Abstract
Background
Patient falls in acute care hospitals represent a significant patient safety concern. Although cross-sectional studies have shown that fall rates vary widely between acute care hospitals, it is not clear whether hospital fall rates remain consistent over time.
Purpose
The aim of this study was to determine whether hospitals can be categorized into fall rate trajectory groups over time and to identify nurse staffing and hospital characteristics associated with hospital fall rate trajectory groups.
Methodology/Approach
We conducted a 54-month (July 2006–December 2010) longitudinal study of U.S. acute care general hospitals participating in the National Database for Nursing Quality Indicators® (2007). We used latent class growth modeling to categorize hospitals into groups based on their long-term fall rates. Nurse staffing and hospital characteristics associated with membership in the highest hospital fall rate group were identified using logistic regression.
Findings
A sample of 1,529 hospitals (mean fall rate of 3.65 per 1,000 patient days) contributed data to the analysis. Latent class growth modeling findings classified hospital into three groups based on fall rate trajectories: consistently high (mean fall rate of 4.96 per 1,000 patient days), consistently medium (mean fall rate of 3.63 per 1,000 patient days), and consistently low (mean fall rate of 2.50 per 1,000 patient days). Hospitals with higher total nurse staffing (odds ratio [OR] = 0.92, 95% confidence interval [CI] [0.85, 0.99]), Magnet status (OR = 0.49, 95% CI [0.35, 0.70]), and bed size greater than 300 beds (OR = 0.70, 95% CI [0.51, 0.94]) were significantly less likely to be categorized in the “consistently high” fall rate group.
Practice Implications
Over this 54-month period, hospitals were categorized into three groups based on long-term fall rates. Hospital-level factors differed among these three groups. This suggests that there may be hospitals in which “best practices” for fall prevention might be identified. In addition, administrators may be able to reduce fall rates by maintaining greater nurse staffing ratios as well as fostering an environment consistent with that of Magnet hospitals.
Keywords: Hospitals, magnet status, nursing staffing, patient falls
Patient falls in acute care hospitals represent a significant public health concern in the United States, with nearly 1 million falls occurring annually (Currie, 2008; Oliver, Healey, & Haines, 2010). Inpatient falls are the most commonly reported adverse event in hospitals, and falls among patients over age 65 years are the most frequent cause of nonfatal injuries among hospitalized patients (Currie, 2008; Morse, 2002). Approximately 2% of patients in acute care settings will experience a fall during their stay, and nearly one quarter of patients who fall will sustain an injury because of falling (Coussement et al., 2008; Oliver et al., 2010). Inpatient falls have long-term effects on patient well-being and quality of life through loss of independence, fear of future falls, depression, and immobility (Currie, 2008; Faes et al., 2010). Falls are also a concern because of the estimated cost of $16–$19 billion to the health care system for treating fall-related injuries, which are no longer reimbursed by the Centers for Medicare and Medicaid (CMS, 2008; Stevens, Corso, Finkelstein, & Miller, 2006).
To date, a majority of the research on patient falls has been conducted in rehabilitation and long-term care settings with less research on falls in acute care hospitals (Fischer et al., 2005). The current evidence on hospital falls has been conducted primarily using cross-sectional data sets, single sites, or small sample sizes, which limits the generalizability of findings to other hospitals (Currie, 2008). Furthermore, research on the prevention of inpatient falls has largely been focused on two main areas of inquiry: (1) patient risk factors related to inpatient falls (i.e., neurological impairment, age, sedative medications, etc.) and (2) interventions to reduce falls in hospitals, including fall risk assessment tools (Oliver, Daly, Martin, & McMurdo, 2004), armband identification bracelets (Mayo, Gloutney, & Levy, 1994), toileting needs assessments (Bakarich, McMillan, & Prosser, 1997), medication reviews (Cumming et al., 2008), and use of physical restraints (Shorr et al., 2002). However, there remains unexplained variation in hospital falls, and a prevalence of between 2 and 25 falls per 1,000 patient days, on average, has been documented (Currie, 2008; Hitcho et al., 2004). As a result, falls continue to be a growing issue that is not resolved by any one measure, and it is unclear whether some hospitals perform consistently better than others in terms of falls over time (Evans, Hodgkinson, Lambert, & Wood, 2001).
Nurse Staffing and Patient Falls
Between 1990 and 2006, three systematic literature reviews found insufficient evidence to support the causal association between nurse staffing and falls in acute care settings (Kane, Shamliyan, Mueller, Duval, & Wilt, 2007; Lake & Cheung, 2006; Lang, Hodge, Olson, Romano, & Kravitz, 2004). However, a number of researchers have shown a significant association between reductions of inpatient falls and several nurse staffing measures, including total nursing hours per patient day (TNHPPD) (Dunton, Gajewski, Klaus, & Pierson, 2007; Dunton, Gajewski, Taunton, & Moore, 2004), registered nursing skill mix (Dunton et al., 2004, 2007), and registered nursing hours per patient day (Lake, Shang, Klaus, & Dunton, 2010). In addition, falls were added by the National Quality Forum (NQF) in 2004 as one of the first measurements of hospital quality, demonstrating that falls are important measures for maintaining high quality of care in acute care settings and nursing care may play a significant role in whether a patient will fall in a hospital (NQF, 2004).
