Abstract
Objectives
Existing studies of disparities in access to oral health care for underserved populations often focus on supply measures such as number of dentist. This approach overlooks the importance of other aspects of dental care delivery system such as personal and practice characteristics of dentists that determine the capacity to provide care. This study aims to assess the role of such characteristics in access to care of underserved populations.
Methods
We merged the 2003 California Health Interview Survey and a 2003 survey of California dentists at the Medical Study Service Areas (MSSA). We examined the role of overall supply and other characteristics of dentists in income and racial/ethnic disparities in access, which was measured by annual dental visits and unmet need for dental care due to costs.
Results
We found that some characteristics including higher proportion of dentists who were older, white, busy or overworked, and did not accept public insurance or discounted fees in the MSSA inhibited access for low income and minority populations.
Conclusions
These findings highlight the importance of monitoring characteristics of dentists in addition to traditional measures of supply such as licensed dentist to population ratios. The findings identify specific aspects of the delivery system such as dentists’ participation in Medicaid, provision of discounted care, busyness, age, race/ethnicity, and gender should be regularly monitored. These data will provide a better understanding of how the dental delivery system is organized and how this knowledge can be used to develop more narrowly targeted policies to alleviate disparities.
Oral disease is a significant health problem in the U.S. and the burden of oral disease falls more heavily on the poor and racial/ethnic minorities who have less access to oral health care.(1, 2) These populations experience disparities in access to dental care, including fewer dentist visits, and this lower utilization has been linked to poorer oral health.(2–4) Disparities are partly due to lack of dental insurance, leading to policies to promote access by providing public insurance and directing federal funds to low-cost providers in dental health shortage areas. Yet, difficulties in access to care for the underserved exist due to the inadequacies of the dental care delivery system.(2, 5, 6)
Efforts to improve access often focus on increasing supply of providers, frequently measured as presence of licensed dentists in an area.(7, 8) These efforts are based on the assumption that availability of more dentists will increase access to dental care for everyone. But general supply measures fall short of evaluating the true capacity for providing dental care to the underserved. A comprehensive evaluation should examine characteristics such as part-time employment, size of staff and operatories, accepting public coverage or reduced fees, or multilingual practices. The dearth of such information hinders the development of more effective policies to address systemic barriers that lead to racial/ethnic disparities.
Studies of the role of supply using limited licensure or professional association membership data provide a broad overview of supply but lack sufficient detail.(7) Other studies of the role of dental care delivery system in access are slowly emerging. Dental health professional shortage areas are designated based on age of the dentist, the number of hours the dentist works (full-time equivalent or FTE), and the number of allied personnel in the practice.(9) Two studies have indicated that dentists’ characteristics were linked to provision of care to publicly insured patients. Specifically, dentists who were less busy, pediatrician, African American, or Latino were more likely to see Medicaid patients, but dentists who were non-solo, female, and older were less likely to do so.(10, 11) Another study found that bilingual/multilingual capacity in practice, acceptance of discounted fees, multiple practice locations, shorter appointment times, and provision of more operative, periodontic, and surgical care were positively associated with dentists’ provision of care to publicly insured patients.(5) However, few available studies have directly assessed the role of the dental delivery system as measured by a broad range of dentist characteristics on access to care in general and on disparities in access to care in particular.
