ||||
| Current Smoker | 179 | 25.6 | 25.6 | 0 |
| Former Smoker | 63 | 6.7 | 0 | 9.03 |
| Never Smoker | 625 | 67.7 | 0 | 90.97 |
| Frequency of Smoking | ||||
| Daily | 105 | 14.2 | 55.42 | 0.05 |
| Some Days | 102 | 13.8 | 44.58 | 3.09 |
| Not at all | 665 | 72.0 | 0 | 96.86 |
Includes homemakers, students, retired individuals and those unable to work.
First generation includes individuals who were born outside of the US, 2nd generation includes those born in the US with at least one foreign-born parent, and 3rd generation includes those born in the US with US-born parents.
The sample distribution by smoking status revealed that among current cigarette smokers men were more likely to smoke than women. Similarly, among smokers, the prevalence of smoking was highest among those with less than a high school degree, those reporting an annual household less than $25,000/ year, and those who were currently employed. The distribution of smoking status by acculturation status showed that among smokers the US-born, those who mostly/ only spoke English and third generation individuals had the highest prevalence of smoking. When asked about frequency of smoking (for all respondents), 55.4% of current smokers reported smoking on a daily basis and 44.6% smoked on some days.
Correlates of Social Norms
Bivariate analysis of demographic characteristics, SEP measures and all three acculturation proxies with smoking social norms are presented in Table 2. A larger percentage of women reported that their Latina peers find smoking unacceptable compared to men’s smoking social norms (33.1% vs. 17.7%, p<0.01). There was no consistent pattern for social norms less accepting of smoking by educational attainment. While those with the lowest levels of education tended to report that Latino peers find smoking unacceptable, there was no significant difference across categories of education (p=0.21). Gradients in income were more discernible, with no acceptance of smoking highest in the lowest income group (31%) dropping in the two middle income groups and then peaking again in the highest income group (29%) (p<0.05). Lastly, there was no discernible or significant pattern of social norms by employment status (p=0.21).
Table 2.
Correlates of smoking social norms among Latinos, National Young Adult Health Survey, 2012
| Acculturation Proxy | Smoking Social Norm | |||
|---|---|---|---|---|
| Do Not Accept | Accept | Do Not Care | P-value | |
| Age, Mean (SE) | 25.9 | 25.7 | 25.4 | 0.68 |
| Gender | <0.01 | |||
| Female | 33.09 | 17.96 | 48.95 | |
| Male | 17.68 | 28.49 | 53.89 | |
| Education | 0.10 | |||
| < High School | 38.2 | 16.5 | 45.2 | |
| High School | 20.41 | 20.68 | 58.91 | |
| Some college | 20.93 | 27.68 | 51.40 | |
| College graduate or more |
25.68 | 28.54 | 45.78 | |
|
Annual household income, $ |
<0.01 | |||
| <$24,999 | 31.06 | 17.26 | 51.68 | |
| $25,000–49,999 | 14.67 | 28.54 | 56.79 | |
| $50,000–74,999 | 13.85 | 27.30 | 58.85 | |
| $75,000 or more | 29.35 | 39.21 | 31.44 | |
| Employment* | 0.25 | |||
| Unemployed | 28.98 | 14.38 | 56.64 | |
| Other work status | 30.10 | 23.13 | 46.77 | |
| Employed | 21.86 | 25.20 | 52.94 | |
| Nativity Status | <0.01 | |||
| Foreign-born | 35.25 | 28.16 | 36.59 | |
| US-born | 20.93 | 20.67 | 58.40 | |
| Language Use | 0.05 | |||
| Only/ mostly Spanish | 39.39 | 22.01 | 38.60 | |
| Spanish and English About the Same |
29.45 | 17.86 | 52.69 | |
| Only/ mostly English | 19.65 | 26.36 | 53.98 | |
| Generational Status** | <0.01 | |||
| 1st Generation | 36.14 | 26.34 | 37.52 | |
| 2nd Generation | 23.57 | 22.50 | 53.92 | |
| 3rd Generation | 17.27 | 16.54 | 66.19 | |
Includes homemakers, students, retired individuals and those unable to work.
First generation includes individuals who were born outside of the US, 2nd generation includes those born in the US with at least one foreign-born parent, and 3rd generation includes those born in the US with US-born parents.
