Abstract
Purpose
There is an increasing incidence of mortality among trauma patients; therefore, it is important to analyze the trauma epidemiology in order to prevent trauma death. The authors reviewed the trauma epidemiology retrospectively at a regional emergency center of Korea and evaluated the main factors that led to trauma-related deaths.
Materials and Methods
A total of 17007 trauma patients were registered to the trauma registry of the regional emergency center at Wonju Severance Christian Hospital in Korea from January 2010 to December 2012.
Results
The mean age of patients was 35.2 years old. The most frequent trauma mechanism was blunt injury (90.8%), as well as slip-and-fall down injury, motor vehicle accidents, and others. Aside from 142 early trauma deaths, a total of 4673 patients were admitted for further treatment. The most common major trauma sites of admitted patients were on the extremities (38.4%), followed by craniocerebral, abdominopelvis, and thorax. With deaths of 126 patients during in-hospital treatment, the overall mortality (142 early and 126 late deaths) was 5.6% for admitted patients. Ages ≥55, injury severity score ≥16, major craniocerebral injury, cardiopulmonary resuscitation at arrival, probability of survival <25% calculated from the trauma and injury severity score were independent predictors of trauma mortality in multivariate analysis.
Conclusion
The epidemiology of the trauma patients studied was found to be mainly blunt trauma. This finding is similar to previous papers in terms of demographics and mechanism. Trauma patients who have risk factors of mortality require careful management in order to prevent trauma-related deaths.
Keywords: Trauma, epidemiology, mortality, injury severity score, predictor
INTRODUCTION
Trauma is a major cause of death and social problem.1 In low and middle income countries, which make up 85% of the world, 11% of all disability-adjusted life years are due to trauma.2 In these countries, trauma-related mortality before 70 years of age is more frequent than in high income countries, and the life expectancy projections are very low.3 Also, according to the Annual Report of Emergency Medicine in Korea, the proportion of trauma patients have steadily grown, and the overall mortality of trauma patients in emergency centers have gradually increased from 1.87% in 2007 to 2.71% in 2011.4 For these reasons, major attention is given to improving treatment of trauma patients, preventing trauma itself, and developing various emergency medical services to reduce preventable trauma death. Particularly, understanding the epidemiology of trauma helps to analyze risk factors, to develop treatment strategy, to reduce disability, to prevent mortality, and to construct a precise intervention system. However, the lack of trauma epidemiology data limits the growth of these trauma management systems.5,6
The purpose of this study is to examine the epidemiology of trauma within a local community in Korea through data gained from one emergency center and to analyze trauma patients in order to find the predictors that led to the deaths of trauma patients.
MATERIALS AND METHODS
All data were based on patients registered on the trauma registry at the emergency center of Wonju Severance Christian Hospital, located in Wonju city, Gangwon province, Korea. The aforementioned center is run on national funds and is composed of emergency physicians, trauma surgeons, trained nurses, and clinical research coordinators. When patients are admitted to the emergency center, patient information such as age, gender, address, and method of admission is gathered; additionally, clinical information such as mechanisms of injury, the time of injury, revised trauma score (RTS), injury severity score (ISS), major injury site, history of hospitalization and surgery, transfer history, and death on arrival (DOA) is composed in detail. The major injury site is determined by the highest abbreviated injury score (AIS) among the measured areas or the area that led to death or admission. It is divided into subgroups: craniocerebral, thoracic, abdominopelvic, and extremity. The information was constantly updated in order to assess each patient's progress. To ensure the accuracy of the data, confirmation by the trauma surgeon and senior doctors took place before they were entered into Excel (Microsoft, 2005).
The trauma registry data had been collected since January 1, 2010, and 21697 patients were registered from that time until Dec 31, 2012. Cases relating to poisoning, burns, drowning, and suicide were excluded, leaving 17007 selected patients, who were examined retrospectively and approved by the Institutional Review Board of Wonju Severance Christian Hospital (YWMR 14-5-001).
All statistical calculations were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). The frequencies for variables were identified using descriptive statistics. Student's t-tests, or non-parametric tests when necessary, were employed for quantitative variable analysis, and Pearson chi-square tests were used for categorical variable analysis between survivors and non-survivors. Multivariate analysis and identification of the independent factors associated with trauma mortality was achieved through the adjustment of a logistic regression model. Only the variables associated with mortality that yielded p values lower than 0.5 in the initial analysis were input into the logistic regression analysis. Odds ratios and 95% confidence intervals were used to estimate the associations with non-survivors.
