Abstract
Chemotherapy-induced nausea and vomiting (CINV) is associated with a significant deterioration in quality of life. The emetogenicity of the chemotherapeutic agents, repeated chemotherapy cycles, and patient risk factors significantly influence CINV. The use of a combination of a 5-hydroxytryptamine-3 (5-HT3) receptor antagonists, dexamethasone, and a neurokinin-1 (NK-1) receptor antagonist has significantly improved the control of acute and delayed emesis in single-day chemotherapy. Palonosetron, a second generation 5-HT3 receptor antagonist with a different half-life, different binding capacity, and a different mechanism of action than the first generation 5-HT3 receptor antagonists, appears to be the most effective agent in its class. Netupitant, is a new NK-1 receptor antagonist with a high binding affinity, a long half-life of 90 hours, is metabolized by CYP3A4, and is an inhibitor of CYP3A4. NEPA is an oral fixed-dose combination of netupitant and palonosetron which has recently been employed in Phase II and Phase III clinical trials for the prevention of CINV in patients receiving moderately and highly emetogenic chemotherapy (MEC and HEC). The clinical trials demonstrated that NEPA (300 mg of netupitant plus 0.50 mg of palonosetron) significantly improved the prevention of CINV compared to the use of palonosetron alone in patients receiving either HEC or MEC. The clinical efficacy was maintained over multiple cycles of chemotherapy. NEPA (Akynzeo®) has recently been approved by the Food and Drug Administration (FDA) to treat nausea and vomiting in patients undergoing cancer chemotherapy.
Keywords: 5-HT3 receptor antagonists, NK-1 receptor antagonists, palonosetron, netupitant, chemotherapy-induced nausea and vomiting
Introduction
Chemotherapy-induced nausea and vomiting (CINV) adversely affects patients’ quality of life and may affect patients’ treatment decisions.1–3 The emetogenicity of the chemotherapy administered and specific patient characteristics such as female sex, age, and history of the amount of alcohol intake affect patients’ risk factors for CINV (Table 1).3
Table 1.
Patient-related risk factors for emesis following chemotherapy
| Major factors | Minor factors |
|---|---|
| Female | History of motion sickness |
| Age <50 years | Emesis during past pregnancy |
| History of low prior chronic alcohol intake (<1 ounce of alcohol/day) | |
| History of previous chemotherapy-induced emesis |
Significant and uncontrolled CINV may result in patients returning to the chemotherapy treatment facility 1–3 days post chemotherapy for rehydration, emesis or nausea control. If CINV cannot be controlled in an outpatient facility, patients may subsequently be treated in an emergency department or require hospitalization.1,3 Patients who have an electrolyte imbalance or those who have recently undergone surgery or radiation therapy, are at greater risk of experiencing serious complications from CINV.1–3
The use of 5-hydroxytryptamine-3 (5-HT3) receptor antagonists has improved the control of CINV.4,5 Additional improvement in the control of CINV has occurred with the use of aprepitant, the first agent available in the drug class of neurokinin-1 (NK-1) receptor antagonists,6 and olanzapine, an antipsychotic which blocks multiple neurotransmitters in the central nervous system.7–9
The primary endpoint used for studies evaluating various agents for the control of CINV has been complete response (no emesis, no use of rescue medication) over the acute (24 hours postchemotherapy), delayed (24–120 hours), and overall (0–120 hours) periods.3 The combination of a 5-HT3 receptor antagonist, dexamethasone, and a NK-1 receptor antagonist have improved the control of emesis in patients receiving either HEC or MEC over a 120-hour period following chemotherapy administration.5,6 Many of these same studies have measured nausea as a secondary endpoint, but nausea has not been well controlled.10,11
The use of effective antiemetic agents in various clinical settings has been described in established guidelines from the Multinational Association of Supportive Care in Cancer (MASCC), the European Society of Medical Oncology (ESMO),12 the American Society of Clinical Oncology (ASCO),13 and the National Comprehensive Cancer Network (NCCN).14 The purpose of this review is to define the role of a new neurokinin-1 receptor antagonist netupitant and its use in the prevention of CINV when combined with the second generation 5-HT3 receptor antagonist palonosetron.
