Abstract
Background
Previous studies from North America and Iceland have shown that the youngest children within a grade are up to twice as likely to be diagnosed and treated for attention-deficit/hyperactivity disorder (ADHD) compared with their older classmates. We aimed to investigate whether younger age in class is associated with an increased probability of being prescribed medication for ADHD among school-aged children in Denmark.
Methods
We followed all Danish children between 2000 and 2012 from 1st through 6th grade (7–12 years). Among children who started school on their age-assigned grade level, we estimated the prevalence proportion ratio (PPR) of receiving ADHD medication between the youngest children in class (born in October–December) and the oldest in class (born in January–March), specified by grade level, calendar year and gender. As a sensitivity analysis, we added children not on their age-assigned grade level to the main calculations.
Results
We identified 932,032 eligible children for the main analysis, of whom 17.3% were among the youngest and 26.5% among the oldest in class. In total, 1.2% eligible children filled at least one prescription for ADHD medication in 2000–2012. The average PPR over the study period was 1.08 (95% CI, 1.04–1.12) and remained stable across subgroups and sensitivity analyses. Overall, 40% of children born October–December had entered school a year after their age-assigned grade level.
Conclusions
Contrary to previous study results, we observed almost no relative age effect on medication use for ADHD among children in Denmark. We postulate that this may be due to the high proportion of relatively young children held back by 1 year in the Danish school system and/or a generally low prevalence of ADHD medication use in the country.
Keywords: Attention-deficit hyperactivity disorder, central stimulants, children, age factors, drug utilization evaluation
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most commonly diagnosed mental conditions in children and may have lasting effects through adolescence and into adulthood (Biederman, 2005; Faraone, Biederman, & Mick, 2006; Steinhausen, 2009). Its diagnosis in children is a multiple-step process based on clinical evaluation, teacher ratings of behavior and performance in school and parental rating (Barkley & Edwards, 2006). The Diagnostic and Statistical Manual of Mental Disorders standard requires several symptoms to be present in two or more settings (e.g. at school and home) with evidence of clinically significant impairment in social or school/work functioning (American Psychiatric Association, 2013). Over the past two decades, an increasing number of children worldwide has been diagnosed with the condition and use of medication as a therapeutic option has risen (Asheim, Nilsen, Johansen, & Furu, 2007; Castle, Aubert, Verbrugge, Khalid, & Epstein, 2007; McCarthy et al., 2009; Pottegard, Bjerregaard, Glintborg, Hallas, & Moreno, 2012; Pottegard et al., 2013; Scheffler, Hinshaw, Modrek, & Levine, 2007; Winterstein et al., 2008; Zoega, Baldursson, & Halldorsson, 2007; Zuvekas, Vitiello, & Norquist, 2006). The underlying reasons for this increase remain somewhat unclear.
Recent studies suggest that a within-grade relative maturity disadvantage in childhood could have long-lasting negative effects on personal achievements and health outcomes (Bedard & Dhuey, 2006; Goodman, Gledhill, & Ford, 2003; Helsen, Van Winckel, & Williams, 2005). Studies from North America and Iceland also showed that the youngest children in the grade are more likely to be diagnosed and treated for ADHD (Elder, 2010; Evans, Morrill, & Parente, 2010; Morrow et al., 2012; Zoëga, Valdimarsdóttir, & Hernández-Díaz, 2012). The prevalence of use of medication for ADHD in children ranged from 3.7% to 6.3% in these studies, and the relative difference of use between the youngest and the oldest groups in the class ranged from approximately 50% (Canada, Iceland) to 100% (United States).
To better understand the structural and social mechanisms at play, the association between relative age in class and prescribing of medication for ADHD needs further study. Understanding these associations may have an impact on how maturity differences in the classroom are evaluated and handled. Importantly, they could have an impact on clinical practice by avoiding unnecessary ADHD medication of children relatively young or immature in class.
We hypothesize that being young relative to one's classmates increases the probability of being prescribed medication for ADHD and that this probability varies by children's grade level in school. Further, we hypothesize that this phenomenon has increased over the past decade with rising use of ADHD medication in Denmark. These hypotheses were addressed by using nationwide data on prescribed psychotropic medication to children living in Denmark 2000–2012.