The clearest gradients in smoking social norms were observed for the three acculturation proxies. The foreign-born in general, those who only/ mostly spoke Spanish and 1st generation Latinos had significantly less acceptable social norms regarding smoking (F-test p<0.01 for all three associations) than their peers who were US-born, spoke only/ mostly English or were 3rd generation.
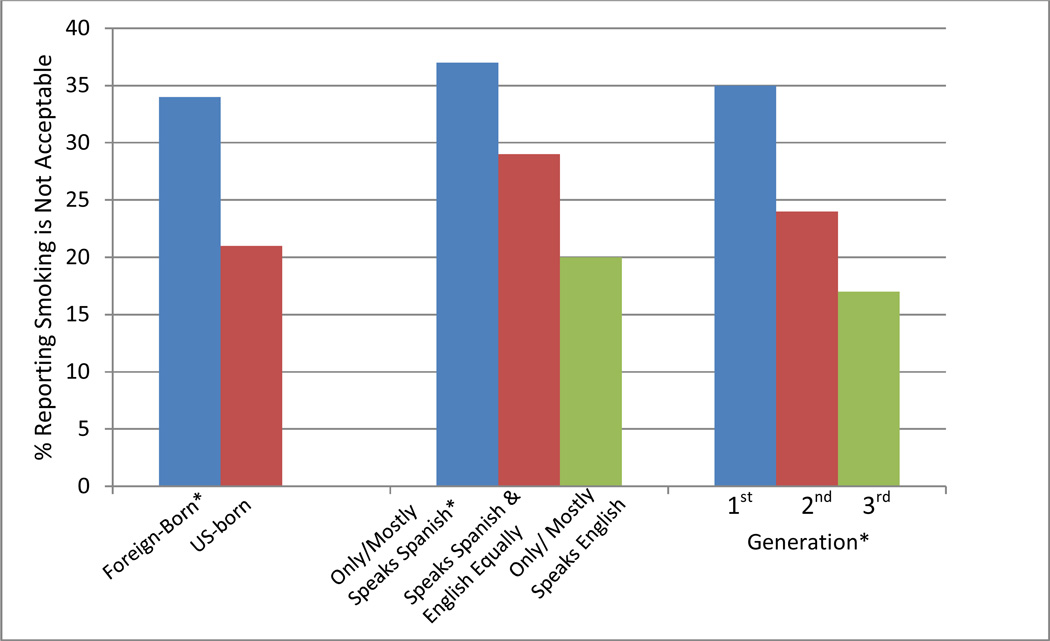
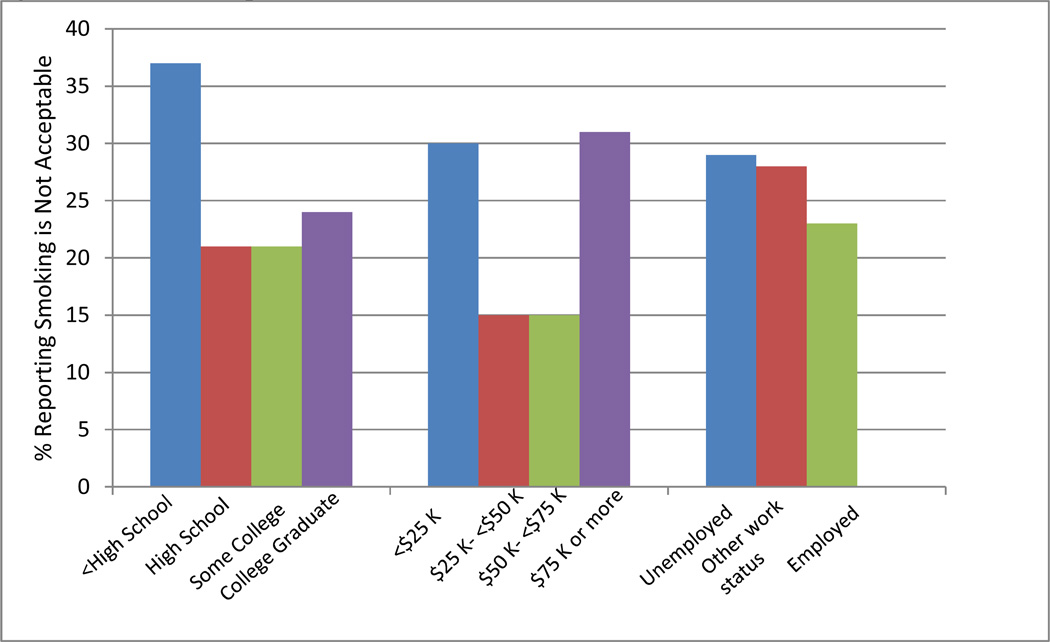
Age and sex-adjusted probabilities of social norms
Figures 1 and 2 present age and sex-adjusted predicted probabilities of having co-ethnic peers who do not accept smoking by acculturation proxies and SEP measures. The bivariate associations observed in Table 2 in the age and sex-adjusted models. Foreign-born individuals reported less acceptance of smoking among their co-ethnic peers (p<0.05). For language most often used and generational status, there was a graded decrease in acceptance of those who only/mostly spoke Spanish and first generation immigrants (p for trend <0.05 for all measures). The income, education, and employment variables showed no clear and significant gradients in smoking social norms (p for trend >0.05).
