Abstract
Background
Over the years several methods have been developed to reliably quantify functional capacity in patients with heart failure. Few studies have investigated the prognostic value of these assessment tools beyond cardio-renal prognostic biomarkers in stable patients with chronic heart failure.
Methods and Results
We performed Duke Activity Status Index (DASI, a self assessment tool comprised of 12 questions for estimating functional capacity) questionnaire in 1,700 stable, non-acute coronary syndrome patients with history of heart failure who underwent elective diagnostic coronary angiography with 5-year follow-up of all-cause mortality. In a subset of patients (n=800), B-type natriuretic peptide (BNP) was measured. In our study cohort, the median DASI score was 26.2 (IQR 15.5–42.7). Low DASI score provided independent prediction of a 3.3-fold increase in 5-year mortality risk (Quartile 1 versus 4: Hazard ratio [95% confidence interval] 3.33 [2.57–4.36], p<0.0001). After adjusting for traditional risk factors, BNP, and estimated glomerular filtration rate, low DASI score still conferred a 2.6-fold increase in mortality risk (2.57 [1.64–4.15], p<0.0001).
Conclusion
A simple self-assessment tool of functional capacity provides independent and incremental prognostic value for mortality prediction in stable patients with chronic heart failure beyond cardio-renal biomarkers.
Keywords: chronic heart failure, functional status, prognosis, heart failure, and functional capacity
INTRODUCTION
There are nearly 6 million adults in the United States carrying a diagnosis of heart failure (HF), with the lifetime risk estimated to be 1 in 5.(1) Although current medical and device therapies for HF have dramatically improved outcomes, HF mortality remains high in some subgroups.(2) Therefore, identifying poor prognostic markers early may provide opportunities for intensifying therapy. High natriuretic peptides,(3) cardiac troponin elevation,(4) and poor performance on exercise stress testing identify heart failure cohorts at increased risk for death over time. Functional status impairment can occur in the setting of chronically impaired cardiac output and chronic central or peripheral venous congestion.
The Duke Activity Status Index (DASI) is a simple 12 question self-assessment tool for estimating functional capacity (Table 1). DASI scores correlate well with peak oxygen uptake (Spearman rho=0.81, p<.0001) and are validated (Spearman rho=0.58, p<.0001) measures of functional status in patients with HF.(5) After admission for acute decompensated HF, DASI scores predict event-free survival.(6) However, the long-term prognosis of functional status measures in stable patients with HF has not been elucidated. In this study, we will determine the long-term prognostic value of functional status assessment in stable patients with chronic HF.
Table 1.
Duke Activity Status Index (DASI)
| Can you: | Weight |
|---|---|
| Take care of yourself, that is, eat, dress, bathe or use the toilet? | 2.75 |
| Walk indoors, such as around your house? | 1.75 |
| Walk a block or two on level ground? | 2.75 |
| Climb a flight of stairs or walk up a hill? | 5.50 |
| Run a short distance? | 8.00 |
| Do light work around the house like dusting or washing dishes? | 2.70 |
| Do moderate work around the house like vacuuming, sweeping floors or carrying groceries? | 3.50 |
| Do heavy work around the house like scrubbing floors or lifting or moving heavy furniture? | 8.00 |
| Do garden work like raking leaves, weeding or pushing a lawn mower? | 4.50 |
| Have sexual relations? | 5.25 |
| Participate in moderate recreational activites like golf, bowling, dancing, doubles tennis or throwing a ball? | 6.00 |
| Participate in strenuous sports like swimming, singles tennis, football, basketball or skiing? | 7.50 |
| Range 0 (worst) – 58.2 (best) | |
METHODS
Study Population
The Cleveland Clinic GeneBank study prospectively enrolled a total of 8,987 subjects who underwent coronary angiography in the absence of an acute coronary syndrome, without a history of revascularization within 30 days prior to enrollment, and at least 5 years of long-term adjudicated follow-up data. Detailed medical histories were obtained on all subjects (predominantly outpatients) at enrollment. Blood samples were collected at the time of cardiac catheterization after arterial sheath placement, but prior to the catheterization procedure or any therapy (including anticoagulation medications). All participants gave written informed consent approved by the Institutional Review Board.
Data Collected
The present analysis included 1,700 of consecutive subjects with a medical history of HF with reduced or preserved left ventricular ejection fraction (LVEF) enrolled in GeneBank, who completed the DASI questionnaire (Table 1) and with corresponding blood samples for analysis. Chronic heart failure was defined as a documented history of heart failure by treating physician in the electronic medical record and confirmed by study personnel at the time of enrollment. Heart failure was defined as a documented history of heart failure by the treating cardiologist in the electronic medical record at the time of enrollment.