Organizational Characteristics and Patient Falls
Furthermore, research on hospital organizational structure and patient fall outcome measures has been inconclusive. For instance, Mark and colleagues (2008) conducted a study at 143 hospitals with a total of 278 medical–surgical units to examine the association between hospital organizational structure, patient-level characteristics, and safety climate on the risk of inpatient falls. Results from this study did not find a significant effect of hospital structural components on patient falls, but hospital units with greater patient capacity resulted in higher fall rates. Several hospital organizational characteristics have been linked to lower patient falls, including Magnet status (Lake et al., 2010) and larger hospital bed size (Dunton et al., 2004), but it is still unclear whether certain organizational characteristics are associated with patient fall rates over time and whether hospital fall rates remain consistently high or low over time.
To address prior limitations in the falls literature, we conducted a longitudinal study using latent class growth modeling (LCGM) to assess whether hospitals could be separated into fall rate trajectory groups. In addition, we examined the relationship between hospital organizational characteristics, nurse staffing, and membership in hospital fall rate trajectories. These areas of inquiry represent a significant gap in the literature given the potential importance of nurses in preventing falls as well as the need to understand characteristics of hospitals with consistently high and low patient fall measures. For instance, if hospitals remain in the “consistently high” fall rate trajectory group over 54 months, then the 2008 CMS nonreimbursement policy may not be as effective in reducing patient falls as policy-makers anticipated after October 1, 2008.
Therefore, the objective of this study is to categorize hospitals based on their long-term fall rates using LCGM and to explore nursing and hospital characteristics associated with membership in hospital fall rate trajectory groups.
Theoretical Framework
We used Donabedian’s seminal Structure–Process–Outcomes model (Donabedian, 1988) and Aiken, Clarke, and Sloane (2002) theoretical framework to explain the effect of organizational characteristics and nurse staffing on patient fall outcomes. Figure 1 depicts our study model and illustrates mechanisms through which nurse staffing and organizational characteristics of the hospital impact patient falls in hospitals.
Figure 1.
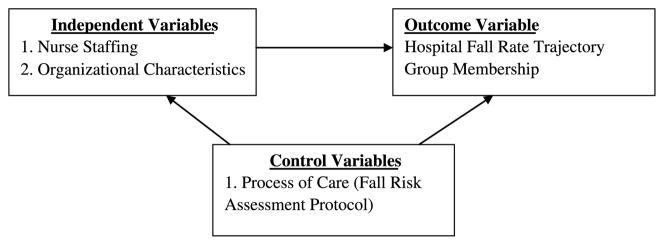
Study model
Organizational Structure and Nurse Staffing
In our study model, both nurse staffing and organizational characteristics play an important role in patient falls in hospitals. These organizational characteristics and nurse staffing measures create an environment in which there are two possible outcomes: (1) chronically understaffed hospitals give rise to latent/active errors and ineffective care processes or (2) adequately staffed hospitals lead to improved detection of patients at risk for falling (Cho, 2001). In addition, empirical studies have concluded that hospital organizational characteristics are associated with variations in levels of nurse staffing and patient falls (Lake et al., 2010). Therefore, we incorporated both nurse staffing and hospital organizational characteristics in our study as covariates.
Process of Care
Process of care reflects the manner in which care is delivered to patients within hospitals (Donabedian, 1988). In terms of falls, this is directly attributed to the ability of nurses to assess and monitor patients. Fall risk assessments are implemented by nurses, and staffing significantly contributes to adequately assessing at-risk fall patients (Lake & Cheung, 2006). Therefore, we added fall risk assessment protocols as a process-of-care indicator for patient fall prevention and as a control variable in our study.
Fall Outcomes
In our study model, the outcome measure is the total fall rates per 1,000 patient days, which is further classified into fall rate trajectory groups. This measure is consistent with prior empirical studies that examined the influence of nurse staffing on patient falls (Lake & Cheung, 2006). Our model posits that this adverse outcome will be lower in hospitals with adequate nurse staffing and organizational characteristics that contribute to high rates of staffing levels, such as Magnet status (Lake et al., 2010).
From this study model, we will examine the following hypotheses:
H1: Greater levels of nurse staffing (i.e., TNHPPD and registered nurse [RN] skill mix) will be associated with hospitals with lower fall rate trajectory groups.
H2: Hospital organizational characteristics of Magnet status, larger bed size, teaching status, and location in a metropolitan area will be associated with hospitals with lower fall rate trajectory groups.
