Abstract
Adopting a multi-level approach, this study examined risk factors for adolescent suicidal ideation, with specific attention to (a) hypothalamic-pituitary-adrenal (HPA) axis stress responses and (b) the interplay between HPA-axis and other risk factors from multiple domains (i.e., psychological, interpersonal and biological). Participants were 138 adolescent females (Mage=14.13 years, SD=1.40) at risk for suicidal behaviors. At baseline, lifetime suicidal ideation and a number of risk factors were assessed (i.e., depressive symptoms, impulsiveness, pubertal status and peer stress). Participants were exposed to a psychosocial stress task and HPA-axis responses were assessed by measuring cortisol levels pre- and post-stressor. At 3 months post-baseline, suicidal ideation again was assessed. Using group-based trajectory modeling, three groups of cortisol stress-response patterns were identified (i.e., hyporesponsive, normative, and hyperresponsive). As compared to females in the normative and hyporesponsive group, females in the hyperresponsive group were more likely to report a lifetime history of suicidal ideation at baseline, above and beyond the effects of the other predictors. Moreover, as compared to females in the normative group, females in the hyperresponsive group were at increased risk for reporting suicidal ideation 3 months later, after controlling for prior ideation. No interactions between cortisol group and the other risk factors were significant, with the exception of a non-significant trend between impulsiveness and cortisol group on lifetime suicidal ideation. Findings highlight the importance of HPA-axis responses to acute stressors as a risk factor for suicidal ideation among adolescents.
Keywords: Suicidal ideation, Hypothalamic-pituitary-adrenal axis, Adolescence, Pubertal status, Peer stress, Impulsiveness
Suicide is a major worldwide public health concern, especially among youth. In the United States, suicide is the second leading cause of death among 10–18 year olds (Center for Disease Control and Prevention [CDC] 2010), and rates of suicidal thoughts and behaviors are strikingly high in adolescence, especially among females. Suicidal ideation is the most commonly reported form of suicidality, with lifetime prevalence rates of approximately 12 % among community adolescents aged 13–18 years (15.3 % and 9.1 % for females and males respectively; Nock et al. 2013). Notably, about 41 % of adolescent females and 23 % of adolescent males with a lifetime history of suicidal ideation ultimately attempt suicide, in most cases within the first year of onset of suicidal ideation (Nock et al. 2013).
Despite these alarming statistics, research examining suicidal behaviors during adolescence has mostly relied on cross-sectional and retrospective data, thus yielding limited information to prevent suicidal behaviors or to develop evidence-based treatments. Although extant longitudinal work has revealed some distal risk factors (e.g., mental illness) for engaging in suicidal behaviors, a multi-level approach that integrates different domains of distal and proximal risk rarely has been applied to examine adolescent suicidality. In particular, relatively little attention has been devoted to risk factors other than mental illness (e.g., mental disorders and psycho-pathological symptoms; Sourander et al. 2001) and social adversity (e.g., child maltreatment and interpersonal stressful life events; King and Merchant 2008), such as risk factors within the biological domain (Bridge et al. 2006).
To address this gap in the literature, this study adopted a developmental psychopathology perspective (Cicchetti and Rogosch 2002) to investigate, in a sample of adolescent females, several risk factors for suicidal ideation across multiple domains of functioning (i.e., psychological, interpersonal and biological). Specific attention was devoted to examining adolescents’ physiological responses to stress (i.e., hypothalamic-pituitary-adrenal [HPA] axis); moreover, the interplay between biological stress-responses and other well-established risk factors for youth suicidal ideation was explored.
Developmental psychopathology theory posits dynamic interplay across multiple systems of development (e.g., social, psychological, biological) that must be considered holistically to understand both normative and atypical behavior (Cicchetti and Rogosch 2002). The transition to adolescence is accompanied by notable changes across several developmental systems, including psychological (e.g., heightened self-scrutiny), social (e.g., increase in interpersonal stressors), and biological (e.g., pubertal development, heightened physiological responses to stress) domains (Rudolph 2014). Developmental theorists have recognized that different factors within each system may confer heightened vulnerability to several psy-chopathological symptoms in adolescence (e.g., depressive symptoms, self-injurious thoughts), perhaps especially among adolescent females who experience earlier pubertal development and more increased interpersonal stress than do males (e.g., Conley et al. 2012). Within the psychological literature, relatively little attention has been dedicated towards understanding biological processes that may predict adolescent females’ suicidality, however.
Biological processes likely are quite relevant for understanding suicide risk, either as main effect predictors or as factors that moderate the effects of other developmental systems on suicidal thoughts and behaviors. Within the adult literature, neurobiological models of suicide (e.g., Mann 2003; Turecki et al. 2012) indicate that HPA dysfunction may play a key role in the development of suicidal behaviors. The HPA-axis represents one of the main human stress response systems. Activation of the HPA-axis initiates in the central nervous system, where an individual’s perception of a threatening and aversive environmental stimulus (e.g., a stressful event) gives rise to a physiological cascade process that eventually stimulates the adrenal gland to release glucocorticoids, cortisol in humans (Gunnar and Quevedo 2007). Circulating cortisol binds to glucocorticoid receptors located in several body cells, including brain cells, thus regulating gene expression and leading to a number of physiological alterations, for instance in the immune system (Sapolsky et al. 2000).
Although the molecular changes resulting from the HPA-axis responses are adaptive and prepare the individual to deal with stressful stimuli, dysregulated HPA-axis activity—which may be the result of both genetic and environmental effects (Gunnar and Quevedo 2007)—may have negative consequences on the individual’s mental health. Research generally has demonstrated that both hyper- as well as hyporesponsivity of the HPA-axis to psychosocial stressors, as measured by cortisol levels, are associated with heightened risk for developing psychopathological symptoms in youth, including internalizing and externalizing symptomatology (Obradović 2012). Dysregulated HPA activity may increase risk for suicidal behaviors by altering cognitive functions, such as decision-making and emotional processing (Turecki et al. 2012). Whereas moderate cortisol levels facilitate cognitive functioning by binding to glucocorticoid receptors in the brain regions involved in these processes (e.g., prefrontal cortex; limbic system; Lupien et al. 2007) both hyper- and hyporesponsivity of the HPA-axis to acute psychosocial stressors may compromise cognitive functioning, for instance, by interfering with decision making processes and increasing emotional reactivity. Notably, impairments of these cognitive functions have been associated with suicidal behaviors (Jollant et al. 2011). Hence, there are strong reasons to believe that altered physiological responses to interpersonal stressors may affect the occurrence of adolescent suicidal ideation.
The stronger empirical support for the role of the HPA responses in suicidal behaviors, at least among adults, comes from studies conducted among inpatients with mood disorders (Mann et al. 2006). To examine HPA functioning, most of this work has relied on a pharmacological method, the Dexamethasone Suppression Test (DST). Findings from DST studies suggest that HPA hyperresponsivity may distinguish between inpatients who die by suicide from those who do not. Specifically, meta-analyses of prospective studies indicate that non-suppression of cortisol in response to the DST increased the risk for suicide about 4.5-fold (Mann et al. 2006). Yet, although prior research generally suggests that HPA hyperresponsivity may be predictive of completed suicide, results are less consistent with respect to suicidal thoughts and behaviors (e.g., ideation and attempts). Indeed, both HPA hyperresponsivity (e.g., Jokinen and Nordström 2009) as well as hyporesponsivity (e.g., Lindqvist et al. 2008) have been found to associate with suicidal thoughts and behaviors (but also see Duval et al. 2001).
There has been little examination of the predictive effect of HPA activity on adolescent suicidal behaviors. To our knowledge, the only study conducted among adolescents revealed that high levels of evening cortisol were associated with increased risk for attempting suicide within the 10 years among adolescents who also experienced a lifetime major depression episode (Mathew et al. 2003). HPA dysregulation may be a particularly salient risk factor for suicidal behaviors during adolescence. Indeed, not only is adolescence characterized by normative changes in the social context (e.g., increase in stress; Rudolph 2009) and physiological response systems (e.g., stress hyperreactivity; Gunnar et al. 2009), but also research suggests that the effects of high levels of gluco-corticoids on the activity of developing brain regions in adolescence (e.g., prefrontal cortex) may be accentuated during this period as compared to adulthood (Lupien et al. 2009). Thus, adolescents with HPA hyperresponsivity may be expected to be at high risk for engaging in suicidal behaviors.