Biomarkers and Echocardiography
B-type natriuretic peptide (BNP), creatinine, fasting lipid profiles, cardiac troponin I (TnI), and uric acid, and high sensitivity C-reactive protein (hs-CRP) were measured on the Abbot Architect platform (Abbott Laboratories, Abbot Park, Ill). An estimate of glomerular filtration rate (eGFR) was calculated via the Modification of Diet in Renal Disease equation. Left ventricular ejection fraction was determined via transthoracic echocardiography by the Cleveland Clinic echocardiography laboratory reviewed by Board-certified cardiologists via chart review of the electronic medical record. Adjudicated outcomes were prospectively ascertained over the ensuing 5 years for all subjects after enrollment.
DASI Questionnaire
Patients were asked to complete the DASI survey, supervised by study personnel, at the time of coronary angiography. The DASI was a self-administered questionnaire that measured both functional capacity and quality of life aspects. This correlated well with peak oxygen uptake on stress testing.(5) This survey attempted to capture major aspects of physical function: personal hygiene, ambulation, routine tasks, recreation, and sexual function. High scores correlated with better functional capacity. This questionnaire has been validated in similar populations.(7–8)
Statistical Analysis
This cohort was split into quartiles of DASI score for the population. P-values of ≤ 0.05 were considered significant to reject the null hypothesis that there were no differences in mortality at 5 years of follow-up between the highest and lowest DASI score quartiles. Independent variables were DASI score quartile and dependent variables were mortality at 5 years. Parametric and non-parametric approaches were used to express continuous variables. Survival analyses were completed via the Kaplan-Meier method and log-rank analysis to compare survival curves among the four quartiles. Cox proportional hazards models were used to compare time-to-event analysis to determine hazard ratios and 95% confidence intervals for 5-year mortality between the first and fourth quartiles of DASI scores. Multivariate models adjusted for traditional cardiac risk factors including, age, sex, systolic blood pressure, cigarette smoking, history of diabetes, and fasting low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol levels. Additional adjustments were made for a subset with both measured BNP and eGFR values. Subgroups were divided according to age ≥ 60 years old, LVEF < 45%, eGFR < 60 [mL/min/1.73 m2], history of coronary artery disease (CAD), TnI ≥ 0.03 [ng/mL], sex, uric acid ≥ 9.8 [mg/dl], hs-CRP ≥ 2 [mg/dl], history of diabetes mellitus, and history of chronic obstructive pulmonary disease (COPD). Statistical analyses were performed using JMP Pro version 9 (SAS Institute, Inc, Cary, North Carolina).
RESULTS
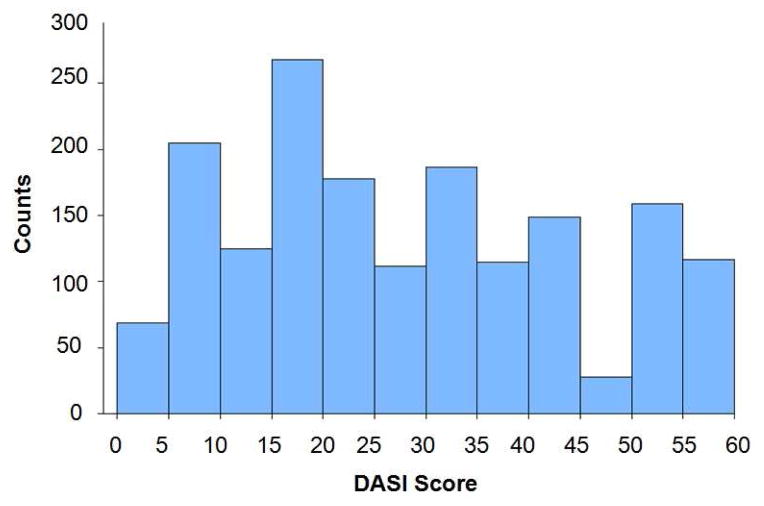
Baseline characteristics are described in Table 2, which is representative of a patient population with chronic heart failure. The following is the description of reasons for cardiac catheterization within the study cohort (subjects can have more than one reason per person): history of positive or abnormal stress test (30%), evaluation for possible ischemic causes of symptoms (63.5%), preoperative evaluation (24%), and history of cardiomyopathy (14%). DASI surveys were successfully completed in 1,700 study participants, and scores across this study cohort were non-parametrically distributed (Figure 1). The median DASI score was 26.2 [interquartile range from 15.5–42.7]. The mean DASI scores for quartiles 1–4 were 8.7±3.7, 20.2±3.2, 33.4±3.9, and 50.0±5.9, respectively. Decreasing DASI scores were associated with increasing comorbidity (Table 2), but not with LVEF (p=0.4). There were no differences in either angiotensin converting enzyme inhibitor (ACEI)/angiotensin receptor blocker (ARB) or beta-blocker usage across DASI quartiles (p=0.2 and p=0.8, respectively).