Methods
For all children aged 7–12 years in Denmark, we obtained data from nationwide registries during the period July 1, 2000–June 31, 2012. To address the hypothesis that children's relative age in class influences their probability of receiving medication for ADHD, we compared the 1-year period prevalence proportion of ADHD medication use between the oldest and youngest children within a given grade level, thus using a prevalence proportion ratio (PPR).
Data sources
The Danish National Prescription Registry (Kildemoes, Sørensen, & Hallas, 2011) contains data on all filled prescriptions among Danish citizens since 1995. Prescription data include the type of medication, quantity and date of dispensing, but information on dosing and indication is not available. Drugs are categorized according to the World Health Organization (WHO) Anatomic Therapeutic Chemical (ATC) classification (WHO Collaborating Centre for Drug Statistics Methodology, 2012).
The Danish Student Register (Jensen & Rasmussen, 2011), was used to obtain information of children's school grade level. Since 1973, the Student Register contains information on all students in Denmark, attending 8th grade through PhD-training and, since 2007, data on the entire elementary school stage have been added, from grade 0 onwards. For children who entered school before 2007, we used children's age in 8th grade to assess whether or not they were on grade level.
The Danish Civil Registration System (Pedersen, 2011) contains data on vital status (dates of birth and death) and migrations to and from Denmark, which allowed us to keep track of all study subjects.
We merged the different national registries by use of the personal identification number, a unique identifier encoding gender and date of birth, assigned to all Danish residents (Pedersen, 2011). Data linkages were performed within Statistics Denmark, a governmental institution that collects and maintains electronic records for statistical and scientific purposes.
Study population and relative age
By default, children start 1st grade in the calendar year of their 7-year birthday. Relative age in the Danish classroom, thus, normally coincides with the order of birth months, i.e. children born in January are the oldest and children born in December are the youngest. However, parents may opt for a delayed entry into grade school if their child is considered immature for his/her age. Occasionally, they may opt for an early school entry if their child is considered particularly mature.
We started observing the study children in the year they attended 1st grade (age 7) and classified them into relative age groups within the grade level depending on month of birth; the oldest being born in January–March and the youngest being born in October–December. Of 1,209,901 children aged 7–12 years identified during the study period, we excluded a total of 75,378 (6.2%) children who did for one reason or another did not appear in the Student Registry, i.e. those home schooled, deceased, or with a delayed school entry during the last study year.
Of the 1,209,901 identified children, 202,491 (16.7%) were either behind (n = 173,791) or ahead (n = 30,543) of their age-assigned grade level. Based on data from the Student Register for study years 2008–2012, the vast majority (over 99%) of these children had entered school later or earlier than their peers, but only 1% had repeated or skipped a grade. To avoid the effect of misclassification due to grade retention or acceleration, we excluded all children (n = 202,491) not on age-assigned grade level from the main analysis. Table1 shows, however, that children behind their age-assigned grade level were mainly the relatively youngest children, i.e. those born in October–December, and were more likely to be boys than girls, thus potentially introducing a selection bias. We attempted to address the effects of such bias with multiple sensitivity analyses as described below.
Table 1.