Palonosetron: second generation serotonin (5-HT3) receptor antagonist
Palonosetron is a second generation 5-HT3 receptor antagonist which has antiemetic activity at both central and GI sites.4,5 In comparison to the first generation 5-HT3 receptor antagonists, it has a higher potency, a 30-fold higher receptor binding affinity, a significantly longer half-life, and a different molecular interaction with 5-HT3 receptors4,5,15–18 (Table 2) and may have increased efficacy in controlling delayed CINV compared to the first generation 5-HT3 receptor antagonists.4,5,15
Table 2.
5-HT3 receptor antagonists’ binding affinity and plasma half-life
| Drug | pKi [−log(Ki)] | Half-life (hours) |
|---|---|---|
| Palonosetron | 10.45 | 40 |
| Ondansetron | 8.39 | 4 |
| Granisetron | 8.91 | 9 |
| Dolasetrona | 7.60 | 7.3 |
Notes:
Half-life reported for hydrodolasetron, the active metabolite of dolasetron.
Rojas et al18 reported that palonosetron exhibited allosteric binding and positive cooperativity when binding to the 5-HT3 receptor compared to simple bimolecular binding for both granisetron and ondansetron. Rojas et al18 also suggested that palonosetron triggers 5-HT3 receptor internalization and causes prolonged inhibition of receptor function. Differences in binding and effects on receptor function may explain some differences between palonosetron and the first generation 5-HT3 receptor antagonists.4,5,15 These differences may explain palonosetron’s efficacy in delayed CINV compared to the first generation receptor antagonists.4,5,15
In a systematic review and meta-analysis of all randomized controlled trials comparing a single dose of palonosetron with other 5-HT3 receptor antagonists, Botrel et al19 concluded that palonosetron was more effective than the first generation receptor antagonists in preventing acute and delayed CINV in patients receiving MEC or HEC, regardless of the use of concomitant corticosteroids. Schwartzberg et al20 concluded that palonosetron is more effective than the first generation 5-HT3 receptor antagonists in controlling CINV in the delayed and overall postchemotherapy periods based on a pooled analysis of Phase III clinical studies of palonosetron versus ondansetron, dolasetron, and granisetron. In an additional review, Popovic et al21 concluded that palonosetron is safer and more efficacious than the other 5-HT3 receptor antagonists. Boccia et al22 recently demonstrated that oral palonosetron had similar efficacy and safety as intravenous (IV) palonsetron for the prevention of acute CINV in patients receiving MEC.
Neurokin-1 (NK-1) receptor antagonists
Substance P is a mammalian tachykinin that is found in vagal afferent neurons innervating the brainstem, which sends impulses to the vomiting center.23 Substance P induces vomiting and binds to NK-1 receptors in the abdominal vagus, the brainstem, and the area postrema.23 Compounds that block NK-1 receptors lessen emesis after cisplatin, ipecac, apomorphine, and radiation therapy.23 These observations have recently led to the development of NK-1 receptor antagonists and the study of the role they may play in controlling CINV.
Aprepitant
Aprepitant is an NK-1 receptor antagonist that blocks the emetic effects of substance P.6,24,25 When combined with the corticosteroid dexamethasone and a 5-HT3 receptor antagonist, aprepitant is effective in the prevention of CINV in patients receiving HEC.24–27 This regimen is recommended in the guidelines of multiple international groups for the control of CINV in patients receiving HEC.12–14
In a study involving breast cancer patients receiving cyclophosphamide and doxorubicin or epirubicin, aprepitant was added to ondansetron and dexamethasone for the prevention of CINV. The addition of aprepitant to the 5-HT3 receptor antagonist plus dexamethasone improved the complete response, but there was no improvement in nausea.28 Palonosetron and aprepitant have been combined with dexamethasone for the prevention of CINV in a Phase II study of 58 patients who received doxorubicin and cyclophosphamide.29 This three-drug antiemetic regimen was found to be safe and highly effective in preventing emesis and rescue in the acute, delayed and overall periods, but there was poor control of nausea.