Figure 1. Age and sex-adjusted probability of not accepting smoking among Latinos by acculturation proxies, NYAHS 2011 and 2013.*.
Note: Predicted probabilities modeled from logistic regression models adjusted for age and sex. *F-test p-value <0.05 for nativity status and p-for trend <0.05 for language use and generation.
Figure 2. Age and sex-adjusted probability of not accepting smoking among Latinos by socioeconomic position, NYAHS 2011 and 2013.
Note: Predicted probabilities modeled from logistic regression models adjusted for age and sex. *p-for trend >0.05 for all measures.
Social norms and current smoking status
Table 3 presents results from models examining the association between smoking social norms, acculturation proxies and current smoking status. The first model demonstrates that Latinos with injunctive norms less accepting of smoking were significantly less likely to be current smokers when compared to those who report that Latino peers do not care if a person smokes (PR=0.44, CI=0.24, 0.82). Conversely, the probability of smoking was 22% higher among Latinos who report that smoking is acceptable among their peers, when compared to those who say their peers do not care either way but results were non-significant (PR=1.22, CI=0.80, 1.85). Additionally, both generational status and language most often spoken were each independently associated with current smoking status. First- generation Latinos were significantly less likely to smoke than third-generation Latinos (PR=0.28, CI=0.16, 0.50) and those who spoke mostly Spanish also had a lower probability of smoking than those who mostly spoke English (PR=0.14, CI=0.07,0.28).
Building on our predictor of interest, Models 2 examines if social norms remains associated with current smoking status after adjusting for demographic, socioeconomic and acculturation factors. Model 2 shows that estimates remain virtually unchanged for respondents with smoking norms not accepting of smoking (Model 3, PR= 0.48, CI=0.27, 0.87) and among those who say peers accept smoking (Model 3, PR=1.30, CI=0.93, 1.89), after adjusting for age, sex, education, and income.
In Models 3 and 4 we included generational status and language spoken most often to determine if these acculturation proxies further explained associations observed between smoking social norms and current smoking status. The inclusion of these variables reduced the estimated parameters, and in some instances estimates became statistically non-significant or marginally significant. For example, after adjusting for generational status, the probability of being a current smoker in Model 3 was 40% lower among those with social norms less acceptable of smoking compared to 56% lower in Model 2. In our final model (Model 4), we additionally adjusted for language spoken most often to determine if language may be an additional measure of cultural retention. Results continued to show a reduced probability of smoking for respondents with social norms less acceptable of smoking compared to those who report that Latino peers are ambivalent about smoking, although results were no longer significant (PR=0.64, CI=0.38, 1.08). Moreover, those reporting that co-ethnic Latino peers were accepting of smoking continued to be more likely to smoke (PR=1.38, CI=0.95, 2.01). Generational status and language spoken also revealed strong associations with current smoking status. First generation individuals and those who mostly/ only spoke Spanish remained significantly less likely to be current smokers than their third generation counterparts and those who mostly/ only English (PR=0.31, CI=0.16, 0.60 and PR=0.27, CI=0.10, 0.72, respectively). While those in the second generation and who spoke English and Spanish equally were also less likely to smoke, the estimates did not reach statistical significance.
Discussion
Using a novel sampling design to reach the young adult population, our study adds key information to the scarce body of literature examining the factors that potentially contribute to smoking norms and how smoking social norms relate to smoking in young adults. We examined the extent to which acculturation proxies were associated with social norms in bivariate and age-sex adjusted models and showed that injunctive norms less accepting of smoking were higher among the foreign-born, first generation immigrants and those who spoke mostly/only Spanish young Latino adults. However, the patterning of social norms by socioeconomic position was not evident. Finally, we examined if smoking social norms was associated with smoking status and found that young adults who report that co-ethnic Latino peers are less accepting of smoking were significantly less likely to be current smokers after adjusting for demographic, socioeconomic and acculturation proxies.