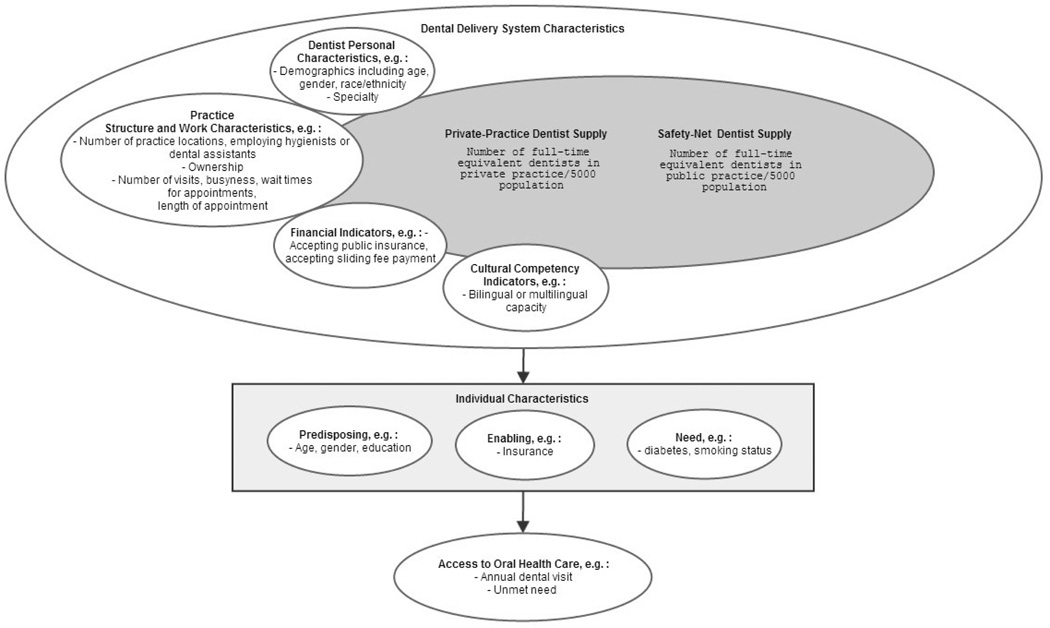
We developed an analytic framework (Figure 1) to examine the role of the dental care delivery system in disparities in access to dental care. This framework complements Andersen’s conceptual framework by developing the contextual indicators of access to care (12) and builds on another framework to identify indicators of service provision by dentists.(13) In this study, we propose that overall measures of supply of dental care include the safety net and private practice dentist supply (e.g., the ratio of full-time equivalent dentists per 5,000 population in private and safety net settings). The capacity for providing care in private practice further consists of personal characteristics of dentists (e.g., sex, years in practice), their practice structure and work characteristics (e.g., number of dental assistants, how busy), financial indicators (e.g., payer source), and cultural competency (e.g., non-English capacity). Access to oral health in general, and for underserved populations in particular, is determined by overall supply and capacity in the private setting, but these effects are modified by population’s characteristics including predisposing, enabling, and the level of need. In our analyses, we anticipated that access is promoted with more public and private practice dentists per 5,000 population. Also, more dentists who accept discounted fees or publicly insured patients, or are multilingual promote access, particularly for the underserved. Alternatively, access in inhibited when dentists are older, newly graduated, female, specialist, white, not busy or overworked or have smaller practices (no hygienists, fewer dental assistants, fewer visits, longer wait times, longer appointment time per visit) or multiple locations. We examined if these effects differed by race/ethnicity and income.
Figure 1.
The framework for assessing the role of dental care delivery system on access to care overall and for underserved populations
Source: Developed by authors
Methods
Sample and Data
We used data on the civilian non-institutionalized adult population in California from the 2003 California Health Interview Survey (CHIS), a statewide and nationally used health survey.(14, 15) CHIS (60% adult response rate) is geocoded to allow for merging of external variables at the geographic unit of interest, is conducted in Spanish and multiple Asian languages, and is the largest source of data on limited English proficient populations nationally. Data on private practice dentists was obtained from the 2003 California Dentist Survey, a representative survey of California dentists in private practice conducted by authors. The sample included 4,400 completed surveys with an overall unadjusted response rate of 31% and an adjusted response rate of 46% discounting ineligible, not-locatable, and unknown eligibility.(13, 16) Eligible dentists were actively practicing in dentist-owned private practices and were not public health dentists or oral and maxillofacial surgeons, pathologists, or radiologists. CDS data was weighted to account for sampling design and non-response.(17) The primary practice location of each dentist in CDS was geocoded at the Medical Study Service Area (MSSA). MSSAs are designated by the California Office of Statewide Health Planning and Development (OSHPD) after each decadal census. MSSAs include one or more complete census tracts, are confined within county lines, and are recognized by the U.S. Public Health Service as a rational service area for providing primary health care services.(18)
Data on size of the population and percentage who were white were obtained from Census 2000 Summary File 3.(19) The number of the public practice dentists was obtained from the 2003 OSHPD Primary Care Clinics Annual Utilization Data, which includes dentists working in federally-funded or free-standing community clinics as well as those affiliated with hospitals, or dental and hygiene schools. OSHPD data does not represent the universe of public providers, but is the best approximation. We also obtained data from California dental schools on the total number of full-time equivalent students and faculty providing patient care in 2003 in schools and satellite clinics and removed the overlap in FTE dentists between these providers and OSHPD data.
The CDS and CHIS data were merged at the MSSA level. Of 542 California MSSAs, 14 had no dentists in 2003, 85 were not represented in the CDS survey and were excluded from the final dataset. Up to 29 additional MSSAs were excluded from analysis due to CDS survey item non-response. All MSSAs had CHIS respondents. Of the 42,044 adult respondents in CHIS, 40,249 resided in MSSAs where data on characteristics of dentists was available in CDS. The final sample size ranged from 39,216 to 40,084 and 414 to 443 MSSA.