RESULTS
Distribution of trauma patients according to age and sex
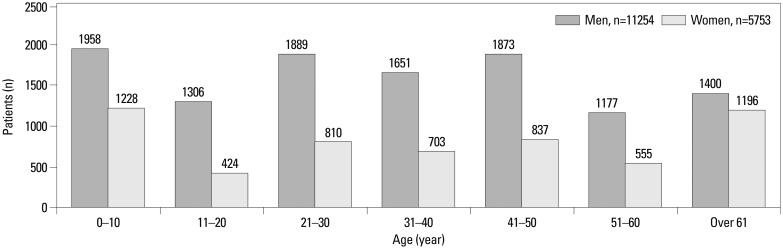
When assessing the 17007 patients, the average age was 35.2±22.4 (range 0-105), and the percentage of males was 66.2%. The age and sex distribution is shown in Fig. 1. For all age groups, the frequency of trauma in males was higher than in females, and the changes in trauma frequency between age groups were similar for males and females. The distribution of trauma according to age was highest for those under the age of 10, after which it was low until the age of 20. The trauma frequency then maintained a slightly higher rate until the age of 50. Between the ages of 51 and 60, the incidence of trauma decreased somewhat, then increased after the age of 61.
Fig. 1.
Age and sex distribution of trauma patients.
Disposition of trauma patients at emergency center
As shown in Table 1, 56.0% (n=9516) of a total of 17007 patients were discharged from the emergency center after early recovery, and 15.6% (n=2642) transferred to a regional hospital after primary treatment. In total, 27.4% (n=4673) were admitted to the emergency center for further treatment. Additionally, 21.4% (n=3643) of patients were admitted to the general ward for in-hospital treatment, and 3.0% (n=511) were admitted to the intensive care unit for close vital sign monitoring without emergency surgery. Only 3.0% (n=519) of patients did undergo emergency surgery, and 0.2% (n=41) of all patients were DOA. The remaining 0.6% (n=101) died after receiving cardiopulmonary resuscitation (CPR) at the emergency center.
Table 1.
Treatment Results of Trauma Patients (n=17007)
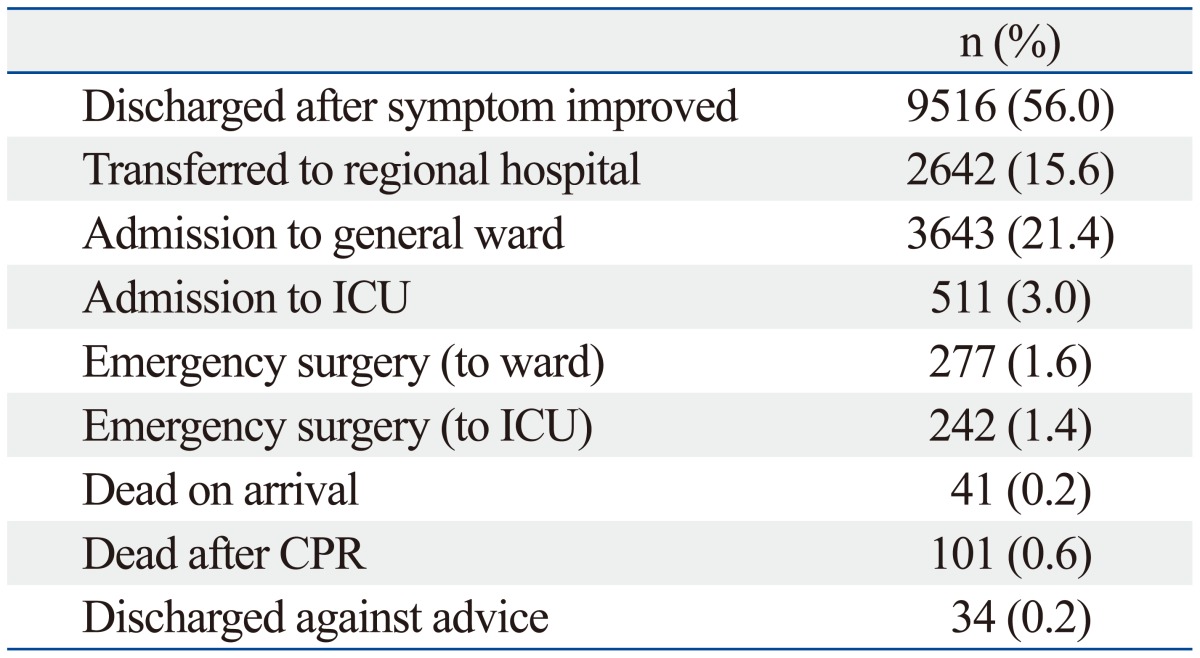
ICU, intensive care unit; CPR, cardiopulmonary resuscitation.