Methodology
We used monthly retrospective data from the National Database of Nursing Quality Indicators (NDNQI). NDNQI provides monthly, quarterly, and annual reporting of structure, process, and outcome indicators to evaluate nursing care at the hospital and unit levels (Montalvo, 2007). Approximately one third of all U.S. hospitals participate in NDNQI, and the strengths and limitations of which have been discussed elsewhere (Dunton et al., 2004; Lake et al., 2010). For this study, we extracted NDNQI data for the 54 months from July 1, 2006, through December 31, 2010. We excluded from the study hospital observations without complete monthly patient fall count data or complete reporting of nursing hours. Our final sample was composed of 1,529 U.S. hospitals nationwide. All statistical analyses were conducted using Statistical Analysis Software (SAS) version 9.2 (SAS, 2007).
Variables and Measurement
Dependent variable
The outcome of interest in the current study was the rate of patient falls per 1,000 patient days. Falls are reported to NDNQI on a monthly basis and are identified through incident reports. A patient day was defined as a total of 24 hours beginning the hour of admission. This outcome variable is the most commonly used measure of patient falls in hospitals (Currie, 2008).
Covariates
Seven explanatory variables were considered as predictors of fall rates in these hospitals. Table 1 outlines study variables and operational definitions from the NDNQI.
Table 1.
Variable descriptions
| Variablea | Definition | Variable type |
|---|---|---|
| Dependent variable | ||
| Hospital fall rate | Patient falls per 1,000 patient days | Continuous |
| Covariates | ||
| Hospital factors | ||
| Hospital bed size | Number of hospital beds (0 = less than 300 beds, 1 = 300 beds or more) | Dichotomous |
| Magnet status | ANCC Magnet status (0 = non-Magnet, 1 = Magnet) | Dichotomous |
| Teaching status | Hospital teaching status (0 = non-teaching, 1 = teaching) | Dichotomous |
| Metropolitan status | Located in metropolitan area (0 = non-MSA, 1 = MSA) | Dichotomous |
| Census region | Hospital geographic region in the South, Midwest, Northeast, and West | Categorical |
| Hospital nurse staffing | ||
| Total nursing hours | Total nursing hours per patient day | Continuous |
| RN skill mix | RN hours divided by total nursing hours | Continuous |
| Process of care | ||
| Patient fall protocol | Proportion of hospitals with fall prevention protocols | Continuous |
Note. MSA = metropolitan statistical area; RN = registered nurse.
Data were from the National Database of Nursing Quality Indicators.
Nurse Staffing
Nurse staffing variables were measured according to the recommendations from the NQF (2004) and previous expert recommendations of the most effective nurse staffing measurements (Lake et al., 2010; Van den Heede, Clarke, Sermeus, Vleugels, & Aiken, 2007). The two nurse staffing variables incorporated in our study included the TNHPPD (i.e., the total amount of nursing care received by patients) and RN skill mix (the percentage of total nursing care hours provided by RNs). TNHPPD was calculated by adding the total hours provided by RNs, licensed practical nurses, and nursing assistants and dividing by the total number of patient days. These nurse staffing variables were reported to NDNQI on a monthly basis and aggregated to the hospital level.
Hospital Organizational Variables
The organizational variables included in our study were not time varying. Metropolitan status was dichotomized as hospitals located in metropolitan versus nonmetropolitan locations. Census region was operationalized as a categorical variable that reflected the location of the hospital in the Northeast, Midwest, South, or West region of the United States. Teaching status was a dichotomized variable of either teaching or nonteaching. Total bed size was categorized as less than 300 beds or greater than or equal to 300 beds. Finally, Magnet status was a dichotomized variable used to differentiate ANCC-Magnet-certified hospitals from non-Magnet hospitals.
In the NDNQI data set used for this study, there are three types of reported adult hospital units: (1) medical (i.e., general medical or medical specialty care including cardiac, infectious disease, etc.), (2) surgical (i.e., general surgical or surgical specialty care including bariatric, transplant, trauma, etc.), and (3) medical/surgical units (i.e., provide care to both types of patients). Because medical units have higher fall rates when compared with other units (Dunton et al., 2004), we created a control variable that assessed the percentage of fall observations from medical units and aggregated this to the hospital-level. This variable was created to control for higher acuity fall units within hospitals and as a proxy measure for hospital patient acuity. We created this variable by dividing monthly aggregating medical unit observations by all unit-level observations to create a hospital-level percentage of medical unit contribution at each hospital.
Process of Care
The process-of-care control variable incorporated in our study includes the proportion of fallers with a fall prevention protocol in place at the hospital level, which reflects a hospital’s assessment and evaluation of patients at risk for falling.