Dependent Variables
Access to dental care was measured at the individual level (CHIS data) by an annual visit or whether a respondent had a dental visit within the past year (objective measure). Access was also measured by unmet need or whether a respondent reported having foregone or delayed needed dental care due to costs (subjective measures).
Independent Variables
The dental care delivery system measures included CDS indicators calculated at the MSSA level. Personal characteristics included percentage of dentists who were over age 60, nonwhite, generalist, and female in an MSSA. Practice structure and work characteristics included percentage of dentists who employed two or more dental assistants, employed a dental hygienist, had multiple practice locations, were owners or partners in their practice, reported being busy or overworked, reported lower than median wait time for an appointment of five days, and reported lower than median appointment length of 45 minutes. The average number of dental visits per dentist in a week per MSSA was also calculated. Financial and cultural competency indicators included percentage of dentists who accepted discounted fees, accepted public insurance, and whether dentists and staff only spoke English. Safety net and private practice dentist supply were measured by calculating the ratio of full-time equivalent dentist in each setting to 5,000 population per MSSA. The proportion of white population per MSSA was also included from Census data as a contextual measure of population characteristics.
The individual level control variables included age (65 years of age or older vs. 18–64), gender, race/ethnicity (African American, Latino, Asian American, and American Indian and other vs. white), U.S. citizen (vs. not), any college education (vs. none), and rural residence (vs. urban) as predisposing characteristics.(12) Income was determined by 200% of federal poverty level (FPL) (vs. higher) and public or private dental insurance coverage (vs. none) as enabling determinates of access. Self-assessed health (fair/poor vs. excellent/very good/good), being a current smoker or a past smoker (vs. never smoked), and having been diagnosed with asthma, diabetes, or high blood pressure were included to control for the impact of need for health care.
Analysis Methods
We assumed that the CDS variables were independent and normally distributed and accounted for the sampling error associated with CDS data by calculating the variance of the CDS variables at the MSSA level and using the resulting variance data in the models. We used generalized linear mixed models (GLIMMIX) with binomial distribution and logistic link in SAS (v. 9.1.3) in order to specify the variance of CDS data and account for the multilevel nature of the data. We included the ratio of private practice and public practice FTE dentists to 5,000 in all models to control for the overall effect of supply of dental providers. We examined the relationship of additional dentist characteristics in separate models, because our models did not converge when using more than three external variance estimates in GLIMMIX. We also included the proportion of the population that was white and all the individual control variables described above, in all the models. We further stratified each model by race/ethnicity and poverty level to examine racial/ethnic and income disparities in access. All analyses were weighted for the CHIS survey design. We reported the Bonferroni adjustment to the probability values in tables to account for multiple comparisons, but discussed the significant variables based on their original probability values because of the high likelihood of type II error. This study was approved by the appropriate committee for protection of human subjects.
RESULTS
The population characteristics are displayed in Table 1 and dental delivery system characteristics are displayed in Table 2. Table 2 includes the average characteristic per MSSA, and the number of MSSAs, and the population size available for the analyses of the entire population.
Table 1.
Characteristics of adults, California, 2003
| Access to Dental Care | N= 40,084 |
|---|---|
| Annual dental visit: dental visit in the past year | 67% |
| Unmet need: delayed or forgone needed dental care due to costs in the past year | 20% |
| Predisposing Characteristics | |
| Age 65 years or older (vs. 18–64) | 15% |
| Female | 51% |
| Race/Ethnicity | |
| White (reference group) | 52% |
| African American | 6% |
| Latino | 26% |
| Asian-American | 12% |
| American Indian | 1% |
| Other | 3% |
| College Education or Higher (vs. less education) | 56% |
| US Born or Naturalized Citizen (vs. non-citizen) | 82% |
| English Language Proficiency | |
| Native English Speaker (reference group) | 73% |
| Speaks English Well | 11% |
| Speaks English Not Well/Not At All | 16% |
| Rural residence (vs. urban) | 10% |
| Enabling Characteristics | |
| 200% FPL or greater (vs. lower FPL) | 67% |
| Dental Insurance | |
| No Dental Insurance (reference group) | 35% |
| Public Insurance | 12% |
| Private Insurance | 53% |
| Need Characteristics | |
| Has Asthma | 12% |
| Has Diabetes | 7% |
| Smoking Status | |
| Currently smokes | 16% |
| Quit smoking | 24% |
| Never smoked (reference group) | 60% |
Note: Weighted estimates are presented.
Source: 2003 California Health Interview Survey (CHIS)
Table 2.