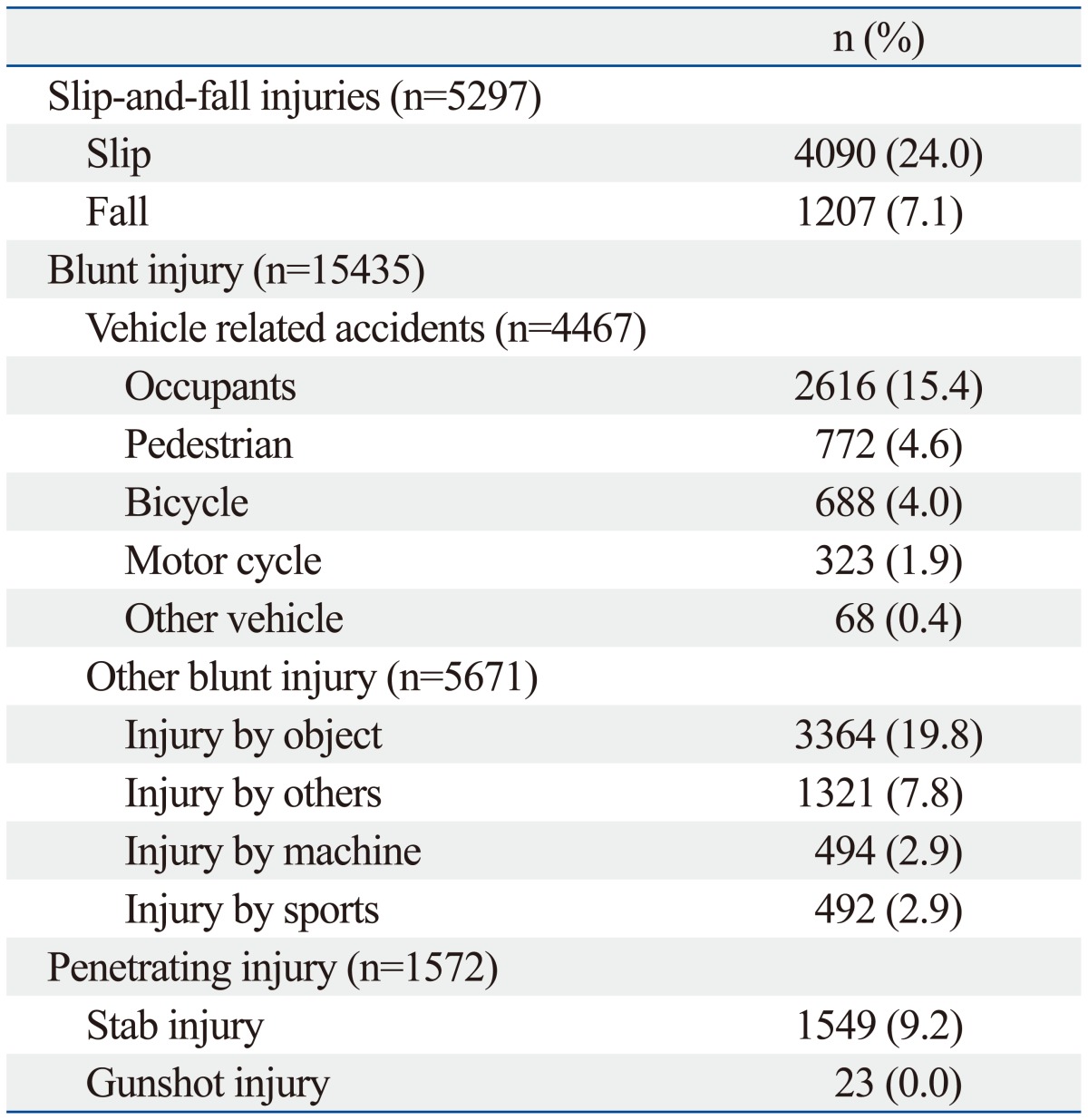
Mechanism of injuries in trauma patients
Among 17007 patients, slip-and-fall-down injuries were the most prominent cause of trauma (31.1%; n=5297) as can be observed in Table 2. A total of 26.2% (n=4467) suffered a vehicle-associated accident, with 15.4% (n=2616) riding as passengers, 4.6% (n=772) as pedestrians, 4.1% (n=688) riding motorcycles, and 1.9% (n=323) riding bicycles. The remaining 0.4% (n=68) of patients were injured from other vehicle accidents. Additionally, 33.3% (n=5671) of patients were injured by blunt force trauma, such as contusion by objects, beatings by others, and sports-related or machine-related injuries. The remaining 9.2% (n=1572) had penetrating injuries with stab or gunshot wounds.
Table 2.
Injury Mechanism of Trauma Patients (n=17007)
Major injury site and treatment results after hospital admission
Table 3 shows the distribution of admitted patients according to major trauma site, which was determined by the area with the highest measured AIS that led to admission. The most common major injury sites were the extremities (38.4%; n=1759). Major craniocerebral damage (27.5%; n=1286) was second, followed by abdominopelvic injury (20.7%; n=965) and major thoracic injury (13.4%; n=627).
Table 3.
