Abstract
Background
Former prison inmates experience high rates of hospitalizations and death during the transition from prison to the community, particularly from drug-related causes and early after release. We designed a randomized controlled trial (RCT) of patient navigation to reduce barriers to healthcare and hospitalizations for former prison inmates.
Methods
Forty former prison inmates with a history of drug involvement were recruited and randomized within 15 days after prison release. Participants were randomized to receive three months of patient navigation (PN) with facilitated enrollment into an indigent care discount program (intervention) or facilitated enrollment into an indigent care discount program alone (control). Structured interviews were conducted at baseline, three and six months. Outcomes were measured as a change in self-reported barriers to care and as the rate of health service use per 100 person days.
Results
The mean number of reported barriers to care was reduced at three months and six months in both groups. At six months, the rate of emergency department/urgent care visits per 100 person days since baseline was 1.1 among intervention participants and 0.5 among control participants (p=0.04) whereas the rate of hospitalizations per 100 person days was 0.2 in intervention participants and 0.6 in control participants (p=0.04).
Conclusions
Recruitment of former inmates into an RCT of patient navigation was highly feasible, but follow-up was limited by re-arrests. Results suggest a significantly lower rate of hospitalizations among navigation participants, although the rate of emergency department/ urgent care visits was not improved. Patient navigation is a promising, pragmatic intervention that may be effective at reducing high-cost health care utilization in former prison inmates.
Keywords: Prisoners, vulnerable populations, patient navigation, randomized controlled trials, substance abuse, healthcare utilization
INTRODUCTION
The prison population in the United States is large,1 with a high prevalence of substance use disorders.2 The transition from prison to the community is a vulnerable time for many individuals. A number of international studies have demonstrated high mortality rates among former inmates, particularly within the first two weeks after release and from drug-related causes.3–6 Certain demographic factors, length of incarceration, and type of incarceration and release are associated with the risk of death.7 Rates of emergency department (ED) visits and hospitalization are also elevated after release.8,9 Former inmates suffer discontinuities in treatment for substance use disorders, mental health, and medical conditions, and in medication therapy.10–12 They are thus at risk for decompensating chronic medical conditions and acquiring new medical complications from drug and alcohol use. Effective interventions to improve health outcomes during the transition from prison to the community are needed.
During re-entry, individuals move from the highly structured prison environment into community environments, which may be chaotic and unsupported. Re-entry may be stressful as former inmates try to obtain health care, housing, and employment despite their conviction.13–16 During re-entry, individuals may find it difficult to engage the health care system through appropriate channels, such as primary care. Prior to the Affordable Care Act, most former inmates had limited access to health insurance and means to pay for care. In a qualitative study, many former inmates reported trouble obtaining prescription refills and sought emergency care to meet basic health needs.16 Intensive, tailored support after release has been recommended to assist with this care transition.17,18
Patient navigation is a strategy designed to reduce barriers to care and health disparities for complex patients in the context of their social, economic, and cultural milieu.19–24 Patient navigators are trained, culturally competent health care workers who assist patients with negotiating healthcare systems and accessing quality care.19,25,26 While patient navigators may be professionals, lay navigators are more common, and peers support is generally considered an important facet of patient navigation.25,26
The role of the patient navigator has frequently included connecting patients to resources, streamlining appointments and paperwork, helping patients access financial services, helping patients arrive at scheduled appointments on time and prepared, assuaging patients’ anxiety, and identifying appropriate social services.22,27 Navigators may also assist with transportation, health insurance, health literacy and patient education.28 Psychosocial support is often provided either directly or by referring patients to social workers or counselors. Navigators can help patients make their way through multidisciplinary health care systems, utilize available resources, communicate better with providers, and sustain care over time.23,27
In this study, we designed a patient navigation intervention for the complex transition from prison to the community among drug-involved former inmates. The objective of this study was to test the feasibility of a randomized controlled trial (RCT) of patient navigation to reduce barriers to healthcare and hospitalizations during the transition from prison to the community. We sought to assess the effectiveness of patient navigation with assisted enrollment into an indigent care program compared to assisted enrollement into an indigent care program alone.
METHODS
Study Design
This was a prospective, RCT comparing three months of patient navigation (PN) with facilitated enrollment into an indigent care discount program (intervention) to facilitated enrollment into an indigent care discount program alone (control). The intervention duration was three months and follow-up was conducted at three and six months after enrollment.
Study Setting
Forty individuals were recruited after release from Colorado state prisons. The Colorado Department of Corrections had 11,033 releases in 2010, of which 85% were paroled and 13% were discharged. Women accounted for 13% of releases.29 Recruitment took place at the Denver Community Re-entry Center, a branch of parole that provides support for former inmates living in the community. This program provides employment, housing and other assistance by re-entry specialists, and is not a locked facility. Inmates may be assigned to Community Re-entry or voluntarily seek their services. Linkage to health care services was not a standard part of re-entry services.
Study Population
Drug-involved individuals were recruited between 1 and 15 days after release from prison. Drug-involved was operationalized as release from a sentence for a drug offense or the endorsement of at least three criteria for drug abuse or dependence in the year before prison admission. These criteria were selected because some individuals with significant drug use disorders were not using drugs within the last month due to difficulty obtaining drugs in prison and parole requirements for drug testing. Additional eligibility criteria included ability to understand the study procedures in English, no intention to leave the area for six months, and a phone number or address where they could be contacted. Pregnant women were eligible to participate because the study was minimal risk. Children under 18 were excluded because they are generally released from juvenile facilities. Individuals in a locked halfway house, on “current inmate status,” or with pending jail time in the subsequent six months were ineligible because they were not fully released to the community. Individuals who reported they had a serious mental illness were considered ineligible because they also had access to specialized services offered by the DOC for serious mental illness.