Dental Delivery System Characteristics and MSSA and adult population sample size per characteristic
| Average per SSA |
Number of MSSAs |
Population size | |
|---|---|---|---|
| Safety net dentist supply | |||
| Public safety-net dentist to population ratio (per 5,000) | 0.34 | 443 | 40,084 |
| Private practice dentist supply | |||
| Private practice dentist to population ratio (per 5,000) | 2.86 | 443 | 40,084 |
| Personal characteristics of dentists in private practice | |||
| Percent of dentists who are over age 60 | 14% | 423 | 39,499 |
| Percent of dentists who graduated within past 5 years | 10% | 423 | 39,499 |
| Percent of dentists who are nonwhite | 10% | 422 | 39,488 |
| Percent of dentists who are generalist | 87% | 423 | 39,499 |
| Percent of dentists who are female | 25% | 422 | 39,488 |
| Practice structure and work characteristics of private dental practices | |||
| Average number of dental visits in a week | 39 | 421 | 39,393 |
| Percent of dentists who own or are partner in dental practice | 80% | 422 | 39,452 |
| Percent of dentists who employ a dental hygienist | 45% | 420 | 39,395 |
| Percent of dentists who employ 2 or more dental assistants | 62% | 422 | 39,452 |
| Percent of dentists who have multiple practice locations | 15% | 421 | 39,429 |
| Percent of dentists who report being busy or overworked | 24% | 422 | 39,452 |
| Percent of dentists who report lower than median appointment length (45 min) | 38% | 418 | 39,277 |
| Percent of dentists who report lower than median wait time for an appointment (5 days) | 50% | 414 | 39,048 |
| Financial indicators of private dental practices | |||
| Percent of dentists who accept discounted fees | 52% | 416 | 39,216 |
| Percent of dentists who accept public insurance | 47% | 418 | 39,277 |
| Cultural competency of private dental practices | |||
| Percent of dentists and office staff who speak English only | 26% | 423 | 39,499 |
MSSA: Medical Study Service Area
The MSSA sizes for income and racial/ethnic stratified analysis varied by each characteristic: less than 199% FPL (411–416), 200% FPL or more (416–421), whites (417–422), African Americans (296–298), Asian Americans (327–328), and Latinos (385–390). Similarly, the population size for stratified analysis varied: less than 199% FPL (10,868–11,103), 200% FPL or more (28,339–28,557), whites (24,832–25,025), African Americans (2,432–2,483), Asian Americans (3,815–3,826), and Latinos (6,436–6,610).
Table 3 shows that odds of annual visits were higher with some dentist characteristics. For example, a higher proportion of female dentists in an MSSA increased the odds of annual visits (OR=1.2) in general and by whites in particular (1.27). In contrast, a higher proportion of dentists over the age of 60 in an MSSA reduced the odds of visits by lower income groups (0.65), Asian Americans (0.39) and Latinos (0.63). Other significant dentist characteristics associated with disparities are indicated in Table 3.
Table 3.
Population Odds of Dental Visit within the Past Year Given Dental System Characteristics
| Total Population |
Less Than 200% FPL |
200% FPL or More |
White | African American |
Asian American |
Latino | |
|---|---|---|---|---|---|---|---|
| Safety net dentist supply | |||||||
| Public safety-net dentist to population ratio (per 5,000) | 0.99* | 1.00 | 1.00 | 0.98*§ | 0.99 | 1.00 | 1.00 |
| Private practice dentist supply | |||||||
| Dentist to population ratio (per 5,000) | 1.02*§ | 1.04 | 1.02*§ | 1.05*§ | 0.94 | 1.00 | 1.01 |
| Personal characteristics of private practice dentists | |||||||
| Percent of dentists over age 60 | 0.83 | 0.65* | 0.80 | 0.96 | 0.73 | 0.39*§ | 0.63* |
| Percent of dentists who graduated within past 5 years | 1.18 | 1.06 | 0.98 | 1.19 | 0.90 | 1.31 | 1.15 |
| Percent of nonwhite dentists | 0.90 | 0.83 | 0.92 | 0.80 | 0.56* | 1.03 | 1.00 |
| Percent of dentists who are generalist | 0.92 | 0.77 | 1.03 | 0.87 | 1.33 | 0.82 | 0.87 |
| Percent of female dentists | 1.20* | 1.13 | 1.21 | 1.27* | 0.81 | 1.46 | 1.17 |
| Practice structure and work characteristics of private dental practices | |||||||
| Average number of dental visits in a week | 1.01 | 1.02 | 1.00 | 1.01 | 1.03 | 1.01 | 1.00 |
| Percent of dentists who own or are partner in dental practice | 0.93 | 0.96 | 0.91 | 0.86 | 0.64 | 1.17 | 1.01 |
| Percent of dentists who employ a dental hygienist | 1.00 | 0.90 | 1.12 | 1.08 | 0.91 | 1.25 | 0.94 |
| Percent of dentists who employ 2 or more dental assistants | 0.98 | 1.03 | 0.95 | 0.82* | 1.28 | 1.27 | 1.17 |
| Percent of dentists who have multiple practice locations | 1.24 | 1.47* | 1.00 | 1.04 | 1.52 | 1.45 | 0.96 |