According to a developmental psychopathology perspective (e.g., Cicchetti and Rogosch 2002), examining the dynamic interplay between different domains of functioning may be especially helpful for understanding youth development and identifying adolescents who are at particular risk for developing psychopathology. In line with such a perspective, not only may HPA dysregulation be expected to predict suicidal ideation, above and beyond the effects of risk factors from other domains, but also the cost associated with dysregulated HPA responses may be particularly evident for those adolescents who also display other risk factors.
Several social-psychological risk factors for suicide were examined in this study. A well-established finding is that adolescents who experience high levels of depressive symptoms are at increased risk for suicidal ideation (e.g., Prinstein et al. 2008). Among behavioral traits, impulsiveness has been documented as a strong predictor of adolescent suicidal behaviors, including ideation (Brezo et al. 2006). Hence, it seems plausible that the effects of dysregulated HPA stress-responses are exacerbated for adolescents who are already psychologically predisposed to develop suicidal ideation, such as more depressed and impulsive adolescents (Mathew et al. 2003).
Moreover, HPA responses may interact with interpersonal risk factors to predict suicidal ideation. It generally has been recognized that interpersonal factors enhance risk for suicidal behaviors, above and beyond the effect of psychological vulnerabilities. The notion that stressful interpersonal events contribute to the development of suicidal behaviors is presumed by different theoretical models. For instance, in line with the interpersonal theory of suicide (Van Orden et al. 2010), interpersonal stress may lead to suicidal ideation by threatening an individual’s sense of belongingness. Given the central role that peer relationships assume in adolescents’ lives (Parker et al. 2006), stressors within the peer domain may represent crucial proximal risk factors for the occurrence of adolescent suicidal ideation. Previous studies have empirically supported this hypothesis, showing that stressful peer experiences, such as peer victimization and lacking friends, may prospectively predict suicidal ideation above and beyond the effect of psychological risk factors, especially among adolescent females (e.g., Bearman and Moody 2004; Heilbron and Prinstein 2010). Thus, as posited by diathesis stress models of psychopathology (e.g., Monroe and Simons 1991), adolescents with heightened physiological sensitivity (i.e., HPA dysregulation) may be at risk for suicidal ideation especially when exposed to adverse interpersonal contexts, such as a stressful peer context.
Finally, a more advanced pubertal status also may constitute a vulnerability factor for adolescent suicidal ideation. Pubertal development is accompanied by a number of normative changes across different domains of development (i.e., psychological, social and biological) which may increase adolescents’ vulnerability for developing psychopathology (Rudolph 2014). Accordingly, perceived early pubertal development has been shown to be prospectively associated with increased risk for suicidal behaviors, especially among adolescent females (e.g., Wichstrøm 2000). The costs of dysregulated HPA responses may therefore be augmented among adolescents with a more mature pubertal status, resulting in increased risk for suicidal ideation. This hypothesis seems highly plausible especially given existing evidence suggesting that the hormonal changes occurring with the onset of puberty (e.g., increase in gonadal hormones) are reciprocally interrelated with HPA-axis activity (Viau 2002).
The first aim of this short-term longitudinal study was to investigate whether individual differences in HPA-axis response patterns to an acute psychosocial stressor predicted suicidal ideation in adolescent females. The effect of adolescents’ HPA response patterns on suicidal ideation was examined in the context of a multi-level model, which integrated other developmentally salient predictors of suicidal ideation, including depressive symptoms, impulsiveness, pubertal status, and peer stress. Adolescents’ HPA responses to stress were evaluated by measuring cortisol levels before and after exposure to a psychosocial stress task. Importantly, adolescents’ cortisol responses were analyzed using group-based trajectory modeling (Nagin 2005). Recent work (Van Ryzin et al. 2009) has shown the advantages of applying this analytic approach to identify different atypical response patterns to stress. Based on the aforementioned evidence from the adult literature and on prior work examining psychopathological outcomes associated with adolescent physiological responses to stress, we expected dysregulated cortisol response patterns (in particular hyperresponses) to predict suicidal ideation over time, above and beyond other predictors. The second aim of the study was to explore the interplay between HPA-axis responses to stress and risk factors from other domains. In line with existing theoretical models (e.g., diathesis stress models), the effect of cortisol response patterns was hypothesized to be stronger among adolescents with other risk factors.
Method
Participants
Participants included 138 adolescent females, between 12 and 16 years old (Mage=14.13 years, SD=1.40), with a history of mental health concerns (e.g., affective disorders, anxiety, substance use, disruptive behavior disorders) in the 2 years prior to the study. Participants were mostly born in the United States (90.6 %); 61.6 % identified as Caucasian, 26.1 % as African-American, 2.2 % as Latino American, 1.4 % as Asian-American and 8.7 % as belonging to mixed or other ethnic groups. About half of the adolescents reported that they lived with two biological parents (36.8 %) or in a family with two adults in the household (15.4 % with a parent and a step-parent, grandparent, or other relative; 4.4 % with adoptive parents); the other participants reported living in a single-adult household (37.5 % with the biological mother; 2.2 % with the biological father; 3.7 % with another relative). At baseline, 56.5 % of participants reported current use of prescription medication. Participants’ medications primarily included an-tidepressants (n=38), stimulants (n=15), antipsychotics (n= 14), antihistamines (n=7), antibiotics (n=7), anxiolytic (n=6) and anticonvulsants (n=4). Three months post-baseline, approximately 89 % (n=127) of adolescents completed a follow-up interview. No significant differences were revealed between adolescents with and without follow-up data on any of the main study variables.
Procedure
Data from this study were drawn from an ongoing longitudinal project examining youth cognitive and physiological responses to interpersonal stressors to understand the development of self-injurious thoughts and behaviors. For the current investigation, data from participants who had completed the baseline and first follow-up assessment were analyzed (n=138).
Participants were recruited via local psychiatric inpatient units (approximately 40 %) and community advertisements, such as flyers, e-mails and TV commercials. Eligibility for the study was determined based on four main criteria: (a) female gender; (b) 12 to 16 years old; (c) caregiver (e.g., parent or guardian) available to take part in the study; and (d) a history of mental health concerns (e.g., affective disorders, anxiety, substance use, disruptive behavior disorders) in the past 2 years. Adolescents’ history of mental health concerns was determined via a phone interview with adolescents’ care-givers, and was defined as either having (a) prior diagnosis; (b) prior treatment; or (c) prior symptomatology assessed with an interview by trained researchers. These inclusion criteria were employed to recruit a sample of adolescents at high risk for engaging in suicidal behaviors. Several participants experienced clinical levels of psychopathological symptoms at baseline, as indicated by the caregivers’ report on the parent version of the Behavioral Assessment System for Children (BASC-PRS; Reynolds and Kamphaus 1992). Specifically, about 24 % of females had clinical scores on the conduct disorder scale, 23.2 % on the attention problem scale, 17.4 % on the hyperactivity scale, 11 % on the anxiety scale and 8.7 % on the depression scale. 1 Notably, participants with either active psychosis, mental retardation or any pervasive developmental disorder were not considered eligible for the study.
At baseline, participants were invited to the laboratory together with a primary caregiver. Upon arrival, adolescents and their caregivers were welcomed by trained research assistants who described the content of the laboratory visit and asked them to complete a consent form. During the laboratory visit, participants completed a series of different tasks, beginning with: (a) a structured clinical interview to assess prior self-injurious thoughts and behaviors (see Measures); (b) self-report questionnaires (e.g., depressive symptoms, impulsiveness); and (c) a modified Trier Social Stressor Task (TSST; Kirschbaum et al. 1993). Participants’ caregivers also completed a series of measures, including adolescents’ current medication usage and pubertal development (see Measures).
The TSST began about 3 h after arrival at the laboratory. To ensure that pre-task cortisol reflected resting HPA-axis activity, before the TSST participants underwent a pre-task relaxation period consisting of watching an emotionally neutral movie clip. The TSST included instructions for adolescents to pretend to audition for a reality show about how teenagers make friends and interact with other teens (Calhoun et al. 2012). To be chosen for the reality show, participants were instructed to give a 3-min audition speech about this topic, immediately after a 1-min preparation period. During the preparation and the speech, participants were oriented towards a camera connected to a closed-circuit feedback screen displaying their own live image. A young adult male judge was present in the room with the adolescent female during the speech task, ostensibly evaluating the quality of their performance. The presence of an adult and opposite-sex judge was intended to increase the social-evaluative nature of the task, given that laboratory tasks that elicit social evaluation and threaten an individual’s social self are known to specifically activate HPA-axis stress responses (Dickerson and Kemeny 2004). Participants were told that the judge could not answer any question and attended their speech to evaluate their audition and ensure that they performed at their best. The judge was instructed not to provide any feedback during the speech; however, he prompted participants to continue their speech if they stopped before the end of the 3 min.