Analytical Approach
First, hospital-level descriptive statistics were conducted to determine the distribution of the variables in the model. LCGM was then selected to categorize hospitals based on their fall rates over a 54-month period (i.e., July 2006–December 2010). We aggregated fall rates per month by dividing the sum of all fall counts by the total number of patient days. LCGM is a semiparametrical method that allows researchers to classify subgroups of a population following a consistent pattern of change in a given outcome (Andruff, Carraro, Thompson, Gaudreau, & Louvet, 2009; Jones, Nagin, & Roeder, 2001; Nagin, 2005). For instance, although each hospital has a distinct course of fall rates over 54 months, the change patterns between individual hospitals are summarized by an intercept and slope that corresponds equally to a given trajectory of hospitals (Andruff et al., 2009; Nagin, 1999, 2005). Because LCGM categorizes each hospital into a distinct latent trajectory based on their fall rates over time, this methodology allows for further analysis of nurse staffing and organizational characteristics that impact membership in each particular group.
The PROC TRAJ procedure in SAS 9.2 was used for LCGM (Nagin, 2005; SAS Institute, 2007). For model selection, we used an iterative stepwise approach based on the number of latent class categories of hospitals, probability distributions, and overall best model fit statistics from the data, including the Bayesian Information Criteria, log Bayes approximation calculations, and statistical significance at the level of p < .05 (Andruff et al., 2009; Nagin, 2005). In particular, we compared the Bayesian Information Criteria and log Bayes approximation values after adding additional latent class groups, continually analyzing parameter estimates for significant p values less than .05 and percentages of group membership in each latent class trajectory, which should be a minimum of 5% (Andruff et al., 2009). To ensure model accuracy and reliability, we followed recommendations from Nagin and calculated average posterior probabilities, which were all substantially higher than the recommended minimum of .7.
Next, logistic regression was used to determine the impact of nurse staffing and organizational characteristics on the probability of membership in the “consistently high” hospital fall rate group. The dependent variable in this model was a dichotomous variable that distinguished between hospitals in the highest fall rate group compared with all other hospitals in our sample (i.e., a combination of hospitals in lower fall rate trajectory groups). This analysis produced adjusted odds ratios (ORs) predicting membership in the “consistently high” hospital fall rate group. All analyses were conducted in SAS version 9.2 using the PROC LOGISTIC procedure (SAS Institute, 2007).
Findings
Fall Rate Trajectory Groups
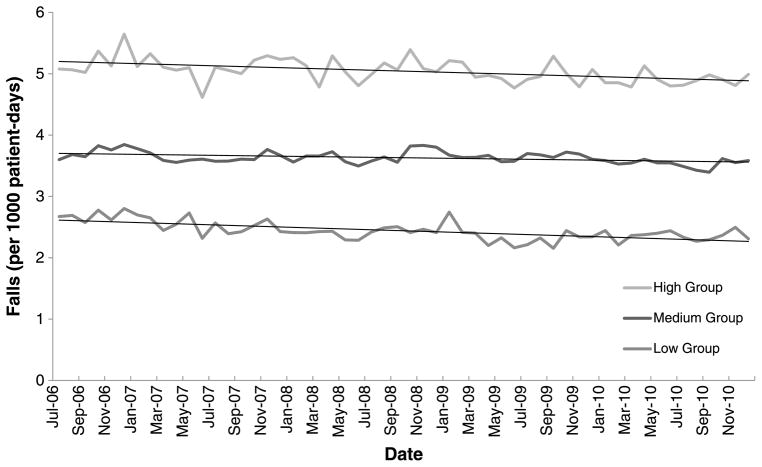
The overall mean (± standard deviation) fall rate for all observations in the data set was 3.65 (± 3.19) falls per 1,000 patient days. Using LCGM, hospitals were classified into three groups based on the linear trajectories of their monthly fall rates (see Figure 2). Of the 1,529 hospitals in the study, 348 (22.8%), 840 (54.9%), and 341 (22.3%) were classified by LCGM as consistently high, medium, and low hospital fall rate trajectory groups, respectively. Although there was a secular trend toward lower fall rates over time in each group, the mean (± standard deviation) fall rate among the high-, medium- and low-fall hospital groups was 4.96 (± 3.85), 3.63 (± 3.02), and 2.50 (± 2.50) falls per 1,000 patient days, respectively.
Figure 2.
Monthly hospital fall rate trajectory model with three groups of “consistently high” (n = 348), “consistently medium” (n = 840), and “consistently low” (n = 341)
Descriptive Characteristics of Nurse Staffing and Hospital Organizations
Table 2 summarizes the nursing staffing and organizational characteristics of hospitals in the NDNQI sample. The average TNHPPD was 8.31, and the average RN skill mix was 65.70%. In terms of bed size, approximately 51.08% of hospitals reported more than 300 total beds. When compared with general acute care hospitals in the United States, the NDNQI has a higher percentage of hospitals with bed sizes over 300 (Lake et al., 2010). In our sample, 55.20% of hospitals were classified as teaching facilities, 94.16% were located in a metropolitan location, and 28.50% of hospitals were reported as Magnet status. Sample hospitals were mainly located in the South (46.51%) and Northeast (24.68%), with the West (11.75%) and Midwest (14.38%) regions accounting for the other geographic regions. Finally, 75% of hospital falls were reported having a fall prevention protocol in place, and approximately 31% of all fall observations at the hospital-level were reported from medical units.