Study staff provided re-entry specialists with information about the study and eligibility criteria during informational sessions. Re-entry specialists referred potential participants to a study staff member. In addition, study staff conducted brief presentations about the study at orientation sessions for individuals recently released from prison. Potential participants could meet with study staff members after the orientation and/or schedule a time for eligibility screening and enrollment. Eligibility screening took place over the phone or in person.
Ethical Considerations
This study was approved by the Colorado Multiple Institutional Review Board (COMIRB) and the Colorado Department of Corrections Research Review Board. We also obtained a Federal Certificate of Confidentiality. Once eligibility was established, study staff members explained study procedures, including randomization, to potential participants, and gave them written consent documents and a Health Insurance Portability and Accountability Act (HIPAA) authorization form to review. Participants had the opportunity to ask questions and consented by signing the consent form.
Participants received compensation of $12.50 (bus tokens) for the baseline visit, a $15.00 grocery gift card for the three month follow-up survey, and a $20.00 grocery gift card for the 6 month follow-up survey. Participants in the navigation arm received $4.50 in bus tokens as compensation for travel to the study site (if necessary).
Instruments
The structured baseline instrument assessed socio-demographic characteristics. Baseline and follow-up instruments included the following measures. Health status, having a personal or health care provider (primary care provider), health problems, and health insurance were assessed using questions from the Behavioral Risk Factor Surveillance System, 2010,30 with a follow-up question on type of insurance (e.g., private, Medicaid, Medicare, VA/Tricare, Indigent Care or Financial Assistance program). Drug use was assessed using questions from the Addiction Severity Index-Lite (ASI-Lite), adapting some questions to refer to the period after release from prison. Recent and current criminal justice involvement were assessed with questions we developed. The instruments assessed the presence of specific barriers to health care and substance abuse services identified in the literature and our prior qualitative work, including no perceived need for treatment, having a job, lack of money for treatment, lack of transportation, childcare, and time, fear of poor treatment by doctors or other providers, too many classes, and low priority for care.16,31,32 Urgent care, ED visits and hospitalizations were assessed by self-report, using questions adapted from a prior study.33,34 Depression symptoms were assessed using the validated Patient Health Questionnaire-9 (PHQ-9).35
Baseline and follow-up instruments were administered in person via interview by a study interviewer. Data were entered and managed using Research Electronic Data Capture (REDCap).36
Randomization Procedures and Timing
After the baseline interview, but prior to randomization, the interviewer scheduled appointments for all participants to meet with an enrollment specialist to enroll in the indigent care discount program. The interviewer then opened an envelope with the random assignment for that participant, provided by the study statistician. This randomized participants to one of two arms: 1) patient navigation plus assistance with enrollment into the indigent care discount program or 2) assistance with enrollment into the indigent care discount program alone.
Intervention arm
Participants in the patient navigation arm received three months of patient navigation plus facilitated enrollment into the Colorado Indigent Care Program (CICP) or the Denver Health Financial Assistance Program (DFAP). CICP is a discount sliding fee program which provides funding to clinics and hospitals so that medical services can be provided at a discount. CICP is not a health insurance program. Eligible individuals must be Colorado residents or migrant farm workers, U.S. citizens or legal immigrants, have income and resources combined at or below 250% of the Federal Poverty Level, and cannot be eligible for Medicaid.
The patient navigator was an employee of the local safety-net community health system and hospital. For intervention participants who were county residents (n=16), the navigator could access electronic medical records, prescription medications lists, verify whether the participant had an assigned primary care provider, and confirm patient appointments (but not schedule them). Participants who were out-of-county residents were navigated to medical clinics where they lived. The patient navigator had a Bachelor of Arts (B.A.), had worked in a jail as a research assistant, demonstrated empathy towards the population, and had experience with incarceration among family members, but no personal history as an inmate. Thus, we considered him a near-peer navigator. He was trained in a formal Patient Navigator Training Program, which included content on assessment, chronic disease, preventive care, and care coordination, and took a public health course on HIV and sexually transmitted infection (STI) prevention and counselling. He assessed the self-reported medical, mental health and substance abuse treatment needs of participants, assisted with coordination of medication refills and patient appointments, provided social support, and provided health education, including HIV and STI prevention counselling. For participants who did not have an established primary care provider, the navigator helped them get on a wait list for primary care appointments, or on a cancellation list, which shortened the wait. He communicated with intervention participants approximately weekly in person and via text messaging and telephone. The navigator was supervised by an expert in patient navigation (E.W.) and a physician (I.B.). All significant contacts with participants were recorded in an electronic significant contact spreadsheet for supervision purposes.
