Abstract
Objective:
To estimate effective dose of cone beam CT (CBCT) of the facial skeleton with focus on measurement methods and scanning protocols.
Methods:
A systematic review, which adhered to the preferred reporting items for systematic reviews (PRISMA) Statement, of the literature up to April 2014 was conducted. Data sources included MEDLINE®, The Cochrane Library and Web of Science. A model was developed to underpin data extraction from 38 included studies.
Results:
Technical specifications of the CBCT units were insufficiently described. Heterogeneity in measurement methods and scanning protocols between studies made comparisons of effective doses of different CBCT units and scanning protocols difficult. Few studies related doses to image quality. Reported effective dose varied across studies, ranging between 9.7 and 197.0 μSv for field of views (FOVs) with height ≤5 cm, between 3.9 and 674.0 μSv for FOVs of heights 5.1–10.0 cm and between 8.8 and 1073.0 μSv for FOVs >10 cm. There was an inconsistency regarding reported effective dose of studies of the same CBCT unit with the same FOV dimensions.
Conclusion:
The review reveals a need for studies on radiation dosages related to image quality. Reporting quality of future studies has to be improved to facilitate comparison of effective doses obtained from examinations with different CBCT units and scanning protocols. A model with minimum data set on important parameters based on this observation is proposed.
Advances in knowledge:
Data important when estimating effective dose were insufficiently reported in most studies. A model with minimum data based on this observation is proposed. Few studies related effective dose to image quality.
Since introduction in the late 1990s, cone beam CT (CBCT) has become a common modality to image the facial skeleton. There is currently a large variety of CBCT units on the market,1,2 and technical improvements are made continuously, such as the development of the field of view (FOV) from one fixed size to several sizes as well as stitched FOVs in the more recent models.
The use of CBCT has increased dramatically, but published evidence supporting informed clinical decision-making is weak.1 As is the case with emerging healthcare technologies, it will take some time to produce evidence on the cost-effectiveness of CBCT for different diagnostic tasks including “costs” in terms of radiation dosages. Meanwhile, the use of CBCT and choice of scanning protocol has to rely on good practice related to the image quality needed for the actual diagnostic task and the amount of radiation exposure to the patient. The literature on dose levels of CBCT is, however, difficult to grasp and interpret owing to the diversity of CBCT units and different approaches taken in radiation dosimetry.
The aim of this systematic review was to estimate the effective dose of CBCT of the facial skeleton with focus on measurement methods and scanning protocols used. Such a review can be beneficial when aiming to perform CBCT examinations with a radiation exposure as low as diagnostically acceptable (ALADA).3 A review may also highlight both strengths and weaknesses in study design to date and can thereby support sound study design in future research.
METHODS AND MATERIALS
The literature review was conducted in accordance with the preferred reporting items for systematic reviews (PRISMA) Statement4 and guidance of Centre for Reviews and Dissemination for undertaking reviews in healthcare.5 The following steps were defined: (i) review questions, (ii) literature searches, (iii) study selection and (iv) data extraction and synthesis.
REVIEW QUESTIONS
Regarding CBCT of the facial skeleton, the review questions were as follows:
– Which methods and scanning protocols were used when measuring and estimating the radiation dosage?
– What are the effective doses?
The following terms were based on Medical Subject Headings (MeSH):
– CBCT/instrumentation: CT modalities that use a cone- or pyramid-shaped beam of radiation.
– Facial bones: the facial skeleton, consisting of bones situated between the cranial base and the mandibular region. While some consider the facial bones to comprise the hyoid (hyoid bone), palatine (hard palate), zygomatic (zygoma) bones, mandible and maxilla, others include also the lacrimal and nasal bones, inferior nasal concha and vomer but exclude the hyoid bone.
– Radiation dosage as stated above defined according to MeSH.
– Thermoluminescent dosimetry as stated above defined according to MeSH.
The following terms not included in MeSH were defined as:
– Dental CT: CBCT used for the oral and maxillofacial region.
– Effective dose according to International Commission on Radiation Protection (ICRP) publication 103:6 the tissue-weighted sum of the equivalent doses in all specified tissues and organs of the body.
– Material to measure radiation dosages: dosemeters and read-outs.
– Scanning protocols: exposure parameters and phantom features.
LITERATURE SEARCHES
The searches were designed together with university librarians. The search strategies are presented in Table 1. The following electronic databases were searched: MEDLINE® using PubMed as search engine, the Web of Science and the Cochrane Database of Systematic Reviews in The Cochrane Library. The search in MEDLINE was based on MeSH terms and free-text terms. The searches in Web of Science and The Cochrane Library (the Cochrane Database of Systematic Reviews) were performed using free-text terms. Additional hand search was carried out using the reference lists of retrieved systematic reviews.