Number of children in Denmark in 1st grade to 6th grade on age-assigned grade level, behind (delayed) or ahead (accelerated) of their grade level in school, according to birth month
| Youngest in class (October–December) | Oldest in class (January–March) | |||||
|---|---|---|---|---|---|---|
| On grade level (%) | Accelerated (%) | Delayed (%) | On grade level (%) | Accelerated (%) | Delayed (%) | |
| Overall | 112,095 (59) | 1,758 (1) | 76,750 (40) | 176,728 (88) | 14,619 (7) | 8,572 (4) |
| Gender | ||||||
| Boys | 45,814 (47) | 1,098 (1) | 49,812 (51) | 91,806 (90) | 4,686 (5) | 5,750 (6) |
| Girls | 66,281 (71) | 660 (1) | 26,938 (29) | 84,922 (87) | 9,933 (10) | 2,822 (3) |
| Study year | ||||||
| 2000 | 9,215 (57) | 302 (2) | 6,529 (41) | 14,349 (85) | 1,595 (9) | 975 (6) |
| 2001 | 10,077 (56) | 358 (2) | 7,510 (42) | 14,802 (86) | 1,507 (9) | 889 (5) |
| 2002 | 9,303 (55) | 116 (1) | 7,554 (45) | 15,775 (87) | 1,405 (8) | 877 (5) |
| 2003 | 9,181 (54) | 117 (1) | 7,848 (46) | 15,209 (87) | 1,232 (7) | 954 (5) |
| 2004 | 8,458 (53) | 142 (1) | 7,333 (46) | 15,146 (88) | 1,171 (7) | 904 (5) |
| 2005 | 8,591 (53) | 112 (1) | 7,444 (46) | 14,708 (89) | 1,045 (6) | 851 (5) |
| 2006 | 8,456 (53) | 92 (1) | 7,284 (46) | 14,727 (89) | 1,036 (6) | 783 (5) |
| 2007 | 9,324 (57) | 106 (1) | 7,065 (43) | 14,904 (89) | 1,111 (7) | 674 (4) |
| 2008 | 9,185 (58) | 154 (1) | 6,379 (41) | 14,668 (89) | 1,174 (7) | 582 (4) |
| 2009 | 9,187 (59) | 88 (1) | 6,233 (40) | 14,256 (90) | 1,118 (7) | 542 (3) |
| 2010 | 10,007 (64) | 94 (1) | 5,571 (36) | 13,811 (89) | 1,147 (7) | 541 (3) |
| 2011 | 11,111 (99) | 77 (1) | 14,373 (93) | 1,078 (7) | ||
Excluded from the main study analysis. Included in sensitivity analyses for bias.
Children with delayed school entry in 1st grade 2011 were not registered in the Student Registry by the end of the study period and did therefore not appear in any of the analyses.
The main study population comprised 932,032 children on age-assigned grade level in 1st through 6th grade (ages 7–12). To examine whether the hypothesized relative age effect continued through puberty, we then also analyzed data on children on age-assigned grade level in 7th through 9th grade (ages 13–15).
ADHD medication
We defined medication for ADHD according to the ATC classification as the following substances within the category of centrally acting sympathomimetics (N06BA): methylphenidate (N06BA04), atomoxetine (N06BA09) and modafinil (N06BA07). Children were considered prevalent users if they, at any time during the relevant study year, filled a prescription for any of these substances.
We defined use of other psychotropic medication as the filling of prescriptions for antiepileptics (N03), antipsychotics (N05A), anxiolytics (N05B), hypnotics and sedatives (N05C), or antidepressants (N06A) during the relevant study year.
Data analysis
The primary study outcome was the PPR of ADHD medication use in 2000–2012, which we calculated by dividing the 1-year prevalence proportion of ADHD medication use among the youngest children in class (born in October–December) by the 1-year prevalence proportion among the oldest in class (born in January–March). PPRs were first calculated for each individual stratum of study year (July 1–June 30), children's grade level, and gender and then reported as the average PPR from these individual strata.
As sensitivity analyses, we conducted the same calculations as in our main analysis, but changed the classification of relative age; comparing cohorts born in January with those born in December, cohorts born in January–February with those born in November–December, and finally children born in January–April with those born in September–December. Furthermore, we analyzed the PPR estimates by calendar period (2000–2005, 2006–2012), each study year, children's grade level, gender, and region of residence (the five Danish regions), as well as upon exclusion of all children using other psychotropic medication.
Lastly, we ran sensitivity analyses to examine if our results were affected by a selection bias due to exclusion of children not on age-assigned grade level: we repeated the risk analysis adding the excluded children who were behind or ahead of their grade level separately to the main study population.
All calculations were performed using STATA Release 12.0 (StataCorp, College Station, TX). The Danish Data Protection Agency and Statistics Denmark's Scientific Board approved this study. According to Danish law, ethical approval is not required for registry-based studies.