Distribution of Admitted Patients According to Major Injury Site (n=4673)
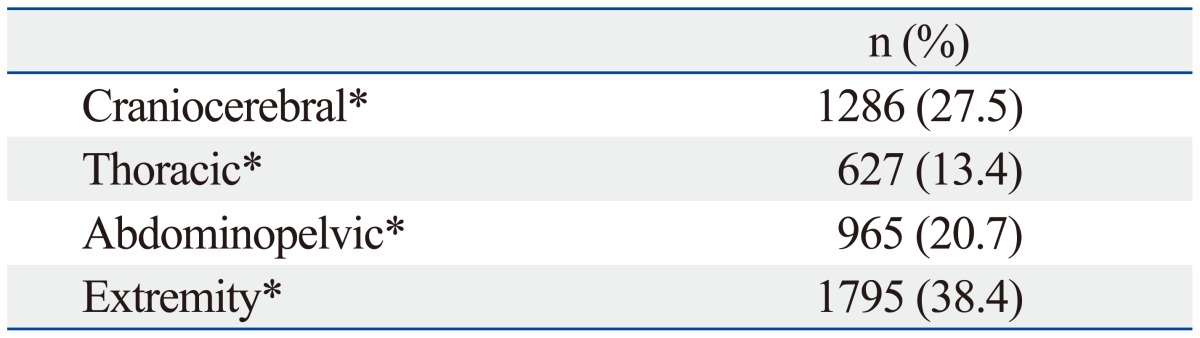
AIS, abbreviated injury score.
*Major injury site is determined by the area with the highest measured AIS that led to admission.
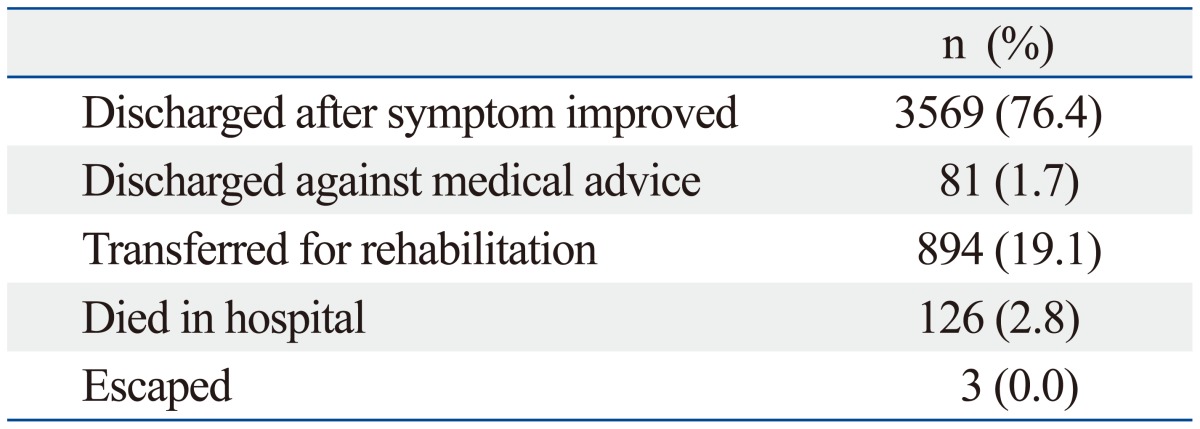
76.4% (n=3569) of 4673 patients were discharged after proper treatment. Among the remaining patients, 19.1% (n=894) transferred to rehabilitation facilities, and 2.8% (n=126) died during hospitalization. Table 4 details these results.
Table 4.
Treatment Results of Admitted Patients (n=4673)
Analysis of trauma mortality in admitted patients and predictors of mortality
The total number of survivors and non-survivors among admitted patients was 4815 patients. Among them, a total of 268 patients (5.6%) died including 126 hospitalized patients and 142 patients who were DOA or died after CPR in the emergency center. The average age for survivors was 44.9±21.3 years (range 0-93 years) 53.5±21.9 years (range 0-96 years) for non-survivors; the percentage of males was 68.0% for survivors and 67.2% for non-survivors. Time intervals from accident to arrival at the emergency center were 2.4±3.5 (median 1.4) hours for survivors and 1.8±2.4 (median 0.8) hours for non-survivors. Differences of RTS, ISS, and other variables between the two groups are shown in Table 5. Among non-survivors, 42.2% of patients (n=113) died due to major craniocerebral injury, 33.6% (n=90) died due to major thoracic injury, and 24.2% (n=65) died due to major abdominopelvic injury. Probability of survival (Ps) based on a trauma score and injury severity score (TRISS) of less than 25% was 51.6% for non-survivors. Additionally, the Ps was 25-75% for 20.8% of non-survivors and 75% or more for the remaining 27.6% of non-survivors.
Table 5.