Approximately 3 months post-baseline, a trained researcher re-administered a structured clinical interview to assess recent suicidal thoughts and behaviors (see Measures). All procedures were approved by the human subjects committee of the University of North Carolina at Chapel Hill.
Measures
Suicidal Ideation
Suicidal ideation was assessed with the Self-Injurious Thoughts and Behaviors Interview (SITBI; Nock et al. 2007). The SITBI is a structured clinical interview designed to assess a variety of self-injurious thoughts and behaviors, including suicidal ideation. Two main variables were derived from this measure. At baseline, lifetime history of suicidal ideation (e.g., “Have you ever had thoughts of killing yourself?”) was assessed. At follow-up, the interview was administered by phone and suicidal ideation in the prior 3 months was assessed. The suicidal ideation variables were used as dichotomous indicators, distinguishing between adolescents who reported suicidal ideation and those who did not. The SITBI has been widely used to assess self-injurious thoughts and behaviors in community and clinical samples of youth (e.g., Nock and Banaji 2007), and its psychometric properties have been previously established (Nock et al. 2007).
Depressive Symptoms
Depressive symptoms were measured with the Mood and Feelings Questionnaire (MFQ; Costello and Angold 1988). The MFQ is a 33-item self-report measure designed to assess depressive symptoms in children and adolescents aged 8–18 years old. Participants were asked to indicate on a 3-point scale how true (0 = not true, 1 = sometimes true, 2 = mostly true) each statement (e.g., “I felt miserable or unhappy”, “I did everything wrong”) describing depressive symptoms was in the prior 2 weeks. The MFQ is a widely used measure and has shown good psychometric properties both in non-clinical and clinical samples of adolescents (e.g., Daviss et al. 2006). For the purpose of the present investigation, four items referring to suicidal thoughts (e.g., “I thought about killing myself,” “I thought that life wasn’t worth living”) were omitted. A sum score was computed across the remaining 29 items, with higher scores indicating greater depressive symptoms (α=0.94).
Impulsiveness
A global measure of impulsiveness was collected using a short-version of the UPPS Impulsive Behavior scale (Whiteside and Lynam 2001). The UPPS is a 45-item multi-dimensional measure developed to tap four personality facets leading to impulsive behaviors, including urgency, lack of premeditation, lack of perseverance, and sensation seeking. The brief version used in this study consisted of 16 items, four items for each dimension of impulsiveness. Participants were instructed to report on a 4-point scale their agreement (1 = agree strongly, 4 = disagree strongly) with each of the 16 items (e.g., “I usually make up my mind through careful reasoning”, “It is hard for me to resist acting on my feelings”). This brief version has been previously employed in studies involving clinical and non-clinical youth to examine associations with suicidal ideation (e.g., Klonsky and May 2010). In the present study, a global score of impulsiveness was computed by averaging across the 16 items (reverse-coded as needed), with higher scores indicating higher impulsiveness (α=0.78).
Pubertal Status
The Pubertal Development Scale (PDS; Petersen et al. 1988) was used to assess pubertal status. The PDS consists of five items about physical development, including body hair, skin changes, growth spurt, breast development and menarche. All items are scored on a 4-point scale (1 = no development, 4 = development seems complete) with the exception of the menarche item, which is rated dichotomously (1 = no, 4 = yes). The psychometric properties of the PDS have been well established (e.g., Petersen et al. 1988). The PDS was administered to both adolescents and their primary caregivers. For both adolescent and caregiver reports, a mean score was computed across the five items (α=0.75 and 0.69, respectively), with higher scores indicating more advanced pubertal status. Consistent with prior work (e.g., Rudolph 2008), a combined measure of pubertal status was computed by averaging between adolescents’ and their care-givers’ report (r=0.70).
Peer Stress
The peer subscale of the Child Chronic Strain Questionnaire (CCSQ; Rudolph et al. 2001) was administered to measure peer stress. The peer subscale includes 11 items assessing a number of common stressors within the peer/friend domain (e.g., “Do kids at school pick on or tease you?” “Has it been hard for you to make friends?”). Adolescents were asked to indicate on a 5-point scale how much (1 = not at all, 5 = very much) they experienced each stressor in the prior 6 months. The psychometric properties of this measure have been previously documented (Rudolph et al. 2001). A mean score was computed across the 11 items with higher values indicating higher peer stress (α=0.78).
Cortisol Responses
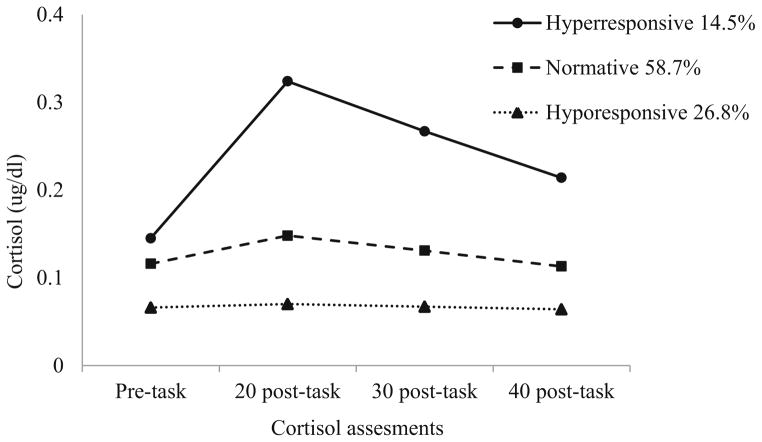
To examine adolescents’ HPA-axis responses to the TSST, cortisol levels were assessed four times: immediately prior to the stress task, and 20, 30 and 40 min post-task. Cortisol was measured by saliva sampling via salivettes. Cortisol salivary samples were frozen for storage at −25 °C and then shipped on dry ice to Pennsylvania State University’s Behavioral Endocrinology Laboratory for assay (Salimetrics, PA). Samples were assayed for cortisol using a 510-k cleared high-sensitive enzyme immunoassay designed to assess adrenal function. This test, which uses 25 μl of saliva (for singlet determinations), has a lower limit sensitivity of 0.007 μg/dl and a range of sensitivity from 0.007 to 1.2 μg/dl. As common practice, all cortisol values were log transformed to correct for skewness prior to analyses, but non-transformed values are presented in Table 1 and Fig. 1 for ease of interpretation.
Table 1.
Descriptive statistics and bivariate correlations of main study variables
| N (%) | M (SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Suicidal ideation | ||||||||||||
| 1. Lifetime | 64 (46.4 %) | 1 | ||||||||||
| 2. 3-month follow-up | 24 (19.5 %) | 0.38*** | 1 | |||||||||
| Cortisol (ug/dl) | ||||||||||||
| 3. Pre-task | 0.12 (0.06) | 0.26* | 0.15 | 1 | ||||||||
| 4. 20 min post-task | 0.16 (0.09) | 0.10 | 0.10 | 0.49*** | 1 | |||||||
| 5. 30 min post-task | 0.14 (0.07) | 0.14 | 0.16† | 0.47*** | 0.96*** | 1 | ||||||
| 6. 40 min post-task | 0.12 (0.05) | 0.22* | 0.20* | 0.54*** | 0.90*** | 0.94*** | 1 | |||||
| Baseline predictors | ||||||||||||
| 7. Depressive symptoms | 13.51 (11.16) | 0.41*** | 0.45*** | 0.02 | −0.07 | −0.03 | 0.01 | 1 | ||||
| 8. Pubertal Status | 3.37 (0.47) | 0.30*** | 0.15 | 0.10 | 0.16† | 0.21* | 0.18* | 0.19* | 1 | |||
| 9. Impulsiveness | 2.40 (0.45) | 0.35*** | 0.22* | −0.06 | 0.03 | 0.04 | 0.08 | 0.40*** | 0.31*** | 1 | ||
| 10. Peer stress | 2.07 (0.69) | 0.25** | 0.19* | −0.05 | −0.04 | −0.01 | 0.01 | 0.53*** | 0.08 | 0.18* | 1 | |
Cortisol mean values are raw scores; yet, log transformed cortisol values were employed for bivariate correlations
p<0.10.
p<0.05.
p<0.01.
p<0.001
Fig. 1.