Fosaprepitant
Fosaprepitant (also known as MK-0517 and L-758,298) is a water-soluble phosphoryl pro-drug for aprepitant that, when administered IV, is converted to aprepitant within 30 minutes via the action of ubiquitous phosphatases. The pharmacological effect of fosaprepitant is attributed to aprepitant. Due to the rapid conversion of fosaprepitant to the active form (aprepitant) by phosphatase enzymes, it is expected to provide the same aprepitant exposure in terms of area under the curve (AUC) and a correspondingly similar antiemetic effect.30,31
Fosaprepitant in the IV dose of 115 mg has been approved by the FDA (February 2008) and the European Union (January 2008) as an alternative to oral aprepitant 125 mg on day 1 of a 3-day regimen, with oral aprepitant 80 mg administered on days 2 and 3.26 Further studies have demonstrated that a single dose of IV fosaprepitant 150 mg on day 1 of cisplatin chemotherapy was noninferior to a 3-day oral regimen of aprepitant in the prevention of CINV in the 120-hours postchemotherapy period.32
Rolapitant
Recent Phase III clinical trials have reported the use of Rolapitant, a new NK-1 receptor antagonist, for the prevention of CINV in patients receiving MEC and HEC.33–36 Rolapitant has a long half-life of 180 hours and does not induce or inhibit CYP3A4.33 Poma et al33 reported that rolapitant and its major metabolite SCH720 881 do not affect the pharmacokinetics of midazolam, a sensitive cytochrome P450 3A4 substrate. Rolapitant does not induce CYP3A4, and single oral doses of rolapitant, co-administered with midazolam were safe and well tolerated.33 Administration of rolapitant, unlike other NK-1 receptor antagonists does not require dose adjustment of concomitantly administered drugs metabolized by CYP34A.
In a randomized, Phase III double-blind active-control study, 555 chemotherapy-naïve patients receiving HEC were randomized to receive rolapitant (200 mg PO) plus granisetron plus dexamethasone versus placebo plus granisetron plus dexamethasone prior to chemotherapy. Complete response (no emesis, no rescue) for the acute, delayed, and overall periods was significantly improved in the patients receiving rolapitant.34 In addition, “no nausea” was significantly improved for the rolapitant group in the delayed period (58.3% versus 46.9%) and the overall period (55.0% versus 44.0%).34
In an additional randomized Phase III double-blind active-control study, 1,369 chemotherapy-naïve patients receiving MEC were randomized to receive rolapitant (200 mg PO) plus granisetron plus dexamethasone versus placebo plus granisetron plus dexamethasone prior to chemotherapy. Complete response (no emesis, no rescue) for the acute, delayed, and overall periods was significantly improved in the patients receiving rolapitant.35 Fifty-two percent of the patients who received rolapitant received the high risk chemotherapy anthracycline-cyclophosphamide and 47% received non anthracycline-cyclophosphamide MEC chemotherapy.
Rolapitant 200 mg in combination with granisetron and dexamethasone was demonstrated to be safe and well tolerated in the two Phase III clinical trials involving patients receiving MEC or HEC.36
Netupitant
Netupitant is a new NK-1 receptor antagonist currently in clinical trials. In vitro and in vivo pharmacologic characterization demonstrated that it inhibits substance P in NK-1 receptors but was inactive for NK-2 and NK-3 receptors. This was demonstrated with intrathecal injections in mice, and intraperitoneally in both mice and gerbils. In all assays, aprepitant exhibited similar effects.37
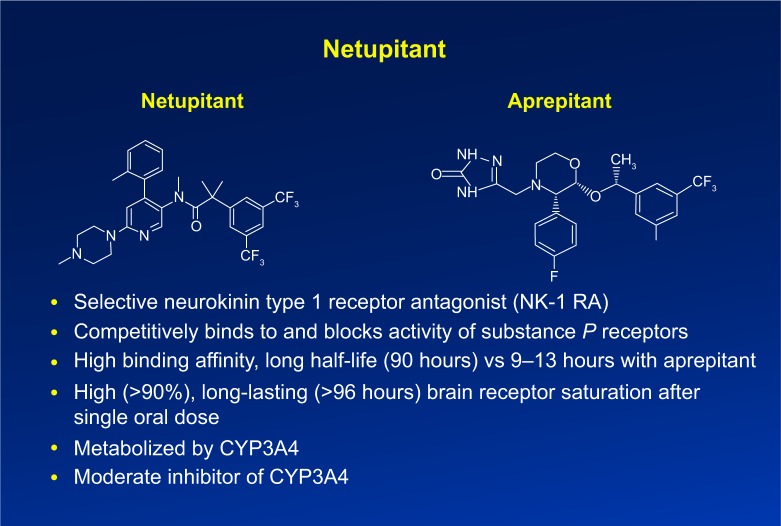
Netupitant behaves as a brain penetrant, is orally active, and is a potent and selective NK-1 antagonist.37–39 Rossi et al38 and Spinelli et al39 reported that positive emission tomography results demonstrate that netupitant is a potent agent targeting NK-1 receptors. It appears to have a high degree of occupancy (90%) for a long duration (96 hours) when given as a single oral dose and appears to be well tolerated.38,39 Figure 1 illustrates the chemical structure of netupitant compared to the structure of aprepitant.6,24,40 Netupitant has a high binding affinity, and a long half-life of 90 hours compared to a 9–13-hour half-life of aprepitant.6,24,37–40 It is metabolized by CYP3A4 and is a moderate inhibitor of CYP3A4.37–39
Figure 1.
