Abstract
The incidence and longitudinal trends of patients with ST-elevation myocardial infarction (STEMI) presenting to U.S. emergency departments (EDs) are currently unknown. Efforts to use effective treatments for cardiovascular disease may decrease ED STEMI presentation. We conducted a descriptive epidemiological analysis of STEMI visits to EDs between 2006 and 2011 using the Nationwide ED Sample (NEDS), the largest source of U.S. ED data, to determine the incidence of patients with STEMIs presenting to U.S. EDs. We included adult ED visits with an ICD-9CM diagnosis of STEMI and calculated incidence rates for STEMI ED visits using U.S. census population data. Incidence calculations were stratified by age group, geographic region, and year. From 2006–2011, there was a mean of 258,106 STEMIs presenting to EDs per year, declining from 300,466 in 2006 to 227,343 in 2011. Incidence of ED STEMI visits per 10,000 adults declined from 10.1 (95% CI 9.8, 10.8) in 2006 to 7.3 (95% CI 6.8, 7.8) in 2011. The Midwest had the highest rate of ED STEMIs at 10.0 (95% CI 9.2, 10.8) and the West had the lowest with 6.6 (95% CI 6.1, 7.0). The incidence of STEMI decreased for all age groups during the study period. In conclusion, we report the first national estimates of STEMI presentation to U.S. EDs, which demonstrate decreasing incidence across all age groups and all geographic regions between 2006 and 2011. A declining STEMI incidence may affect the quality and timeliness of STEMI care. Continued national STEMI surveillance is needed to guide healthcare resource allocation.
Keywords: Acute MI, emergency department, care delivery system, resource allocation, access to care
Presentation of a patient with ST-elevation myocardial infarction (STEMI) to an emergency department (ED) represents an acute medical emergency requiring immediate complex care coordination to achieve narrow timeliness guidelines for myocardial reperfusion.1 While cardiovascular disease prevalence is expected to increase in the United States,2 a more recent study of nearly 50,000 patient hospitalizations found significant reductions in hospitalizations for STEMI since 1999.3 However, neither of these earlier studies describes ED utilization for STEMI, national trends, or regional differences within the United States. If the incidence of STEMI across the United States is truly declining, particularly in combination with recent systematic efforts to take STEMI patients straight to cardiac catheterization for reperfusion (i.e., bypassing the ED), significant changes may affect the ED’s role in the acute management of patients with STEMI.4–7 Therefore, we sought to quantify the contemporary incidence of STEMI in United States EDs through a national sample of ED visits.
METHODS
We conducted a cross-sectional analysis of STEMI visits to EDs in the United States between 2006 and 2011, using the largest source of ED data in the United States, the Nationwide Emergency Department Sample (NEDS). NEDS, a publicly available database from the Healthcare Cost and Utilization Project (HCUP), contains a 20% sample of all hospital-based ED visits annually in the United States.8 NEDS tracks geographic, hospital and patient characteristics including diagnosis codes for patient visits. NEDS was constructed using the HCUP State Emergency Department Databases (SEDD) and State Inpatient Databases (SID). In 2011, the most recent year with NEDS data available, 30 states and 951 hospitals contributed data for 29 million ED visits. NEDS contains weights to calculate national estimates using the sample of ED visits contained within the dataset. Prior research evaluated the quality of hospital discharge data and found that NEDS’ estimates of ED use are comparable to other national datasets for ED data. 9,10
For the current analysis, we included all adult (age ≥ 18 years) ED visits with a diagnosis of STEMI (International Classification of Diseases, Ninth Revision, Clinical Modification codes: 410.01, 410.11, 410.21, 410.31, 410.41, 410.51, 410.61, 410.81, or 410.91) and calculated incidence rates for STEMI ED visits using United States census data.11 Incidence calculations were stratified by year (2006, 2007, 2008, 2009, 2010, 2011), age group (18–34, 35–44, 45–54, 55–64, 65–74, 75–84, ≥ 85 years old) and geographic region (Northeast, South, Midwest, West).