The study of social norms in shaping smoking behaviors remains relatively scant,51 although several tobacco control initiatives have developed messages intended to change group norms related to smoking (e.g., the anti-tobacco “truth” campaign).52 Research on this topic has been largely focused on adolescents and no study of which we are aware has involved racially/ ethnically diverse young adult populations. In a meta-analysis conducted by Freedman et al.,53 the authors showed that the majority of studies conducted on young adults have focused on those enrolled in college and those in military service, which is a limited segment of the young adult population. Our study found an overall smoking prevalence of 25.6%, which is higher than estimates obtained through other national surveys (e.g., the Behavioral Risk Factor Surveillance System or the National Health Interview Survey) but is in line with some of our prior work suggesting that estimates may differ due to a range of methodological issues, including not adequately reaching young adults due to the use of landline sampling techniques.38,39 Further, aside from the population reached, smoking social norms remain important to study even under today’s more regulated climate. As an example, while the causal role of any single policy change in decreasing smoking prevalence has not been conclusively demonstrated, it is clear that the combined effect of the public’s awareness of the dangers of smoking, removal of cigarette advertising from television and billboards, state tobacco control funding , smoking bans in public places and increased sales taxation of cigarettes all played crucial roles in changing norms regarding the acceptability of smoking and ultimately smoking behaviors,54–56 despite the fact that these initiatives were initially met with great resistance by the general public.51,57
Our study showed consistent associations between smoking norms specific to Latino populations and current smoking status, suggesting the need for future research to replicate these findings and corroborate whether this association systematically differs according to nativity status, length of residence in the US, and language spoken. As the nation’s largest and fastest growing racial/ ethnic minority group, it is imperative to determine smoking norms among Latinos that may influence the success of public health smoking prevention efforts. In one of the few studies to examine norms regarding smoking bans among immigrants, Osypuk et al.58 found that immigrants overall, including immigrants of Latin American origin, were more accepting of smoking bans than their US-born counterparts. The authors also showed that support for smoking bans decreased across generation, with higher support observed among first generation immigrants (i.e., foreign-born) than in third generation immigrants (US-born of US-born parents). Our findings corroborate this study for a young adult population and support the notion that individuals who perceive that their co-ethnic peers have less acceptable views of smoking are less likely to be current smokers. Moreover, the study of social norms also has implications for influencing behaviors outside of socially defined groups. For example, social network theory suggests that addressing group-level dynamics can have a cascading effect even to individuals outside of defined groups or networks.59 Thus, in terms of policy and public health implications, an intervention targeted at select groups of the population found to have more health-enhancing smoking norms could create the conditions for the prevention or cessation of smoking in the population at large.
An additional goal of our study was to determine if injunctive norms specific to Latino young adults may serve as a potential mechanism underlying previously reported acculturation-health associations. We found that each of the acculturation proxies examined- nativity, generational status, and language use- was consistently associated with smoking norms and current smoking status. Nonetheless, our data did not allow us to conduct formal tests of mediation (direct and indirect effects) given recent methodological work that suggests that quantifying the extent of mediation is often violated in practice. Specifically, mediation tests require strong assumptions of no unmeasured confounding between the exposure and mediator or mediator and outcome, and no interaction between the effects of the exposure and the mediator on the outcome,60–62 which we were not able to adequately test in this cross-sectional study. Nevertheless, the present analysis is one of the few studies to examine the association between social norms and an important health behavior in young adults. Future research would be strengthened by examining if measures not available in our study (e.g., neighborhood or work-based contexts regarding smoking) confound potential mediation analyses, or our observed association more generally. Our hypothesis of a gradient effect on smoking social norms by education, income and employment was not supported. One explanation for this finding may be the fact that our study population is young (18–34 years of age) and hence still transitioning across socioeconomic position, leading to inconsistent and non-significant gradients. Additionally, at least for our employment measure, we were not able to capture the full range of work experiences that may be meaningful for smoking behaviors in this population (e.g., polices surrounding smoking at place of employment, full or part-time work status, and length of unemployment).