| Percent of dentists reporting being busy or overworked | 0.81* | 0.95 | 0.74* | 0.79* | 0.74 | 0.58* | 1.25 |
| Percent of dentists who report lower than median appointment length (45 min) | 1.02 | 1.67 | 0.95 | 0.90 | 1.35 | 0.89 | 1.31* |
| Percent of dentists who report lower than median wait time for an appointment (5 days) | 0.95 | 0.96 | 0.96 | 1.00 | 1.13 | 1.12 | 0.79 |
| Financial indicators of private dental practices | |||||||
| Percent of dentists who accept discounted fees | 1.11 | 1.27* | 0.98 | 1.00 | 0.77 | 1.10 | 1.44*§ |
| Percent of dentists who accept public insurance | 0.92 | 0.98 | 0.88 | 0.74*§ | 1.08 | 1.34 | 1.09 |
| Cultural competency of private dental practices | |||||||
| Percent of dentists and office staff who speak English only | 0.71 | 1.08 | 0.53* | 0.60 | 0.28 | 0.62 | 2.22 |
Notes:
FPL: Federal Poverty Level; MSSA: Medical Study Service Area
Each row represents a regression with the same dependent variable and control variables. The control variables are population characteristics including predisposing, enabling, and need variables identified in Table 1.
Significant at p<0.05 without Bonferroni adjustment
Significant at p<0.05 with Bonferroni adjustment
Source: Based on authors’ analysis of a 2003 survey of California dentists and the 2003 Health Interview Survey
Table 4 shows that the odds of experiencing unmet need in the past year increased with some dentist characteristics. For example, the odds of unmet need decreased with a higher proportion of female dentists in an MSSA in general (OR=0.72) and by all racial/ethnic groups and higher income populations but not by the low-income. But a higher proportion of dentists who graduated within the past 5 years increased the odds of unmet need by African Americans (2.95). Other dentist characteristics associated with more unmet need are indicated in Table 4.
Table 4.
Population Odds of Unmet Need within the Past Year Given Dental System Characteristics
| Total | Less Than 200% FPL |
200% FPL or More |
White | African American |
Asian American | Latino | |
|---|---|---|---|---|---|---|---|
| Safety net dentist supply | |||||||
| Public safety-net dentist to population ratio (per 5,000) | 1.01 | 1.00 | 1.01 | 1.00 | 1.00 | 1.01 | 1.04* |
| Private practice dentist supply | |||||||
| Dentist to population ratio (per 5,000) | 0.99 | 0.98 | 1.00 | 0.99 | 0.99 | 1.00 | 0.96 |
| Personal characteristics of private practice dentists | |||||||
| Percent of dentists over age 60 | 0.93 | 1.00 | 0.89 | 0.92 | 1.10 | 0.68 | 0.96 |
| Percent of dentists who graduated within past 5 years | 1.07 | 0.98 | 1.22 | 1.11 | 2.95* | 1.59 | 0.82 |
| Percent of nonwhite dentists | 0.90 | 0.86 | 0.98 | 0.97 | 0.94 | 0.32* | 0.92 |
| Percent of generalist dentists | 0.92 | 0.32 | 1.11 | 0.88 | 0.54 | 3.50* | 1.02 |
| Percent of female dentists | 0.72*§ | 0.85 | 0.70*§ | 0.71*§ | 0.54* | 0.52* | 0.70* |
| Practice structure and work characteristics of private dental practices | |||||||
| Average number of dental visits in a week | 1.01 | 0.99 | 1.01 | 1.01 | 1.00 | 0.99 | 0.98 |
| Percent of dentists who own or are partner in dental practice | 0.93 | 1.03 | 1.09 | 1.26 | 1.67 | 0.76 | 0.86 |
| Percent of dentists who employ a dental hygienist | 1.00 | 0.98 | 0.76*§ | 0.83 | 0.64 | 0.12 | 0.85 |
| Percent of dentists who employ 2 or more dental assistants | 0.98 | 0.94 | 1.15 | 1.17 | 1.30 | 0.94 | 0.97 |
| Percent of dentists who have multiple practice locations | 1.24 | 0.84 | 1.06 | 1.22 | 0.72 | 0.87 | 0.67* |
| Percent of dentists reporting being busy or overworked | 0.81* | 1.20 | 1.18 | 1.19 | 1.29 | 1.12 | 1.01 |
| Percent of dentists who report lower than median appointment length (45 min) | 1.02 | 1.05 | 0.93 | 1.04 | 1.02 | 0.71 | 0.89 |
| Percent of dentists who report lower than median wait time for an appointment (5 days) | 0.95 | 0.74* | 0.82* | 0.78* | 0.64 | 0.82 | 0.70* |
| Financial indicators of private dental practices | |||||||
| Percent of dentists who accept discounted fees | 1.11 | 0.98 | 1.08 | 0.98 | 1.48 | 0.70 | 0.86 |
| Percent of dentists who accept public insurance | 0.92 | 0.90 | 1.34*§ | 1.08 | 2.03*§ | 0.98 | 0.89 |
| Cultural competency of private dental practices | |||||||
| Percent of dentists and office staff who speak English only | 0.71 | 2.40* | 0.98 | 1.47 | 0.79 | 15.20 | 0.69 |
Each row represents a regression with the same dependent variable and control variables. The control variables are population characteristics including predisposing, enabling, and need variables identified in Table 1.