Control arm
Participants in the control arm were referred to the enrollment specialist for facilitated enrollment into CICP or DFAP, similar to the intervention participants. The enrollment specialist provided assistance assessing eligibility and registering individuals for these programs in various community sites. Our team arranged for the enrollment specialist to be based at the re-entry center once a week for a half-day. After enrollment, the research assistant scheduled an appointment with the enrollment specialist for all participants. Selecting this as our control arm was considered ethical by our team, the Department of Corrections Research Review Committee and the prisoner advocate on the Institutional Review Board. Thus, both arms obtained some services above and beyond usual care. From then on, the control arm received care as usual. This included any services normally provided by the Division of Adult Parole or Community Re-entry Center, such as parole supervision, case management, substance abuse classes, or employment training. Former inmates may or may not be required to have drug monitoring through urinalysis, and may be referred to drug and alcohol treatment. Standard services do not typically include medical services, prescription assistance, or medical needs assessment. Parole officers and re-entry specialists do not generally help former inmates navigate the health system and medical care is generally not provided as part of parole, in contrast to prison, where inmates can receive medical services.
Follow-up
Participants in both arms completed three and six month follow-up study visits, during which they were asked about current health care coverage, barriers to health care and substance abuse services, health status, urgent care visits, ED visits and hospitalizations. Participants were eligible for the six month follow-up even if they were incarcerated and not interviewed at three months. We did not conduct follow-up interviews in jail and prison because the focus of this investigation was on navigation to health care in the community. The burden of obtaining approvals from all local jails and prisons for in-facility follow-up was prohibitive for this feasibility study. Structured follow-up interviews included most of the same questions as the baseline.
Analysis
For the baseline participant characteristics, including socio-demographic and criminal justice characteristics, we described proportions for categorical variables, means and standard deviations for continuous variables, and compared between the two intervention groups using chi-square tests, t-tests, or non-parametric tests, as appropriate. For the primary outcome, the change in number of barriers was calculated for each participant, and compared between intervention groups using Wilcoxon tests. The intervention effect was not adjusted for baseline group due to the small sample size. For categorical secondary outcomes, proportions were compared between groups using chi-square tests or Fisher’s exact tests. For continuous secondary outcomes, t-tests or Wilcoxon tests were used for the comparison between groups. Attrition analyses compared those who followed up to those lost to follow-up and examined assumptions about baseline characteristics (i.e., all those who did not follow-up had substantially more barriers). Rates were calculated for the other primary outcome, ED/urgent care visits and hospitalizations per 100 person days since baseline were calculated and compared using a normal approximation. Significance is defined as p<0.05 in all reporting of results. SAS version 9 (SAS Institute, Cary, NC) was used for all analyses.
RESULTS
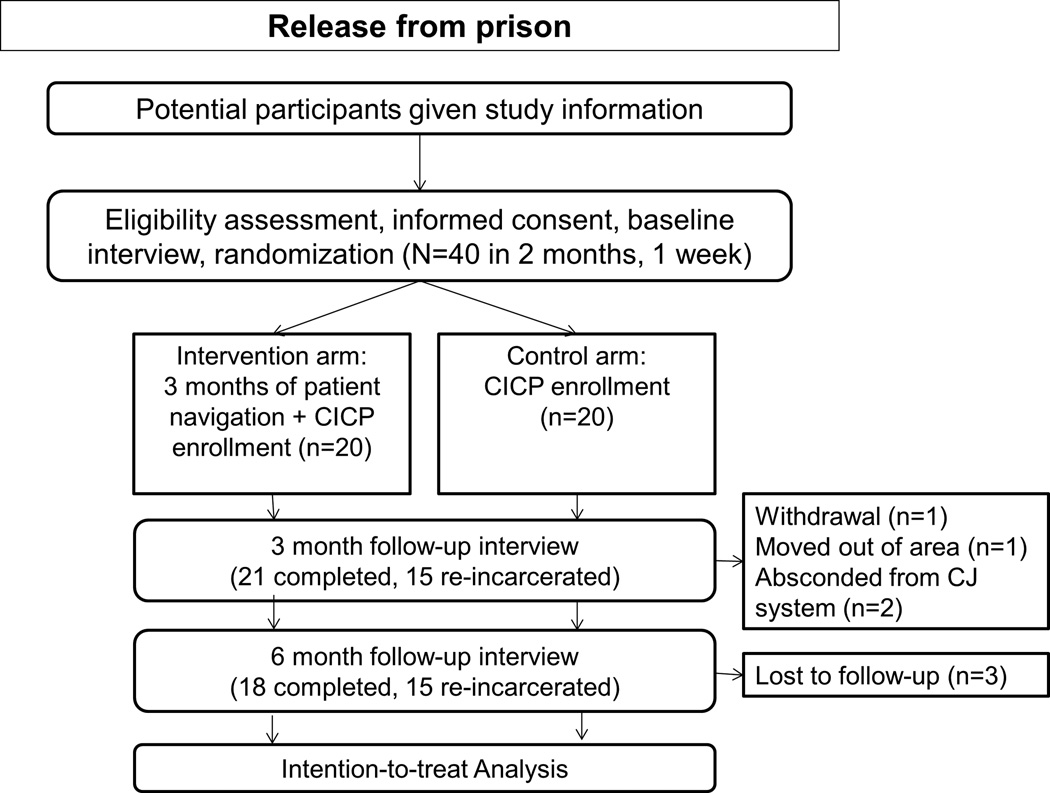
Figure 1 presents the study flow diagram. Forty participants were enrolled between April and June 2011. At three months, 15 were re-incarcerated in jail or prison. At six months, 15 were re-incarcerated and three participants were lost to follow-up. Two individuals who were re-incarcerated at three months completed the six month interview. Two people in the control arm were arrested between the three and six month interviews but still completed both interviews. Thus, we conducted six month interviews with 18 (72%) of those who were not re-incarcerated. Follow-up and re-incarceration was not significantly different by group assignment at three or six months.