It is worth noting that the main findings in our study do not suggest a pan-ethnic and homogeneous set of shared norms specific to Latinos.13 The extent to which injunctive norms regarding smoking vary across racial/ ethnic groups remains to be established. Rather, an implication of our findings is that cultural processes may explain some variation in health and should be considered in understanding the production of health inequalities and the process individuals undertake to make meaning of their world and the extent to which this cultural process of meaning-making is shaped by broader socioeconomic conditions.48,63 This area of research also opens opportunities to shift our conceptual framework from one that only considers the health deficits operating in marginalized and socioeconomically disadvantaged populations, to a perspective that recognizes and harnesses the positive attributes disenfranchised communities possess to ensure that proposed health interventions are culturally meaningful, respectful and sustainable.64
Several limitations warrant attention in our study. The cross-sectional nature of the study limits causal inferences regarding the extent to which social norms directly influence the adoption of smoking, and conversely, whether current smoking status influences report of acceptability of smoking among co-ethnic peers. Longitudinal studies are best suited to answer questions of temporality, but other large-scale studies have suggested that social norms can be one mechanism influencing the adoption of smoking over time.24 Our question on social norms did not distinguish if norms were perceived differently according to specific groups, such as family members, friends and peers, both internal and external to a person’s ethnic group of origin. Individuals are involved in multiple social groups and each group may pattern smoking behaviors in different ways. While we included a new measure of social norms specific to Latinos, we were limited by time constraints and survey costs and hence only included a single item on smoking social norms. While a modified version of this measure has been used in prior work,25 the validity of this construct would be greatly enhanced with the use of a multi-item scale. Another limitation is that while results are based on a representative sample of young Latino adults in the United States we were not able to conduct analyses by specific groups of Latinos due to sample size limitations. Latinos are a heterogeneous population with varying demographic, social and political backgrounds, all of which can shape health in different ways. Thus, we caution that results may not be generalizable to specific groups of Latinos. Lastly, we were not able to examine if social norms vary by broader social contexts such as the person’s neighborhood of residence or state-level policies that may create distinct environments that may either promote or place constraints on smoking behaviors.
Overall, this study advances our understanding of potential pathways involved in smoking status among young Latino adults. Findings provide insights into the patterning of smoking norms by commonly used acculturation proxies such as nativity status, length of stay in the US, and generational status. For each of these measures, acceptable views of smoking increased with longer duration in the US and across generations, supporting prior evidence that health-enhancing attributes diminish over time. Results lend support to the notion that social norms among Latino populations are important to consider in public health interventions.
Research Highlights.
We examined how social norms pattern smoking status among young Latino adults.
Individuals were less likely to smoke if co-ethnic peers did not accept smoking.
We observed smoking norms gradients by language, nativity and generational status.
Smoking norms were not associated with socioeconomic position.
Smoking norms may represent cultural processes patterning smoking behaviors.
Acknowledgements
This study was supported by a grant from the National Institutes of Health (R01CA149705).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Daniel A. Gundersen, Email: gunderda@rwjms.rutgers.edu.
Michelle T.B. Manderski, Email: bovermi@sph.rutgers.edu.
Cristine D. Delnevo, Email: delnevo@sph.rutgers.edu.
REFERENCES
- 1.Centers for Disease Control and Prevention. Current Cigarette Smoking Among Adults — United States, 2005–2012. MMWR. 2014;63(02):29–34. [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 50th Anniversary of the First Surgeon General’s Report on Smoking and Health. MMWR. 2014;63(02):29–29. [Google Scholar]
- 3.King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. American journal of public health. 2012 Nov;102(11):e93–e100. doi: 10.2105/AJPH.2012.301002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Center for Health Statistics. Hayattsville, MD: Department Health Human Services; Available at http://www.cdc.gov/nchs/datawh/statab/unpubd/mortabs.htm. [Google Scholar]