Table 2.
Baseline Characteristics
| DASI Score Quartile | |||||
|---|---|---|---|---|---|
| Variable | <15.5 | 15.5–26.1 | 26.2–42.7 | >42.7 | p-value |
| Age [years] | 68 ± 11 | 69 ± 11 | 66 ± 11 | 64 ± 11 | <.0001 |
| Male (%) | 45.4 | 60.0 | 72.6 | 81.0 | <.0001 |
| BMI [kg/m2] | 29.8 [25.9, 35.1] | 28.4 [24.8, 33.3] | 28.1 [25.2, 32.3] | 28.9 [25.5, 32.3] | 0.001 |
| Diabetes Mellitus (%) | 49.3 | 44.4 | 35.8 | 27.2 | <.0001 |
| Hypertension (%) | 83.0 | 80.0 | 79.3 | 78.2 | 0.4 |
| Coronary Artery Disease (%) | 80.3 | 75.4 | 77.3 | 69.7 | 0.003 |
| Smoking History (%) | 66.6 | 72.1 | 74.3 | 75.2 | 0.03 |
| LVEF [%] | 45 [30, 55] | 40 [25, 55] | 40 [25, 55] | 40 [29, 55] | 0.4 |
| BNP [pg/ml] | 457 [155, 971] | 337 [136, 781] | 316 [119, 639] | 205 [86,411] | <.0001 |
| eGFR [mL/min/1.73 m2] | 56.1 [41.9, 74.0] | 57.1 [42.8, 74.1] | 59.0 [46.8, 75.0] | 61.7 [49.9, 76.0] | 0.001 |
| Beta-Blocker (%) | 66.8 | 68.0 | 68.0 | 65.2 | 0.8 |
| ACEI/ARB (%) | 63.9 | 67.7 | 68.8 | 70.5 | 0.2 |
| Loop Diuretic (%) | 68.1 | 69.3 | 55.2 | 40.7 | <.0001 |
Values are either mean +/− standard deviation or median [IQR] unless stated; p-values calculated via ANOVA or Kruskall-Wallis test for continuous variables and chi-square method for categorical variables.
Abbreviations: BMI: body mass index; DASI: Duke Activity Score Index; LVEF: left ventricular ejection fraction; BNP: brain natriuretic peptide; eGFR: estimated glomerular filtration rate, MDRD; ACEI: angiotensin converting enzyme inhibitor; and ARB: angiotensin receptor blocker.
Figure 1.
DASI Score Distribution in Study Cohort (n=1,700)
Predicting Mortality Risk with DASI score
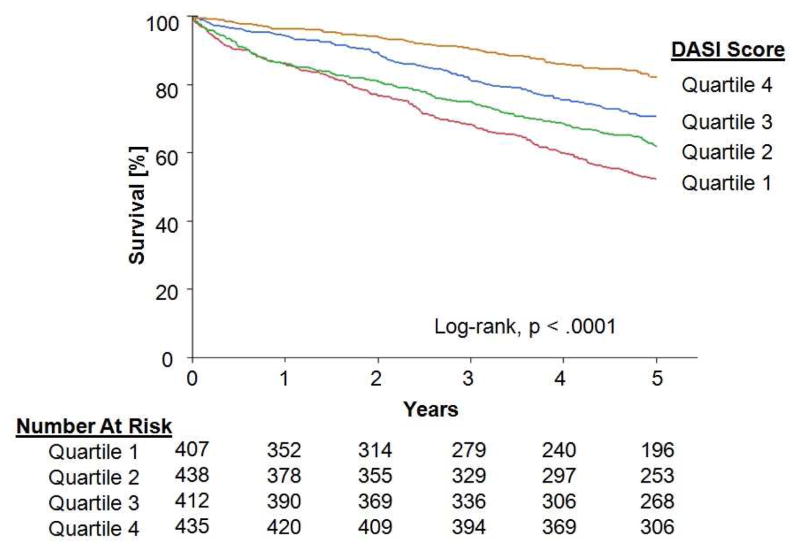
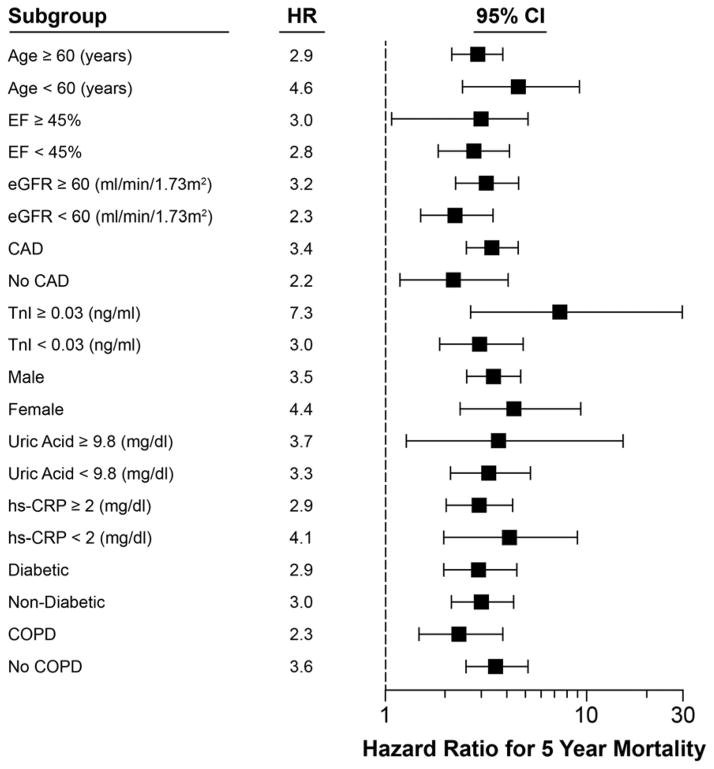
In our study cohort, 1,692 study participants were followed for all-cause mortality over 5 years after study entry. At 5 years there were total 556 deaths and 1023 subjects made it to the end of follow-up. 113 study participants were lost to follow-up. Kaplan-Meier estimates of survival were calculated for 