Comparison of Demographics and Clinical Characteristics between Survivors and Non-Survivors Who Were Admitted (n=4815)
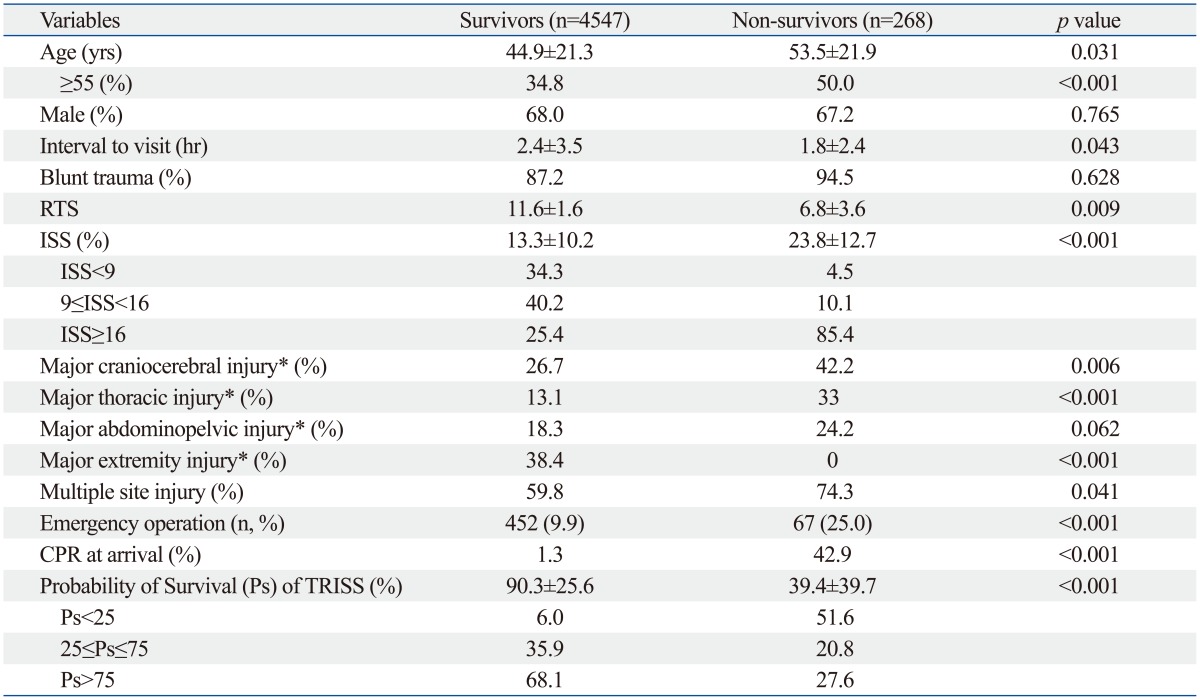
RTS, revised trauma score; ISS, injury severity score; CPR, cardiopulmonary resuscitation; TRISS, trauma and injury severity score; Ps, probability of survival.
Data are presented as the means±SD or numbers (%) of patients.
*Highest area of measured abbreviated injury score that led to death or admission.
Non-survivors with major thoracic injuries had the statistically highest ISS of 27.3±10.1 with or without multiple injuries, followed by those with craniocerebral injuries (22.4±16.2) and abdominopelvic injuries (21.5±10.1; p=0.018). A univariate analysis of survivors and non-survivors revealed significant differences for age, RTS, ISS, major injury site, multiple site injury, emergency operation, CPR at arrival, and Ps from TRISS. In a multivariate analysis, age ≥55, ISS ≥16, major craniocerebral injury, CPR at arrival, and Ps <25% from TRISS are independent predictors of trauma mortality. These results are detailed in Table 6.
Table 6.
Independent Mortality Predictors of Trauma Patients Admitted to Hospital
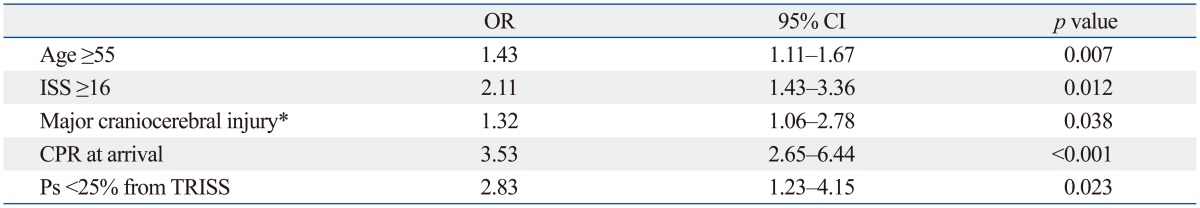
ISS, Injury Severity Score; CPR, cardiopulmonary resuscitation; TRISS, trauma and injury severity score; OR, odds ratio; CI, confidence interval; Ps, probability of survival.
*Highest area of measured abbreviated injury score that led to death.
