Abstract
Purpose
This study aimed to evaluate the effects of a case management program for diabetics, using a pre-post comparison design.
Materials and Methods
The study population comprised 6007 diabetics who received case management intervention in 2006 and were sampled nationwide in Korea. Before and after the intervention, the study population answered questions regarding their knowledge of diabetes, self-management ability, and health behaviors. Body mass index (BMI) was also calculated. Healthcare service utilization for diabetes was extracted from health insurance claim data from 2005 to 2007.
Results
The case management program significantly improved the study population's knowledge of diabetes and ability to self-manage nutrition, blood glucose monitoring, foot and oral care, and medications. This program also significantly changed the study population's health behaviors regarding smoking, alcohol drinking, and exercise, and BMI was positively affected. In the over-serviced subgroup, there was a significant decrease in the number of consultations (mean=7.0; SD=19.5) after intervention. Conversely, in the under-serviced subgroup, there was a significant increase in the number of consultations (mean=3.2; SD=7.9) and the days of prescribed medication (mean=66.4; SD=120.3) after intervention.
Conclusion
This study showed that the case management program led the study population to improve their knowledge, self-management ability, health behaviors, and utilization of health care. It is necessary in future studies to evaluate the appropriateness of healthcare usage and clinical outcome by using a control group to determine the direct effectiveness of this case management program.
Keywords: Case management, diabetes, intervention, Korea
INTRODUCTION
Diabetes is a major, growing health problem in the Korean population, due to its increased morbidity, mortality, and economic costs. Diabetes has been ranked as Korea's fifth leading cause of death after cancer, cerebrovascular diseases, cardiovascular diseases, and suicide, with a mortality rate of 21.5 per 100000 people in 2011.1 Diabetes-related medical expenditures accounted for 19.2% of all medical expenditures funded through the National Health Insurance Service (NHIS) in Korea in 2003.2 Thus, diabetes is not only a serious public health problem, but also a major burden for the national health insurance budget in Korea.
However, diabetes management in Korea is generally poor. Only 16.8% of Korean patients with diabetes reported self-monitoring their blood glucose, and about 40% had suboptimal glycemic control.3 In addition, about half (52.9%) of patients with diabetes in Korea sought medical attention every year.2
In order to provide information on how patients could manage their diabetes, a case management program for diabetes was launched in 2002 as a pilot project, was adopted as a full program in 2004, and has been extended nationwide in Korea since 2006. The program provides chronically ill patients with guidance and advice on how to manage their conditions and use healthcare services appropriately. It aims to help consumers make better-informed decisions when practicing self-management activities and using healthcare services. The program also aims to prevent diabetic complications and excess costs due to unreasonable use of healthcare services.4,5
Recently, the hypertension case management program of the NHIS was evaluated and found to improve lifestyle and reduce blood pressure within the case management group.6 However, the case management program for diabetes was not evaluated. We aimed to estimate the changes in knowledge of diabetes, self-management skills, health behaviors, body mass index (BMI), and changes in healthcare service utilization in order to evaluate the effects of this case management program for people with diabetes.
MATERIALS AND METHODS
Structure and process of the NHIS case management program for diabetes
Interventions were carried out using a 12-week plan for complex patients, consisting of four visits and two telephone calls, or an 8-week plan for under-serviced and uncomplicated patients, which consisted of three contacts made by visits or telephone calls. However, the instruction manual allowed case managers to increase or decrease the number of contacts or to extend or shorten the length of the intervention by 1 week, depending on patient needs. The average length of the intervention program was 10.7 weeks (SD=4.9), and 72.9% of patients received the interventions for 7-13 weeks. Of 413 case managers, including 33 nurses and 177 social workers, only 52.1% had qualifications related to the job. The detailed structure and process of case management, such as the selection and assessment of subjects, selection of case management issues, intervention, and evaluation were described in a previous study.6
Study design and subjects
We adopted a pre-post design to estimate the effects of the case management program between baseline and post-intervention.
In Korea, national health insurance is a social insurance scheme. All Koreans join a national insurance program as a form of health insurance or medical aid. All medical institutions have also been registered with the medical insurance program. After treatment of diseases that are covered by national health insurance, the medical institutions (hospitals or private clinics) submit insurance claims to the Health Insurance Review & Assessment Service (HIRA). Then, following review and assessment of these claims, HIRA makes payments to the healthcare institutions. These data from HIRA were shared with NHIS.