Profile of Netupitant.
NEPA
NEPA is an oral fixed-dose combination of netupitant and palonosetron which has recently been employed in Phase II and Phase III clinical trials for the prevention of CINV in patients receiving MEC and HEC. This drug combination targets two critical pathways associated with acute and delayed CINV, the serotonin and the substance P mediated pathways. The binding of palonosetron to the 5-HT3 receptor has been reported to be distinctly different from the binding of the first generation 5-HT3 receptor antagonists,18,41 possibly accounting for its effects on improving delayed CINV compared to the first generation 5-HT3 receptor antagonists. In addition, in vitro studies42–44 with NG108-15 cells have demonstrated that in the absence of serotonin, palonosetron inhibited the substance P mediated response while ondansetron and granisetron had no effect. In the same system, Netupitant also inhibited the substance P response as expected from an NK-1 receptor antagonist. When both palonosetron and netupitant were present, they exhibited an enhanced inhibition of the substance P response compared to the two antagonists alone. It is speculated that palonosetron may inhibit substance P mediated responses through its unique interactions with the 5-HT3 receptor.44 Based on these molecular mechanisms, NEPA has been used in a number of clinical trials45–47 for the prevention of CINV.
A randomized, double-blind parallel group study in 694 chemotherapy naïve patients undergoing cisplatin-based chemotherapy compared three different oral doses of Netupitant (100, 200, and 300 mg) plus oral palonosetron (0.50 mg) (NEPA) with oral palonosetron (0.50 mg) with all agents given prior to chemotherapy (day 1). A standard three-day oral aprepitant plus IV ondansetron (32 mg) regimen was used as an additional comparative arm. All patients in all treatment arms received oral dexamethasone on days 1–4.45 The primary efficacy endpoint was complete response for the overall (0–120 hour) phase.
All NEPA treatment arms of the study were significantly superior in overall complete response rates compared to palonosetron alone. The 300 mg NEPA dose appeared to have a numerical advantage over the lower doses. There was no significant difference in the overall complete response in the NEPA treatment arms and the aprepitant arm. The number of adverse events were low and comparable across all treatment groups.45
The Phase II dose-ranging study45 suggested that the 300 mg NEPA dose was the most effective dose, and this prompted a Phase III clinical trial for the prevention of CINV in patients receiving MEC.46 A multinational, randomized, double-blind, parallel group Phase III study in 1,455 chemotherapy-naïve patients receiving MEC (including patients receiving anthracycline and cyclophosphamide) were randomized to a single oral dose of NEPA (300 mg netupitant plus 0.50 mg palonosetron) or a single oral dose of palonosetron (0.50 mg) prior to chemotherapy, day 1. All patients received oral dexamethasone on day 1 only (12 mg in the NEPA arm; 20 mg in the palonosetron arm). The primary efficacy endpoint was complete response during the delayed (24–120 hours) period. The complete response during the delayed period was significantly higher for the NEPA group of patients compared to the palonosetron patient group. NEPA was well tolerated with a similar safety profile as palonosetron.46
One thousand, two hundred and eighty-six patients of the original 1,455 patients in the Phase III trial participated in a multiple cycle extension of the study. Seventy-six percent of the patients completed four cycles. Treatment groups were comparable, and the superiority of the NEPA group compared to the palonosetron group for complete response in the overall (0–120 hour) period in cycle one was maintained over the multiple chemotherapy cycles. There was a low incidence of adverse events for the patients receiving NEPA, 3.5% headache, 2.0% constipation, during the multiple cycle extension. There was no difference in adverse events in the NEPA versus the palonosetron group.47