Table 2.
Descriptive characteristics of study hospitals (N = 1,529)
| Variable | Proportion |
|---|---|
| Hospital characteristics | |
| Bed size | |
| ≥300 | 51.08 |
| Magnet | 28.50 |
| Teaching | 55.20 |
| Metropolitan (urban/suburban) | 94.16 |
| Region | |
| Northeast | 24.68 |
| Midwest | 14.38 |
| South | 46.51 |
| West | 11.75 |
| Hospital-level nurse staffing | |
| Total nursing hours per patient day | 8.31 |
| Skill mix (mean RN, %) | 65.70 |
| Process of care | |
| Fall prevention protocol in place | 0.75 |
Note. RN = registered nurse.
Organizational Characteristics Associated With Membership in the “Consistently High” Hospital Fall Rate Group
Table 3 displays the average nurse staffing and organizational characteristics in each latent trajectory group, as well as the results of our logistic regression, including estimated ORs predicting hospital membership in the “consistently high” fall rate group.
Table 3.
Hospital-level characteristics of high, medium, and low hospital fall rate trajectory groups with odds ratios comparing “consistent high” fall rate trajectory group to “consistently medium and low” fall rate trajectory groups (N = 1,529)
| Hospital-level variable | High
|
Medium
|
Low
|
OR [95% CI]a |
|---|---|---|---|---|
| (n = 348) | (n = 840) | (n = 341) | ||
| Bed size (≥300) | 41.22 | 53.73 | 51.80 | 0.70 [0.51, 0.94]* |
| Magnet | 16.13 | 31.46 | 30.82 | 0.49 [0.34, 0.70]** |
| Teaching | 53.31 | 58.53 | 46.23 | 1.16 [0.86, 1.56] |
| Metropolitan (urban/suburban) | 91.76 | 93.97 | 94.16 | 0.81 [0.48, 1.37] |
| Region | ||||
| Northeast | 27.96 | 23.49 | 26.56 | 1.07 [0.66, 1.74] |
| Midwest | 20.07 | 14.79 | 7.14 | 1.55 [0.93, 2.58] |
| South | 39.79 | 48.75 | 45.83 | 0.81(0.51–1.28) |
| West | 10.92 | 11.29 | 13.69 | Referent |
| Hospital nurse staffing | ||||
| Total nursing hours per patient day | 8.01 | 8.36 | 8.39 | 0.92 [0.85, 0.99]* |
| Skill mix (mean RN, %) | 64.91 | 66.00 | 65.45 | 0.99 [0.98, 1.01] |
| Process of care variables | ||||
| Fall prevention protocol | 0.76 | 0.74 | 0.75 | 1.45 [0.67, 3.18] |
Note. RN = registered nurse; OR = odds ratio; CI = confidence interval.
Comparing hospitals in high-fall group with all other hospitals in medium- and low-fall groups, controlling for the proportion of medical unit observations per hospital.
Significance at p < .05.
Significance at p < .01.
In terms of nurse staffing, a higher number of TNHPPD was found to be significantly associated with lower odds of membership in the “consistently high” fall rate group (OR = 0.92, 95% confidence interval [CI] [0.85, 0.99]). In other words, a one-unit increase in TNHPPD was associated with 9% greater odds of membership in the lower fall rate groups. RN skill mix percentage was not significantly related with hospital membership in the “consistently high” fall rate group.
Findings from our logistic regression analysis also indicated that hospitals with Magnet status designation and larger bed size are significantly less likely to be in the “consistently high” fall rate trajectory group. In particular, hospitals with Magnet status were less than half as likely to be in the “consistently high” fall rate group relative to hospitals that were not reported as Magnet status (OR = 0.48, 95% CI [0.33, 0.67]). Furthermore, hospitals with 300 or more beds were associated with 43% lower odds of being in the “consistently high” fall rate group compared with hospitals with less than 300 beds (OR = 0.70, 95% CI [0.51, 0.94]).
Discussion
This study adds to the current literature in several ways. First, a majority of prior hospital falls studies have not incorporated a longitudinal design using nationwide hospital data to understand whether hospital fall rates remain consistent over time. In addition, prior studies of patient falls have been conducted predominantly at the patient level. Second, we used an innovative methodology that categorizes hospitals based on their fall rate trajectories. To our knowledge, no other study has used LCGM to classify high-and low-performing hospitals based on their fall rates over time, which represents a significant advancement in the patient safety literature. A recent article by Unruh and Zhang (2012) used a latent growth curve model to analyze the association between changes in nurse staffing and patient safety events in Florida from 1994 to 2004, but this study did not include falls as an outcome measure.