RESULTS
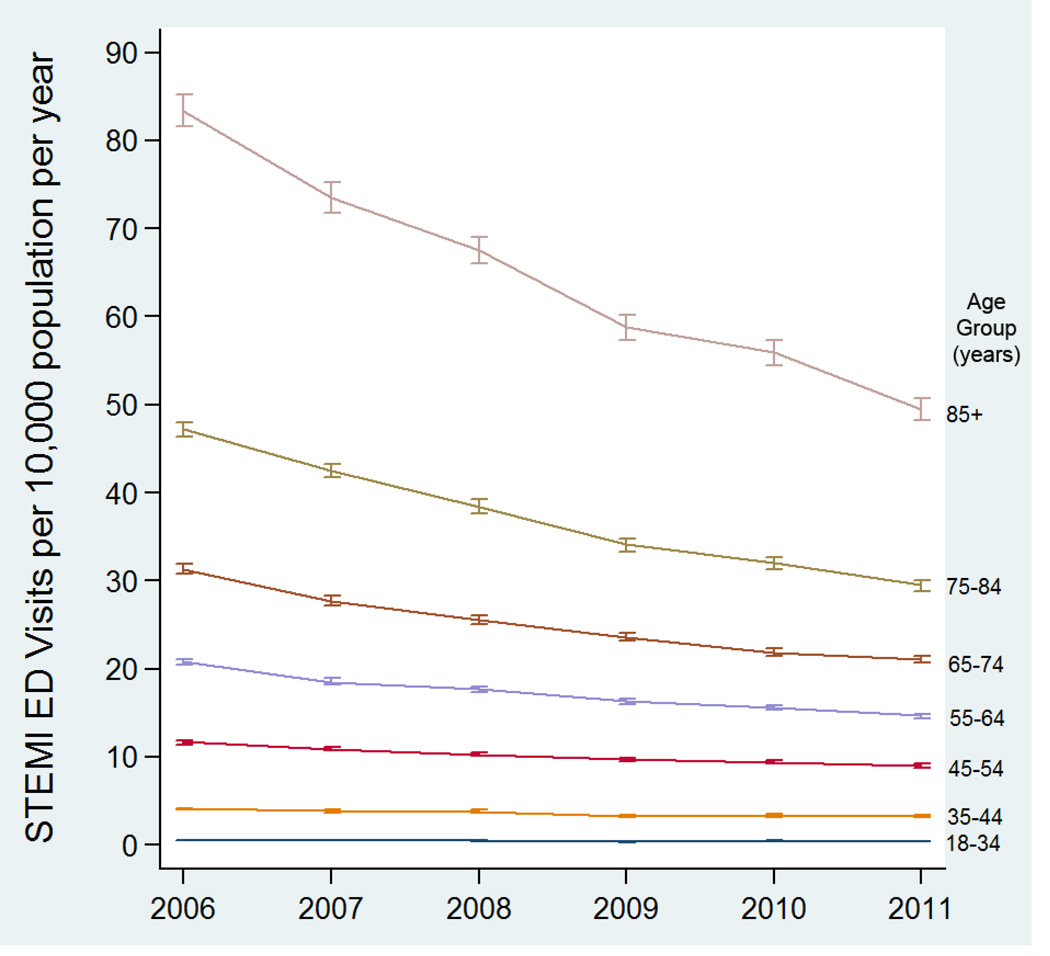
Between 2006 and 2011, there were an estimated 1,548,634 ED visits for STEMIs in the United States, representing 0.26% of all ED visits. The annual incidence rate of STEMI ED visits during this entire 6-year period was 8.5 (95% CI 8.1, 8.8) per 10,000 adults. When considering incidence separately by year, incidence decreased from 2006 to 2011, with declining incidence each subsequent year throughout the study period and across all age groups (Figure 1) and geographic regions (Table 1). Patients ≥ 85 years old had the highest incidence of STEMI ED visits, but also experienced the greatest decline in incidence during the study period. Among the 4 geographic regions in the United States, the West had the lowest overall rate of STEMI with 5.8 (95% CI 5.0, 6.5) STEMI ED visits per 10,000 adults and the Midwest had the largest reduction in STEMI incidence during the study period.
Figure 1. Annual incidence of emergency department visits for ST-elevation myocardial infarction (STEMI) per 10,000 adults in the United States by age group, 2006–2011.
Error bars indicate 95% confidence intervals.
Table 1.