- 5.Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. American journal of preventive medicine. 2005 Aug;29(2):143–148. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Castro Y, Reitzel LR, Businelle MS, et al. Acculturation differentially predicts smoking cessation among Latino men and women. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2009 Dec;18(12):3468–3475. doi: 10.1158/1055-9965.EPI-09-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perez-Stable EJ, Ramirez A, Villareal R, et al. Cigarette smoking behavior among US Latino men and women from different countries of origin. American journal of public health. 2001 Sep;91(9):1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Cancer Society. Cancer Facts & Figures for Hispancis/Latinos 2012–2014. Atlanta: American Cancer Society; 2012. [Google Scholar]
- 9.Berry JW. A psychology of immigration. Journal of Social Issues. 2001;57:615–631. [Google Scholar]
- 10.Gundersen DA, Echeverria SE, Lewis MJ, Giovino GA, Ohman-Strickland P, Delnevo CD. Heterogeneity in past year cigarette smoking quit attempts among Latinos. Journal of environmental and public health. 2012;2012:378165. doi: 10.1155/2012/378165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Broesch J, Hadley C. Putting culture back into acculturation: Identifying and overcoming gaps in the definition and measurement of acculturation. The Social Science Journal. 2012;49(3):375–385. [Google Scholar]
- 12.Carter-Pokras O, Bethune L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. A commentary on Thomson and Hoffman-Goetz. Social science & medicine (1982) 2009 Oct;69(7):992–995. doi: 10.1016/j.socscimed.2009.06.042. discussion 999–1001. [DOI] [PubMed] [Google Scholar]
- 13.Zambrana RE, Carter-Pokras O. Role of acculturation research in advancing science and practice in reducing health care disparities among Latinos. American journal of public health. 2010 Jan;100(1):18–23. doi: 10.2105/AJPH.2008.138826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hunt LM, Schneider S, Comer B. Should "acculturation" be a variable in health research? A critical review of research on US Hispanics. Social science & medicine (1982) 2004 Sep;59(5):973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Social science & medicine (1982) 2007 Oct;65(7):1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Carter-Pokras OD, Feldman RH, Kanamori M, et al. Barriers and facilitators to smoking cessation among Latino adults. Journal of the National Medical Association. 2011 May;103(5):423–431. doi: 10.1016/s0027-9684(15)30339-4. [DOI] [PubMed] [Google Scholar]
- 17.Echeverria SE, Pentakota SR, Abraido-Lanza AF, et al. Clashing paradigms: an empirical examination of cultural proxies and socioeconomic condition shaping Latino health. Annals of epidemiology. 2013 Oct;23(10):608–613. doi: 10.1016/j.annepidem.2013.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abraido-Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. American journal of public health. 2006 Aug;96(8):1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cialdini RB, Kallgren CA, Reno RR. A focus theory of normative conduct. Advances in Experimental Social Psychology. 1991;24:201–234. [Google Scholar]
- 20.Fishbein M, Ajzen I. Belief, attitude, intention and behavior: An introduction to theory and research. MA: Addison-Wesley; 1975. [Google Scholar]
- 21.Lapinski MK, Rimal RN. An explication of social norms. Communication Theory. 2005;15:127–147. [Google Scholar]
- 22.Phua JJ. The reference group perspective for smoking cessation: an examination of the influence of social norms and social identification with reference groups on smoking cessation self-efficacy. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2013 Mar;27(1):102–112. doi: 10.1037/a0029130. [DOI] [PubMed] [Google Scholar]
- 23.Thoits PA. Mechanisms linking social ties and support to physical and mental health. Journal of health and social behavior. 2011 Jun;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- 24.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. The New England journal of medicine. 2008 May 22;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karasek D, Ahern J, Galea S. Social norms, collective efficacy, and smoking cessation in urban neighborhoods. American journal of public health. 2012 Feb;102(2):343–351. doi: 10.2105/AJPH.2011.300364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Social science & medicine (1982) 2008 Aug;67(3):420–430. doi: 10.1016/j.socscimed.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iwelunmor J, Newsome V, Airhihenbuwa CO. Framing the impact of culture on health: a systematic review of the PEN-3 cultural model and its application in public health research and interventions. Ethnicity & health. 2014 Feb;19(1):20–46. doi: 10.1080/13557858.2013.857768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Livingood WC, Allegrante JP, Airhihenbuwa CO, et al. Applied social and behavioral science to address complex health problems. American journal of preventive medicine. 2011 Nov;41(5):525–531. doi: 10.1016/j.amepre.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 29.Unger JB, Schwartz SJ. Conceptual considerations in studies of cultural influences on health behaviors. Preventive medicine. 2012 Nov;55(5):353–355. doi: 10.1016/j.ypmed.2012.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.U.S. Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [PubMed] [Google Scholar]