Results
Of 932,032 children in the main analysis, 161,116 (17.3%) were born in October–December (relatively young) and 246,596 (26.5%) in January–March (relatively old). Among these, 10,932 (1.2%) children filled at least one prescription for ADHD medication while under observation: 10,786 (98.7%) for methylphenidate, 2,458 (22.5%) for atomoxetine and 69 (0.6%) for modafinil. The 1-year prevalence proportion of ADHD medication use in 2011–2012 specified by birth month is depicted in Figure1.
Figure 1.
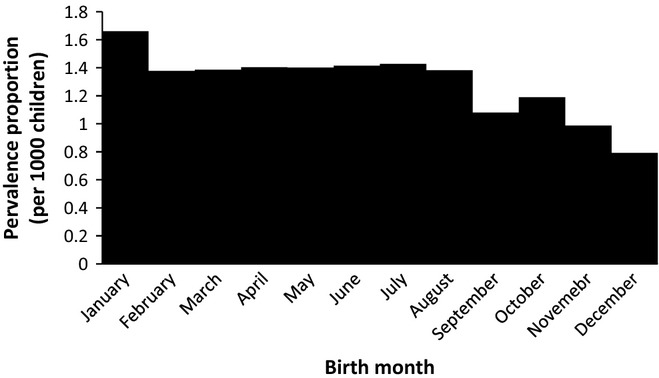
Prevalence proportions of ADHD medication use in 2011–2012 among children on age-assigned grade level, according to birth month
Over the study period (2000–2012), the 1-year prevalence proportion of ADHD medication use increased from 0.16 to 1.52 per 1,000 children among the youngest children in class and from 0.13 to 0.91 per 1,000 children among those oldest in class. The average PPR, comparing the relatively youngest children with those relatively oldest was 1.08 (95% CI, 1.04–1.12) over the entire the study period (2000–2012), but 0.93 (95% CI, 0.89–0.97) during study years 2006–2012.
The relative age effect was similar between genders. The PPR was 1.11 (CI, 1.02–1.21) for boys and 1.05 (CI, 1.00–1.09) for girls averaged over all study years and diminished respectively decreased to 0.89 (CI, 0.82–0.97) and 0.98 (CI, 0.93–1.02) in 2006–2012.
Figure2 shows that that the relative age effect was only apparent children in 4th–8th grade (ages 10–14) averaged over all study years. Throughout all study years, the youngest children in 6th grade were 1.3-fold (95% CI, 1.19–1.41) more likely to use ADHD medication compared with the oldest in 6th grade. However, in the study years 2006–2012, the younger 6th grade students were no more likely than the older 6th graders to use medication for ADHD, PPR = 0.97 (95% CI, 0.88–1.06).
Figure 2.
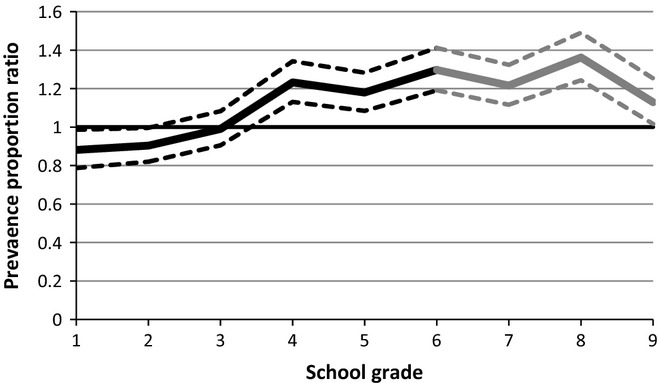
Prevalence proportion ratios* of ADHD medication use with 95% confidence intervals (dashed lines), comparing the youngest (born October–December) with the oldest (born January–March) children in class, according to grade level in school. *Prevalence proportion ratios are averaged over the total study period and calculated only for children on age-assigned grade level
Figure3 shows how the relative age effect for children in 1st–6th grade diminished with time. In the early study years, the relatively younger children were up to 1.52-fold (95% CI, 1.17–1.95) more likely than their older classmates to use medication for ADHD, while the association disappeared in study years 2004–2009 and became reversed in 2010–2012. In 2011–2012 the youngest children in class were 17% (PPR = 0.83, 95% CI, 0.75–0.92) less likely to use ADHD medication than the oldest children.