Cortisol response trajectory groups to the modified Trier Social Stressor Task. Trajectory groups were identified using log transformed cortisol values; yet, raw cortisol values are reported in the figure
Because for some participants (n=53) pre-task cortisol was assessed using a different procedure (i.e., passive drool procedure), these cortisol values were considered missing, in order to allowed comparison with the other cortisol assessments. Missing values on pre-task cortisol levels were handled in M-plus using the full information maximum likelihood (FIML) method (see Strategy of Analyses).
Cortisol Timing
Upon the arrival in the laboratory, which ranged approximately from 11:00 a.m. to 1:00 p.m., participants were asked to report at what time they woke up that morning. A cortisol timing variable was computed by subtracting adolescents’ awakening time from the time of the first cortisol assessment. Given the diurnal rhythm of cortisol, cortisol timing was controlled to account for individual differences in the time of cortisol assessment. The cortisol timing variable ranged between 3 and 13 h (Mdn=5 h; M= 5.92 h, SD=2.05).
Medication
Both adolescents and their caregivers reported participants’ current medication usage. A dichotomous variable was created distinguishing between adolescents who currently used medications that may have affected cortisol levels (i.e., birth control, corticosteroid) and those who did not. Approximately 13 % of females (n=18) reported using birth control and 8 % of females (n=11) reported using corticosteroids.
Strategy of Analyses
Three sets of analyses were conducted. First, descriptive statistics were performed for primary study variables, and mean changes in cortisol levels across the four assessments (i.e., from pre-task to 40 min post-task) were examined to determine adolescents’ HPA-axis responses to the TSST. Second, group-based trajectory modeling (GBTM; Nagin 2005) was employed to identify different subgroups of adolescents showing diverse cortisol response patterns to the TSST. Specifically, GBTM aims to identify the smallest number of trajectory groups approximating the continuous distribution of trajectories within a given population (Nagin 2005). GBTM has been previously shown to be a valuable approach to examine cortisol changes (Van Ryzin et al. 2009). Models were estimated using a piecewise linear growth curve model, consisting of two separate linear slopes. The first slope was specified to capture adolescents’ reactivity to the TSST, from pre-task to 20 min post-task. The second slope was specified to capture adolescents’ recovery to the TSST, from 20 to 40 min post-task. Although typically at least three measurements are required to define a slope, because in GBTM random effects (i.e., variances around the intercept and growth factors) are not estimated (i.e., constrained to zero), the reactivity slope could be specified with two measurements only. To ensure that cortisol response patterns were not influenced by medication usage and cortisol diurnal rhythm, each manifested cortisol indicator was regressed on both medication usage (i.e., no medication vs. medication usage) and cortisol timing. Different criteria were used to select the best-fitting model, including the Bayesian information criteria (BIC) and the sample size adjusted BIC (aBIC; lower values indicate more parsimonious models), the Lo-Mendell-Rubin ratio likelihood test (LMR-LRT; significant p value indicates better fit), entropy (critical value>0.70), and the theoretical value of the classes (Nagin 2005). Each model was fitted using 100 random perturbations of starting values to ensure replication of the best likelihood and avoid local maxima. GBTMs were estimated in M-plus version 6.0 (Muthén and Muthén 1998–2010), using the FIML method to handle cortisol missing data. Last, cortisol trajectory membership and other baseline predictors (i.e., depressive symptoms, impulsiveness, pubertal status and peer stress) were used to predict suicidal ideation (at baseline and at follow-up) in multivariate logistic regression analyses, while adjusting for adolescent age. Additional logistic regression models were performed in which the interaction effects between cortisol trajectory membership and each of the other baseline predictors were explored separately. Given the exploratory nature of some hypotheses, effects approaching significance (p<0.10) also were interpreted with caution.
Results
Descriptive Analyses
Table 1 presents descriptive statistics and bivariate correlations among the main study variables. At baseline, 46.4 % of participants reported a lifetime history of suicidal ideation, and at follow-up, 19.5 % reported suicidal ideation within the previous 3 months. A total of 17.4 % of participants had a score of 25 or higher on the depressive symptoms scale, corresponding to a clinical cut-off of 29 on the 33-item version of the MFQ (e.g., Daviss et al. 2006). Moreover, more than half of participants (56.5 %) reported experiencing low or mild peer stress (mean score≤2), 32.6 % reported isolated stress (mean score> 2 and≤3) and 10.9 % more than isolated stress (mean scores> 3).
A repeated measures ANOVA with cortisol at the four assessments as within-subject factors was performed to examine mean changes in cortisol levels from pre- to 40 min post-task. A significant effect of time was observed, F (3, 81)= 24.86, p<0.001. Polynomial contrasts revealed a significant quadratic trend, F(1, 83)=50.09, p<0.001, indicating that cortisol levels increased from pre- to 20 min post-task and subsequently decreased approximately to pre-task levels at 40 min post-task. A significant cubic effect also was observed, F(1, 83)=45.91, p<0.001, suggesting an asymmetric cortisol trend characterized by an initial sharp increase and a subsequent more gradual decline.
Several significant correlations were found among the main study variables. Lifetime suicidal ideation modestly correlated with pre-task cortisol, whereas both lifetime suicidal ideation and suicidal ideation at 3 months post-baseline were modestly associated with cortisol assessed at 40 min post-task. Small to moderate correlations were observed between lifetime suicidal ideation and each of the other baseline predictors, including depressive symptoms, pubertal status, impulsiveness and peer stress. Similarly, suicidal ideation at 3 months post-baseline was positively associated with the baseline predictors, with the exception of pubertal status. Moderate to large correlations were revealed across the different cortisol assessments. Among the baseline predictors, only pubertal status was significantly correlated with cortisol levels, with small positive associations with cortisol assessed at 30 and 40 min post-task. Finally, depressive symptoms, impulsiveness, pubertal status, and peer stress all were positively correlated with one other, with the exception of pubertal status and peer stress.
Cortisol Response Trajectory Groups
Based on fit indices from group-based cortisol trajectory models and the theoretical value of the trajectory groups, a three-class model was selected as the best fitting model (see Table 2).2 The final three trajectory groups are displayed in Fig. 1. The first trajectory group, labeled normative group, included over half of participants (58.7 %) who exhibited a typical cortisol response pattern to the TSST. This trajectory group was characterized by moderate reactivity, as indicated by a significant positive reactivity slope (b=0.26, p=0.001), in combination with a full recovery 40 min after the TSST (i.e., cortisol decreased to pre-task levels), evident in a significant negative recovery slope (b=−0.08, p<0.001). In addition to the normative group, two trajectory groups of adolescents showing dysregulated cortisol response patterns were identified. One group (26.8 %) consisted of adolescents who revealed a blunted cortisol response to the psychosocial stress task. Adolescents in this trajectory group, labeled hyporesponsive group, displayed an essentially flat reaction to the TSST, although the mean estimates of the reactivity and recovery slopes, despite remarkably small, both emerged to be significant (b=0.16, p=0.018; b=−0.04, p=0.027, respectively). Finally, the last trajectory group (14.5 %), labeled hyperresponsive group, was composed of adolescents who exhibited heightened cortisol responses to the TSST. The hyperresponsive group was characterized by a significant large mean estimate for the reactivity slope (b=0.53, p<0.001) and a significant negative mean estimate for the recovery slope (b=−0.12, p<0.001). Notably, contrary to adolescents in the normative group, adolescents in the hyper-responsive group did not show full recovery of cortisol at 40 min post-task.3
Table 2.