1,692 participants. (Figure 2) The estimated 5-year survival rate was 67%. DASI score quartiles 1–4 had 193, 166, 120, and 77 deaths, respectively, by the end of follow-up. There were significant decrements in survival across increasing DASI score quartiles, Log-rank chi-square 96.1 and p<.0001. The lowest DASI score quartile predicted 3.3-fold increase in risk of 5-year mortality when compared to the highest DASI score quartile (Hazard ratio [HR] 3.33, 95% confidence interval [CI] 2.57–4.36, p<.0001). (Table 3). After additional adjustment for traditional risk factors, lower DASI scores still independently predicted an increased risk for death (HR 2.78 [95% CI 2.10–3.72], p<0.0001). Furthermore, when stratifying DASI score by median (26.2), in addition to multivariate adjustment for traditional risk factors, the area under the curve for 5-year mortality is 69.4%. In a sensitivity analysis with multivariate adjustment for LVEF in addition to traditional risk factors, lower DASI scores remained predictive of increased mortality (HR 2.79 [95% CI 2.10–3.72], p<.0001). Compared to DASI scores > 40, DASI scores ≤ 40 predicted a two-fold increased risk for death (HR 2.00 [95% CI 1.58–2.58], p<.0001). Sub-group analyses reveal that DASI scores predict all-cause mortality across dichotomized sub-groups of: age, gender, history of coronary artery disease, history of diabetes mellitus, history of COPD, eGFR, and LVEF (Figure 3)
Figure 2.
Kaplan-Meier Estimates of 5-Year Survival Rates According to DASI Score
Table 3.
Cox Proportional Hazards Model for Risk of 5-Year Mortality Stratified According to DASI Scores
| Model | Hazard Ratio | 95% Confidence Interval | p-value |
|---|---|---|---|
| Univariate | 3.33 | 2.57–4.36 | <.0001 |
| Multivariate | |||
| Adjusted for traditional risk factors* | 2.78 | 2.10–3.72 | <.0001 |
| Adjusted for traditional risk factors* + BNP +eGFR** | 2.57 | 1.64–4.15 | <.0001 |
Quartile 1 versus 4; Abbreviations, BNP: brain natriuretic peptide; and eGFR: estimated glomerular filtration rate.