The results of our LCGM identified distinct latent classes of hospitals based on their fall rates from July 2006 through December 2010. Specifically, three linear trajectory groups emerged, and these were categorized as hospitals with “consistently high,” “consistently medium,” or “consistently low” fall rates over time. In addition, we found that hospitals did not change their fall performance over time, and if a hospital was categorized in a particular fall rate trajectory, they likely remained in this group for the entire duration of the study. These findings suggest that hospitals persistently remained in low-performing (above the mean fall rate) or high-performing (at or below the mean fall rate) linear trajectory groups over 54 months and that the 2008 CMS policy may not be as effective in reducing patient falls as policymakers anticipated after October 1, 2008.
Our investigation of nurse staffing predictors revealed that a greater number of TNHPPD were associated with membership in the consistently lower hospital fall groups, which partially supports hypothesis 1. RN skill mix was not significantly associated with membership in the “consistently high” group. The total hours of nursing care finding is not unprecedented, and a higher number of TNHPPD have been shown to be associated with lower fall rates in the nurse staffing literature (Dunton et al., 2004). However, these prior studies have not used trajectory modeling techniques to classify hospitals based on their fall rates over time, which is a significant contribution of our study. In addition, nurse staffing has been found to be important in reducing rates of adverse patient outcomes, such as mortality and failure to rescue (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002), urinary tract infections, pneumonia, and cardiac arrest (Needleman, Buerhaus, Mattke, Stewart, & Zelevinsky, 2002). Our mixed nurse staffing findings do necessitate the need for further research to better understand the association between nurse staffing and patient falls.
Magnet status was found to be a significant predictor of membership in the consistently lower fall rate trajectories, and understanding the contextual factors that contribute to these findings might provide insight into why Magnet hospitals have been successful in reducing fall rates over time. In the nurse staffing and patient falls literature, Magnet status has been shown to be associated with reductions in patient fall rates (Dunton et al., 2007; Lake et al., 2010), and other studies have also found better patient outcomes in Magnet hospitals when compared with other hospitals (Scott, Sochalski, & Aiken, 1999). A recent article by Kelly, McHugh, and Aiken (2011) found that nurses who work in Magnet hospitals reported significantly better work environments and were consistently more satisfied with their work. This may be because of the fact that Magnet hospitals tend to have more advanced technology (e.g., advanced capabilities for clinical procedures), focus more on education for nurses, and have a higher proportion of bachelor’s-prepared nurses. In addition, other key characteristics of Magnet hospitals include “flat organizational structures, unit-based decision-making processes, influential nurse executives and investments in the education and expertise of nurses” (Aiken, Havens, & Sloane, 2009, p. 26). These organizational culture and leadership factors may play an important role in nurses’ perceptions of their work environment, which in turn may lead to better nurse and patient outcomes.
Finally, hospitals with smaller bed size (less than 300 beds) were more likely to be in the “consistently high” fall rate trajectory group. These findings are consistent with an article by Dunton and colleagues (2004), who used 2002 NDNQI data and found that smaller hospitals were more likely to have higher fall rates when compared with larger hospitals. This relationship may be the result of fewer resources in smaller hospitals and an inability to maintain adequate nurse staffing levels, which represents an area for future inquiry. Although Magnet status and bed size were significantly associated with membership in the lower fall rate trajectory groups, teaching status and metropolitan area were not found to be statistically significant predictors, which only partially supported our hypothesis 2.
Limitations
Several limitations should be considered in the interpretation of our findings. First, the NDNQI sample represents a self-selected sample of hospitals. Furthermore, the NDNQI data do not allow for adjustment of patient acuity beyond controlling for unit type, which is a common and useful approach that distinguishes between severity of patient illness across clinical units (Dunton et al., 2004; Lake & Cheung, 2006). Other limitations in our study include the potential for omitted variables that are related to both the independent and dependent variables, such as hospital for-profit status and nursing-level characteristics (i.e., perceived work environment and nurse educational level). Future research should be conducted to account for these missing variables to allow for better statistical control and adjustment for additional hospital characteristics, such as those found in the American Hospital Association survey data. Finally, because fall measures and nursing covariates were aggregated to the hospital level, there is a potential for loss in variability at the unit level, which represents an area for future exploration.
Practice Implications
The results of this study have implications for policymakers, managers, and future research studies. First, given the importance of nurses to the quality of patient care, including potential reductions in falls and other important nurse-sensitive indicators, policymakers and managers should continue to assist in maintaining an adequate nursing work-force in the United States through educational programs for nurses and retention programs in health care settings (Donley et al., 2003). In addition, policy and hospital administration strategies may need to focus on some of the key aspects of Magnet accreditation, such as improving on areas of nursing education, organizational leadership, and providing better nursing work environments (Kelly et al., 2011). Because of financial constraints, all hospitals may not be able to achieve Magnet status, but there may be particular aspects of Magnet certification that might assist in reducing fall rates, and hospitals could attempt to replicate these principles of Magnet in their organizations. In addition, future qualitative studies should be conducted to better understand these mechanisms in Magnet hospitals.