Notes:
FPL: Federal Poverty Level; MSSA: Medical Study Service Area
Significant at p<0.05 without Bonferroni adjustment
Significant at p<0.05 with Bonferroni adjustment
Source: Based on authors’ analysis of a 2003 survey of California dentists and the 2003 Health Interview Survey
DISCUSSION
The findings confirm that practice norms of private practice dentists, who constitute the great majority of U.S. dentists, promote or inhibit income and racial/ethnic disparities in access. For example, older, newly graduated, and female dentists work fewer hours, and female dentists see fewer patients per hour and have fewer staff.(8, 20, 21) Alternatively, non-white, dentists are more likely to have non-white or low-income patients.(22) The CDS data show that most California dentists are white or Asian American, which is discordant with the size of the Latino and African American populations. Female dentists also tend to spend more time on provision of preventive care, which is more often received by white patients.(13, 23)
The results provide insights into how some private dentists practice: those with larger and busier practices often employ hygienists and multiple dental assistants, have multiple locations, shorter appointment times and longer wait times, accept public insurance and discounted fees, and have multiple language capacity in their practice. These dentists are more likely to provide care to lower-income, publicly-insured, non-white, and limited English proficient patients, and operate in densely populated areas.(5) They may also focus less on preventive care, but more on services such as extractions and aesthetic care. (13) Other dentists are more likely to provide care to privately insured and higher income patients.
The relationship of access with supply of FTE dentists/5,000 also indicates a tiered system of care by income and race/ethnicity. While more private practice dentists in a community increase rates of annual visits, their presence tends to benefit higher income and white patients more than their low-income and non-white counterparts. However, the presence of more dentists in safety net community clinics and dental schools is insufficient to address the level of need in communities populated by low-income and non-white populations.(24)
We had limitations and strengths. The California Dentist Survey excluded dentists who exclusively practiced in non-private settings. Comprehensive data on the universe of practicing dentists in corporate practices, school-based clinics, mobile clinics, hospital-based clinics, VA facilities, public hospitals, and county health facilities were not available. But all public dentists practicing in licensed clinics in OSHPD data and California dental schools were included. Our study includes the substantial majority of the providers of low cost dental care and the absence of providers in alternative settings does not limit the generalizability of the results. We used the FTE concept to address the potential overlap between private and public settings, though some overlap may exist when dentists volunteer in public settings.
We may have underestimated the impact of some dentist characteristics because individuals’ travel between MSSA to use dental care. Also, we excluded MSSAs (2.6%) without practicing dentists or due to non-response (15.7%). However, travel across MSSA lines is more likely for those living at MSSA borders, when safety-net providers are unavailable, or in densely populated urban areas with multiple MSSAs than in rural MSSAs. But, factors such as language limitations, heavier reliance on public transportation, and less flexibility in paid time off from work may prevent underserved populations from traveling across MSSAs or cause delays in visits.
We were unable to simultaneously assess all dentist variables because of technical limitations and insufficient sample for more complicated analyses, but included the indicators of public and private dentists-population ratios in all models to address this limitation to some degree. We used smoking status, chronic conditions, and general health status as reasonable proxies for oral health status because CHIS lacked direct measures. We also lacked information on obesity and whether dental care was received from private dentists or public sources.