Traditional risk factors including age, gender, systolic blood pressure, history of diabetes, smoking, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol;
Subset of 800 subjects with biomarker data available.
Figure 3.
Subgroup Analysis of DASI Score and 5-Year Mortality
Prognostic value of DASI adjusting for cardio-renal biomarkers
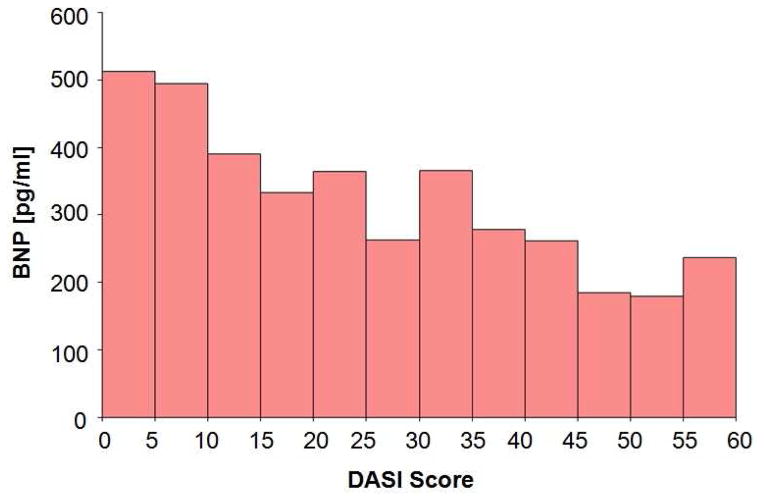
In a subset of patients with available BNP data (Figure 4) at the time of DASI questionnaire, we observed only a modest correlation between BNP (Spearman’s rho=0.210, p<0.0001) and DASI score. Estimated glomerular filtration rate was also modestly correlated with DASI score (Spearman’s rho=0.107, p<.0001) for the total cohort. Lower DASI scores still independently predicted an increased risk for death after adjusting for traditional risk factors, BNP, and eGFR (HR 2.57 [95% CI 1.64–4.15], p<0.0001, respectively).
Figure 4.
Median BNP by DASI Score (n=819)
DISCUSSION
There are several key findings in our study. First, we surveyed a large cohort of patients with chronic stable heart failure undergoing elective coronary evaluation and observed an association between lower functional status (as measured by the DASI questionnaire) and greater risk of 5-year mortality. Second, this association remains robust after multivariate adjustment for traditional cardiac risk factors and, in a subset of patients, after additional adjustment for cardio-renal biomarkers. While commonly attributed to the underlying co-morbid conditions, the association between diminished functional capacity and 5-year all-cause mortality appears consistent across a variety of subgroups of patients with different co-morbid conditions and clinical characteristics. Taken together, these findings illustrate the potential of patient-centric insight gained by conducting a simple questionnaire tool developed to assess overall functional capacity.
Functional capacity is an important component of a patient-centric evaluation of heart failure, and recommendations for its careful assessment have been recommended in the latest clinical management guidelines.(9–10) While the DASI has been developed for over 20 years,(5) its application has been largely restricted as a subjective assessment tool in clinical trials. The DASI is a simple, self-administered questionnaire that assesses perceived functional status. Rather than relying on recall, it is comprised of questions relating to the self-assessment one’s ability to perform activities that represent major aspects of physical function. Set up as a continuous measure, DASI scores correlate with peak oxygen uptake in during cardiopulmonary stress testing.(5) The DASI has been validated in cohorts of patients with HF, obstructive CAD, and COPD.(5, 11–12) Although the accuracy of DASI score in predicting peak oxygen uptake in the setting of HF has been challenged,(8, 13) our findings support the notion that the clinical utility may likely extend beyond performance on stress testing. Indeed, a recent comparison of several commonly utilized objective assessments of functional capacity did not validate cardiopulmonary exercise stress testing as equivalent to other simpler forms of exercise capacity evaluation like the 6-minute walk test in terms of prognostic utility.(14)
To our knowledge this is the largest cohort of patients with HF who have completed the DASI survey and have been followed longitudinally for adverse outcomes. Our findings confirm several smaller studies that have suggested the prognostic value of functional status assessment in the setting of heart failure. For example, DASI scores were lower in a population of 130 patients with impaired LVEF recently hospitalized for decompensated HF who experienced adverse events after 9 months of follow-up compared to those that did not.(6) Paired with BNP, those with low DASI scores and higher BNP levels were more likely to have a lower event-free survival.(6) In adults >75 years old, lower functional status, as measured by a preadmission Barthel Index, was strong predictor of 3-month mortality.(15) In the setting of cardiac surgery, lower DASI scores have also been associated with higher mortality risk,(16) and changes in DASI scores have observed post-operatively.(17) It has been suggested that DASI scoring may vary based upon factors that affect functional capacity such as age, gender, COPD, and the presence of diabetes mellitus.(18) Yet, based on our findings its prognostic value in these cohorts remained robust. Additionally, we found DASI scores correlate with mortality in patients with either reduced or preserved left ventricular function and were not related to systematic differences (e.g. ACEI/ARB or beta-blocker usage) in medical management of heart failure.