There were 985707 diabetic patients in the NHIS database in 2006. Of them, 6519 subjects were selected as an intervention group by case managers using a convenience sampling, and these subjects received the case management program from January 2006 to December 2006. Among these subjects, 401 did not complete the intervention program of diabetic case management, and 111 did not maintain eligibility for two years over the observation period. Therefore, 6007 subjects were selected as the study population. Inclusion criteria for the study population were defined to include those who were diagnosed with diabetes in the NHIS database, had completed the intervention program, and had maintained eligibility for national health insurance for two years.
Based on the International Classification of Diseases-10, data for patients with codes E10 (insulin-dependent diabetes mellitus), E11 (non-insulin-dependent diabetes mellitus), E12 (malnutrition-related diabetes mellitus), E13 (other specified diabetes mellitus), and E14 (unspecified diabetes mellitus) were extracted from the NHIS claim database and health check-up database.
Data collection
Data for the pre-post questionnaire and the utilization of healthcare services were extracted from the NHIS administrative system. The questionnaire concerned demographic information, knowledge of diabetes, self-management activities, health behaviors, height, and weight. Demographic information consisted of gender, age, place of residence, marital status, education level, and insurance type. Knowledge of diabetes was assessed with ten items (Supplementary Table 1, only online); these questions were designed to evaluate patient knowledge of diabetes and its management. Total scores for knowledge of diabetes ranged from 1 to 10. Each question was scored as 1 for a correct answer and 0 for a wrong or "don't know" answer. Self-management activities included nutrition management, monitoring blood glucose, foot care, oral care, and medication management (Supplementary Table 2, only online). Fifteen items were used to evaluate patients' abilities to self-manage in five domains: nutritional management (four items), monitoring blood glucose (three items), foot care (three items), oral care (two items), and medication management (three items). Each self-management question was scaled using a five-point Likert-type scale, with 5 indicating "always," 4 indicating "often," 3 indicating "half of the time," 2 indicating "sometimes," and 1 indicating "never." However, for one question ("Do you take any snacks between meals?"), the scale for nutritional management was reversed, with 1 indicating "always" and 5 indicating "never." Health behaviors included smoking, alcohol consumption, and exercise. To assess the subjects' health behaviors, three questions were asked about smoking, alcoholic drinking, and regular exercises. Height and weight were also recorded to allow calculation of BMI. BMI (unit: kg/m2) was classified into five categories, according to the criteria of WHO Western Pacific Region: underweight (BMI <18.5), normal or healthy weight (BMI 18.5-23.0), overweight (BMI 23.0-25.0), obese I (BMI 25.0-30.0), and obese II (BMI >30.0). This questionnaire was first developed in 2002 by a research and development team that included 19 Korean professors, including representatives from medicine, nursing, and public health. After the developed questionnaire had been used for a year with diabetic patients in the NHIS case management program, it was validity-tested for content and reliability.7
To evaluate changes in the utilization of healthcare services, NHIS claims data were extracted from the health insurance claim database during the period from January 1, 2005 to December 31, 2007, based on the dates during which patients visited the clinics. The observation period differed in individual cases according to the days on which patients commenced the case management program, and data were therefore collected and computed individually. If a patient began the program on May 4, 2006, claims data were collected for that patient during the period from May 4, 2005 to May 3, 2006 for the pre-intervention observation and from May 4, 2006 to May 3, 2007 for the post-intervention observation. The dates of patients' initial visits for the case management program ranged from January 10, 2006 to December 29, 2006. Indicators of healthcare services utilization for diabetes were the number of ambulatory consultations, days of medication prescribed, and medical expenses in one year. Ambulatory consultations were consultations with doctors in a single year, occurring in medical clinics, outpatient departments in hospitals, and community health centers. Days of prescribed medication were the cumulative days of medication prescribed by doctors in one year. Medical expenses were the total expenses covered by the National Health Insurance Medical Benefit Scheme, the Pharmaceutical Benefit Scheme, and the Medical Treatment Material Benefit Scheme in one year, including co-payments.
We classified the study population into three subgroups according to the number of ambulatory consultations and days of medication prescribed per year before intervention. Based on the previous study,7 the under-serviced subgroup had 3-11 consultations per year, the over-serviced subgroup had more than 27 consultations, and the others were the "average" subgroup, regardless of the days of medication prescribed per year.
Data analysis
Statistical analyses were performed using SAS software (ver. 9.1, SAS Institute, Cary, NC, USA). First, we presented the general characteristics of the study population and the general population under national health insurance. Next, a paired t-test was used for pre/post comparisons within each group, and the McNemar test was used for ordinary variables. A p value <0.05 was considered statistically significant.