The data reported in the Phase II and Phase III NEPA studies45,46 were for cycle one of chemotherapy. Chemotherapy-naïve patients receiving HEC or MEC in these two studies were further studied to determine the safety and efficacy of NEPA over multiple cycles of chemotherapy.48 Four hundred and thirteen patients were randomized, with 309 patients allocated to NEPA (300 mg netupitant plus 0.50 mg palonosetron) plus dexamethasone, and 104 patients allocated to 3 days of oral aprepitant plus palonosetron plus dexamethasone. Dexamethasone was administered on days 1–4 for patients receiving HEC and on day 1 only for patients receiving MEC. Patients completed 1,961 chemotherapy cycles (1,446 NEPA, 515 aprepitant plus palonosetron) (76% MEC, 24% HEC). Ninety-eight percent of patients completed cycle one, 75% completed at least four cycles, 40% completed six cycles. The incidence of adverse events was comparable in both groups with the most frequent adverse events being constipation (3.6%) and headache (1.0%). The adverse events were mild/moderate with no cardiac safety concerns. The complete response rates were maintained over repeated cycles for both the NEPA patient group and the group receiving aprepitant plus palonosetron.48
In an attempt to determine the degree of nausea control with the use of NEPA compared to palonosetron, patients from two randomized, multinational studies45,46 who received a single dose of NEPA (netupitant 300 mg plus palonosetron 0.50 mg) or palonosetron and dexamethasone prior to cisplatin or an anthracycline plus cyclophosphamide were evaluated for no significant nausea (<25 mm, 0–100 mm, visual analog scale). The NEPA group had more patients with no significant nausea and this was most apparent in the delayed nausea phase of the cisplatin patients.49
On October 10, 2014, NEPA (Akynzeo®, Helsinn Helathcare SA, Switzerland) was approved by the FDA to treat nausea and vomiting in patients undergoing cancer chemotherapy.50
Conclusion
Netupitant is a new NK-1 receptor antagonist with a structure and mechanism of action similar to aprepitant, the first agent approved by the FDA in this drug class. Netupitant has a high binding affinity, a long half-life of 90 hours, is metabolized by CYP3A4, and is an inhibitor of CYP3A4.
NEPA is an oral fixed-dose combination of netupitant and palonosetron which has recently been employed in Phase II and Phase III clinical trials for the prevention of CINV in patients receiving MEC and HEC. The clinical trials demonstrated that NEPA (300 mg of netupitant plus 0.50 mg of palonosetron) significantly improved the prevention of CINV compared to the use of palonosetron alone in patients receiving either HEC or MEC. The significant improvement in the delayed period (24–120 hours) and the overall period (0–120 hours) postchemotherapy was maintained over multiple cycles of chemotherapy. Adverse events were few in number (≤3.5%) and were mild to moderate in severity. No cardiac adverse events were noted. In a subgroup analysis of patients receiving cisplatin or an anthracycline plus cyclophosphamide, data from two clinical trials demonstrated that NEPA may have improved no significant nausea (a secondary endpoint) compared to palonosetron.
One of the clinical trials involving patients receiving HEC included a comparative arm consisting of oral aprepitant plus palonosetron. All patients in all arms received standard doses of dexamethasone. Based on the data and the analysis reported in the NEPA clinical trials, there appeared to be no significant differences in the prevention of CINV between NEPA and the aprepitant and palonosetron combination.
The FDA has recently approved NEPA (Akynzeo®, Helsinn Healthcars SA) for the treatment of nausea and vomiting in patients undergoing cancer chemotherapy.
Footnotes
Disclosure
The author reports no conflicts of interest and there are no sources of funding for this manuscript.