Figure 1.
Study flow diagram (CICP=Colorado Indigent Care Program)
There were no significant differences in baseline characteristics between intervention and control groups (Table 1). Participants were enrolled a median of 7 days since release and all but one were on parole. The median age was 42. Overall, 18% were women, 30% reported being Hispanic or Latino, and 18% were African American. Approximately three quarters (77%) were Denver County residents and therefore eligible for primary care in the safety net medical system. The majority (55%) had a history of a drug-related offense. Few (n=2) reporting having Medicaid prior to their incarceration. Only two participants were receiving substance abuse treatment at baseline. One third of participants (34%) reported having hepatitis C and half (50%) reported they were taking prescribed medication for a physical condition or medical problem.
TABLE 1.
Baseline Participant Characteristics and Comparisons between Intervention (Patient Navigation [PN]) and Control Groups
| Baseline Characteristics | Overall (N=40) |
PN (N=20) |
Control (N=20) |
P-value |
|---|---|---|---|---|
| Days since release, mean (SD) | 7.4 (4.2) | 7.1 (4.2) | 7.8 (4.3) | 0.58 |
| On parole, n (%) | 39 (98%) | 20 (100%) | 19 (95%) | >.99a |
| Age (years), mean (SD) | 42.4 (9.1) | 41.6 (9.0) | 43.2 (9.3) | 0.58 |
| Female, n (%) | 7 (18%) | 4 (20%) | 3 (15%) | >.99a |
| Race/Ethnicity, n (%) | ||||
| White | 20 (50%) | 10 (50%) | 10 (50%) | |
| Hispanic/Latino | 12 (30%) | 7 (35%) | 5 (25%) | 0.69 |
| Black/African American American | 7 (18%) | 3 (15%) | 4 (20%) | |
| Indian/Alaska Native | 1 (3%) | 0 (0%) | 1 (5%) | |
| Highest grade completed, n (%) | ||||
| Grade 1 – 8 | 4 (10%) | 1 (5%) | 3 (16%) | |
| Grade 9 – 11 | 4 (10%) | 2 (10%) | 2 (11%) | 0.35b |
| Grade 12 or GED | 22 (56%) | 15 (60%) | 10 (53%) | |
| College 1 – 3 years | 9 (23%) | 5 (25%) | 4 (21%) | |
| County of residence, n (%) | ||||
| Denver | 30 (77%) | 16 (80%) | 14 (74%) | |
| Arapahoe | 2 (5%) | 2 (10%) | 0 (0%) | 0.18 |
| Jefferson | 7 (18%) | 2 (10%) | 5 (26%) | |
| Medicaid before prison, n (%) | 2 (5%) | 0 (0%) | 2 (10%) | 0.49a |
| Ever had a drug offense, n (%) | 22 (55%) | 9 (45%) | 13 (65%) | 0.20 |
| Medical problems (ever had), n (%) | ||||
| Hepatitis C | 13 (34%) | 9 (45%) | 4 (22%) | 0.14 |
| Hepatitis B | 2 (5%) | 1 (5%) | 1 (5%) | >.99a |
| HIV | 1 (3%) | 0 (0%) | 1 (5%) | >.99a |
| Taking prescribed medication for physical problem, n (%) | 20 (50%) | 9 (45%) | 11 (55%) | 0.53 |
| Receiving medicine or treatment for substance abuse, n (%) | 2 (5%) | 0 (0%) | 2 (10%) | 0.49a |
Note. Percentages were calculated based on non-missing cases. Percentage may not total 100% due to rounding. Wilcoxon tests for continuous variables, and chi-square tests for categorical variables were used, except
Fisher’s exact test
Mantel-Haenszel test.
At baseline, few participants (n=4) had any health coverage; only one had private insurance (Table 2). At three and six months, 100% of intervention participants and 90% of control participants had health care coverage, but the difference was not significant by intervention allocation.
TABLE 2.