Ethics statement
This study was reviewed and approved by the Faculty [of Health Sciences] Human Ethics Committee at La Trobe University (FHEC07/147).
RESULTS
General characteristics of the subjects are shown in Table 1; 54% were females, and the mean age was 60.4 (SD=9.2) years. Most subjects were married (83.2%), and education levels varied: 11.5% had no education, 29.6% graduated from elementary school, 20.3% graduated from middle school, 28.0% graduated from high school, and only 8.1% were at the tertiary level. The residency demographics of the study population were metropolitan (39.6%), city (42.5%), and rural (17.9%). In addition, 45.5% of the study population remembered their blood glucose level at diagnosis, and 43.9% had diabetic complications.
Table 1.
General Characteristics of the Study Population
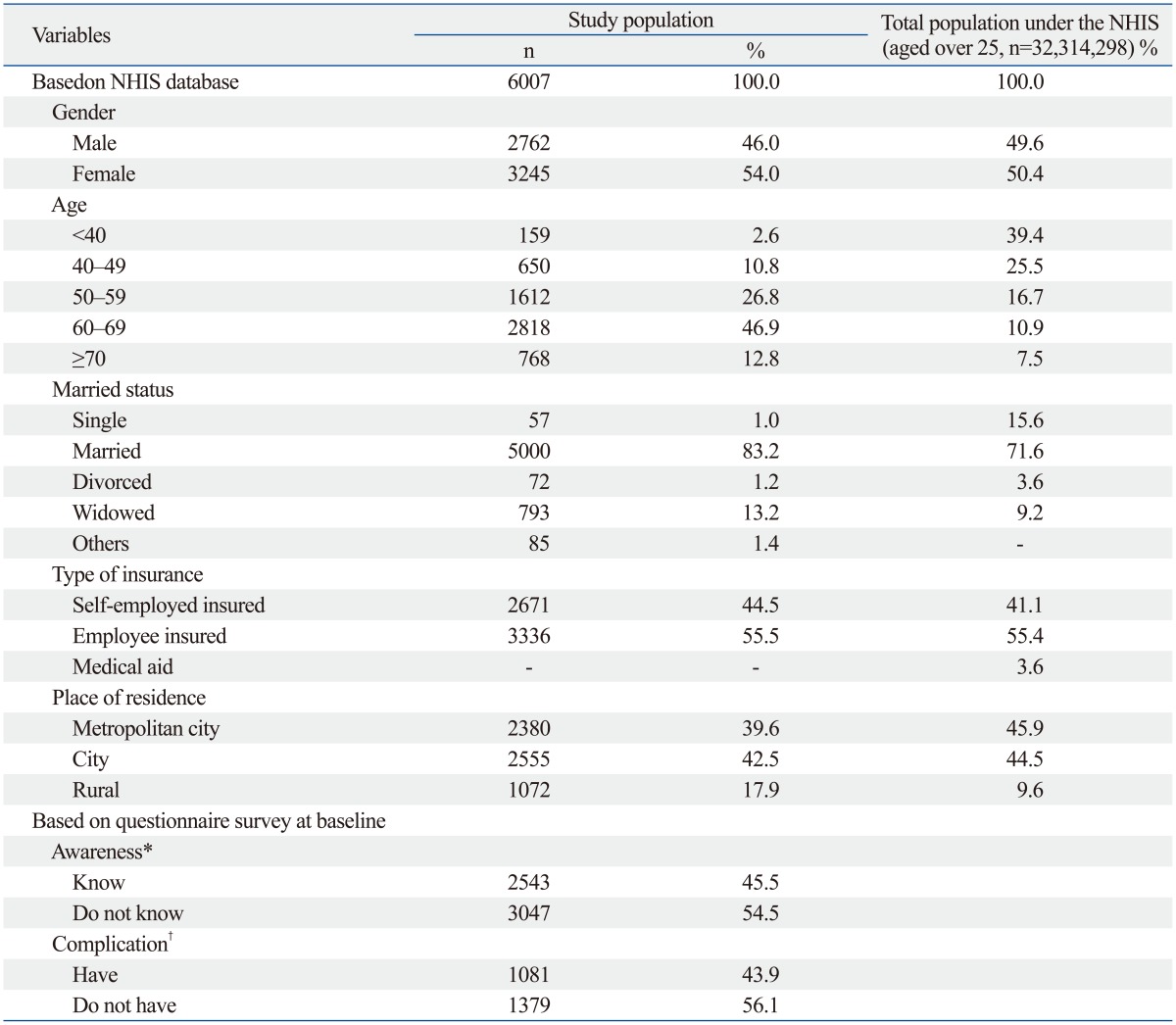
NHIS, National Health Insurance Service.