Patient characteristics for ST-elevation Myocardial Infarction emergency department visits in the United States for the years 2006 and 2011. All rates are reported as ST-elevation Myocardial Infarction emergency department visits per 10,000 adults.
| Visits (95% CI) | ||||||
|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
| U.S. STEMI ED visits (n) | ||||||
| 300,466 | 276,779 | 263,475 | 243,471 | 237,100 | 227,343 | |
| Incidence of STEMI ED visits in U.S. (visits/10,000 adults/year) | ||||||
| 10.1 (9.3, 10.8) | 9.2 (8.5, 9.9) | 8.7 (8.0, 9.3) | 7.9 (7.3, 8.6) | 7.7 (7.1, 8.3) | 7.3 (6.8, 7.8) | |
| Incidence of STEMI ED visits by Age Group (visits/10,000 adults/year) | ||||||
| 18–34 | 0.5 (0.4, 0.5) | 0.5 (0.4, 0.6) | 0.5 (0.4, 0.5) | 0.4 (0.3, 0.4) | 0.5 (0.4, 0.5) | 0.4 (0.4, 0.4) |
| 35–44 | 4.1 (3.7, 4.5) | 3.9 (3.5, 4.2) | 3.8 (3.5, 4.2) | 3.3 (3.0, 3.6) | 3.4 (3.0, 3.7) | 3.3 (3.0, 3.6) |
| 45–54 | 11.7 (10.7, 12.6) | 10.9 (10.0, 11.8) | 10.3 (9.4, 11.2) | 9.7 (8.9, 10.5) | 9.4 (8.6, 10.2) | 9.0 (8.3, 9.8) |
| 55–64 | 20.8 (19.1, 22.5) | 18.5 (17.0, 20.1) | 17.7 (16.2, 19.1) | 16.3 (14.9, 17.6) | 15.6 (14.3, 16.8) | 14.7 (13.6, 15.8) |
| 65–74 | 31.3 (28.8, 33.8) | 27.7 (25.5, 30.0) | 25.6 (23.6, 27.7) | 23.6 (21.8, 25.5) | 21.8 (20.1, 23.6) | 21.1 (19.5, 22.7) |
| 75–84 | 47.2 (43.6, 50.8) | 42.5 (39.2, 45.9) | 38.4 (35.3, 41.6) | 34.1 (31.3, 36.8) | 32.0 (29.5, 34.6) | 29.5 (27.3, 31.6) |
| 85+ | 83.4 (76.9, 90.0) | 73.5 (67.6, 79.4) | 67.5 (61.9, 73.1) | 58.8 (53.7, 63.8) | 55.9 (51.4, 60.5) | 49.5 (45.8, 53.2) |
| Incidence of STEMI ED visits by U.S. Geographic Region (visits/10,000/year) | ||||||
| Northeast | 8.8 (7.1, 10.5) | 8.1 (6.6, 9.6) | 7.8 (6.2, 9.4) | 7.3 (5.9, 8.8) | 7.1 (5.8, 8.4) | 6.8 (5.5, 8.0) |
| Midwest | 12.4 (10.5, 14.3) | 11.0 (9.4, 12.7) | 9.8 (8.3, 11.3) | 9.2 (7.8, 10.6) | 9.2 (7.8, 10.7) | 8.4 (7.2, 9.7) |
| South | 10.9 (9.6, 12.3) | 10.0 (8.7, 11.3) | 9.6 (8.3, 10.8) | 8.5 (7.4, 9.6) | 8.0 (6.9, 9.1) | 7.9 (7.0, 8.8) |
| West | 7.5 (6.2, 8.7) | 6.9 (5.7, 8.1) | 6.9 (5.8, 7.9) | 6.3 (5.2, 7.3) | 6.1 (5.2, 7) | 5.8 (5.0, 6.5) |
Note: ED, emergency department; STEMI, ST-elevation myocardial infarctions
DISCUSSION
We report the first national estimates of STEMI incidence in EDs in the United States. Our results show that STEMI remains a common emergency treated in EDs in the United States, but its incidence is decreasing in the setting of increased cardiovascular disease in the population.2
There are a number of possible explanations for this observation. First, improved acute and chronic management of cardiovascular disease, so-called guideline-directed medical therapies (GDMT) by the American Heart Association, prevents acute, severe manifestations, such as STEMI. 12, 13 Second, recent efforts to reduce time-to-reperfusion have focused on transporting STEMI patients from pre-hospital providers directly to cardiac catheterization laboratories bypassing the ED. Guidelines published by the American Heart Association in 2004 first recommended that hospitals without PCI capabilities should be bypassed by pre-hospital personnel caring for a STEMI patient.14 Subsequent research supported the concept of earlier STEMI recognition by pre-hospital providers and ED bypass to reduce the time to myocardial reperfusion.4, 7, 15 Finally, as seen in our study, the largest reduction in STEMI incidence occurred in the age group ≥ 85 years old; older patients not pursuing ED care for STEMIs as frequently as in the past may be due to advanced directives and patient preferences.16
Our findings build on prior studies that reported declining annual incidence rates for STEMI hospitalizations in 2 separate regions of the United States.3, 13 The longitudinal trends of Yeh’s data combined with our findings further support the idea that STEMI incidence is decreasing. Moreover, the magnitude of decline in STEMI presentations is similar both in hospitalization and ED visit rates. Yeh et al. reported 5.0 STEMI hospitalizations per 10,000 population in 2008,4 whereas we identified 6.9 STEMI ED visits per 10,000 population in the western United States during the same year in our study. Considering the incidence rates between both hospitalizations and ED visits are so close, this suggests that the reduction may be due an actual reduction in STEMIs within the population.