- 31.Lariscy JT, Hummer RA, Rath JM, Villanti AC, Hayward MD, Vallone DM. Race/Ethnicity, nativity, and tobacco use among US young adults: results from a nationally representative survey. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2013 Aug;15(8):1417–1426. doi: 10.1093/ntr/nts344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Graham JW, Marks G, Hansen WB. Social influence processes affecting adolescent substance use. The Journal of applied psychology. 1991 Apr;76(2):291–298. doi: 10.1037/0021-9010.76.2.291. [DOI] [PubMed] [Google Scholar]
- 33.Hansen WB, Graham JW. Preventing alcohol, marijuana, and cigarette use among adolescents: peer pressure resistance training versus establishing conservative norms. Preventive medicine. 1991 May;20(3):414–430. doi: 10.1016/0091-7435(91)90039-7. [DOI] [PubMed] [Google Scholar]
- 34.Eisenberg ME, Forster JL. Adolescent smoking behavior: measures of social norms. American journal of preventive medicine. 2003 Aug;25(2):122–128. doi: 10.1016/s0749-3797(03)00116-8. [DOI] [PubMed] [Google Scholar]
- 35.Chen PH, White HR, Pandina RJ. Predictors of smoking cessation from adolescence into young adulthood. Addictive behaviors. 2001 Jul-Aug;26(4):517–529. doi: 10.1016/s0306-4603(00)00142-8. [DOI] [PubMed] [Google Scholar]
- 36.Weiss JW, Garbanati JA. Effects of acculturation and social norms on adolescent smoking among Asian-American subgroups. Journal of ethnicity in substance abuse. 2006;5(2):75–90. doi: 10.1300/J233v05n02_05. [DOI] [PubMed] [Google Scholar]
- 37.Kumar R, O’Malley PM, Johnston LD, Schulenberg JE, Bachman JG. Effects of School-Level Norms on Student Substance Use. Prevention Science. 2002;3(2):105–124. doi: 10.1023/a:1015431300471. [DOI] [PubMed] [Google Scholar]
- 38.Gundersen DA, ZuWallack RS, Dayton J, Echeverria SE, Delnevo CD. Assessing the feasibility and sample quality of a national random-digit dialing cellular phone survey of young adults. American journal of epidemiology. 2014 Jan 1;179(1):39–47. doi: 10.1093/aje/kwt226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Delnevo CD, Gundersen DA, Hagman BT. Declining estimated prevalence of alcohol drinking and smoking among young adults nationally: artifacts of sample undercoverage? American journal of epidemiology. 2008 Jan 1;167(1):15–19. doi: 10.1093/aje/kwm313. [DOI] [PubMed] [Google Scholar]
- 40.Blumberg SJ, Luke JV, Ganesh N, Davern ME, Boudreaux MH. Wireless substitution: state-level estimates from the National Health Interview Survey, 2010–2011. National health statistics reports. 2012 Oct 12;(61):1–15. [PubMed] [Google Scholar]
- 41.US Census Bureau. American Community Survey 1-year estimates B14004. Washington, DC: US Census Bureau; 2012. [Accessed July 2014]. College or graduate school enrollment by type of school by age for the population 18–24 years of age. ( http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_1YR_S1401&prodType=table). [Google Scholar]
- 42.Pew Research Center Internet and American Life Project. April 2012 mobile crosstab file. Washington, DC: Pew Internet and American Life Project; 2012. [(Accessed May 2, 2013)]. Spring tracking survey 2012. ( http://pewinternet.org/Shared-Content/Data-Sets/2012/April-2012-Cell-Phones.aspx). [Google Scholar]
- 43.Almeida J, Molnar BE, Kawachi I, Subramanian SV. Ethnicity and nativity status as determinants of perceived social support: testing the concept of familism. Social science & medicine (1982) 2009 May;68(10):1852–1858. doi: 10.1016/j.socscimed.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 44.Viruell-Fuentes EA, Morenoff JD, Williams DR, House JS. Contextualizing nativity status, Latino social ties, and ethnic enclaves: an examination of the ‘immigrant social ties hypothesis’. Ethnicity & health. 2013;18(6):586–609. doi: 10.1080/13557858.2013.814763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abraido-Lanza AE, Viladrich A, Florez KR, Cespedes A, Aguirre AN, De La Cruz AA. Commentary: fatalismo reconsidered: a cautionary note for health-related research and practice with Latino populations. Ethnicity & disease. 2007 Winter;17(1):153–158. [PMC free article] [PubMed] [Google Scholar]
- 46.Florez KR, Aguirre AN, Viladrich A, Cespedes A, De La Cruz AA, Abraido-Lanza AF. Fatalism or destiny? A qualitative study and interpretative framework on Dominican women's breast cancer beliefs. Journal of immigrant and minority health / Center for Minority Public Health. 2009 Aug;11(4):291–301. doi: 10.1007/s10903-008-9118-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cook B, Alegria M, Lin JY, Guo J. Pathways and correlates connecting Latinos' mental health with exposure to the United States. American journal of public health. 2009 Dec;99(12):2247–2254. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Small ML, Harding DJ, Lamont ME. Reconsidering culture and poverty. Ann Am Acad Political Soc Sci. 2010;629:6–27. [Google Scholar]
- 49.Alegria M. The challenge of acculturation measures: what are we missing? A commentary on Thomson & Hoffman-Goetz. Social science & medicine (1982) 2009 Oct;69(7):996–998. doi: 10.1016/j.socscimed.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. American journal of epidemiology. 2010 Mar 1;171(5):618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 51.Gutman M. [Accessed on December 2013];Social Norms and Attitudes About Smoking 1991–2010. A companion report to The Tobacco Campaigns of the Robert Wood Johnson Foundation and Collaborators, 1991 – 2010. 2011 at http://www.rwjf.org/en/research-publications/find-rwjf-research/2011/04/the-tobacco-campaigns-/social-norms-and-attitudes-about-smoking.html.