Health Care Coverage and Barriers to Health Care and Substance Abuse Services Reported by Participants Assigned to the Intervention (Patient Navigation [PN]) and Control Groups at Baseline, Three Months and Six Months (CICP=Colorado Indigent Care Program)
| Baseline | 3 months | 6 months | ||||
|---|---|---|---|---|---|---|
| PN (N=20) |
Control (N=20) |
PN (N=10) |
Control (N=11) |
PN (N=8) |
Control (N=10) |
|
| Health care coverage, n (%) | ||||||
| None | 18 (90%) | 17 (89%)b | 0 (0%) | 1 (9%)b | 0 (0%) | 1 (10%)b |
| CICP | 1 (5%) | 0 (0%) | 10 (100%) | 6 (55%) | 7 (88%) | 5 (50%) |
| VA/Tri care | 1 (5%) | 1 (5%) | 0 (0%) | 1 (9%) | 1 (13%) | 2 (20%) |
| Private | 0 (0%) | 1 (5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Medicaid and/or Medicare | 0 (0%) | 0 (0%) | 0 (0%) | 3 (27%) | 0 (0%) | 2 (20%) |
| Trouble getting medication, n (%) | ||||||
| No trouble/A little | 5 (25%) | 4 (20%) | 4 (40%) | 3 (27%) | 5 (63%) | 5 (50%) |
| A lot | 0 (0%) | 3 (15%) | 0 (0%) | 1 (9%) | 0 (0%) | 0 (0%) |
| Not able to get | 1 (5%) | 1 (5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| N/A or missing | 14 (70%) | 12 (60%) | 6 (60%) | 7 (64%) | 3 (38%) | 5 (50%) |
| Reported any barriers to health care, n (%) | 20 (100%) | 20 (100%) | 7 (70%) | 11 (100%)*b | 4 (50%) | 6 (60%)b |
| Mean number of barriers to health care (SD) | 3.9 (1.8) | 3.9 (2.2) | 2.6 (2.6) | 2.5 (2.3) | 2.4 (3.2) | 2.9 (3.2) |
| Change, mean (SD)a | −1.8 (2.7) | −1.5 (2.4) | −2.0 (2.9) | −0.5 (3.2) | ||
| Specific barriers to health care, n (%) | ||||||
| Money | 19 (95%) | 19 (95%)b | 5 (50%) | 9 (82%)b | 3 (38%) | 5 (50%)b |
| Insurance | 14 (70%) | 17 (89%)b | 3 (30%) | 4 (36%)b | 3 (38%) | 5 (50%)b |
| Transportation | 12 (60%) | 10 (50%) | 6 (60%) | 4 (36%)b | 3 (38%) | 4 (40%)b |
| Knowledge | 9 (45%) | 8 (40%) | 2 (20%) | 1 (9%)b | 1 (13%) | 2 (20%)b |
| Too many classes | 8 (40%) | 6 (30%) | 0 (0%) | 1 (9%)b | 3 38%) | 3 (30%)b |
| Time | 5 (25%) | 3 (15%)b | 3 (30%) | 1 (9%)b | 1 (13%) | 3 (30%)b |
| Low priority | 5 (25%) | 2 (10%)b | 2 (20%) | 2 (18%)b | 0 (0%) | 1 (10%)b |
| Job | 3 (15%) | 3 (16%)b | 4 (40%) | 2 (18%)b | 3 (38%) | 4 (40%)b |
| Childcare | 2 (10%) | 4 (20%)b | 0 (0%) | 1 (9%)b | 0 (0%) | 1 (10%)b |
| Bad experiences | 0 (0%) | 2 (10%)b | 1 (10%) | 2 (18%)b | 1 (13%) | 0 (0%)b |
| Poor treatment | 0 (0%) | 2 (10%)b | 0 (0%) | 0 (0%) | 1 (13%) | 0 (0%)b |
| Reported any barriers to substance abuse services, n (%) | 16 (80%) | 16 (84%)b | 7 (70%) | 11 (100%)*b | 5 (71%) | 7 (70%)b |
| Mean number of barriers to substance abuse services (SD) | 2.6 (2.2) | 3.7 (2.7) | 2.3 (2.7) | 3.1 (2.8) | 2.7 (3.0) | 3.6 (3.3) |
| Change, mean (SD)a | −1.1 (2.4) | −0.9 (3.0) | −0.7 (3.9) | −0.3 (3.7) | ||
| Specific barriers to substance abuse services, n (%) | ||||||
| Money | 9 (45%) | 14 (74%)* | 4 (40%) | 6 (55%) | 2 (25%) | 7 (70%)b |
| Insurance | 8 (40%) | 11 (58%) | 3 (30%) | 3 (27%)b | 3 (43%) | 5 (50%)b |
| Transportation | 9 (45%) | 9 (45%) | 4 (40%) | 3 (27%)b | 3 (38%) | 5 (50%)b |
| Knowledge | 5 (25%) | 7 (35%) | 2 (20%) | 3 (30%)b | 0 (0%) | 2 (20%)b |
| Too many classes | 6 (30%) | 7 (35%) | 0 (0%) | 2 (18%)b | 2 (25%) | 4 (40%)b |
| Time | 3 (15%) | 4 (20%) | 3 (30%) | 3 (27%)b | 1 (13%) | 3 (30%)b |
| Low priority | 6 (30%) | 8 (40%) | 3 (30%) | 4 (36%)b | 3 (38%) | 2 (20%)b |
| Job | 3 (15%) | 3 (15%)b | 2 (20%) | 1 (9%)b | 3 (38%) | 4 (40%)b |
| Childcare | 1 (5%) | 1 (5%) | 0 (0%) | 1 (9%)b | 0 (0%) | 0 (0%) |
| Bad experiences | 1 (5%) | 4 (20%)b | 2 (20%) | 3 (27%)b | 1 (13%) | 1 (10%)b |
| Poor treatment | 0 (0%) | 3 (15%)b | 0 (0%) | 1 (9%)b | 1 (13%) | 0 (0%)b |
Note.
p<0.1;
Percentages were calculated based on non-missing cases. Percentage may not total 100% due to rounding.
Changes from baseline were compared. Wilcoxon tests for continuous variables, and chi-square tests for categorical variables were used, except
Fisher’s exact test
Mantel-Haenszel test
At baseline, all participants reported barriers to health care. Fewer individuals reported any barriers to health care at three months in the intervention arm than in the control arm (p=0.09). We observed reductions in the mean number of barriers to health care in both control and intervention arms at three and six months. Although both groups had the same number of participants with any barrier to substance abuse services at baseline (n=16), fewer individuals reported any barriers at three months (p=0.09). We observed reductions in mean number of barriers to substance abuse services in both groups at both time points.