Furthermore, our study reveals that there may be hospitals from which “best practices” for fall prevention might be disseminated to reduce falls. For instance, if hospitals remain in the “consistently low” fall rate trajectory group, future research could identify differences in unit-level processes of care and structural components that may impact fall rates, which would assist managers and policymakers to target interventions to these areas or create fall prevention protocols.
Acknowledgments
This study is partially funded by a National Institutes of Health Grant #RO1AG03305.
Footnotes
The authors have disclosed that they have no significant relationship with, or financial interest in, any commercial companies pertaining to this article.
Contributor Information
Damian Everhart, Email: damian.everhart@unf.edu, Assistant Professor, Brooks College of Health, University of North Florida, Jacksonville.
Jessica R. Schumacher, Associate Director of Analytics, Department of Population Health Sciences, University of Wisconsin-Madison.
R. Paul Duncan, Malcom and Christine Randall Professor and Chair, Department of Health Services Research, Management and Policy, University of Florida, Gainesville.
Allyson G. Hall, Associate Professor, Department of Health Services Research, Management and Policy, University of Florida, Gainesville.
Donna F. Neff, Associate Professor, College of Nursing, University of Central Florida, Orlando.
Ronald I. Shorr, Professor, Department of Epidemiology, University of Florida, Gainesville.
References
- Aiken L, Clarke S, Sloane D. Hospital staffing, organization, and quality of care: Cross-national findings. Nursing Outlook. 2002;50:187–194. doi: 10.1067/mno.2002.126696. [DOI] [PubMed] [Google Scholar]
- Aiken L, Clarke S, Sloane D, Sochalski J, Silber J. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken L, Havens D, Sloane D. The Magnet nursing services recognition program: A comparison of two groups of Magnet hospitals. Journal of Nursing Administration. 2009;100(3):26–35. [PubMed] [Google Scholar]
- Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent class growth modeling: A tutorial. Tutorials in Quantitative Methods for Psychology. 2009;5(1):11–24. [Google Scholar]
- Bakarich A, McMillan V, Prosser R. The effect of a nursing intervention on the incidence of older patient falls. Australian Journal of Advanced Nursing. 1997;15(1):26–31. [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Medicare program: Changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Federal Register. 2008;73(16):48433–49084. [Google Scholar]
- Cho S. Nurse staffing and adverse patient outcomes: A systems approach. Nursing Outlook. 2001;49:78–85. doi: 10.1067/mno.2001.114381. [DOI] [PubMed] [Google Scholar]
- Coussement J, De Paepe L, Schwendimann R, Denhaerynck K, Dejaeger E, Milisen K. Interventions for preventing falls in acute- and chronic-care hospitals: A systematic review and meta-analysis. Journal of the American Geriatrics Society. 2008;56:29–36. doi: 10.1111/j.1532-5415.2007.01508.x. [DOI] [PubMed] [Google Scholar]
- Cumming R, Sherrington C, Lord S, Simpson J, Vogler C, Camerson I, Naganathan V. Cluster randomized trial of a targeted multifactorial intervention to prevent falls among older people in hospital. British Medical Journal. 2008:1–6. doi: 10.1136/bmj.39499.546030.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie L. Fall and injury prevention. In: Hughes RG, editor. Patient safety and quality: An evidence-based handbook for nurses. Chapter 10. Rockville, MD: Agency for Healthcare Research and Quality; 2008. AHRQ Publication No. 08-0043. [PubMed] [Google Scholar]
- Donabedian A. The quality of care: How can it be assessed? Journal of the American Medical Association. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Donley R, Flaherty MJ, Sarsfield E, Taylor L, Maloni H, Flamagan E. What does the Nurse Reinvestment Act mean to you? Online Journal of Issues in Nursing. 2003;1(8) [PubMed] [Google Scholar]
- Dunton N, Gajewski B, Klaus S, Pierson B. The relationship of nursing workforce characteristics to patient outcomes. The Online Journal of Issues in Nursing. 2007;12(3) [Google Scholar]
- Dunton N, Gajewski B, Taunton R, Moore J. Nurse staffing and patient falls on acute care hospital units. Nursing Outlook. 2004;42:53–59. doi: 10.1016/j.outlook.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Evans D, Hodgkinson B, Lambert L, Wood J. Falls risk factors in the hospital setting: A systematic review. International Journal of Nursing Practice. 2001;7:38–45. doi: 10.1046/j.1440-172x.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- Faes M, Reelich M, Joosten-Weyn Banningh L, Gier M, Esselink R, Olde Rikkeert M. Qualitative study on the impact of falling in frail older persons and family caregivers: Foundations for an intervention to prevent falls. Aging and Mental Health. 2010;14(7):834–842. doi: 10.1080/13607861003781825. [DOI] [PubMed] [Google Scholar]