Fit indices for group-based trajectory models of cortisol
| Classes |
|
|||||
|---|---|---|---|---|---|---|
| Log likelihood | AIC | BIC | aBIC | Entropy | LMR-LRT | |
| 1 | 45.13 | −60.27 | −16.36 | −63.82 | ||
| 2 | 138.22 | −238.44 | −182.82 | −242.93 | 0.820 | 0.157 |
| 3 | 244.68 | −443.37 | −376.04 | −448.80 | 0.946 | 0.030 |
| 4 | 295.75 | −537.50 | −458.47 | −543.89 | 0.941 | 0.102 |
| 5 | 344.21 | −626.42 | −535.68 | −633.75 | 0.944 | 0.261 |
AIC akaike information criterion, BIC bayesian information criterion, aBIC sample size adjusted Bayesian information criterion; entropy=measure of classification accuracy; LMR-LRT lo-mendell-rubin ratio likelihood test
Multivariate Predictors of Adolescent Suicidal Ideation
Lifetime Suicidal Ideation
Results from the logistic regression model predicting adolescents’ lifetime history of suicidal ideation at baseline are presented at the left side of Table 3. After adjusting for age, most predictors had unique and additive associations with suicidal ideation. Specifically, high levels of depressive symptoms and impulsiveness independently increased the probability of adolescents’ report of lifetime suicidal ideation. Similarly, more advanced pubertal status was associated with an increased likelihood of lifetime suicidal ideation.4 Although peer stress correlated with lifetime suicidal ideation, it was not associated with a lifetime history of suicidal ideation in the multivariate model.
Table 3.
Predictors of lifetime and follow-up adolescent suicidal ideation
| Predictors | Suicidal ideation
|
|||
|---|---|---|---|---|
| Lifetime N=138
|
3-month follow-up N=123
|
|||
| OR | (95 % CI) | OR | (95 % CI) | |
| Lifetime suicidal ideation | – | – | 3.99 | (1.01–15.84)* |
| Age | 0.96 | (0.68–1.35) | 1.73 | (1.01–2.97)* |
| Depressive symptoms | 1.08 | (1.03–1.13)** | 1.15 | (1.06–1.24)*** |
| Pubertal status | 3.94 | (1.03–15.13)* | 0.30 | (0.45–2.05) |
| Impulsiveness | 3.10 | (1.06–9.06)* | 1.33 | (0.30–5.87) |
| Peer stress | 1.11 | (0.55–2.22) | 0.55 | (0.21–1.46) |
| Cortisol groupsa | ||||
| Hyporesponsive | 0.94 | (0.37–2.41) | 4.01 | (0.82–19.76)† |
| Hyperresponsive | 4.98 | (1.38–17.95)* | 16.23 | (2.44–107.94)** |
OR odds ratio, CI confidence interval
Reference group is Normative. Wald tests were χ2 (2)=6.54, p=0.038 and χ2 (2)=8.45, p=0.015, for lifetime suicidal ideation and suicidal ideation at 3-month follow-up, respectively
p<0.10.
p<0.05.
p<0.01.
p<0.001
After accounting for the effects of these predictors, cortisol trajectory membership also was associated uniquely with lifetime suicidal ideation (see Table 3). That is, adolescent females who belonged to the hyperresponsive group were approximately five times more likely to report a lifetime history of suicidal ideation as compared to adolescent females in the normative group. However, adolescents in the hyporesponsive group did not differ from those in the normative group in their likelihood of reporting a lifetime history of suicidal ideation. Additional analyses comparing the hyperresponsive and hyporesponsive groups indicated that females in the hyperresponsive group also were about five times more likely to report a lifetime history of suicidal ideation than females in the hyporesponsive group (OR=5.31, p=0.020, 95 % CI [1.30, 21.65]).
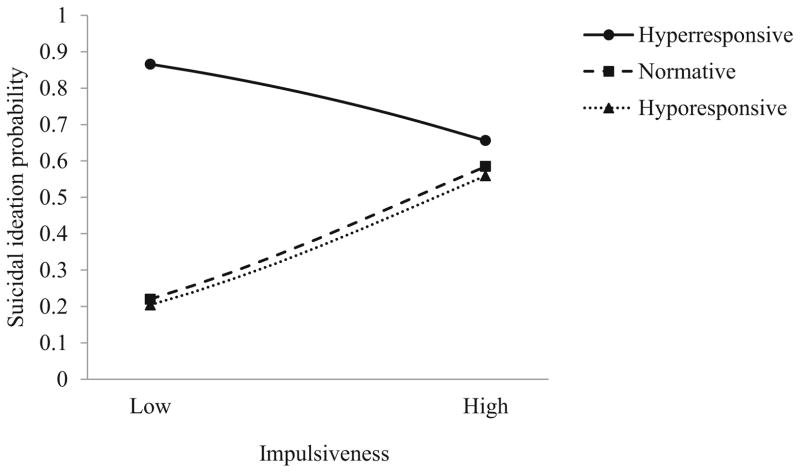
Finally, only the interaction between impulsiveness and cortisol trajectory membership was found to approach significance, Wald test χ2(2)=5.57, p=0.062. To probe this interaction, the effect of impulsiveness on suicidal ideation was examined separately by cortisol trajectory groups (Fig. 2). Among adolescents in the hyporesponsive and normative trajectory groups, a positive effect was revealed between impulsiveness and suicidal ideation (OR=15.20, p=0.063, 95 % CI [0.86, 267.51], and OR= 7.14, p=0.016, 95 % CI [1.45, 35.10], respectively), indicating that higher levels of impulsiveness increased adolescents’ likelihood of reporting a history of suicidal ideation. Conversely, among adolescents in the hyperresponsive group a nonsignificant negative association emerged between impulsiveness and suicidal ideation (OR=0.19, p=0.272, 95 % CI [0.01, 3.77]). Examination of the pattern of effects suggests that adolescents in the hyperresponsive group reported a higher probability of suicidal ideation regardless of their level of impulsiveness, whereas youths with normative or hyporesponsive cortisol responses were very unlikely to report suicidal ideation if they were low in impulsiveness.
Fig. 2.
Interaction effect between cortisol trajectory membership and impulsiveness on the probability of lifetime history of suicidal ideation. Low and High impulsiveness indicate scores one standard deviation below and above the mean, respectively
Follow-up Suicidal Ideation
Results from the logistic regression model predicting suicidal ideation at 3 months post-baseline are presented at the right side of Table 3. Older adolescents and those who reported a lifetime history of suicidal ideation at baseline were more likely to report suicidal ideation at 3 months post-baseline. After controlling for the effect of age and a history of suicidal ideation, only depressive symptoms and cortisol trajectory membership emerged as significant predictors of suicidal ideation at follow-up. Specifically, high levels of depressive symptoms increased adolescents’ probability of reporting suicidal ideation at 3 months post-baseline. Moreover, adolescents in the hyper-responsive group were about 16 times more likely to report suicidal ideation at follow-up than those in the normative group, after controlling for lifetime suicidal ideation. A trend also was found when comparing adolescents in the hyporesponsive and normative groups (p=0.087): as compared to adolescents who showed a normative cortisol pattern to the TSST, those showing a hyporesponsive pattern were about 4 times more likely to report suicidal ideation at follow-up. This suggests there was a non-linear association between HPA responsitivity to acute social stress and risk for subsequent suicidal ideation. No significant difference in the probability of reporting suicidal ideation at follow-up was revealed when comparing adolescents in the hyperresponsive and hyporesponsive trajectory groups (OR = 4.04, p = 0.128, 95 % CI [0.69, 24.50]). Finally, no prospective effects of pubertal status, impulsiveness, and peer stress on suicidal ideation at follow-up were observed. Similarly, no significant interactions between cortisol trajectory membership and any other predictor were revealed.
Discussion
Although suicidal behaviors have been recognized as multi-determined phenomena, adolescent research rarely has examined multiple risk factors for suicidal behaviors across different developmental domains. In particular, prior work has provided limited evidence about the biological risk factors for adolescent suicidal behaviors. In line with a developmental psychopathology perspective (e.g., Cicchetti and Rogosch 2002), the present study applied a multi-level approach to examine (a) the independent associations between HPA-axis stress responses and suicidal ideation and (b) conjoint effects of HPA-axis stress responses and known social-psychological risk factors for suicidal ideation. Associations with lifetime ideation were examined, as were prospective associations with suicidal ideation at 3 months post-baseline, after controlling for prior ideation. Using group-based trajectory modeling, three groups of adolescents showing distinct cortisol responses to a psychosocial stress task were identified (i.e., hyporesponsive, normative and hyperresponsive). As hypothesized, a hyperresponsive cortisol pattern, a more mature pubertal status, as well as high levels of depressive symptoms and impulsiveness, all uniquely differentiated females with a lifetime history of suicidal ideation from those without. Moreover, as compared to females with a normative cortisol response pattern, females showing a hyperreponsive pattern were about 16 times more likely to report suicidal ideation at follow-up, after accounting for lifetime history of suicidal ideation. Intriguingly, a hyporesponsive pattern also was (marginally) associated with a more modestly elevated level of suicidal ideation at follow-up. In addition to cortisol responses, only depressive symptoms increased the likelihood of reporting suicidal ideation at follow-up, and little support for the interplay between cortisol responses and the other risk factors was found.