Declining ED visits for STEMI could have important implications for the quality of care delivered to these patients in the ED. Patients with classic clinical presentations of STEMI may be more likely to get sent directly for cardiac catheterization, bypassing the ED, while those with atypical presentations (e.g., without chest pain) continue to present to the ED. This shift in presenting characteristics seen by ED physicians may make timely identification of a patient with STEMI more challenging. Atypical patients are harder to diagnose with STEMI, have more delays to definitive care,17 and may result in unnecessary testing and hospitalizations for chest pain18, 19 due to the medicolegal risk of emergency physicians misdiagnosing patients with suspected cardiac ischemia.20, 21
Finally, the declining incidence of STEMIs also affects policy decisions and the distribution of financial resources in the care of patients with cardiovascular disease. For heart disease, estimated costs for acute care in the form of hospital inpatient stays ($67.4 billion) and ED visits ($5.6 billion) accounted for more than 7 times the cost of prevention in the form of prescribed medicines ($9.9 billion).22 In addition, acute management of STEMI process improvement efforts may have plateaued as evidenced by shorter door-to-balloon times no longer improving hospital mortality.23 Therefore, at what point do we re-evaluate whether the current distribution of funding should change? Should the incidence rate of STEMI influence this decision? Given the declines in STEMI incidence and the low likelihood that further reductions in door-to-balloon times would substantially improve clinical outcomes, we suspect that further improving acute care timeliness for STEMI is reaching a level of diminishing returns. An examination of resource allocation, perhaps with re-distribution of more funds toward preventive care, is warranted.
This study has several limitations. First, the focus of this study was presentation to the ED so it has a limited ability to describe the overall incidence of STEMI not treated in the ED. Second, NEDS is an administrative dataset and does not provide all of the variables necessary to explain why the incidence of STEMI is decreasing. For example, there are no data on ED bypass to understand whether STEMI patients were sent directly to a PCI center. In addition, there are no clinical data to understand whether patients presented with characteristic features of STEMI, whether the same patient returned for a recurrence of STEMI, the quality or timeliness of care provided nor clinical outcomes for these patients.
In summary, in this dataset, the incidence of patients with STEMI presenting to United States EDs has declined between 2006 and 2011, and has declined across all age groups and United States regions.
Acknowledgments
Funding Sources: The project described was supported by Award Number K12 HL109019 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW. American College of Cardiology Foundation/American Heart Association Task Force on Practice G. 2013 accf/aha guideline for the management of st-elevation myocardial infarction: A report of the American College of Cardiology foundation/American Heart Association task force on practice guidelines. Circulation. 2013;127:e362–e425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ. American Heart Association Advocacy Coordinating C, Stroke C, Council on Cardiovascular R, Intervention, Council on Clinical C, Council on E, Prevention, Council on A, Thrombosis, Vascular B, Council on C, Critical C, Perioperative, Resuscitation, Council on Cardiovascular N, Council on the Kidney in Cardiovascular D, Council on Cardiovascular S, Anesthesia, Interdisciplinary Council on Quality of C, Outcomes R. Forecasting the future of cardiovascular disease in the united states: A policy statement from the american heart association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 3.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 4.Bagai A, Al-Khalidi HR, Munoz D, Monk L, Roettig ML, Corbett CC, Garvey JL, Wilson BH, Granger CB, Jollis JG. Bypassing the emergency department and time to reperfusion in patients with prehospital ST-segment-elevation: Findings from the reperfusion in acute myocardial infarction in carolina emergency departments project. Circ Cardiovasc Interv. 2013;6:399–406. doi: 10.1161/CIRCINTERVENTIONS.112.000136. [DOI] [PubMed] [Google Scholar]