In terms of risk behaviors, smoking was the most common risk behavior reported by participants, followed by unprotected sex. We found no significant differences between groups in drug use, drug injection, tobacco use, or alcohol use to intoxication, but more people in the control arm reported unprotected sex at three months than in the intervention arm (p=0.07; Table 3).
TABLE 3.
Health Risk Behaviors Reported by Participants Assigned to the Intervention (PN) and Control Groups at Baseline, Three Months and Six Months
| Baseline | 3 months | 6 months | ||||
|---|---|---|---|---|---|---|
| PN (N=20) |
Control (N=20) |
PN (N=10) |
Control (N=11) |
PN (N=8) |
Control (N=10) |
|
| Used injection drugs | 0 (0%) | 0 (0%) | 0 (0%) | 1 (10%)a | 0 (0%) | 0 (0%) |
| Used drugs | 2 (10%) | 0 (0%) | 1 (10%) | 2 (18%) | 1 (13%) | 2 (20%) |
| Smoking | 11 (55%) | 12 (60%) | 7 (70%) | 7 (64%)a | 7 (88%) | 6 (60%)a |
| Alcohol use to intoxication | 0 (0%) | 0 (0%) | 0 (0%) | 1 (9%)a | 1 (13%) | 3 (30%)a |
| Unprotected sex | 2 (12%) | 6 (38%)a | 1 (13%) | 6 (60%)*a | 5 (63%) | 4 (40%)a |
Note.
p <0.1;
Percentages were calculated based on non-missing cases. Percentage may not total 100% due to rounding. Chi-square tests were used, except
Fisher’s exact test
Table 4 describes health status and health care utilization reported by participants at baseline, three months and six months. There was no statistically significant difference in the change in number of days physical or mental health were not good among intervention and control arms at three and six months. Several individuals had a high number of days with poor physical health, which skewed the data. Few participants had a primary care provider at baseline, and the number reporting a primary care provider at three and six months increased in both intervention and control arms. Both groups experienced increases in receipt of treatment for medical conditions.
TABLE 4.
Health Status and Health Care Utilization Reported by Participants Assigned to the Intervention (PN) and Control Groups at Baseline, Three Months and Six Months
| Baseline | 3 months | 6 months | ||||
|---|---|---|---|---|---|---|
| PN (N=20) |
Control (N=20) |
PN (N=10) |
Control (N=11) |
PN (N=8) |
Control (N=10) |
|
| Days physical health not good in last 30 days, mean (SD) | 8.7 (14.5) | 13.2 (13.5) | 6.0 (9.5) | 14.5 (13.1) | 9.0 (11.4) | 8.8 (12.7) |
| Change, mean (SD)a1 | 1.3 (10.7) | −1.1 (14.2) | 0.3 (7.5) | −2.3 (13.3) | ||
| Days mental health not good in last 30 days, mean (SD) | 10.3 (8.6) | 11.2 (12.9) | 6.7 (10.1) | 13.6 (13.8) | 7.5 (8.5) | 8.6 (10.2) |
| Change, mean (SD)a1 | −0.3 (14.4) | 4.1 (13.6) | 2.5 (7.1) | 1.1 (9.4) | ||
| Have primary care provider, n (%) | 0 (0%) | 2 (11%)b | 3 (30%) | 5 (50%)b | 4 (50%) | 6 (60%)b |
| Now receiving treatment for medical condition, n (%) | 0 (0%) | 1 (5%)b | 3 (30%) | 3 (30%)b | 5 (63%) | 4 (40%)b |
| Any ED/urgent care visit, n (%)a2 | 1 (5%) | 1 (5%)b | 7 (70%) | 7 (64%)b | 8 (100%) | 6 (60%)*b |
| ED/urgent care visits, rate per 100 daysa2 | 1.4 | 0.6c | 1.1 | 0.7c | 1.1 | 0.5**c |
| Any hospitalization, n (%)a2 | 1 (5%) | 0 (0%)b | 1 (10%) | 3 (27%)b | 3 (38%) | 4 (40%)b |
| Hospitalizations, rate per 100 daysa2 | 1.4 | 0.0c | 0.1 | 0.7**c | 0.2 | 0.6**c |
Note.
0.05<=p<0.1
p<0.05;
Percentages were calculated based on non-missing cases. Percentage may not total 100% due to rounding.
Changes from baseline were compared, and a2time periods considered were “since release” for baseline and “since baseline interview” for 3 and 6 months. Wilcoxon tests for continuous variables, and chi-square tests for categorical variables were used, except
Fisher’s exact test
Z-test
Differences were observed at three and six months in high-intensity health service utilization (Table 4). At six months, the rate of ED/urgent care visits since baseline was significantly higher (1.1 per 100 person-days) among participants in the intervention arm than in the control arm (0.5 per 100 person-days; p=0.04). At three months, the rate of hospitalizations since baseline in intervention participants (0.1 per 100 person days) was significantly lower than among control participants (0.7 per 100 person-days; p=0.02). This difference persisted at six months (intervention group [since baseline]: 0.2 per 100 person days; control group: 0.6 per 100 person-days; p=0.04).