There are other prognostic instruments exist that capture functional status as well. In a cohort of 6,975 outpatients with chronic heart failure from the Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico-Heart Failure Trial (GISSI-HF), a NYHA classification III or IV was independently associated with a more adverse prognosis than NYHA classification II.(19) NYHA is a simple score ordinally assessing exertional symptoms in H. Yet it has notable limitations: (1) no consistent assessment method and (1) high interoperator variability.(20) The Minnesota Living with Heart Failure Questionnaire® (MLHFQ) is a validated heart failure specific questionnaire based on a Likert scale.(21) Data from the Irbesartan in Heart Failure With Preserved Ejection Fraction Study (I-PRESERVE) suggests that lower MHLF scores are associated with adverse outcomes in patients with HF with preserved LVEF.(22) In contrast to these scores, the DASI can provide a continuum of scores, is easily administered with simple yes/no patient responses either orally or written.
Increasing plasma levels of natriuretic peptides have been associated with adverse outcomes in chronic HF (23) and may provide incremental prognostic information independent of clinical assessment.(24) Furthermore, based on an ancillary study from the Studies on Left Ventricular Dysfunction (SOLVD) trial worsening renal function is independently associated with both mortality and disease progression in patients with LV dysfunction.(25) Renal function also provides additional prognostic information in patients with HF independent of functional status as measured by the 6 minute walk test.(26) Our observation regarding the incremental prognostic value of DASI after inclusion of BNP and eGFR in multivariate adjustment suggested that factors incremental to cardio-renal disease progression that are captured by the patient’s own perception of their own functional status may affect long-term outcomes. For example, other underlying metabolic derangements or physical limitations maybe uncovered during DASI assessment.
Our results must be interpreted in the context of several limitations in our study design. Because DASI scores were only measured at one point in time, we were unable to examine the variability and prognostic value of changing DASI scores over time or the impact of different therapies in the interim. Furthermore, baseline New York Heart Association functional class was unavailable and hospitalization readmissions were not adjudicated. We cannot exclude the presence of unmeasured confounding by baseline depressive symptoms as these were not assessed upon study inclusion or selection bias for those undergoing coronary angiography for further evaluation and management of HF at a tertiary care center, even though based on baseline clinical characteristics it appears relatively representative of a contemporary patient population with HF. However, the majority of the patients in this analysis had an ischemic cardiomyopathy and there was low usage of beta- and renin-angiotensin- blocking agents. Nevertheless, based on our promising results and in the era where patient-centric outcomes are valued, further investigations into the clinical utility of baseline and serial DASI questionnaire administrations are warranted.
CONCLUSIONS
In patients with stable HF, functional status assessment, as measured by the DASI questionnaire, predicts mortality at 5-years. This assessment provides independent and additional prognostic information beyond the measurement of BNP and eGFR. Lower DASI scores predict mortality across a variety of subgroups of differing prognosis in patients with HF. These results highlight the importance of assessing functional status in patients with HF. Future studies using functional status assessment as a tool for treatment intensification in HF are warranted.
HIGHLIGHTS.
The Duke Activity Status Index is a simple self-assessment tool estimating functional capacity.
1,700 subjects with chronic heart failure completed the questionnaire.
All subjects were undergoing elective coronary angiography upon entry to this prospective cohort.
Lower scores were associated with higher mortality on long term follow-up.
These results highlight the importance of functional status assessment in chronic heart failure.
Acknowledgments
FUNDING
This research was supported by grants from the National Institutes of Health (R01HL103931, P20HL113452, P01HL076491, P01HL098055), NIH/Office of Dietary Supplements (R01HL103866), and the Cleveland Clinic Clinical Research Unit of the Case Western Reserve University CTSA (UL1TR 000439). Dr. Hazen is also partially supported by a gift from the Leonard Krieger endowment and by the Foundation LeDucq.