Figure 3.
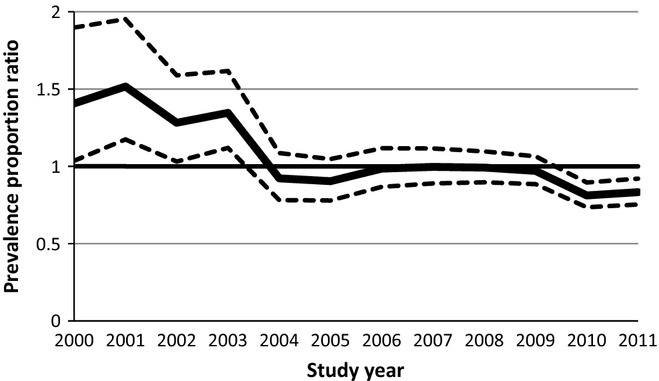
Prevalence proportion ratios* with 95% confidence intervals (dashed lines), comparing the youngest (born October–December) with the oldest (born January–March) children in class, according to study year (July 1- June 30). *Prevalence proportion ratios are averaged over all grade levels (1st–6th) and calculated only for children on age-assigned grade level
The results were not altered when we excluded users of other psychotropic medication from the analyses. Nor did stratification by children's region of residence change the results (data not shown).
Altering the limits for classification of relative age groups had only a minimal effect on in the observed relative age effect. Averaged over all study years, the overall PPR was 1.11 (95% CI, 1.03–1.19) comparing children born in December versus January; 1.02 (95% CI, 0.97–1.07) comparing children born in January–February versus November–December; and finally 1.14 (95% CI, 1.10–1.17) comparing those born in January–April versus September–December.
Finally, our sensitivity analyses for potential selection bias due to a higher proportion of excluded children born in October–December than January–March indicated that the study results were not affected by this exclusion. Adding children behind their age-assigned grade level to the main risk calculations changed the overall PPR from 1.08 to 1.09 (95% CI, 1.06–1.12).
Discussion
Contrary to our hypothesis, we found nearly no overall association between relative age among classmates and use of medication for ADHD for children in Denmark. The results of this nationwide study suggested a slightly increased probability of ADHD medication use for the relatively youngest children in grades 4th–8th during study years 2000–2004 only. But opposite to the expected, while the use of medication for ADHD became more frequent in Denmark, the slight relative age effect on ADHD medication use decreased and then vanished altogether in 2005–2012.
The strength of this study lies in its nationwide approach, covering nearly 1 million children in Denmark over more than a decade. Furthermore, the individual-level linkage with the Student Registry allowed for a detailed assessment of the use of medication for ADHD among children not attending their age-assigned grade level. The validity of the Danish prescription data used is regarded to be very high (Kildemoes et al., 2011). Denmark has a publicly funded educational system and universal health care, which may limit the generalizability of our results to other populations. However, we find the Danish classroom to be a key advantage to this study, as the high number of relatively young children with a delayed school entry allows for interpretations beyond those of previous studies on the subject in question. Given the nature of the exposure of interest (i.e. birth month), this observational study design is in effect a quasi-randomized natural experiment, with comparable risk factors distribution among relative age groups within a grade, except for season of birth. However, to avoid misclassification of relative age groups, we excluded children not on age-assigned grade level. This exclusion might in turn have distorted an otherwise equal risk factor distribution. The excluded children were more likely to be born in October–December, than during other months, and also more likely to be boys than girls. Nevertheless, our sensitivity analyses indicated that the study results remained almost the same irrespective of whether children behind or accelerated in school were included to the risk calculations.
Among the major limitations of the study are the abovementioned characteristics of the study setting, i.e. the publicly funded universal health care and education, structural and cultural factors, which may, additional to acting as a key advantage, compromise the generalizability of the results. Secondly, the study design is based on filled prescriptions for ADHD medication but not diagnoses of ADHD. Optimally, the study data would have captured all children a diagnosed with ADHD irrespective of treatment status. Finally, in this, we do not assess whether the intensity or duration of treatment with ADHD medication is associated with children's relative age in class, which could be interesting to examine in future studies.