*Awareness: Do you remember your blood glucose levels at initial diagnosis?
†Complication: Do you have diabetic complications? If you do, what diseases do you have?
Changes in scores for knowledge and management of diabetes are shown in Table 2. Knowledge scores increased from 5.66 (SD=2.54) at baseline to 8.35 (SD=1.94) after the intervention (p<0.001). Nutrition scores also increased from 14.07 to 15.46 (p<0.001). The self-monitoring score for blood glucose increased significantly from 6.75 (SD=3.35) to 8.30 (SD=3.28; p<0.001). The foot care score increased from 9.42 (SD=3.16) to 11.52 (SD=2.52; p<0.001). The oral care score increased from 5.74 (SD=2.04) to 6.50 (SD=1.88; p<0.001). The score for self-management of medication increased significantly from 12.18 (SD=3.81) to 13.00 (SD=3.40; p<0.001).
Table 2.
Comparison of Knowledge and Management for Diabetes at Baseline and after Intervention
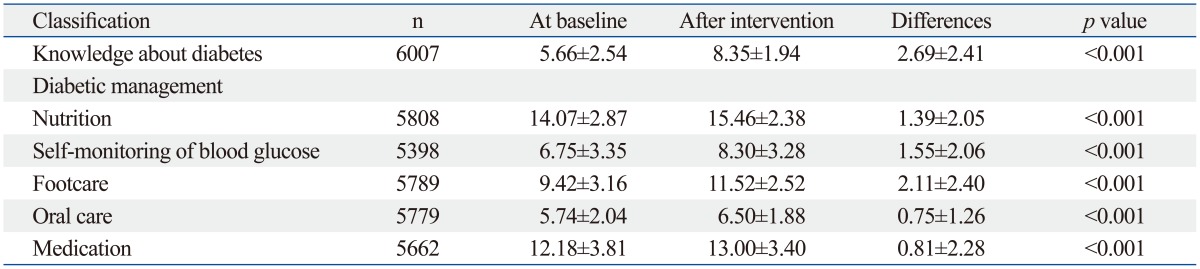
p values from paired t-test.
The proportion of daily smokers was 35.8% in males and 3.4% in females at baseline, and 2.5% of males (n=70, 7.1% of male smokers) and 0.2% (n=8, 7.1% of female smokers) of females had stopped smoking after intervention (males: p<0.001; females: p=0.005). The proportion of alcoholic drinkers among men was greater than among women (51.0% of males, 8.3% of females) at baseline. The percentage abstaining from alcohol drinking was 4.7% in males (n=130, 9.3% of male drinkers) and 1.1% in females (n=37, 13.8% of female drinkers) after intervention (males: p<0.001; females: p<0.001). The proportion of those who exercised increased from 64.6% to 78.7% in males (p<0.001) and from 56.6% to 78.7% in females (p<0.001) after intervention. About half (n=1121) of the study population who did not exercise started to do regular exercise after the intervention (Table 3).
Table 3.