- 52.Farrelly MC, Davis KC, Haviland ML, Messeri P, Healton CG. Evidence of a dose-response relationship between "truth" antismoking ads and youth smoking prevalence. American journal of public health. 2005 Mar;95(3):425–431. doi: 10.2105/AJPH.2004.049692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Freedman KS, Nelson NM, Feldman LL. Smoking initiation among young adults in the United States and Canada, 1998–2010: a systematic review. Preventing chronic disease. 2012;9:E05. [PMC free article] [PubMed] [Google Scholar]
- 54.Tauras JA, Chaloupka FJ, Farrelly MC, et al. State tobacco control spending and youth smoking. American journal of public health. 2005 Feb;95(2):338–344. doi: 10.2105/AJPH.2004.039727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pierce JP, Leon M. Effectiveness of smoke-free policies. The lancet oncology. 2008 Jul;9(7):614–615. doi: 10.1016/s1470-2045(08)70167-0. [DOI] [PubMed] [Google Scholar]
- 56.Albers AB, Siegel M, Cheng DM, Biener L, Rigotti NA. Relation between local restaurant smoking regulations and attitudes towards the prevalence and social acceptability of smoking: a study of youths and adults who eat out predominantly at restaurants in their town. Tobacco control. 2004 Dec;13(4):347–355. doi: 10.1136/tc.2003.007336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Walsh D. Development of Prevention Policy. Health Affairs. 1981;16(1):161–172. [Google Scholar]
- 58.Osypuk TL, Acevedo-Garcia D. Support for smoke-free policies: a nationwide analysis of immigrants, US-born, and other demographic groups, 1995–2002. American journal of public health. 2010 Jan;100(1):171–181. doi: 10.2105/AJPH.2009.160218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Christakis NA, Fowler JH. Social contagion theory: examining dynamic social networks and human behavior. Statistics in medicine. 2013 Feb 20;32(4):556–577. doi: 10.1002/sim.5408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hafeman DM. "Proportion explained": a causal interpretation for standard measures of indirect effect? American journal of epidemiology. 2009 Dec 1;170(11):1443–1448. doi: 10.1093/aje/kwp283. [DOI] [PubMed] [Google Scholar]
- 61.Kaufman JS, Maclehose RF, Kaufman S. A further critique of the analytic strategy of adjusting for covariates to identify biologic mediation. Epidemiologic perspectives & innovations : EP+I. 2004 Oct 8;1(1):4. doi: 10.1186/1742-5573-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.VanderWeele TJ. Invited commentary: structural equation models and epidemiologic analysis. American journal of epidemiology. 2012 Oct 1;176(7):608–612. doi: 10.1093/aje/kws213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kagawa Singer M. Applying the concept of culture to reduce health disparities through health behavior research. Preventive medicine. 2012 Nov;55(5):356–361. doi: 10.1016/j.ypmed.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 64.Airhihenbuwa CO, Ford CL, Iwelunmor JI. Why culture matters in health interventions: lessons from HIV/AIDS stigma and NCDs. Health education & behavior : the official publication of the Society for Public Health Education. 2014 Feb;41(1):78–84. doi: 10.1177/1090198113487199. [DOI] [PubMed] [Google Scholar]