The near absence of a relative age effect on the use of medication for ADHD in Denmark contrasts what has previously been found among children in Iceland, Canada and the United States. Recent data on 12,000 children in Iceland in 2003–2008, indicated that the youngest third of children in the elementary school class were over 50% more likely to be prescribed stimulants for ADHD compared with the oldest third (Zoëga et al., 2012). The youngest children in the Icelandic classroom were also at greater risk for poor academic performance on standardized tests in mathematics and language arts. Similarly, Morrow et al. (2012) found in a recent study of 900,000 children in British Columbia, Canada, that boys and girls born in December were 41% and 77% more likely, than those born in January, to be prescribed stimulants for ADHD. Finally, the influence of relative age on ADHD treatment has been demonstrated in two different datasets within the United States. Based on longitudinal survey data from almost 12,000 US children, Elder (2010) showed that the youngest children in 5th and 8th grades were nearly twice as likely as their older classmates to use stimulants for ADHD. Similarly, based on cross-sectional US survey data, Evans et al. (2010) found that among children 7–17 years the youngest third of children in class had, compared with the oldest third, double the chance of being diagnosed with or treated for ADHD.
None of the above studies have, however, concluded about the potential effect of holding children back in school on their findings. In our data, as many as 51% of boys and 29% of girls born in October–December were behind their age-assigned grade level, the vast majority of whom had been delayed at school entry rather than being held back by a grade later in school. It is highly conceivable that delaying school entry for relatively young and immature children could be perceived as a preventive measure to later being diagnosed and treated for ADHD. Notably, Elder and Lubotsky (2009) used comprehensive survey data to demonstrate, that children in the United States, who were an additional year older at school entry tended to have higher test scores and fewer behavioral problems than those starting school a year younger. Importantly, the authors found that starting school later reduced the chance of being diagnosed with ADHD by 50%.
We propose that the high proportion of relatively young children with delayed school entry in Denmark may play a role in the near absence of a relative age effect in our data. The conventional 12-month age span of children at school entry presents considerable differences in maturity and performance between the youngest and the oldest child in class (West, Denton, & Germino-Hausken, 2000). In addition to previous findings on the relative age effect on ADHD and treatment thereof, recent evidence also suggests that a relative maturity disadvantage in childhood could have long-lasting negative effects on personal achievements and health outcomes (Bedard & Dhuey, 2006; Goodman et al., 2003; Helsen et al., 2005). If delaying school entry for immature children does indeed prevent ADHD diagnoses and treatment, such knowledge could be of major importance for the policy regarding school entry and for the wellbeing of children. The potential benefits of delaying school entry for immature children thus warrant further investigation.
The contrasting findings between the Danish and previous results regarding the effect of relative age on ADHD medication, might also be explained by low prescribing rates of medication for ADHD to children in Denmark. The national prevalence of use among school-aged children is considerably lower in Denmark (0.9% in 7–15 year-olds, 2007) than in North America (4.6% in 6–12 year-olds, 2007) and Iceland (4.7% in 7–15 year-olds, 2007), where the relative age effect has been reported (Zoega et al., 2011; Zuvekas & Vitiello, 2012). Rates of ADHD medication use are also lower than the estimated worldwide prevalence of ADHD in children (Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007; Pottegard et al., 2012), indicating that clinicians in Denmark may be more restrictive when prescribing medication for ADHD than elsewhere. It is possible that the effect of relative age can be partly ascribed to use of ADHD medication in children who are immature rather than affected by ADHD, and that a restrictive policy would channel the medication more toward children who have ADHD in its core sense.
In conclusion, we found that in most recent years the use of medication for ADHD in Denmark is not particularly affected by children's relative age in class. This may be related to the relatively low use of ADHD medication the country and the highly prevailing custom of delaying school entry for relatively young children.