DISCUSSION
Our study demonstrates the feasibility of a randomized trial of patient navigation with former inmates in the early post-release period. We observed a decrease in the number of barriers to health care and a significantly lower rate of hospitalizations among patient navigation participants at three and six months compared with facilitated enrollment indigent care discount program alone. These findings support the potential benefits of patient navigation for drug-involved individuals transitioning from prison to the community.
We also observed increased ED/urgent care visits among participants in the patient navigation arm. In the context of reduced hospitalizations, this finding does not undermine the potential benefit of this intervention. During the conduct of this study, the safety net health system had a three month wait-list for new patient primary care appointments. The navigator encouraged participants on chronic medications to go to urgent care to obtain refills to maximize continuity of medication therapy while awaiting a primary care visit. This practice may have accounted for the increased ED/urgent care visits observed in the patient navigation arm.
Our intervention feasibility work suggests that our method of recruitment of former inmates into a RCT of patient navigation during the immediate post-release period was efficient and feasible. This study involved a productive collaboration between an academic medical center, the Department of Corrections, parole and the local safety net medical system. However, recruitment at the Re-entry Center and receipt of referrals from re-entry specialists may have prevented some participants from enrolling due to lack of trust and limited the generalizability of our results. This affiliation may also have limited our ability to follow-up with patients who absconded. The navigator was an employee of the safety net medical center, which was critical to ensuring access to patient records, including medications and appointment times. Using a peer navigator with a personal history of incarceration or based in a different setting may have resulted in different enrollment, follow-up, and results.
Given the high proportion of repeat incarcerations, future studies should consider arranging approvals for research follow-up in local jails and prisons. A future larger scale intervention should also allow for repeated episodes of navigation to accommodate the real-world problem of multiple transitions through the criminal justice system.
Both arms of this study included an intervention not routinely provided during the re-entry process: facilitated eligibility screening for and enrollment into a Colorado-specific indigent care program. Our study team and research review boards considered it most ethical to provide some services to the control group given the vulnerabilty of this popualtion. With health care reform, approximately one third of former inmates could become eligible for Medicaid,37 but it is unlikely this change will eliminate wait times to establish primary care, the potential benefit of patient navigation, or need for assistance with health insurance enrollment. Our study occurred in a real-world setting with limited access to care for all uninsured patients, in which concerns about equity did not permit us to manipulate wait-lists or establish a special access clinic for the benefit of our intervention participants.
Patient navigation is a promising intervention to improve health outcomes in former inmates. Further research is needed if this intervention could reduce patient-centered outcomes, overdose, deaths and costs of medical care and other services.
ACKNOWLEDGEMENTS
We wish to acknowledge Heather Salazar, Maureen O’Keefe, Sue Felton, Heather Wells, John Steiner, MD, MPH, Jean Kutner, MD, MSPH, Faye S. Taxman, PhD, and William Henderson, PhD, MPH.
FUNDING
This study was supported by the Robert Wood Johnson Physician Faculty Scholars Program and grant number K12HS019464 from the Agency for Healthcare Research and Quality. This study was also supported by NIH/NCRR Colorado CTSI Grant Number UL1 TR000154. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Robert Wood Johnson Foundation, NIH, or the Agency for Healthcare Research and Quality.
Footnotes
AUTHOR CONTRIBUTIONS
IA Binswanger conceived and designed the study, obtained funding for the study, interpreted the data, wrote and revised the manuscript. E Whitley contributed to the design of the study and supervised the intervention. PR Haffey and SR Mueller collected the data. SJ Min analyzed the data.
REFERENCES
- 1.Glaze LE, Herberman EJ. Correctional Populations in the United States, 2012. Washington, DC: Bureau of Justice Statistics, U.S. Department of Justice; 2013. [Google Scholar]
- 2.Mumola CJ, Karberg JC, et al. Drug use and dependence, state and federal prisoners, 2004. Washington, D.C: U.S. Dept. of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2006. [Google Scholar]
- 3.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison--a high risk of death for former inmates. N. Engl. J. Med. 2007 Jan 11;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merrall EL, Kariminia A, Binswanger IA, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010 Sep;105(9):1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kariminia A, Butler TG, Corben SP, et al. Extreme cause-specific mortality in a cohort of adult prisoners--1988 to 2002: a data-linkage study. Int. J. Epidemiol. 2006 Apr;36(2):310–316. doi: 10.1093/ije/dyl225. [DOI] [PubMed] [Google Scholar]