Comparison of Health Behaviors at Baseline and after Intervention
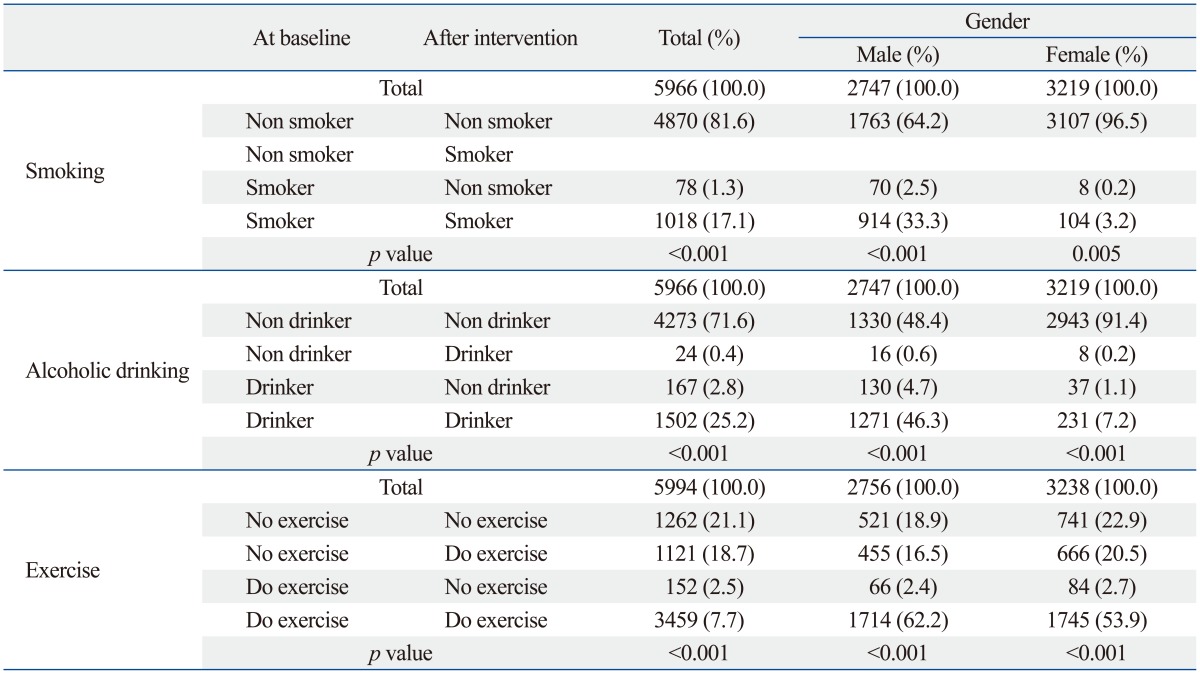
p values from the McNemar test.
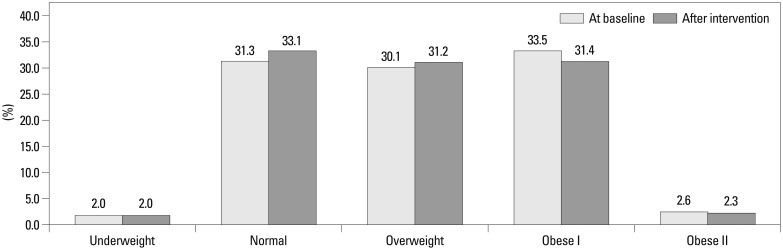
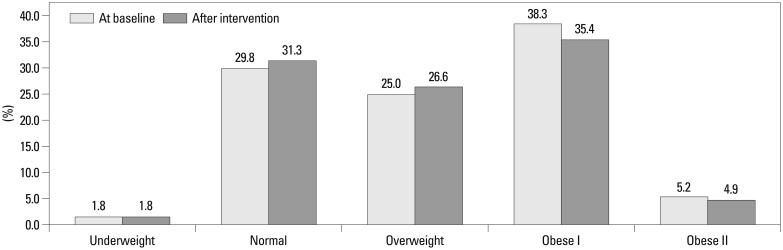
BMI was significantly reduced from 24.13 kg/m2 (SD= 2.85) to 23.98 kg/m2 (SD=2.78) in males and from 24.60 kg/m2 (SD=3.25) to 24.46 kg/m2 (SD=3.17) in females after intervention (males: p<0.001; females: p<0.001). The proportion of obese I and obese II patients significantly decreased from 33.5% to 31.4% (obese I) and from 2.6% to 2.3% (obese II) in men and from 38.3% to 35.4% (obese I) and from 5.2% to 4.9% (obese II) in women after the intervention (males: p<0.001; p<0.001) (Figs. 1 and 2).
Fig. 1.
Distribution of body mass index at baseline and after intervention for males. There was a statistical significance between the two intervals in the McNemar test (χ2=78.62; df=10; p<0.001; n=2752).
Fig. 2.
Distribution of body mass index at baseline and after intervention for females. There was a statistical significance between the two intervals in the McNemar test (χ2=132.23; df=10; p<0.001; n=3236).
Of the three subgroups, the usages of diabetic-specific healthcare services among two of the subgroups were contrary to each other (Table 4). In the under-serviced subgroup, there was a significant increase in the number of consultations (mean=3.2; SD=7.9), days of prescribed medication (mean=66.4; SD=120.3), and medical expenses (mean=287800 KRW; SD=881400 KRW) after intervention (all p<0.001). Conversely, in the over-serviced subgroup, there was a significant decrease in the number of consultations (mean=7.0; SD=19.5) and medical expenses (mean=602100 KRW; SD=2540200 KRW) after intervention (all p<0.001).
Table 4.