Acknowledgments
The study was funded by the University of Southern Denmark. A.P. has participated in research projects funded by Astellas with grants paid to the institution where he was employed. J.H. has participated in research projects funded by Novartis, Pfizer, Menarini, MSD, Nycomed, Astellas and Alkabello with grants paid to the institution where he was employed. He has personally received fees for teaching or consulting from the Danish Association of Pharmaceutical Manufacturers and from Nycomed, Pfizer, Novartis, Astra Zeneca, Lundbeck, Menarini, Leo Pharmaceuticals, and Ferring. S.H-D. has consulted for Novartis and GSK-Biologics for unrelated topics. H.Z. has no conflict of interests to declare. A.P. conceptualized and designed the study, carried out all analyses, interpreted the findings, drafted the methods and results, reviewed and revised the manuscript, and approved the final manuscript as submitted. J.H. verified all analyses, interpreted the findings, reviewed and revised the manuscript, and approved the final manuscript as submitted. S.H-D. interpreted the findings, reviewed and revised the manuscript, and approved the final manuscript as submitted. H.Z. conceptualized and designed the study, interpreted the findings, drafted the introduction and discussion, reviewed and revised the manuscript, and approved the final manuscript as submitted. A.P. and J.H had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Key points
Previous studies from North America and Iceland have shown that the youngest children within a grade are up to twice as likely to be diagnosed and treated for ADHD compared with their older classmates.
The use of medication for ADHD in Denmark is not particularly associated with children's relative age in class. This might be due to the highly prevailing custom in Denmark of delaying school entry for the youngest children in school cohorts.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edn. Arlington, VA: American Psychiatric Publishing; 2013. Available from: WWW.dsm.psychiatryonline.org [last accessed 20 December 2013] [Google Scholar]
- Asheim H, Nilsen KB, Johansen K. Furu K. Prescribing of stimulants for ADHD in Nordland County. Tidsskrift for den Norske Laegeforening. 2007;127:2360–2362. [PubMed] [Google Scholar]
- Barkley RA. Edwards G. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. In: Murphy KR, editor; Barkley RA, editor. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. 3rd edn. New York, NY: Guilford Press; 2006. pp. 337–388. [Google Scholar]
- Bedard K. Dhuey E. The persistence of early childhood maturity: International evidence of long-run age effects. Quarterly Journal of Economics. 2006;121:1437–1472. [Google Scholar]
- Biederman J. Attention-deficit/hyperactivity disorder: A selective overview. Biological Psychiatry. 2005;57:1215–1220. doi: 10.1016/j.biopsych.2004.10.020. [DOI] [PubMed] [Google Scholar]
- Castle L, Aubert RE, Verbrugge RR, Khalid M. Epstein RS. Trends in medication treatment for ADHD. Journal of Attention Disorders. 2007;10:335–342. doi: 10.1177/1087054707299597. [DOI] [PubMed] [Google Scholar]
- Elder TE. The importance of relative standards in ADHD diagnoses: Evidence based on exact birth dates. Journal of Health Economics. 2010;29:641–656. doi: 10.1016/j.jhealeco.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder TE. Lubotsky DH. Kindergarten entrance age and children's achievement impacts of state policies, family background, and peers. Journal of Human Resources. 2009;44:641–683. [Google Scholar]
- Evans WN, Morrill MS. Parente ST. Measuring inappropriate medical diagnosis and treatment in survey data: The case of ADHD among school-age children. Journal of Health Economics. 2010;29:657–673. doi: 10.1016/j.jhealeco.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J. Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Goodman R, Gledhill J. Ford T. Child psychiatric disorder and relative age within school year: Cross sectional survey of large population sample. British Medical Journal. 2003;327:472–475. doi: 10.1136/bmj.327.7413.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helsen WF, Van Winckel J. Williams AM. The relative age effect in youth soccer across Europe. Journal of Sports Sciences. 2005;23:629–636. doi: 10.1080/02640410400021310. [DOI] [PubMed] [Google Scholar]