The generalizability of the findings may be limited due to the age of the data and lack of national data. Since 2003, the number of licensed California dentists has increased but their demographics and practice characteristics have remained consistent both in California and nationally.(21) Similarly, the sociodemographic characteristics of California population have remained relatively stable and economic changes related to the recent recession have occurred nationwide. There is little evidence to indicate that the relationship of the dental delivery system to access to care has changed significantly since 2003.
The major strengths of this study are the unprecedented detailed data on characteristics of the dental delivery system, the use of representative California data that reduced variations in state-level policies and practices, examination of the role of system characteristics in access at the MSSA, and focusing on unmasking disparities in access often hidden in aggregate analysis. We refined the measure of supply by using FTE practicing dentists since many licensed dentists do not practice or practice part-time.
Policy Implications
These findings highlight the deficiencies of focusing on traditional measures of supply such as licensed dentist to population ratios and indicate that dentist characteristics play a role in disparities in access. Lack of such data is a barrier to developing effective state and local policies to address disparities and monitoring their impact. Minimum data sets with consistent information across geographic areas are needed (25) and state licensing boards can be the vehicle for collecting characteristics such as practice setting, accepting public insurance or discounted care, busyness, staffing, age, gender, and ethnicity. These data can be used to promote access for the underserved through policy and would allow for continuous monitoring of the impact of these policies on disparities. Such detailed data would better inform designation of shortage areas beyond current methods using dentist age and staff size.(9) Loan repayment and scholarship programs are tied to shortage designation and would also be more targeted with detailed data. Efforts to train more African American and Latino dentists are sound policy solutions needed to alleviate disparities and should continue. Favorable small business loans or tax incentives can also be used to attract less busy or experienced dentists to underserved areas.
Addressing financial barriers to dental care access have been at the forefront of policy efforts but permanent and effective solutions have consistently eluded policymakers. The problem of dentist participation in Medicaid is long-standing. Less than half of dentists in California reported having any publicly insured patients in their practice in 2003 and their numbers may have declined since 2009 when California cut Medicaid dental benefits. Despite reinstatement of these benefits in 2013, the lower reimbursement in the program is still a barrier. Increase in Medicaid fees to encourage Medicaid participation is unlikely as budget shortages continue to plague the nation. Even with higher fees, Medicaid beneficiaries still have to compete with privately insured and higher income patients and providers may continue to prefer privately insured and self-paying patients to avoid lower fees and authorization delays.
Availability of low cost dental care in the form of discounted fees is an untenable solution, particularly since provider discounts are likely to fluctuate with recession and economic decline. Policies that improve dental insurance coverage and benefits are more effective. Mandating offering of adult dental benefits in Health Benefit Exchange marketplaces, similar to the mandate to offer dental policies for children under the 2010 Patient Protection and Affordable Care Act, is one likely approach.
Acknowledgements
This study was funded under grant #1R03DE018399-01A2 by the National Institute for Dental and Craniofacial Research. The survey of California Dentists was funded by a grant from the California Dental Association Foundation.
Contributor Information
Nadereh Pourat, Email: pourat@ucla.edu.
Ronald M Andersen, Email: radnerse@ucla.edu.
Marvin Marcus, Email: mmarcus@dentistry.ucla.edu.