Overall, results from this study indicate that hyperreactive cortisol responses to stress, more than blunted responses, are associated with increased risk for suicidal ideation among adolescent females, paralleling what has been observed for the relation between depression and HPA responses to stress in adolescents (Guerry and Hastings 2011). These findings are consistent with prior work from the adult literature (Mann et al. 2006) demonstrating that HPA-axis hyperresponsivity – as shown by lower cortisol suppression to the DST –differentiated between psychiatric inpatients who died by suicide from those who did not. However, empirical support for the association between HPA-axis functioning and suicidal behaviors (i.e., attempts and ideation) has been inconsistent within the adult literature (e.g., Jokinen and Nordström 2009; Lindqvist et al. 2008). The present investigation extends this area of research in at least three ways.
First, whereas most prior work examined abnormal HPA-axis functioning by using a pharmacological approach, such as the DST, this study demonstrated the role of HPA-axis regulation by examining cortisol responses to an in vivo psychosocial stress task. Findings from this study thus indicate that the supra-hypothalamic components of the HPA-axis may play a key role in predicting suicidal ideation (Burke et al. 2005). Both the limbic and cortical systems, which include (but are not limited to) the amygdala, hippocampus and pre-frontal cortex, may regulate HPA-axis responses to stress (Hostinar et al. 2014). Specifically, perceived threatening and stressful stimuli activate these brain regions, which, in turn, affect HPA-axis responses. Notably, these brain regions are implicated in emotion regulation processes. Therefore, prevention programs would benefit from incorporating HPA-axis activity into designing emotion regulation strategies in order to improve suicide prevention. In sum, results from this study provide a more complete picture of the physiological processes linking acute stress to suicidal ideation. Second, this study extends findings from the adult literature to a sample of adolescent females, suggesting the intriguing possibility that HPA-axis hyperresponsivity may be a developmentally salient risk factor for suicidal ideation during adolescence. Adolescents may be specifically sensitive to the negative effects of HPA-axis dysregulation due to the normative developmental changes occurring in the brain with the transition to adolescence (Lupien et al. 2009). Prior work has provided some support for this hypothesis, demonstrating that high levels of glucocorticoids in the brain may strongly affect adolescent cognitive functioning (Lupien et al. 2009), thus helping to explain the association between HPA-axis hyperresponsivity and suicidal ideation.
Third, as compared to prior work, the investigation of HPA-axis responses as a predictor of suicidal ideation within a multi-level model, including salient risk factors from different developmental domains, provides important additional information to understand the occurrence of adolescent suicidal ideation. Overall, it is worth noting that all risk factors –with the exception of peer stress – were uniquely associated with lifetime suicidal ideation, replicating findings from previous work (Bridge et al. 2006). Yet, in addition to cortisol responses, only depressive symptoms predicted suicidal ideation at follow-up. These results highlight the challenge of identifying proximal risk factors for suicidal ideation beyond a prior history of ideation. The finding that few baseline risk factors predicted the occurrence of follow-up ideation could be due, at least in part, to study characteristics, including the short-term design (i.e., 3 months follow-up) and the relatively small proportion of participants reporting suicidal ideation at follow-up. However, importantly, the fact that HPA-axis responses and depressive symptoms still emerged as significant predictors, further emphasizes their critical role as proximal risk factors for adolescent suicidal ideation.
More importantly, the effect of HPA-axis on suicidal ideation needs to be interpreted in the context of the effects of the other risk factors. For example, the fact that cortisol responses predicted suicidal ideation above and beyond the effect of pubertal status suggests that developmental changes in HPA-axis stress responses may not be entirely responsible for this effect. This is important given that pubertal development is associated with enhanced HPA-axis reactivity to stress (e.g., Gunnar et al. 2009). Likewise, given the association between psychopathological symptoms and abnormal HPA-axis activity (e.g., Obradović 2012), it is noteworthy that cortisol responses increased risk for suicidal ideation after accounting for depressive symptoms and impulsiveness. Furthermore, the finding that cortisol responses to an acute psychosocial stress-or, rather than peer stress, predicted suicidal ideation suggests that more proximal acute stressful events, and in particular the ways in which adolescents respond to them, may be specifically salient antecedents of adolescent suicidal ideation. Hence, suicidal ideation may represent a maladaptive cognitive and emotional response to regulate the physiological reactivity following acute stressors.
Finding that hyporesponsivity to acute stress marginally predicted subsequent suicidal ideation, but not lifetime ideation, may indirectly support the role of chronic stressors in the etiology of suicidality. Although adverse experiences with peers in the previous 6 months did not predict subsequent suicidal ideation, earlier or more extreme stressors may have played a role in diminished HPA responses. As suggested by allostatic models (e.g., McEwen 2004), HPA-axis hyporesponses may be indicative of allostatic load (i.e., wear-and-tear of organ systems) which likely results from accumulated severe and chronic life experiences of stress often occurring early in life (e.g., parental maltreatment or neglect). These stressors may have long-lasting effects on HPA-axis functioning (Miller et al. 2011), which may begin to pose risks for suicidality only in adolescence, when developmentally salient changes occur (e.g., heightened stress exposure and reactivity). Although the marginally significant trend of this finding demands caution, this interpretation is consistent with neurodevelopmental models of suicide and recent epigenetic work (McGowan et al. 2009; Turecki et al. 2012) suggesting that HPA-axis dysregulation may represent one of the biological pathways underlying the link between social adversities (e.g., early life stress) and the development of suicidal behaviors.
A number of physiological and behavioral pathways may be expected to underlie the effect of HPA-axis responses on suicidal ideation. For example, exaggerated HPA-axis stress responses may increase risk for suicidal ideation by impairing cognitive functions. This notion is supported by parallel research showing that, on one side, high levels of cortisol in the brain – resulting from heightened HPA-axis responses to stress – may alter cognitive performances, such as decision making and problem solving (see Starcke and Brand 2012) and, on the other side, impaired cognitive functioning (e.g., problem solving) is associated with suicidal behaviors, including ideation (e.g., Williams et al. 2005). Furthermore, HPA-axis hyperresponsivity may affect neural activity via regulation of the immune system. Whereas in normal conditions glucocorticoids inhibit inflammatory activity – the main response of the immune system – under conditions of heightened HPA-axis activity the immune system may become insensitive to the effect of glucocorticoids (i.e., glucocorticoid resistance; see Slavich and Irwin 2014). In similar circumstances, high levels of cortisol may increase pro-inflammatory activity, which in turn may affect the serotonergic system (e.g., reduce monoamine availability; Miller et al. 2009). Notably, alterations in the serotonergic system seem to be associated with suicidal behaviors (e.g., Mann 2003). Future research is strongly needed to further elucidate the pathways that connect HPA-axis stress responses and suicidal behaviors, especially during adolescence.
In line with a developmental psychopathology perspective (e.g., Cicchetti and Rogosch 2002), the second goal of this study was to explore the interplay between HPA-axis responses and risk factors from other developmental domains. Contrary to our expectations, findings provided limited support for the interplay between different domains of risk in predicting the occurrence of suicidal ideation. Only the interaction effect between impulsiveness and cortisol responses on lifetime suicidal ideation approached significance. This interaction indicated that impulsiveness was positively associated with a higher probability of reporting a lifetime history of suicidal ideation among females with a normative and hypo-responsive pattern but not a hyperresponsive pattern to stress, for which an overall higher risk for suicidal ideation was observed regardless of adolescents’ level of impulsiveness. Although speculative, it may be the case that high levels of cortisol in the brain affected the dopaminergic and, in particular, serotonergic systems (López et al. 1997), which both underlie impulsive behavior (Dalley and Roiser 2012). Thus, even among females who perceived themselves as less impulsive, high levels of cortisol responses to stress may have increased behavioral dysregulation by activating these neural systems. However, due to the marginally significant effect and the lack of data examining neural processes in this specific study, caution should be used in interpreting these findings.