Comparison of Healthcare Utilization for Diabetic Specific Services at Baseline and after Intervention
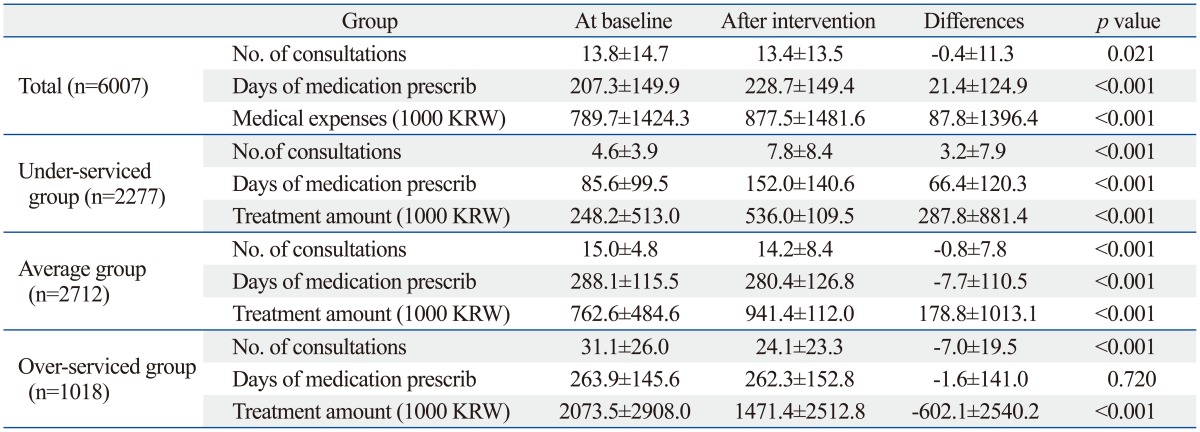
p values from paired t-test.
DISCUSSION
Our aim was to provide evidence as to how well the current program was working and to show its effects by estimating changes in diabetics' knowledge, self-management ability, health behaviors, such as smoking, alcoholic drinking, or exercise, BMI, and the utilization of healthcare services for diabetes.
First, the NHIS case management program improved patients' knowledge and self-management abilities for nutrition, blood glucose monitoring, foot care, oral care, and medication. These findings are consistent with previous studies, which found that supporting patients with diabetes produced positive health outcomes. Fan and Sidani8 concluded from a meta-analysis that diabetes self-management education interventions were effective in improving knowledge, behavior, and metabolic control outcomes in adult patients with type-2 diabetes. Norris, et al.9 reported from their systematic review that self-management training in type-2 diabetes had short-term positive effects of less than six months for knowledge, frequency, and accuracy of self-monitoring blood glucose, self-related dietary habits, and glycemic control. Lim, et al.10 reported that better-educated patients were more likely to monitor their blood glucose.
Second, this program reduced smoking and alcohol drinking rates and increased exercise rates significantly, in addition to significantly reducing BMI. Deakin, et al.11 had the same results as this study and showed that an expert-patient program in the UK made significant improvements in physical activity levels, BMI, and waist circumference when compared with control patients. People who are obese and exercise are more likely to make a greater change in BMI than those who are not obese or who do not exercise. However, Glasgow's study showed that BMI was not significantly different between intervention and control,12 and Norris, et al.13 found insufficient evidence for determining the effectiveness of disease management on BMI. Though the change in BMI has statistical significance, it is difficult to determine whether this small change has public or clinical significance, as this study is a pre-post comparison and has a large sample size. In order to overcome this weakness, it is necessary to compare the outcome of the intervention group with a control group.
Third, this program affected healthcare utilization. The use of diabetic-specific services by the over-serviced subgroup decreased significantly after the interventions, while the under-serviced subgroup showed a significant increase in utilization. International evidence for the impact of programs on the utilization of healthcare services is inconsistent. Several previous studies demonstrated a reduction in medical service utilization. A Spanish diabetes self-management program showed fewer emergency room visits and a trend towards fewer visits to physicians at 6 months.14 Additionally, Berg and Wadhwa15 suggested that providing diabetes disease management in a community-based setting was associated with a substantial reduction in medical-service utilization. However, utilization of healthcare services remained unchanged in the lay-led self-management programs heavily promoted by the UK Department of Health as part of a drive to reduce usage of acute healthcare services.16,17,18,19 Foster, et al.20 and Griffiths, et al.21 argued that if lay-led self-management programs aim to reduce healthcare resource usage, there is insufficient evidence to justify widespread lay-led self-management interventions. However, the NHIS case management program encouraged using healthcare services for diabetes, particularly for patients with under-average or average service usage in the short term. This difference between the studies may result from differences in the participants. Most Korean participants were under-serviced (37.9%) and average-serviced patients (45.1%); however, the participants in Berg and Wadhwa's14 study were high users of inpatient services due to the health plan's selection of patients with the most severe cases of diabetes.