- 5.Bradley EH, Nallamothu BK, Curtis JP, Webster TR, Magid DJ, Granger CB, Moscucci M, Krumholz HM. Summary of evidence regarding hospital strategies to reduce door-to-balloon times for patients with st-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Crit Pathw Cardiol. 2007;6:91–97. doi: 10.1097/HPC.0b013e31812da7bc. [DOI] [PubMed] [Google Scholar]
- 6.Cone DC, Lee CH, Van Gelder C. EMS activation of the cardiac catheterization laboratory is associated with process improvements in the care of myocardial infarction patients. Prehosp Emerg Care. 2013;17:293–298. doi: 10.3109/10903127.2013.773112. [DOI] [PubMed] [Google Scholar]
- 7.Fosbol EL, Granger CB, Jollis JG, Monk L, Lin L, Lytle BL, Xian Y, Garvey JL, Mears G, Corbett CC, Peterson ED, Glickman SW. The impact of a statewide pre-hospital stemi strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation. 2013;127:604–612. doi: 10.1161/CIRCULATIONAHA.112.118463. [DOI] [PubMed] [Google Scholar]
- 8.HCUP Nationwide Emergency Department Sample (NEDS) Rockville, MD: Agency for Healthcare Research and Quality; 2006–2011. Healthcare Cost and Utilization Project (HCUP) www.hcup-us.ahrq.gov/nedsoverview.jsp. [PubMed] [Google Scholar]
- 9.Schoenman JA, Sutton JP, Kintala S, Love D, Maw R. Salt Lake City, UT: 2005. [Accessed October 20, 2014]. The value of hospital discharge databases. Available at: http://www.hcupus.ahrq.gov/reports/final_report.pdf. [Google Scholar]
- 10.Owens PL, Barrett ML, Gibson TB, Andrews RM, Weinick RM, Mutter RL. Emergency department care in the United States: A profile of national data sources. Ann Emerg Med. 2010;56:150–165. doi: 10.1016/j.annemergmed.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 11.National Center for Health Statistics. U.S. Census Populations With Bridged Race Categories. [Accessed June 26, 2014]; http://www.cdc.gov/NCHS/nvss/bridged_race.htm.
- 12.Go AS, Iribarren C, Chandra M, Lathon PV, Fortmann SP, Quertermous T, Hlatky MA. Statin and beta-blocker therapy and the initial presentation of coronary heart disease. Ann Intern Med. 2006;144:229–238. doi: 10.7326/0003-4819-144-4-200602210-00004. [DOI] [PubMed] [Google Scholar]
- 13.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction) Circulation. 2004;110:588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 15.Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, McNamara RL, Parkosewich J, Loeb JM, Krumholz HM. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355:2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 16.Wood FO, Leonowicz NA, Vanhecke TE, Dixon SR, Grines CL. Mortality in patients with st-segment elevation myocardial infarction who do not undergo reperfusion. Am J Cardiol. 2012;110:509–514. doi: 10.1016/j.amjcard.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 17.Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283:3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 18.Kline JA, Shapiro NI, Jones AE, Hernandez J, Hogg MM, Troyer J, Nelson RD. Outcomes and radiation exposure of emergency department patients with chest pain and shortness of breath and ultralow pretest probability: A multicenter study. Ann Emerg Med. 2014;63:281–288. doi: 10.1016/j.annemergmed.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Penumetsa SC, Mallidi J, Friderici JL, Hiser W, Rothberg MB. Outcomes of patients admitted for observation of chest pain. Arch Intern Med. 2012;172:873–877. doi: 10.1001/archinternmed.2012.940. [DOI] [PubMed] [Google Scholar]
- 20.Katz DA, Williams GC, Brown RL, Aufderheide TP, Bogner M, Rahko PS, Selker HP. Emergency physicians' fear of malpractice in evaluating patients with possible acute cardiac ischemia. Ann Emerg Med. 2005;46:525–533. doi: 10.1016/j.annemergmed.2005.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Studdert DM, Mello MM, Sage WM, DesRoches CM, Peugh J, Zapert K, Brennan TA. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293:2609–2617. doi: 10.1001/jama.293.21.2609. [DOI] [PubMed] [Google Scholar]
- 22.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart Disease and Stroke Statistics-- 2014 Update: A Report From the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS. Door-to-balloon time and mortality among patients undergoing primary pci. N Engl J Med. 2013;369:901–909. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]