Footnotes
DISCLOSURE
Dr. Tang has previously received investigator-initiated research grant support from Abbott Laboratories, Inc with no personal financial payments. Dr. Hazen is named as co-inventor on pending patents held by the Cleveland Clinic relating to cardiovascular diagnostics. Dr. Hazen reports having been paid as a consultant for the following companies: Abbott Diagnostics, Cleveland Heart Lab, Esperion, Lilly, Liposcience Inc., Merck & Co., Inc., P&G, and Pfizer Inc. Dr. Hazen reports receiving research funds from Abbott, Cleveland Heart Lab, Liposcience Inc., P&G, and Pfizer Inc. Dr. Hazen reports having the right to receive royalty payments for inventions or discoveries related to cardiovascular diagnostics or therapeutics from the companies shown below: Abbott Laboratories, Inc., Cleveland Heart Lab., Esperion, Frantz Biomarkers, LLC, Liposcience Inc., and Siemens. All other authors have no relationships to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could a3ect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Justin L. Grodin, Email: grodinj@ccf.org.
Muhammad Hammadah, Email: hammadm2@ccf.org.
Yiying Fan, Email: richard_fan90@yahoo.com.
Stanley L. Hazen, Email: hazens@ccf.org.
W. H. Wilson Tang, Email: tangw@ccf.org.
References
- 1.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011 Mar 1;123(8):933–44. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, et al. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004 Jul 21;292(3):344–50. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 3.Tsutamoto T, Wada A, Maeda K, Hisanaga T, Maeda Y, Fukai D, et al. Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation. 1997 Jul 15;96(2):509–16. doi: 10.1161/01.cir.96.2.509. [DOI] [PubMed] [Google Scholar]
- 4.Kociol RD, Pang PS, Gheorghiade M, Fonarow GC, O’Connor CM, Felker GM. Troponin elevation in heart failure prevalence, mechanisms, and clinical implications. J Am Coll Cardiol. 2010 Sep 28;56(14):1071–8. doi: 10.1016/j.jacc.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 5.Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989 Sep 15;64(10):651–4. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 6.Parissis JT, Nikolaou M, Birmpa D, Farmakis D, Paraskevaidis I, Bistola V, et al. Clinical and prognostic value of Duke’s Activity Status Index along with plasma B-type natriuretic peptide levels in chronic heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 2009 Jan 1;103(1):73–5. doi: 10.1016/j.amjcard.2008.08.045. [DOI] [PubMed] [Google Scholar]
- 7.Nelson CL, Herndon JE, Mark DB, Pryor DB, Califf RM, Hlatky MA. Relation of clinical and angiographic factors to functional capacity as measured by the Duke Activity Status Index. Am J Cardiol. 1991 Oct 1;68(9):973–5. doi: 10.1016/0002-9149(91)90423-i. [DOI] [PubMed] [Google Scholar]
- 8.Arena R, Humphrey R, Peberdy MA. Using the Duke Activity Status Index in heart failure. J Cardiopulm Rehabil. 2002 Mar-Apr;22(2):93–5. doi: 10.1097/00008483-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1–194. doi: 10.1016/j.cardfail.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 Oct 15;62(16):1495–539. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 11.Alonso J, Permanyer-Miralda G, Cascant P, Brotons C, Prieto L, Soler-Soler J. Measuring functional status of chronic coronary patients. Reliability, validity and responsiveness to clinical change of the reduced version of the Duke Activity Status Index (DASI) Eur Heart J. 1997 Mar;18(3):414–9. doi: 10.1093/oxfordjournals.eurheartj.a015260. [DOI] [PubMed] [Google Scholar]