Case management generally aims to provide cost efficient and effective care through the coordination of required services. The Case Management Society of America defines case management as "a collaborative process, which assesses, plans, implements, coordinates, monitors and evaluates options and services to meet an individual's health needs through communications and available resources to promote quality and cost-effective outcome."22 In the same manner, the NHIS case management program provides the chronically ill with information and guidance on how to manage their conditions and use healthcare services appropriately. It aims to help consumers make better-informed decisions for choosing healthcare services and practicing self-management. The ultimate goal of this program is to prevent or delay disease complications and excess costs.5,7 Meanwhile, the practice of case management depends largely on the type and structure of the organization that operates the program and varies across the health and social care sectors.23,24 In the UK, case management is mainly a community-based model, while a hospital-based model is predominant in the US.25 However, the case management program of the NHIS is different from those of other countries in its practice and personnel. First, this program is a virtual patient-support program, which was intended to promote healthy behaviors, encourage rational use of healthcare services, and reduce healthcare costs. The content and approaches of the NHIS case management program are closer to self-management interventions than to case management, and its clients are typically living in the community and are not highly complex patients. Case managers set a care plan with patients, which is an action plan for the intervention that is designed to achieve the goals of changing health behaviors and reducing risk factors; it does not include a treatment plan. The NHIS sets target populations, prioritizing people who are under-serviced or over-serviced, and intends to involve coordinating resources available in the communities and to encourage appropriate use of healthcare services for better long-term outcomes. Second, the case managers of this program in Korea work only with patients. The case managers do not coordinate healthcare services or formally collaborate with healthcare providers, which is attributable to the fact that healthcare providers under a fee-for-service system are not motivated to provide continuous or comprehensive care for people with chronic diseases. Thus, the services of the case management program are not integrated into the mainstream healthcare delivery system. Physicians are an important source of motivation and feedback, and their involvement may improve diabetics' behavioral changes. Therefore, a method for integrating case management intervention into an existing healthcare system also needs to be addressed in further research.
The strength of this study is that it is a large study involving a nationwide program and uses not only the subjective answers of the questionnaire but also objective indicators such as healthcare service utilization. However, this study has several limitations. First, the design of the study was a pre-post test; hence, there was no control group with which comparisons of outcomes could be made. The resources available for the study did not allow for a randomized control trial, nor was a randomized control trial considered practical. Additionally, this study had to use data generated from existing administrative data of the Korean NHIS, as well as self-reports from the study population. Second, the study population consisted of patients who consented to participate in the case management program. This recruitment method means that the participants were those who had already paid more attention to their health and showed some elevated motivation for change. Thus, the results of this study may be more reflective of people actively engaged in self-care and seeking social support for their diabetes. In conclusion, this study showed that a case management program for diabetics led the study population to improve their knowledge, self-management ability, health behaviors, BMI, and health care usage. The results indicate that the NHIS case management program for diabetes is a useful intervention for diabetics. However, the effectiveness of case management should be confirmed in rigorously-designed and prospective trials in order to evaluate the appropriateness of healthcare usage and clinical outcome which will in turn show the direct effectiveness of a case management program by including a control group.
Footnotes
The authors have no financial conflicts of interest.
Supplementary Materials
Patients' Responses to Knowledge about Diabetes
Patients' Responses to Nutrition Management Test Items (Unit: %)
References
- 1.Korean Statistical Information Services. Cause of Death in 2012. [accessed on 2013 April 10]. Available at: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1012.