References
- 1.Bloechl-Daum B, Deuson RR, Mavros P, et al. Delayed nausea and vomiting continue to reduce patients’ quality of life after highly and moderately emetogenic chemotherapy despite antiemetic treatment. J Clin Oncol. 2006;24:4472–4478. doi: 10.1200/JCO.2006.05.6382. [DOI] [PubMed] [Google Scholar]
- 2.Cohen L, de Moor CA, Eisenberg P, et al. Chemotherapy-induced nausea and vomiting: incidence and impact on patient quality of life at community oncology settings. Support Care Cancer. 2007;15(5):497–503. doi: 10.1007/s00520-006-0173-z. [DOI] [PubMed] [Google Scholar]
- 3.Navari RM. Management of chemotherapy-induced nausea and vomiting: focus on newer agents and new uses for older agents. Drugs. 2013;73:249–262. doi: 10.1007/s40265-013-0019-1. [DOI] [PubMed] [Google Scholar]
- 4.Navari RM. Palonosetron for the prevention of chemotherapy-induced nausea and vomiting in patients with cancer. Future Oncol. 2010;6:1074–1084. doi: 10.2217/fon.10.74. [DOI] [PubMed] [Google Scholar]
- 5.Navari RM. The current status of the use of palonosetron. Expert Opin Pharmacother. 2013;14:1281–1284. doi: 10.1517/14656566.2013.799141. [DOI] [PubMed] [Google Scholar]
- 6.Curran MP, Robinson DM. Aprepitant: a review of its use in the prevention of nausea and vomiting. Drugs. 2009;69:1853–1858. doi: 10.2165/11203680-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Navari RM. Olanzapine for the prevention and treatment of chronic nausea and chemotherapy-induced nausea and vomiting. Eur J Pharmcol. 2014;722:180–186. doi: 10.1016/j.ejphar.2013.08.048. [DOI] [PubMed] [Google Scholar]
- 8.Tan L, Liu J, Liu X, et al. Clinical research of olanzapine for the prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res. 2009;28:1–7. doi: 10.1186/1756-9966-28-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Navari RM, Gray SE, Kerr AC. Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol. 2011;9:188–195. doi: 10.1016/j.suponc.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Navari RM. Treatment of chemotherapy-induced nausea. Community Oncol. 2012;9:20–26. [Google Scholar]
- 11.Stern RM, Koch KL, Andrews PLR, editors. Nausea: Mechanisms and Management. New York, NY: Oxford University Press; 2011. [Google Scholar]
- 12.Roila F, Herrstedt J, Aapro M, et al. Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol. 2010;21(5):232–243. doi: 10.1093/annonc/mdq194. [DOI] [PubMed] [Google Scholar]
- 13.Basch E, Prestrud AA, Hesketh PJ, et al. Antiemetic American Society Clinical Oncology clinical practice guideline update. J Clin Oncol. 2011;29:4189–4198. doi: 10.1200/JCO.2010.34.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NCCN Clinical Practice Guidelines in Oncology version 2. 2014; Anti-emesis National Comprehensive Cancer Network (NCCN) [online] [Accessed July 8, 2014]. Available from URL: http://www.nccn.org/professionals/physician_gls/PDF/antiemesis.pdf.
- 15.Navari RM. Palonosetron for the treatment of chemotherapy-induced nausea and vomiting. Expert Opin Pharmacother. 2014;15(17):2599–2608. doi: 10.1517/14656566.2014.972366. [DOI] [PubMed] [Google Scholar]
- 16.Egler RM, Lee CH, Smith W, et al. Pharmacologic characterization of RS 25259-197, a novel and selective 5HT3 receptor antagonist in vivo. Br J Pharmacol. 1995;114:860–866. doi: 10.1111/j.1476-5381.1995.tb13283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eisenberg P, MacKintosh FR, Ritch P, et al. Efficacy, safety, and pharmacokinetics of palonosetron in patients receiving highly emetogenic, cisplatin-based chemotherapy: a dose-ranging, clinical study. Ann Oncol. 2004;15:330–337. doi: 10.1093/annonc/mdh047. [DOI] [PubMed] [Google Scholar]
- 18.Rojas C, Thomas AG, Alt J, et al. Palonosetron triggers 5-HT3 receptor internalization and causes prolonged inhibition of receptor function. Eur J Pharmacol. 2010;626:193–199. doi: 10.1016/j.ejphar.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Botrel T, Clark O, Clark L, et al. Efficacy of palonosetron compared to other serotonin inhibitors (5-HT3R) in preventing chemotherapy-induced nausea and vomiting (CINV) in patients receiving moderately or highly emetogenic treatment: systematic review and meta-analysis. Support Care Cancer. 2011;19:823–832. doi: 10.1007/s00520-010-0908-8. [DOI] [PubMed] [Google Scholar]