DISCUSSION
Mortality and morbidity rates for diseases in Korea have gradually decreased due to the development of medical technology, national interest in healthcare, and the enhancement of antibiotics and surgery techniques. However, the development of faster transportation and expansion of leisure activities in Korea have caused a sharp increase in the number of trauma cases. Moreover, Korea's rapid industrialization has led to an increase in injuries caused by people falling or by objects crushing or penetrating the body at industrial sites.7
In considering other studies, motor vehicle accidents and injuries from falling seem to occur more often with men than with women, as stated by WHO3 and Moshiro, et al.8 Such can be inferred by the more prominent social activities of men in comparison to those of women, and as a result, men are more prone to vehicle and work related accidents. Fig. 1 shows the three-point-peak progress for those of ages 10 or younger, 21-50, and 61 or older. It can be presumed that trauma under the age of 10 is dominated by the carelessness of children, whereas trauma between the ages of 21 to 50 is dominated by an increasing number of motor vehicle accidents or work related accidents. It can also be inferred that the increasing trauma after the age of 61 is due to the weakening of the body and lack of attentiveness. The distribution of trauma according to age shown in this study is similar with that of other studies.9,10
Of the total number of patients who visited the emergency center, 56.0% of patients were discharged by the emergency physician after primary treatment. This phenomenon may be attributable to the well-developed health insurance system in Korea, which allows for visits to easily accessible emergency centers at a relatively low cost; thus, our trauma registry contained more minor trauma injuries than other data.11 Although some trauma patients required hospitalization at the emergency center, 15.6% of these patients opted to transfer, as they lived in different region or wanted to move to more renowned hospital. Such cases are due to the distinct features of the region in which our hospital is located, given the surrounding area is ideal for holiday trips and leisure activities; there are also few general hospitals and university-affiliated hospitals in the province. Therefore, when accidents occur, regardless of where the patients originally came from, the primary care is carried out by our emergency center. Furthermore, there is an unusual behavior common to many Koreans to tend to transfer to famous general hospitals in the metropolitan region.
Most of the trauma mechanisms in our data were classified as blunt trauma, slip-and-fall-down injuries, and vehicle related accidents (90.8%). Similarly, slip-and-fall-down injuries and vehicle associated injuries tend to be dominant, as stated by Bulut, et al.12 and Lallier, et al.13 Motor vehicle accidents are among the highest leading causes of death and disability and are a major cause of trauma patients in public health. Drunk driving, drowsy driving, and careless driving are several examples of the causes of motor vehicle accidents, and all of them are prominent in young men and women in general.14,15 Slip-and-fall-down injuries are also among the highest leading causes of blunt trauma; these types of injuries are caused by carelessness or suicidal intentions.16,17 The injury mechanisms mentioned above are health problems that can definitely be prevented by safety education by promoting a safe environment and continuing health education.
Globally, trauma is one of the major causes of death and is especially prominent at a young age.18,19 The first research on death by trauma is a paper written by Baker, et al.20 in 1980 on the epidemiology of death by trauma in San Francisco. According to the results presented in more recent papers, an annual 5.8 million deaths are caused by trauma, and in 2020, this figure is expected to rise up to 8.4 million deaths annually.21 When looking at WHO data from 2007, deaths caused by trauma constitute 9% of total annual deaths.22 Excluding in-hospital deaths in our data, early trauma mortality was 3.0% (146 of 4815 patients). Additionally, overall mortality was 5.6% (268 of 4815) among admitted patients. The results are similar to those of Sogut, et al.23 (4%) and Sanddal, et al.24 (7%). When the data from our hospital was organized by major cause of death, craniocerebral injury accounted for 42.2% of deaths, thoracic injury accounted for 33.6%, and abdominopelvic injury accounted for 24.2%. This is similar to data collected from trauma patients who expired after hospitalization; Sogut, et al.23 stated that 84% of total patients had craniocerebral injuries (p<0.01) as accompanying damage, and 43.5% died of thoracic injury (p<0.01). However, that study involved multiple response data, while our data checked only the most severe single injury that led to death.
Also, in our data collected from non-survivors, we found that the highest ISS for thoracic injury was 27.3±10.1. This score compared thoracic injury to other injuries and was statistically high in non-survivors. However, in contrast to the high ISS score for thoracic injury, Table 3 shows that major thoracic injury was the least common injury. In most accidents, patients were vulnerable to head trauma, increasing the possibility of craniocerebral injuries and severe outcomes. Moreover, although there was a high rate of abdominal injuries due to the soft abdominal wall and the susceptibility of solid organs to undergo sudden acceleration and deceleration, the development of damage control surgery, advanced resuscitation, swift angiography, and less invasive techniques have lowered the mortality rate of abdominal injury. Generally, craniocerebral injury does rank highest among causes of death by trauma; however, thoracic injury also ranks high with 25% mortality and constitutes 50% of fatalities of all traffic accidents,25 thus holding significance and requiring a high degree of attention in patients with major thoracic injuries. However, excluding trauma deaths, many thoracic injuries are of moderate severity due to the stiffness of the thoracic cage and few solid organs. Additionally, most thoracic trauma is treated conservatively with tube thoracostomy and rarely requires surgical intervention.26 This explanation reveals why the number of major thoracic injury patients were small in our data. In the past, trauma in Korea was merely a part of a wide range of surgical fields; however, many general surgeons have recently specialized in trauma and have made efforts to increase survival with prompt life-saving surgery, such as damage control surgery. Yet due to high craniocerebral and thoracic trauma mortality rates, neurosurgeons, thoracic and cardiovascular surgeons, and even orthopedic surgeons must concentrate on trauma dominantly, and these certified trauma surgeons are essential in supporting a multi-disciplinary trauma team approach in the emergency center to decrease trauma mortality rates.