- 2.Korean Diabetes Association, Health Insurance Review & Assessment Service. Report of Task Force Team for Basic Statistical Study of Korean Diabetes Mellitus: Diabetes in Korea 2007. Seoul, Korea: Goldfishery; 2008. [Google Scholar]
- 3.Rhee SY, Kim YS, Oh S, Choi WH, Park JE, Jeong WJ. Diabcare Asia 2001--Korea country report on outcome data and analysis. Korean J Intern Med. 2005;20:48–54. doi: 10.3904/kjim.2005.20.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim EY, Kim YM, Kim CH, Kim HG, So AY, Shin SA, et al. Theories and practice of community-based case management for chronic disease. Seoul, Korea: Hyunmoonsa; 2008. [Google Scholar]
- 5.National Health Insurance Service. The manual of case management Korea National Health Insurance Service. Seoul, Korea: Saekwang Design Printing; 2005. [Google Scholar]
- 6.Kim Y, Lee K, Shin E, Kim H, June KJ. Evaluation of the hypertension disease management program in Korea. Asia Pac J Public Health. 2010;22:365–374. doi: 10.1177/1010539510361947. [DOI] [PubMed] [Google Scholar]
- 7.National Health Insurance Service. Case management program from pilot to regular business program: a study. Seoul, Korea: Saekwang Design Printing; 2004. [Google Scholar]
- 8.Fan L, Sidani S. Effectiveness of diabetes self-management education intervention elements: a meta-analysis. Can J Diabetes. 2009;33:18–26. [Google Scholar]
- 9.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 10.Lim KB, Lee R, Ko KN, Choi EY, Kim JH, Cheong YS, et al. Self-care for diabetic patients in primary care. J Korean Acad Fam Med. 2007;28:106–113. [Google Scholar]
- 11.Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabet Med. 2006;23:944–954. doi: 10.1111/j.1464-5491.2006.01906.x. [DOI] [PubMed] [Google Scholar]
- 12.Glasgow RE, La Chance PA, Toobert DJ, Brown J, Hampson SE, Riddle MC. Long-term effects and costs of brief behavioural dietary intervention for patients with diabetes delivered from the medical office. Patient Educ Couns. 1997;32:175–184. doi: 10.1016/s0738-3991(97)00039-6. [DOI] [PubMed] [Google Scholar]
- 13.Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, Jack L, et al. The effectiveness of disease and case management for people with diabetes. A systematic review. Am J Prev Med. 2002;22(4 Suppl):15–38. doi: 10.1016/s0749-3797(02)00423-3. [DOI] [PubMed] [Google Scholar]
- 14.Lorig K, Ritter PL, Villa F, Piette JD. Spanish diabetes self-management with and without automated telephone reinforcement: two randomized trials. Diabetes Care. 2008;31:408–414. doi: 10.2337/dc07-1313. [DOI] [PubMed] [Google Scholar]
- 15.Berg GD, Wadhwa S. Diabetes disease management in a community-based setting. Manag Care. 2002;11:42, 45–50. [PubMed] [Google Scholar]
- 16.Barlow JH, Turner AP, Wright CC. A randomized controlled study of the Arthritis Self-Management Programme in the UK. Health Educ Res. 2000;15:665–680. doi: 10.1093/her/15.6.665. [DOI] [PubMed] [Google Scholar]
- 17.Buszewicz M, Rait G, Griffin M, Nazareth I, Patel A, Atkinson A, et al. Self management of arthritis in primary care: randomised controlled trial. BMJ. 2006;333:879. doi: 10.1136/bmj.38965.375718.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomised controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease. Br J Gen Pract. 2005;55:831–837. [PMC free article] [PubMed] [Google Scholar]
- 19.Kennedy A, Reeves D, Bower P, Lee V, Middleton E, Richardson G, et al. The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: a pragmatic randomised controlled trial. J Epidemiol Community Health. 2007;61:254–261. doi: 10.1136/jech.2006.053538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev. 2007:CD005108. doi: 10.1002/14651858.CD005108.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Griffiths C, Foster G, Ramsay J, Eldridge S, Taylor S. How effective are expert patient (lay led) education programmes for chronic disease? BMJ. 2007;334:1254–1256. doi: 10.1136/bmj.39227.698785.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Case Management Society of America. Definition of case management. [accessed on 2012 January 14]. Available at: http://www.cmsa.org/ABOUTUS/DefinitionofCaseManagement/tabid/104/Default.aspx.
- 23.Kane RL. Changing the face of long-term care. J Aging Soc Policy. 2005;17:1–18. doi: 10.1300/J031v17n04_01. [DOI] [PubMed] [Google Scholar]
- 24.White P, Hall ME. Mapping the literature of case management nursing. J Med Libr Assoc. 2006;94(2 Suppl):E99–E106. [PMC free article] [PubMed] [Google Scholar]
- 25.Lee DT, Mackenzie AE, Dudley-Brown S, Chin TM. Case management: a review of the definitions and practices. J Adv Nurs. 1998;27:933–939. doi: 10.1046/j.1365-2648.1998.t01-1-00566.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patients' Responses to Knowledge about Diabetes
Patients' Responses to Nutrition Management Test Items (Unit: %)