- 20.Schwartzberg L, Barbour SY, Morrow GR, et al. Pooled analysis of phase III studies of palonosetron versus ondansetron, dolasetron, and granisetron in the prevention of chemotherapy-induced nausea and vomiting. Support Care Cancer. 2014;22:469–477. doi: 10.1007/s00520-013-1999-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Popovic M, Warr DG, DeAngelis C, et al. Efficacy and safety of palonosetron for the prophylaxis of chemotherapy-induced nausea and vomiting (CINV): a systematic review and meta-analysis of randomized controlled trials. Support Care Cancer. 2014;22:1485–1497. doi: 10.1007/s00520-014-2175-6. [DOI] [PubMed] [Google Scholar]
- 22.Boccia R, Grunberg S, Franco-Gonzales E, et al. Efficacy of oral palonosetron compared to intravenous palonosetron for the prevention of chemotherapy-induced nausea and vomiting associated with moderately emetogenic chemotherapy: a phase III trial. Support Care Cancer. 2013;44:1453–1460. doi: 10.1007/s00520-012-1691-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diemunsch P, Grelot L. Potential of substance P antagonists as antiemetics. Drugs. 2000;60:533–546. doi: 10.2165/00003495-200060030-00002. [DOI] [PubMed] [Google Scholar]
- 24.Sankhala KK, Pandya DM, Sarantopoulos J, et al. Prevention of chemotherapy induced nausea and vomiting: a focus on aprepitant. Exp Opin Drug Metab Toxicol. 2009;12:1607–1614. doi: 10.1517/17425250903451675. [DOI] [PubMed] [Google Scholar]
- 25.Navari RM. Pathogenesis-based treatment of chemotherapy-induced nausea and vomiting: two new agents. J Support Oncol. 2003;1:89–103. [PubMed] [Google Scholar]
- 26.Hesketh PJ, Grunberg SM, Herrstedt J, et al. Combined data from two phase III trials of the NK-1 antagonist aprepitant plus a 5HT3 antagonist and a corticosteroid for prevention of chemotherapy-induced nausea and vomiting: effect of gender on treatment response. Support Care Cancer. 2006;14:354–360. doi: 10.1007/s00520-005-0914-4. [DOI] [PubMed] [Google Scholar]
- 27.Warr DG, Grunberg SM, Gralla RJ, et al. The oral NK1 antagonist aprepitant for the prevention of acute and delayed chemotherapy-induced nausea and vomiting: pooled data from two randomized, double-blind, placebo controlled trials. Eur J Cancer. 2005;41(9):1278–1285. doi: 10.1016/j.ejca.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 28.Warr DG, Hesketh PJ, Gralla RJ, et al. Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol. 2005;23:2822–2830. doi: 10.1200/JCO.2005.09.050. [DOI] [PubMed] [Google Scholar]
- 29.Grote T, Hajdenberg J, Cartnell A, et al. Combination therapy for chemotherapy-induced nausea and vomiting in patients receiving moderately emetogenic chemotherapy: palonosetron, dexamethasone, and aprepitant. J Support Oncol. 2006;4(8):403–408. [PubMed] [Google Scholar]
- 30.Navari RM. Fosaprepitant (MK-0517): a neurokinin-1 receptor antagonist for the prevention of chemotherapy-induced nausea and vomiting. Exp Opin Investig Drugs. 2007;16:1977–1985. doi: 10.1517/13543784.16.12.1977. [DOI] [PubMed] [Google Scholar]
- 31.Lasseter KC, Gambale J, Jin B, et al. Tolerability of fosaprepitant and bioequivalency to aprepitant in healthy subjects. J Clin Pharmacol. 2007;47:834–840. doi: 10.1177/0091270007301800. [DOI] [PubMed] [Google Scholar]
- 32.Grunberg S, Chua D, Maru A, et al. Single-dose fosaprepitant for the prevention of chemotherapy-induced nausea and vomiting associated with cisplatin therapy: randomized, double-blind study protocol–EASE. J Clin Oncol. 2011;29(11):1495–1501. doi: 10.1200/JCO.2010.31.7859. [DOI] [PubMed] [Google Scholar]
- 33.Poma A, Christensen J, Pertikis H, et al. Rolapitant and its major metabolite do not affect the pharmacokinetics of midazolam, a sensitive cytochrome P450 3A4 susbstrate. Support Care Cancer. 2013;21:S154. Abstract 441. [Google Scholar]
- 34.Rapoport BL, Poma A, Hedley ML, Martel RE, Navari RM. Phase III trial results for rolapitant, a novel NK-1 receptor antagonist, in the prevention of chemotherapy-induced nausea and vomiting (CINV) in subjects receiving highly emetogenic chemotherapy (HEC) [abstract] J Clin Oncol. 2014;32(Suppl 5):9638. [Google Scholar]