Tan, et al.27 revealed that increasing age was a risk factor for mortality after trauma, and Agalar, et al.28 states that trauma mortality has significant relations with age, ISS, and revised trauma score. In our study, ages ≥55, ISS ≥16, major craniocerebral injury, CPR at arrival, and Ps <25% from TRISS were independent risk factors for trauma mortality. Old age, ISS above 15, and severe craniocerebral injury have already been established as predictors of mortality.23,26,27 Furthermore, CPR at arrival and Ps from TRISS lower than 25% can be easily predictable factors for trauma mortality. According to Ps values calculated from TRISS, our center showed 27.6% mortality in those with a survival probability of more than 75%. This finding may be explained by the fact that about half of deaths occurred in-hospital, and although most died due to the trauma, some suffered trauma-related complications such as septic shock, pneumonia, or acute respiratory distress syndrome in the treatment period, which may have contributed to the increase in mortality despite the high probability of survival. Unusually, the interval from accident to arrival at the emergency center was longer in survivors than non-survivors, differing from the results of other data.23 Most life-threatening patients were transported to our emergency center directly; however, some vital-stable patients were transported to our emergency center from other local hospitals after physical examinations, laboratory tests, and image studies. Although some critical patients were originally taken to local hospitals, after image or laboratory studies, they were transported to our emergency center for further definitive treatment. This delay in arrival is the result of a lack of education in patient triage when at an accident location. Continuous education of proper transportation for emergency transport systems will shorten this delay.
The authors intend to improve treatment and prevent of trauma death by analyzing the results of treatments and causes of trauma-related deaths. In order to enhance the quality of treatment for severe trauma patients, regional trauma centers have been designated and are currently being built in Korea. However, in addition to the need for the development of such trauma centers, software is also required to improve rapid transport, rapid sequence management, effective trauma team approaches (involving general surgeons, thoracic and cardiovascular surgeons, neurosurgeons and orthopedic surgeons), and constant education. Additionally, a shared trauma registry system for epidemiology is required, which will improve the quality of trauma centers; however, the data collection must be standardized, valid, and reliable.
One of the limitations of this study is that the study was not carried out in multiple centers but was limited to one regional emergency center for 3 years; thus, the sample and term were somewhat limited. Also, patients who were dead on arrival and those who expired during CPR should have been considered for major trauma outcome studies taking into consideration autopsy results, operation opinions, and radiation diagnoses; however, autopsy in Korea is very confined, and though limited, causes of deaths have been revealed by doctors of emergency departments and trauma surgeons in discussion. One final limit is the fact that deaths outside of the emergency center such as discharge against advice have not been accounted for in this study.
In conclusion, our results show that injuries of trauma patients are caused mainly by blunt force, falls, and motor vehicle accidents. Major injury sites were on the extremities of most trauma patients. Additionally, the most common cause of trauma mortality was craniocerebral injury. However, the mean ISS of trauma death for thoracic injury ranked high. Finally, ages ≥55, ISS ≥16, severe craniocerebral injury, CPR at arrival, and low Ps (<25%) from TRISS were associated with trauma-related death and require careful surveillance in order to identify patients who are vulnerable to death. Finally, rapid transport, rapid sequence management, effective trauma team approaches, constant education, and a standardized trauma registry may decrease trauma-related deaths.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Gross CP, Anderson GF, Powe NR. The relation between funding by the National Institutes of Health and the burden of disease. N Engl J Med. 1999;340:1881–1887. doi: 10.1056/NEJM199906173402406. [DOI] [PubMed] [Google Scholar]
- 2.Laxminarayan R, Mills AJ, Breman JG, Measham AR, Alleyne G, Claeson M, et al. Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006;367:1193–1208. doi: 10.1016/S0140-6736(06)68440-7. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. The World Health Report 2003: Shaping the Future. Geneva: World Health Organization; 2003. [Google Scholar]