- 12.Carter R, Holiday DB, Grothues C, Nwasuruba C, Stocks J, Tiep B. Criterion validity of the Duke Activity Status Index for assessing functional capacity in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2002 Jul-Aug;22(4):298–308. doi: 10.1097/00008483-200207000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Myers J, Zaheer N, Quaglietti S, Madhavan R, Froelicher V, Heidenreich P. Association of functional and health status measures in heart failure. J Card Fail. 2006 Aug;12(6):439–45. doi: 10.1016/j.cardfail.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Forman DE, Fleg JL, Kitzman DW, Brawner CA, Swank AM, McKelvie RS, et al. 6-min walk test provides prognostic utility comparable to cardiopulmonary exercise testing in ambulatory outpatients with systolic heart failure. J Am Coll Cardiol. 2012 Dec 25;60(25):2653–61. doi: 10.1016/j.jacc.2012.08.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Formiga F, Chivite D, Conde A, Ruiz-Laiglesia F, Franco AG, Bocanegra CP, et al. Basal functional status predicts three-month mortality after a heart failure hospitalization in elderly patients - The prospective RICA study. Int J Cardiol. 2014 Mar 1;172(1):127–31. doi: 10.1016/j.ijcard.2013.12.169. [DOI] [PubMed] [Google Scholar]
- 16.Koch CG, Li L, Lauer M, Sabik J, Starr NJ, Blackstone EH. Effect of functional health-related quality of life on long-term survival after cardiac surgery. Circulation. 2007 Feb 13;115(6):692–9. doi: 10.1161/CIRCULATIONAHA.106.640573. [DOI] [PubMed] [Google Scholar]
- 17.Jaeger AA, Hlatky MA, Paul SM, Gortner SR. Functional capacity after cardiac surgery in elderly patients. J Am Coll Cardiol. 1994 Jul;24(1):104–8. doi: 10.1016/0735-1097(94)90548-7. [DOI] [PubMed] [Google Scholar]
- 18.Koch CG, Khandwala F, Cywinski JB, Ishwaran H, Estafanous FG, Loop FD, et al. Health-related quality of life after coronary artery bypass grafting: a gender analysis using the Duke Activity Status Index. J Thorac Cardiovasc Surg. 2004 Aug;128(2):284–95. doi: 10.1016/j.jtcvs.2003.12.033. [DOI] [PubMed] [Google Scholar]
- 19.Barlera S, Tavazzi L, Franzosi MG, Marchioli R, Raimondi E, Masson S, et al. Predictors of mortality in 6975 patients with chronic heart failure in the Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico-Heart Failure trial: proposal for a nomogram. Circulation Heart failure. 2013 Jan;6(1):31–9. doi: 10.1161/CIRCHEARTFAILURE.112.967828. [DOI] [PubMed] [Google Scholar]
- 20.Raphael C, Briscoe C, Davies J, Ian Whinnett Z, Manisty C, Sutton R, et al. Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure. Heart. 2007 Apr;93(4):476–82. doi: 10.1136/hrt.2006.089656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorkin L, Norvell NK, Rosen RC, Charles E, Shumaker SA, McIntyre KM, et al. Assessment of quality of life as observed from the baseline data of the Studies of Left Ventricular Dysfunction (SOLVD) trial quality-of-life substudy. Am J Cardiol. 1993 May 1;71(12):1069–73. doi: 10.1016/0002-9149(93)90575-w. [DOI] [PubMed] [Google Scholar]
- 22.Komajda M, Carson PE, Hetzel S, McKelvie R, McMurray J, Ptaszynska A, et al. Factors associated with outcome in heart failure with preserved ejection fraction: findings from the Irbesartan in Heart Failure with Preserved Ejection Fraction Study (I-PRESERVE) Circ Heart Fail. 2011 Jan;4(1):27–35. doi: 10.1161/CIRCHEARTFAILURE.109.932996. [DOI] [PubMed] [Google Scholar]
- 23.Anand IS, Fisher LD, Chiang YT, Latini R, Masson S, Maggioni AP, et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT) Circulation. 2003 Mar 11;107(9):1278–83. doi: 10.1161/01.cir.0000054164.99881.00. [DOI] [PubMed] [Google Scholar]
- 24.James SK, Lindahl B, Siegbahn A, Stridsberg M, Venge P, Armstrong P, et al. N-terminal pro-brain natriuretic peptide and other risk markers for the separate prediction of mortality and subsequent myocardial infarction in patients with unstable coronary artery disease: a Global Utilization of Strategies To Open occluded arteries (GUSTO)-IV substudy. Circulation. 2003 Jul 22;108(3):275–81. doi: 10.1161/01.CIR.0000079170.10579.DC. [DOI] [PubMed] [Google Scholar]
- 25.Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2000 Mar 1;35(3):681–9. doi: 10.1016/s0735-1097(99)00608-7. [DOI] [PubMed] [Google Scholar]
- 26.Mahon NG, Blackstone EH, Francis GS, Starling RC, 3rd, Young JB, Lauer MS. The prognostic value of estimated creatinine clearance alongside functional capacity in ambulatory patients with chronic congestive heart failure. J Am Coll Cardiol. 2002 Sep 18;40(6):1106–13. doi: 10.1016/s0735-1097(02)02125-3. [DOI] [PubMed] [Google Scholar]