- 35.Schnadig ID, Modiano MR, Poma A, Hedley ML, Martel RE, Schwartzberg LS. Phase III trial results for rolapitant, a novel NK-1 receptor antagonist, in the prevention of chemotherapy-induced nausea and vomiting (CINV) in subjects receiving moderately emetogenic chemotherapy (MEC) [abstract] J Clin Oncol. 2014;32(Suppl 5):9633. [Google Scholar]
- 36.Urban L, Poma A, Daqrdeno MM, Martel RE. Safety of rolapitant, a novel NK-1 receptor antagonist, in the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients receiving moderately or highly emetogenic chemotherapy (MEC or HEC) [abstract] J Clin Oncol. 2014;32(Suppl 5):9636. [Google Scholar]
- 37.Rizzi A, Campi B, Camarda V, et al. In vitro and in vivo pharmacological characterization of the novel NK-1 receptor selective antagonist Netupitant. Peptides. 2012;37:86–97. doi: 10.1016/j.peptides.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 38.Rossi G, Tilkola SO, Rudengren C, et al. A positron emission tomography study to assess the degree of neurokinin-1 receptor occupancy in the human brain after single doses of netupitant to healthy male subjects [abstract] J Clin Oncol. 2012;30(Suppl):9054. [Google Scholar]
- 39.Spinelli T, Calcagneli S, Giuliano C. Netupitant PET Imaging and ADME Studies in Humans. J Clin Pharm. 2014;54:97–108. doi: 10.1002/jcph.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Cancer Institute Drug Dictionary. [Accessed October 15, 2014]. Available from: http://www.cancer.gov/drugdictionary.
- 41.Rojas C, Slusher BS. Pharmacological mechanisms of 5-HT3 tachykinin NK-1 receptor antagonism to prevent chemotherapy-induced nausea and vomiting. Eur J Pharmacol. 2012;684:1–7. doi: 10.1016/j.ejphar.2012.01.046. [DOI] [PubMed] [Google Scholar]
- 42.Stathis M, Pietra C, Rojas C, Slusher BS. Inhibition of substance P-mediated responses in NG108-15 cells by netupitant and palonosetron exhibit synergistic effects. Eur J Pharmacol. 2012;689:25–30. doi: 10.1016/j.ejphar.2012.05.037. [DOI] [PubMed] [Google Scholar]
- 43.Thomas AG, Stathis M, Rojas C, Slusher BS. Netupitant and palonosetron trigger NK-1 receptor internalization in NG108-15 cells. Exp Brain Res. 2014;232(8):2637–2644. doi: 10.1007/s00221-014-4017-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rojas C, Raje M, Tsukamoto T, Slusher BS. Molecular mechanisms of 5-HT3 and NK-1 receptor antagonists in prevention of emesis. Eur J Pharmacol. 2014;722:26–37. doi: 10.1016/j.ejphar.2013.08.049. [DOI] [PubMed] [Google Scholar]
- 45.Hesketh PJ, Rossi G, Rizzi G, et al. Efficacy and safety of NEPA, an oral combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy: a randomized dose-ranging pivotal study. Ann Oncol. 2014;25:1340–1346. doi: 10.1093/annonc/mdu110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aapro M, Rugo H, Rossi G, et al. A randomized phase III study evaluating the efficacy and safety of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy. Ann Oncol. 2014;25:1328–1333. doi: 10.1093/annonc/mdu101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aapro M, Karthaus M, Schwartzberg LS, et al. Phase 3 study of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting during repeated moderately emetogenic chemotherapy cycles [abstract] J Clin Oncol. 2014;32(Suppl 5):9502. doi: 10.1093/annonc/mdu101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gralla RJ, Bosnjak SM, Hontsa A, et al. A phase III study evaluating the safety and efficacy of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting over repeated cycles of chemotherapy. Ann Oncol. 2014;25:1333–1339. doi: 10.1093/annonc/mdu096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schwartzberg L, Aapro M, Hesketh PJ, et al. do NK-1 receptor antagonists contribute to nausea control? Evaluation of the novel NEPA fixed-dose combination of NK-1 receptor antagonist plus a 5-HT3 receptor antagonist from pivotal trials. Support Care Cancer. 2014;22:S107. Abstract 161. [Google Scholar]
- 50.US Food and Drug Administration . FDA approves Akynzeo for nausea and vomiting associated with cancer chemotherapy [press release] Silver Springs, MD: US Food and Drug Administration; Oct 10, 2014. [Accessed October 10, 2014]. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements. [Google Scholar]