- Fischer I, Krauss M, Dunagan W, Birge S, Hitcho E, Johnson S, Fraser V. Patterns and predictors of inpatient falls and fall-related injuries in a large academic hospital. Infection Control and Hospital Epidemiology. 2005;26:822–827. doi: 10.1086/502500. [DOI] [PubMed] [Google Scholar]
- Hitcho E, Krauss M, Birge S, Dunagon W, Fischer I, Johnson S, Fraser V. Characteristics and circumstances of falls in a hospital setting. Journal of General Internal Medicine. 2004;19:732–739. doi: 10.1111/j.1525-1497.2004.30387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones B, Nagin D, Roeder K. A SAS® procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29(3):374–393. [Google Scholar]
- Kane R, Shamliyan T, Mueller C, Duval S, Wilt T. The association of registered nurse staffing levels and patient outcomes: A systematic review and meta-analysis. Medical Care. 2007;45(12):1195–1204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- Kelly L, McHugh M, Aiken L. Nurse outcomes in Magnet and Non-Magnet hospitals. Journal of Nursing Administration. 2011;41(10):428–433. doi: 10.1097/NNA.0b013e31822eddbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake E, Cheung R. Are patient falls and pressure ulcers sensitive to nurse staffing? Western Journal of Nursing Research. 2006;28(6):654–677. doi: 10.1177/0193945906290323. [DOI] [PubMed] [Google Scholar]
- Lake E, Shang J, Klaus S, Dunton N. Patient falls: Association with hospital magnet status and nursing unit staffing. Research in Nursing and Health. 2010;33(5):413–425. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang T, Hodge M, Olson V, Romano P, Kravitz R. Nurse–patient ratios: A systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes. Journal of Nursing Administration. 2004;34(7/8):326–337. doi: 10.1097/00005110-200407000-00005. [DOI] [PubMed] [Google Scholar]
- Mark B, Hughes L, Belyea M, Bacon C, Chang Y, Jones C. Exploring organizational context and structure as predictors of medication errors and patient falls. Journal of Patient Safety. 2008;4:66. [Google Scholar]
- Mayo N, Gloutney L, Levy A. A randomized trial of identification bracelets to prevent falls among patients in rehabilitation hospital. Archives of Physical Medicine and Rehabilitation. 1994;75(12):1302–1308. [PubMed] [Google Scholar]
- Montalvo I. The National Database of Nursing Quality Indicators TM (NDNQI) OJIN: The Online Journal of Issues in Nursing. 2007;12(3) Manuscript 3. [Google Scholar]
- Morse J. Enhancing the safety of hospitalization by reducing patient falls. American Journal of Infection Control. 2002;30:376–380. doi: 10.1067/mic.2002.125808. [DOI] [PubMed] [Google Scholar]
- Nagin D. Analyzing developmental trajectories: A semi-parametric, group-based approach. Psychological Methods. 1999;4:139–177. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin D. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- National Database for Nursing Quality Indicators. Guidelines for data collection and submission on quarterly indicators. Kansas City, KS: Author; 2007. [Google Scholar]
- National Quality Forum (NQF) National voluntary consensus standards for nursing-sensitive care: An initial performance measure set. Washington, DC: National Quality Forum; 2004. [Google Scholar]
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Medicine. 2002;346:1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- Oliver D, Daly F, Martin F, McMurdo M. Risk factors and risk assessment tools for falls in hospital in-patients: A systematic review. Age and Ageing. 2004;33:122–130. doi: 10.1093/ageing/afh017. [DOI] [PubMed] [Google Scholar]
- Oliver D, Healey F, Haines T. Preventing falls and fall-related injuries in hospitals. Clinical Geriatric Medicine. 2010;26:645–692. doi: 10.1016/j.cger.2010.06.005. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS® System for Microsoft Windows (version 9.2) [computer software] Cary, NC: SAS Institute; 2007. [Google Scholar]
- Scott J, Sochalski J, Aiken L. Review of Magnet hospital research: Findings and implications for professional nursing practice. Journal of Nursing Administration. 1999;29(1):9–19. doi: 10.1097/00005110-199901000-00003. [DOI] [PubMed] [Google Scholar]
- Shorr R, Guillen M, Rosenblatt L, Walker K, Caudie C, Kritchevsky S. Restraint use, restraint orders and the risk of falls in hospitalized patients. Journal of the American Geriatrics Society. 2002;50:526–529. doi: 10.1046/j.1532-5415.2002.50121.x. [DOI] [PubMed] [Google Scholar]
- Stevens J, Corso P, Finkelstein E, Miller T. The costs of fatal and non-fatal falls among older adults. Injury Prevention. 2006;12(5):290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unruh L, Zhang N. Nurse staffing and patient safety in hospitals. Nursing Research. 2012;61(1):3–12. doi: 10.1097/NNR.0b013e3182358968. [DOI] [PubMed] [Google Scholar]
- Van den Heede K, Clarke S, Sermeus W, Vleugels A, Aiken L. International experts’ perspectives on the state of nurse staffing and patient outcome literature. Journal of Nursing Scholarship. 2007;39:290–297. doi: 10.1111/j.1547-5069.2007.00183.x. [DOI] [PubMed] [Google Scholar]