- 4.National Emergency Medical Center. Annual Report of Emergency Medicine. Seoul: Ministry for Health, Welfare and Family Affairs; 2007-2011. [Google Scholar]
- 5.Lagarde E. Road traffic injury is an escalating burden in Africa and deserves proportionate research efforts. PLoS Med. 2007;4:e170. doi: 10.1371/journal.pmed.0040170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hofman K, Primack A, Keusch G, Hrynkow S. Addressing the growing burden of trauma and injury in low- and middle-income countries. Am J Public Health. 2005;95:13–17. doi: 10.2105/AJPH.2004.039354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Police Agency. Annual report of traffic accident in Korea 2006. Seoul: National Police Agency; 2006. [Google Scholar]
- 8.Moshiro C, Heuch I, Astrøm AN, Setel P, Hemed Y, Kvåle G. Injury morbidity in an urban and a rural area in Tanzania: an epidemiological survey. BMC Public Health. 2005;5:11. doi: 10.1186/1471-2458-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Demircan A, Keles A, Gurbuz N, Bildik F, Aygencel SG, Dogan NO, et al. Forensic emergency medicine - six-year experience of 13823 cases in a university emergency department. Turk J Med Sci. 2008;38:567–575. [Google Scholar]
- 10.Mishra B, Sinha Mishra ND, Sukhla S, Sinha A. Epidemiological study of road traffic accident cases from Western Nepal. Indian J Community Med. 2010;35:115–121. doi: 10.4103/0970-0218.62568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polinder S, Haagsma JA, Toet H, van Beeck EF. Epidemiological burden of minor, major and fatal trauma in a national injury pyramid. Br J Surg. 2012;99(Suppl 1):114–121. doi: 10.1002/bjs.7708. [DOI] [PubMed] [Google Scholar]
- 12.Bulut M, Koksal O, Korkmaz A, Turan M, Ozguc H. Childhood falls: characteristics, outcome, and comparison of the Injury Severity Score and New Injury Severity Score. Emerg Med J. 2006;23:540–545. doi: 10.1136/emj.2005.029439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lallier M, Bouchard S, St-Vil D, Dupont J, Tucci M. Falls from heights among children: a retrospective review. J Pediatr Surg. 1999;34:1060–1063. doi: 10.1016/s0022-3468(99)90564-x. [DOI] [PubMed] [Google Scholar]
- 14.Hingson R, Winter M. Epidemiology and consequences of drinking and driving. Alcohol Res Health. 2003;27:63–78. [PMC free article] [PubMed] [Google Scholar]
- 15.Matthews ML, Moran AR. Age differences in male drivers’ perception of accident risk: the role of perceived driving ability. Accid Anal Prev. 1986;18:299–313. doi: 10.1016/0001-4575(86)90044-8. [DOI] [PubMed] [Google Scholar]
- 16.Murray CJL, Lopez AD. Global and regional descriptive epidemiology of disability: incidence, prevalence, health expectancies and years lived with disability. In: Murray CJL, Lopez AD, editors. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Boston: Harvard University Press; 1996. pp. 201–246. [Google Scholar]
- 17.Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- 18.Mohan D. Childhood injuries in India: extent of the problem and strategies for control. Indian J Pediatr. 1986;53:607–615. doi: 10.1007/BF02748664. [DOI] [PubMed] [Google Scholar]
- 19.Elechi EN, Etawo SU. Pilot study of injured patients seen in the University of Port Harcourt Teaching Hospital, Nigeria. Injury. 1990;21:234–238. doi: 10.1016/0020-1383(90)90011-i. [DOI] [PubMed] [Google Scholar]
- 20.Baker CC, Oppenheimer L, Stephens B, Lewis FR, Trunkey DD. Epidemiology of trauma deaths. Am J Surg. 1980;140:144–150. doi: 10.1016/0002-9610(80)90431-6. [DOI] [PubMed] [Google Scholar]
- 21.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Preventing Injuries and Violence. A Guide for Ministries of Health. Geneva: World Health Organization; 2007. pp. 6–9. [Google Scholar]
- 23.Sogut O, Sayhan MB, Gokdemir MT, Boleken ME, Al B, Kose R, et al. Analysis of Hospital Mortality and Epidemiology in Trauma Patient: A Multi-Center Study. J Curr Surg. 2011;1:19–24. [Google Scholar]
- 24.Sanddal TL, Esposito TJ, Whitney JR, Hartford D, Taillac PP, Mann NC, et al. Analysis of preventable trauma deaths and opportunities for trauma care improvement in utah. J Trauma. 2011;70:970–977. doi: 10.1097/TA.0b013e3181fec9ba. [DOI] [PubMed] [Google Scholar]
- 25.Blair E, Topuzlu C, Davis JH. Delayed or missed diagnosis in blunt chest trauma. J Trauma. 1971;11:129–145. doi: 10.1097/00005373-197102000-00005. [DOI] [PubMed] [Google Scholar]
- 26.LoCicero J, 3rd, Mattox KL. Epidemiology of chest trauma. Surg Clin North Am. 1989;69:15–19. doi: 10.1016/s0039-6109(16)44730-4. [DOI] [PubMed] [Google Scholar]
- 27.Tan WT, Choy JM, Foo JM. A 5-year profile of trauma admissions to the surgical intensive care unit of a tertiary hospital in Singapore. Ann Acad Med Singapore. 2010;39:363–367. [PubMed] [Google Scholar]
- 28.Agalar F, Cakmakci M, Sayek I. Factors effecting mortality in urban vertical free falls: evaluation of 180 cases. Int Surg. 1999;84:271–274. [PubMed] [Google Scholar]