REFERENCES
- 1.Institute of Medicine. [Accessed 12/27/132011];Advancing Oral Health in America. [Google Scholar]
- 2.Institute of Medicine. [Accessed 12/27/13 2011];Improving Access to Oral Health Care for Vulnerable and Underserved Populations. [Google Scholar]
- 3.Guay AH. Access to dental care: Solving the problem for underserved populations. J Am Dent Assoc. 2004 Nov 1;135(11):1599–1605. doi: 10.14219/jada.archive.2004.0088. 2004. [DOI] [PubMed] [Google Scholar]
- 4.Seale NS, Casamassimo PS. Access to dental care for children in the United States: a survey of general practitioners. J Am Dent Assoc. 2003 Dec;134(12):1630–1640. doi: 10.14219/jada.archive.2003.0110. [DOI] [PubMed] [Google Scholar]
- 5.Pourat N, Roby DH, Wyn R, Marcus M. Characteristics of dentists providing dental care to publicly insured patients. J Public Health Dent. 2007 Fall;67(4):208–216. doi: 10.1111/j.1752-7325.2007.00024.x. [DOI] [PubMed] [Google Scholar]
- 6.Sweet M, Damiano P, Rivera E, Kuthy R, Heller K. A comparison of dental services received by Medicaid and privately insured adult populations. J Am Dent Assoc. 2005 Jan;136(1):93–100. doi: 10.14219/jada.archive.2005.0034. [DOI] [PubMed] [Google Scholar]
- 7.Mertz EA, Grumbach K. Identifying communities with low dentist supply in California. J Public Health Dent. 2001 Summer;61(3):172–177. doi: 10.1111/j.1752-7325.2001.tb03386.x. [DOI] [PubMed] [Google Scholar]
- 8.Wendling WR. Private sector approaches to workforce enhancement. Journal of Public Health Dentistry. 2010;70:S24–S31. doi: 10.1111/j.1752-7325.2010.00177.x. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services. Health Resources and Services Administration. [Accessed 12/26/13. 2013];Shortage Designation: Health Professional Shortage Areas & Medically Underserved Areas/Populations. Available from: http://www.hrsa.gov/shortage/
- 10.Logan HL, Guo Y, Dodd VJ, Seleski CE, Catalanotto F. Demographic and practice characteristics of Medicaid-participating dentists. Journal of Public Health Dentistry. 2013:1–8. doi: 10.1111/jphd.12037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayer ML, Stearns SC, Norton EC, Rozier RG. The effects of Medicaid expansions and reimbursement increases on dentists’. participation. Inquiry. 2000 Spring;37(1):33–44. [PubMed] [Google Scholar]
- 12.Andersen RM, Davidson PL. Improving Access to Care in America: Individual and Contextual Indicators. In: RM Andersen, TH Rice, GF Kominski., editors. Changing the US Health Care System. 3rd ed. San Francisco, CA: Jossey Bass; 2007. [Google Scholar]
- 13.Pourat N, Marcus M. Variations in self-reported provision of services by general dentists in private practice. The Journal of the American Dental Association. 2011 Sep 1;142(9):1050–1060. doi: 10.14219/jada.archive.2011.0327. 2011. [DOI] [PubMed] [Google Scholar]
- 14.California Health Interview Survey. CHIS Making an Impact—2012. Los Angeles: UCLA Center for Health Policy Research; 2013. [Google Scholar]
- 15.California Health Interview Survey. THE CALIFORNIA HEALTH INTERVIEW SURVEY 2003 RESPONSE RATES. Los Angeles: UCLA Center for Health Policy Research; 2003. [Google Scholar]
- 16.Keil L, Potter F, Reed M. Community Tracking Study, Physician Survey Round 1, Survey Methodology Report, Technical Publication No. 9: Center for Studying Health System Change. 1998 Oct [Google Scholar]
- 17.Yang YM, Wang Y. Weighting Class versus Propensity Model Approaches to Nonresponse Adjustment: The SDR Experience. 2008 [Google Scholar]
- 18.California Office of Statewide Health Planning and Development. Medical Service Study Areas. 2012 [cited 2013 Januaray 18]; Available from: http://www.oshpd.ca.gov/hwdd/MSSA/index.html.
- 19.U.S. Census Bureau: U.S. Department of Commerce EaSA. Product Profile: Census 2000 Summary File 3. Accessed 12/26/13. 2013; Available from: http://www.census.gov/prod/2003pubs/prodpr03-1.pdf.
- 20.Brown L. Adequacy of Current and Future Dental Workforce: Theory and Analysis. Chicago: American Dental Association, Health Policy Resource Center; 2005. [Google Scholar]
- 21.American Dental Association. Characteristics of Dentists in Private Practice and Their Patients. Chicago: p. Il2008. [Google Scholar]
- 22.Brown LJ, Wagner KS, Johns B. Racial/Ethnic Variations of Practicing Dentists. The Journal of the American Dental Association. 2000 Dec;131(12):1750–1754. doi: 10.14219/jada.archive.2000.0122. 2000. [DOI] [PubMed] [Google Scholar]
- 23.Riley JL, Gordan VV, Rouisse KM, McClelland J, Gilbert GH. Differences in male and female dentists’. practice patterns regarding diagnosis and treatment of dental caries: Findings from The Dental Practice-Based Research Network. The Journal of the American Dental Association. 2011 Apr 1;142(4):429–440. doi: 10.14219/jada.archive.2011.0199. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bailit H, Beazoglou T, Demby N, McFarland J, Robinson P, Weaver R. Dental safety net: Current capacity and potential for expansion. Journal of American Dental Association. 2006 Jun 1;137(6):807–815. doi: 10.14219/jada.archive.2006.0294. 2006. [DOI] [PubMed] [Google Scholar]
- 25.Health Resources and Services Administration: National Center for Health Workforce Analysis. Health Professions Minimum Data Set. Accessed 12/25/20132013. [Google Scholar]