To date, very few studies have investigated the interplay between biological factors in general, and HPA-axis stress responses in particular, and other risk factors from different domains in predicting adolescent suicidal behaviors. Although this first attempt did not yield empirical support for the hypothesized effects, the examination of multi-level models of risk will deserve further attention. For example, examining the dynamic transactional effects that occur between risk factors from different developmental domains may be a particularly fruitful next step to better elucidate the developmental course of suicidal ideation.
Further, the findings of this study could be seen as supporting cumulative risk models of psychopathology (e.g., Prinstein et al. 2001). Almost all of the identified risk factors for adolescent suicidal ideation were significantly associated with the lifetime occurrence of ideation, making unique and additive contributions to youths’ likelihood of contemplating suicide. The additive effects of risk factors from different developmental domains still empirically support multi-level models of risk for understanding the etiology of suicidal behaviors. In other words, the cumulative presence of risk factors from multiple developmental systems may help to identify adolescents at risk for suicidal ideation.
Although this study has several strengths, including the prospective design, the examination of multiple levels of risk, and the sophisticated analytic approach to examining cortisol responses to stress, findings must be interpreted in light of a number of limitations. First, since the sample included only adolescent females at risk for engaging in suicidal behaviors, results cannot be generalized to males and to the general adolescent population. Second, this study exclusively focused on suicidal ideation; therefore, it remains unclear whether findings similarly would apply to suicidal behaviors, such as attempts. Although based on our findings and prior theoretical and empirical work it seems likely that results, especially the effect of HPA-axis responses, may equally extend to suicide attempts, the low percentage of participants attempting suicide in our sample prevented us from directly testing this hypothesis. Third, the use of self-report measures to assess several of the predictors may have affected the study findings. For instance, because participants with higher depressive symptoms tend to overestimate their levels of peer stress (e.g., De Los Reyes and Prinstein 2004), the lack of effect of peer stress on suicidal ideation may be due in part to shared-method variance between self-reported depressive symptoms and peer stress. Future research is warranted using multi-method approaches, including multi-informant reports of depressive symptoms, objective measures of stress, and behavioral or biological measures of impulsiveness. Finally, it should be acknowledged that, although in line with most studies examining physiological responses to stress, the sample size may have limited the power to identify interaction effects between predictors.
Despite these limitations, this study is among the first examining biological risk factors for adolescent suicidal ideation within a multi-level model, attempting to explore the complex interplay between different domains of risk. Findings yield strong support for the role of HPA-axis hyperresponsivity to stress as risk factor for the occurrence of suicidal ideation among adolescent females. Future research examining risk factors from multiple-level of analysis is necessary to better understand youth suicidal behaviors and elucidate the cognitive, physiological and behavioral pathways leading to the development of suicidal behaviors during adolescence.
Acknowledgments
This work was supported in part by a grant from the National Institute of Mental Health (R01-MH085505). Correspondence concerning this article should be addressed to Matteo Giletta or Mitch Prinstein, Department of Psychology, University of North Carolina at Chapel Hill, Davie Hall, Campus Box 3270, Chapel Hill, NC 27599.
Footnotes
Clinical scores were identified by calculating appropriate female and age normed T-scores. T-scores equal or higher than 70 indicated clinically relevant scores (Reynolds and Kamphaus 1992).
Group-based trajectory models also were conducted controlling for psy-chotropic medication usage, in addition to birth control and corticosteroids. Although these models supported a four-class solution over a three-class solution, logistic regression models examining the effect of cortisol trajectory membership on suicidal ideation provided identical results, with increased risk for suicidal ideation among adolescents in the hyperresponsive group as compared to adolescents in the other cortisol groups
To ensure that the exclusion of pre-task cortisol data collected using the passive drool saliva procedure (see Measures) did not bias results, additional group-based trajectory models were conducted including in the analyses pre-task cortisol data collected using the passive drool saliva procedure. High similar results emerged as when excluding these pre-task cortisol values. Specifically, a three-class trajectory model was supported, including a normative, a hyporesponsive and a hyperresponsive group. These cortisol groups showed identical patterns to those depicted in Fig. 1. Moreover, 137 of the 138 participants were found to belong to the same cortisol trajectory group when estimating models with and without these cortisol values. Despite the similarity across results, models estimated with pre-task cortisol assessed via passive drool procedure as missing are presented as primary analyses, due to significant differences in cortisol concentration that can emerge by using different methods of saliva collection (i.e., salivette vs. passive drool; Poll et al. 2007).
In this study, the relatively broad age range, including participants between 12 and 16 years, was not ideal for examining the effect of pubertal timing (i.e., pubertal status adjusted by chronological age). However, it should be acknowledged that pubertal timing also may be a relevant predictor of adolescent suicidal ideation (see Wichstrøm 2000). To explore this hypothesis, additional models were estimated in which the effect of pubertal status on suicidal ideation (lifetime and at follow-up) was replaced by pubertal timing. Like pubertal status, pubertal timing predicted lifetime suicidal ideation (OR=1.71, p=0.046, 95 % CI [1.01, 2.90]), suggesting that early maturing females were more likely to report a lifetime history of suicidal ideation as compared to their peers. However, as pubertal status, no effect of pubertal timing was found on suicidal ideation at follow-up (OR=0.63, p=0.220, 95 % CI [0.30, 1.32]).
Conflict of Interest The authors declare that they have no conflict of interest.
Contributor Information
Matteo Giletta, Email: giletta@live.unc.edu, Department of Psychology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Casey D. Calhoun, Department of Psychology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Paul D. Hastings, Department of Psychology, University of California, Davis, CA, USA
Karen D. Rudolph, Department of Psychology, University of Illinois, Urbana Champaign, IL, USA
Matthew K. Nock, Department of Psychology, Harvard University, Cambridge, MA, USA
Mitchell J. Prinstein, Email: mitch.prinstein@unc.edu, Department of Psychology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
References
- Bearman PS, Moody J. Suicide and friendships among American adolescents. American Journal of Public Health. 2004;94:89–95. doi: 10.2105/ajph.94.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatrica Scandinavica. 2006;113:180–206. doi: 10.1111/j.1600-0447.2005.00702.x. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Burke HM, Davis MC, Otte C, Mohr DC. Depression and cortisol responses to psychological stress: a meta-analysis. Psychoneuroendocrinology. 2005;30:846–856. doi: 10.1016/j.psyneuen.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Calhoun CD, Franklin JC, Adelman CB, Guerry JD, Hastings PD, Nock MK, et al. Biological and cognitive responses to an in vivo interpersonal stressor: longitudinal associations with adolescent depression. International Journal of Cognitive Therapy. 2012;5:283–299. [Google Scholar]
- Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System (WISQARS) 2010 Retrieved from http://webappa.cdc.gov/sasweb/ncipc/leadcaus10_us.html.