- Jensen VM. Rasmussen AW. Danish education registers. Scandinavian Journal of Public Health. 2011;39(7 Suppl):91–94. doi: 10.1177/1403494810394715. [DOI] [PubMed] [Google Scholar]
- Kildemoes HW, Sørensen HT. Hallas J. The Danish national prescription registry. Scandinavian Journal of Public Health. 2011;39(7 Suppl):38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- McCarthy S, Asherson P, Coghill D, Hollis C, Murray M, Potts L. Wong ICK. Attention-deficit hyperactivity disorder: Treatment discontinuation in adolescents and young adults. British Journal of Psychiatry. 2009;194:273–277. doi: 10.1192/bjp.bp.107.045245. [DOI] [PubMed] [Google Scholar]
- Morrow RL, Garland EJ, Wright JM, Maclure M, Taylor S. Dormuth CR. Influence of relative age on diagnosis and treatment of attention-deficit/hyperactivity disorder in children. Canadian Medical Association Journal. 2012;184:755–762. doi: 10.1503/cmaj.111619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen CB. The Danish civil registration system. Scandinavian Journal of Public Health. 2011;39(7 Suppl):22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- Polanczyk G, de Lima M, Horta B, Biederman J. Rohde L. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. American Journal of Psychiatry. 2007;164:942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- Pottegard A, Bjerregaard BK, Glintborg D, Hallas J. Moreno SI. The use of medication against attention deficit hyperactivity disorder in Denmark: A drug use study from a national perspective. European Journal of Clinical Pharmacology. 2012;68:1443–1450. doi: 10.1007/s00228-012-1265-y. [DOI] [PubMed] [Google Scholar]
- Pottegard A, Bjerregaard BK, Glintborg D, Kortegaard LS, Hallas J. Moreno SI. The use of medication against attention deficit/hyperactivity disorder in Denmark: A drug use study from a patient perspective. European Journal of Clinical Pharmacology. 2013;69:589–598. doi: 10.1007/s00228-012-1344-0. [DOI] [PubMed] [Google Scholar]
- Scheffler RM, Hinshaw SP, Modrek S. Levine P. The global market for ADHD medications. Health Affairs. 2007;26:450–457. doi: 10.1377/hlthaff.26.2.450. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC. The heterogeneity of causes and courses of attention-deficit/hyperactivity disorder. Acta Psychiatrica Scandinavica. 2009;120:392–399. doi: 10.1111/j.1600-0447.2009.01446.x. [DOI] [PubMed] [Google Scholar]
- West J, Denton K. Germino-Hausken E. America's kindergartners: Findings from the early childhood longitudinal study, kindergarten class of 1998–99, fall 1998 (NCES 2000–070). US Department of Education. National Center for Education Statistics. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2013. Oslo: WHO Collaborating Centre for Drug Statistics Methodology; 2012. [Google Scholar]
- Winterstein AG, Gerhard T, Shuster J, Zito J, Johnson M, Liu HZ. Saidi A. Utilization of pharmacologic treatment in youths with attention deficit/hyperactivity disorder in medicaid database. Annals of Pharmacotherapy. 2008;42:24–31. doi: 10.1345/aph.1K143. [DOI] [PubMed] [Google Scholar]
- Zoega H, Baldursson G. Halldorsson M. Use of methylphenidate among children in Iceland 1989-2006. Læknablaðið. 2007;93:825–832. [PubMed] [Google Scholar]
- Zoega H, Furu K, Halldorsson M, Thomsen PH, Sourander A. Martikainen JE. Use of ADHD drugs in the Nordic countries: A population-based comparison study. Acta Psychiatrica Scandinavica. 2011;123:360–367. doi: 10.1111/j.1600-0447.2010.01607.x. [DOI] [PubMed] [Google Scholar]
- Zoëga H, Valdimarsdóttir UA. Hernández-Díaz S. Age, academic performance, and stimulant prescribing for ADHD: A nationwide cohort study. Pediatrics. 2012;130:1012–1018. doi: 10.1542/peds.2012-0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuvekas SH. Vitiello B. Stimulant medication use among US children: A twelve-year perspective. The American Journal of Psychiatry. 2012;169:160. doi: 10.1176/appi.ajp.2011.11030387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuvekas S, Vitiello B. Norquist G. Recent trends in stimulant medication use among US children. American Journal of Psychiatry. 2006;163:579–585. doi: 10.1176/ajp.2006.163.4.579. [DOI] [PubMed] [Google Scholar]