- 6.Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996–99. Addiction. 2003 Feb;98(2):185–190. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- 7.Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013 Nov 5;159(9):592–600. doi: 10.7326/0003-4819-159-9-201311050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frank JW, Andrews CM, Green TC, Samuels AM, Trinh TT, Friedmann PD. Emergency department utilization among recently released prisoners: a retrospective cohort study. BMC Emerg Med. 2013;13:16. doi: 10.1186/1471-227X-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang EA, Wang Y, Krumholz HM. A high risk of hospitalization following release from correctional facilities in Medicare beneficiaries: a retrospective matched cohort study, 2002 to 2010. JAMA Intern Med. 2013 Sep 23;173(17):1621–1628. doi: 10.1001/jamainternmed.2013.9008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baillargeon J, Giordano TP, Rich JD, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009 Feb 25;301(8):848–857. doi: 10.1001/jama.2009.202. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public Health Implications for Adequate Transitional Care for HIV-Infected Prisoners: Five Essential Components. Clin. Infect. Dis. 2011 Sep;53(5):469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallik-Kane K, Visher CA. Health and Prisoner Reentry: How Physical, Mental, and Substance Abuse Conditions Shape the Process of Reintegration. Washington, DC: Urban Institute, Justice Policy Center; 2008. Feb, [Google Scholar]
- 13.Iguchi MY, London JA, Forge NG, Hickman L, Fain T, Riehman K. Elements of well-being affected by criminalizing the drug user. Public Health Rep. 2002;117(Suppl 1):S146–S150. [PMC free article] [PubMed] [Google Scholar]
- 14.Petersilia J. When Prisoners Come Home: Parole and Prisoner Reentry (Studies in Crime and Public Policy) New York: Oxford University Press; 2003. [Google Scholar]
- 15.La Vigne NG VC, Castro J. Chicago Prisoners' Experiences Returning Home. Washington, DC: The Urban Institute; 2004. [Google Scholar]
- 16.Binswanger IA, Nowels C, Corsi KF, et al. "From the prison door right to the sidewalk, everything went downhill," a qualitative study of the health experiences of recently released inmates. Int. J. Law Psychiatry. 2011 Jul-Aug;34(4):249–255. doi: 10.1016/j.ijlp.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Burgess-Allen J, Langlois M, Whittaker P. The health needs of ex-prisoners, implications for successful resettlement: A qualitative study. International Journal of Prisoner Health. 2006;2(4):291–301. [Google Scholar]
- 18.Wang EA, Hong CS, Samuels L, Shavit S, Sanders R, Kushel M. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public Health Rep. 2010 Mar-Apr;125(2):171–177. doi: 10.1177/003335491012500205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Psooy BJ, Schreuer D, Borgaonkar J, Caines JS. Patient navigation: improving timeliness in the diagnosis of breast abnormalities. Can Assoc Radiol J. 2004 Jun;55(3):145–150. [PubMed] [Google Scholar]
- 20.Freeman HP. Patient navigation: a community based strategy to reduce cancer disparities. J Urban Health. 2006 Mar;83(2):139–141. doi: 10.1007/s11524-006-9030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips CE, Rothstein JD, Beaver K, Sherman BJ, Freund KM, Battaglia TA. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med. 2011 Feb;26(2):123–129. doi: 10.1007/s11606-010-1527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008 Oct 15;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bradford JB, Coleman S, Cunningham W. HIV System Navigation: an emerging model to improve HIV care access. AIDS Patient Care STDS. 2007;21(Suppl 1):S49–S58. doi: 10.1089/apc.2007.9987. [DOI] [PubMed] [Google Scholar]
- 24.Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer practice. 1995 Jan-Feb;3(1):19–30. [PubMed] [Google Scholar]
- 25.Hardy CM, Wynn TA, Huckaby F, Lisovicz N, White-Johnson F. African American community health advisors trained as research partners: recruitment and training. Fam Community Health. 2005 Jan-Mar;28(1):28–40. doi: 10.1097/00003727-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Johnson RE, Green BL, Anderson-Lewis C, Wynn TA. Community Health Advisors as Research Partners: An Evaluation of the Training and Activities. Family & Community Health. 2005;28(1):41–50. doi: 10.1097/00003727-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer. 2005 Aug 15;104(4):848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 28.Cherrington A, Ayala GX, Amick H, Allison J, Corbie-Smith G, Scarinci I. Implementing the community health worker model within diabetes management: challenges and lessons learned from programs across the United States. Diabetes Educ. 2008 Sep-Oct;34(5):824–833. doi: 10.1177/0145721708323643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barr BL, Gilbert CR, O'Keefe M. Statistical Report: Fiscal Year 2010. Colorado Springs: Colorado Department of Corrections; 2011. [Google Scholar]
- 30.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. Altanta, Georgia: U.S. Department of Health and Human Services; 2010. [Google Scholar]
- 31.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am. J. Public Health. 1997 Feb;87(2):217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seid M, Opipari-Arrigan L, Gelhard LR, Varni JW, Driscoll K. Barriers to care questionnaire: reliability, validity, and responsiveness to change among parents of children with asthma. Acad Pediatr. 2009 Mar-Apr;9(2):106–113. doi: 10.1016/j.acap.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 33.Takahashi TA, Baernstein A, Binswanger I, Bradley K, Merrill JO. Predictors of hospitalization for injection drug users seeking care for soft tissue infections. J. Gen. Intern. Med. 2007 Mar;22(3):382–388. doi: 10.1007/s11606-006-0079-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Binswanger IA, Takahashi TA, Bradley K, Dellit TH, Benton KL, Merrill JO. Drug users seeking emergency care for soft tissue infection at high risk for subsequent hospitalization and death. J Stud Alcohol Drugs. 2008 Nov;69(6):924–932. doi: 10.15288/jsad.2008.69.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cuellar AE, Cheema J. As Roughly 700,000 Prisoners Are Released Annually, About Half Will Gain Health Coverage And Care Under Federal Laws. Health Aff. (Millwood) 2012 May 1;31(5):931–938. doi: 10.1377/hlthaff.2011.0501. 2012. [DOI] [PubMed] [Google Scholar]