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology. 2002;70:6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- Conley CS, Rudolph KD, Bryant FB. Explaining the longitudinal association between puberty and depression: sex differences in the mediating effects of peer stress. Development and Psychopathology. 2012;24:691–701. doi: 10.1017/S0954579412000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27:726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- Dalley JW, Roiser JP. Dopamine, serotonin and impulsivity. Neuroscience. 2012;215:42–58. doi: 10.1016/j.neuroscience.2012.03.065. [DOI] [PubMed] [Google Scholar]
- Daviss WB, Birmaher B, Melhem NA, Axelson DA, Michaels SM, Brent DA. Criterion validity of the mood and feelings questionnaire for depressive episodes in clinic and non–clinic subjects. Journal of Child Psychology and Psychiatry. 2006;47:927–934. doi: 10.1111/j.1469-7610.2006.01646.x. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Prinstein MJ. Applying depression-distortion hypotheses to the assessment of peer victimization in adolescents. Journal of Clinical Child and Adolescent Psychology. 2004;33:325–335. doi: 10.1207/s15374424jccp3302_14. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130:355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Duval F, Mokrani MC, Correa H, Bailey P, Valdebenito M, Monreal J, et al. Lack of effect of HPA axis hyperactivity on hormonal responses to d-fenfluramine in major depressed patients: implications for pathogenesis of suicidal behaviour. Psychoneuroendocrinology. 2001;26:521–537. doi: 10.1016/s0306-4530(01)00011-7. [DOI] [PubMed] [Google Scholar]
- Guerry JD, Hastings PD. In search of HPA axis dysregulation in child and adolescent depression. Clinical Child and Family Psychology Review. 2011;14:135–160. doi: 10.1007/s10567-011-0084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar M, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Wewerka S, Frenn K, Long JD, Griggs C. Developmental changes in hypothalamus-pituitary-adrenal activity over the transition to adolescence: normative changes and associations with puberty. Development and Psychopathology. 2009;21:69–85. doi: 10.1017/S0954579409000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heilbron N, Prinstein MJ. Adolescent peer victimization, peer status, suicidal ideation, and nonsuicidal self-injury: examining concurrent and longitudinal associations. Merrill-Palmer Quarterly. 2010;56:388–419. doi: 10.1353/mpq.0.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Sullivan RM, Gunnar MR. Psychobiological mechanisms underlying the social buffering of the hypothalamic–pituitary–adrenocortical axis: a review of animal models and human studies across development. Psychological Bulletin. 2014;140:256–282. doi: 10.1037/a0032671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokinen J, Nordström P. HPA axis hyperactivity and attempted suicide in young adult mood disorder inpatients. Journal of Affective Disorders. 2009;116:117–120. doi: 10.1016/j.jad.2008.10.015. [DOI] [PubMed] [Google Scholar]
- Jollant F, Lawrence NL, Olié E, Guillaume S, Courtet P. The suicidal mind and brain: a review of neuropsychological and neuroimaging studies. World Journal of Biological Psychiatry. 2011;12:319–339. doi: 10.3109/15622975.2011.556200. [DOI] [PubMed] [Google Scholar]
- King CA, Merchant CR. Social and interpersonal factors relating to adolescent suicidality: a review of the literature. Archives of Suicide Research. 2008;12:181–196. doi: 10.1080/13811110802101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, Hellhammer D. The “trier social stress test “—a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28:76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May A. Rethinking impulsivity in suicide. Suicide and Life-Threatening Behavior. 2010;40:612–619. doi: 10.1521/suli.2010.40.6.612. [DOI] [PubMed] [Google Scholar]
- Lindqvist D, Träskman-Bendz L, Vang F. Suicidal intent and the HPA-axis characteristics of suicide attempters with major depressive disorder and adjustment disorders. Archives of Suicide Research. 2008;12:197–207. doi: 10.1080/13811110802100775. [DOI] [PubMed] [Google Scholar]
- López JF, Vazquez DM, Chalmers DT, Watson SJ. Regulation of 5–HT receptors and the hypothalamic–pituitary–adrenal axis. Annals of the New York Academy of Sciences. 1997;836:106–134. doi: 10.1111/j.1749-6632.1997.tb52357.x. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, Maheu F, Tu M, Fiocco A, Schramek TE. The effects of stress and stress hormones on human cognition: implications for the field of brain and cognition. Brain and Cognition. 2007;65:209–237. doi: 10.1016/j.bandc.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Mann JJ. Neurobiology of suicidal behaviour. Nature Reviews Neuroscience. 2003;4:819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Currier D, Stanley B, Oquendo MA, Amsel LV, Ellis SP. Can biological tests assist prediction of suicide in mood dis orders? International Journal of Neuro-Psychopharmacology. 2006;9:465–474. doi: 10.1017/S1461145705005687. [DOI] [PubMed] [Google Scholar]
- Mathew SJ, Coplan JD, Goetz RR, Feder A, Greenwald S, Dahl RE, et al. Differentiating depressed adolescent 24 h corti-sol secretion in light of their adult clinical outcome. Neuropsychopharmacology. 2003;28:1336–1343. doi: 10.1038/sj.npp.1300184. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the patho-physiology of psychiatric disorders. Annals of the New York Academy of Sciences. 2004;1032:1–7. doi: 10.1196/annals.1314.001. [DOI] [PubMed] [Google Scholar]
- McGowan PO, Sasaki A, D’Alessio AC, Dymov S, Labonté B, Szyf M, et al. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nature Neuroscience. 2009;12:342–348. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biological Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Muthén & Muthén. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Nagin DS. Group-based modeling of development. Cambridge: Harvard University Press; 2005. [Google Scholar]
- Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. Journal of Consulting and Clinical Psychology. 2007;75:707–715. doi: 10.1037/0022-006X.75.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, Michel BD. Self-injurious thoughts and behaviors interview: development, reliability, and validity in an adolescent sample. Psychological Assessment. 2007;19:309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the national comorbidity survey replication adolescent supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obradović J. How can the study of physiological reactivity contribute to our understanding of adversity and resilience processes in development? Development and Psychopathology. 2012;24:371–387. doi: 10.1017/S0954579412000053. [DOI] [PubMed] [Google Scholar]
- Parker JG, Rubin KH, Erath SA, Wojslawowicz JC, Buskirk AA. Peer relationships, child development, and adjustment: A developmental psychopathology perspective. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology, Vol 1: Theory and method. 2. Hoboken: Wiley; 2006. pp. 419–493. [Google Scholar]
- Petersen AC, Crockett L, Richards M. A self-report measure of pubertal status: reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Poll EM, Kreitschmann-Andermahr I, Langejuergen Y, Stanzel S, Gilsbach JM, Gressner A, et al. Saliva collection method affects predictability of serum cortisol. Clinica Chimica Acta. 2007;382:15–19. doi: 10.1016/j.cca.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, Spirito A. Adolescents’ and their friends’ health-risk behavior: factors that alter or add to peer influence. Journal of Pediatric Psychology. 2001;26:287–298. doi: 10.1093/jpepsy/26.5.287. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of Consulting and Clinical Psychology. 2008;76:92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. BASC: Behavior Assessment System for Children: Manual. Circle Pines: American Guidance Service; 1992. [Google Scholar]
- Rudolph KD. Developmental influences on interpersonal stress generation in depressed youth. Journal of Abnormal Psychology. 2008;117:673–679. doi: 10.1037/0021-843X.117.3.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD. The interpersonal context of adolescent depression. In: Nolen-Hoeksema S, Hilt LM, editors. Handbook of depression in adolescents. New York: Routledge; 2009. pp. 377–418. [Google Scholar]
- Rudolph KD. Puberty as a developmental context of risk for psychopathology. In: Lewis M, Rudolph KD, editors. Handbook of developmental psychopathology. 3. New York: Plenum Press; 2014. pp. 331–354. [Google Scholar]
- Rudolph KD, Kurlakowsky KD, Conley CS. Developmental and social–contextual origins of depressive control-related beliefs and behavior. Cognitive Therapy and Research. 2001;25:447–475. [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21:55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychological Bulletin. 2014;140:774–815. doi: 10.1037/a0035302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sourander A, Helstelä L, Haavisto A, Bergroth L. Suicidal thoughts and attempts among adolescents: a longitudinal 8-year follow-up study. Journal of Affective Disorders. 2001;63:59–66. doi: 10.1016/s0165-0327(00)00158-0. [DOI] [PubMed] [Google Scholar]
- Starcke K, Brand M. Decision making under stress: a selective review. Neuroscience & Biobehavioral Reviews. 2012;36:1228–1248. doi: 10.1016/j.neubiorev.2012.02.003. [DOI] [PubMed] [Google Scholar]
- Turecki G, Ernst C, Jollant F, Labonté B, Mechawar N. The neurodevelopmental origins of suicidal behavior. Trends in Neurosciences. 2012;35:14–23. doi: 10.1016/j.tins.2011.11.008. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite S, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin MJ, Chatham M, Kryzer E, Kertes DA, Gunnar MR. Identifying atypical cortisol patterns in young children: the benefits of group-based trajectory modeling. Psychoneuroendocrinology. 2009;34:50–61. doi: 10.1016/j.psyneuen.2008.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viau V. Functional cross–talk between the hypothalamic–pituitary–gonadal and–adrenal axes. Journal of Neuroendocrinology. 2002;14:506–513. doi: 10.1046/j.1365-2826.2002.00798.x. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Wichstrøm L. Predictors of adolescent suicide attempts: a nationally representative longitudinal study of Norwegian adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:603–610. doi: 10.1097/00004583-200005000-00014. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Barnhofer T, Crane C, Beck AT. Problem solving deteriorates following mood challenge in formerly depressed patients with a history of suicidal ideation. Journal of Abnormal Psychology. 2005;114:421–431. doi: 10.1037/0021-843X.114.3.421. [DOI] [PubMed] [Google Scholar]