Table 1.
Search strategies and number of publications retrieved from MEDLINE®, the Web of Science and the Cochrane Library
| Indexing terms | Publications (n) |
|---|---|
| MEDLINE | |
| #1 Cone Beam Computed Tomography (MeSH) | 3150 |
| #2 Cone Beam Computed Tomography | 4968 |
| #3 Dental CT | 4727 |
| #4 Radiation Dosage (MeSH) | 67,196 |
| #5 Radiation Dosage | 110,803 |
| #6 Thermoluminescent Dosimetry (MeSH) | 2873 |
| #7 Thermoluminescent Dosimetry | 3274 |
| #8 = #1 OR #2 | 4968 |
| #9 = #8 OR #3 | 9226 |
| #10 = #4 OR #5 | 110,803 |
| #11 = #6 OR # 7 | 3274 |
| #12 = #10 OR #11 | 112,099 |
| #13 = #9 AND #12 | 737 |
| Web of Science | |
| Topic = (Radiation Dosage) OR Topic = (Thermoluminescent Dosimetry) AND Topic = (Cone Beam Computed Tomography) | 3000 |
| Refined by: Web of Science Categories = (DENTISTRY ORAL SURGERY MEDICINE) | 92 |
| The Cochrane Library | |
| There are 6 results from 783,686 records for your search on “(Radiation Dosage OR Thermoluminescent Dosimetry) AND Cone Beam Computed Tomography in title abstract keywords in Trials” | 6 |
MeSH, Medical Subject Headings.
Search conducted on the 22 April 2014.
STUDY SELECTION
Eligibility assessment of half of the retrieved titles and abstracts was performed independently by two authors, and two other authors assessed the other half of the titles and abstracts. When at least one of the authors regarded a record as having met the inclusion criteria, it was ordered and read in full text. Reviewers were not blinded to authors and institutions of the records during the study selection process.
The inclusion criteria were
– Publication type: original study or systematic review.
– CBCT unit: described regarding brand and version, FOV dimensions, degree of rotation, X-ray beam type (pulsed or continuous radiation).
– Anatomical region: facial region, further detailed and described in studies of FOVs ≤10 cm.
– Material: equipment to measure radiation dosage (dosemeters and read-outs).
– Outcomes: data on effective dose based on ICRP 60—19907 or ICRP 103—20076
– Language: abstract in English and full-text publication in English, German or Japanese.
DATA EXTRACTION AND DATA SYNTHESIS
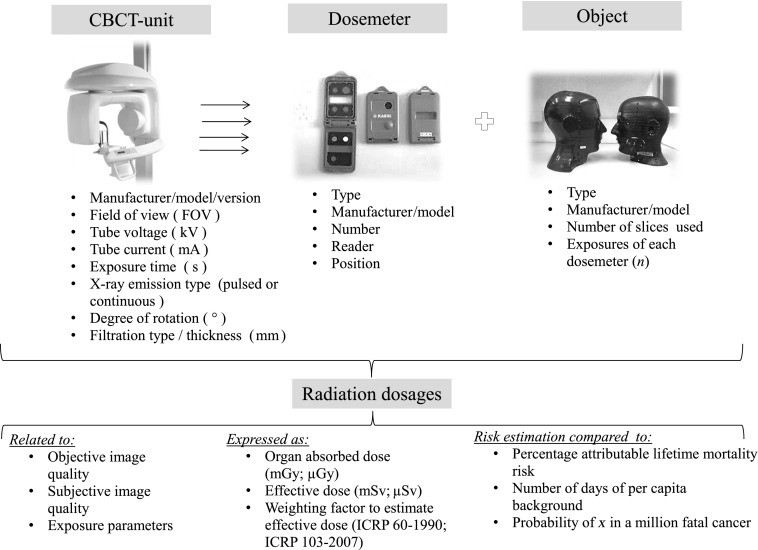
We developed a model with components that were considered important when performing studies of radiation dosages in CBCT (Figure 1) and a data extraction sheet. Information was extracted from each study on (i) the CBCT unit(s), (ii) method to measure and estimate radiation dosages, (iii) scanning protocol, (iii) object and (iv) radiation dosages. When information of the CBCT unit was insufficient, information was searched for on the manufacturer's website. Together, the authors pilot tested the data extraction sheet on five included studies. The authors had different professional backgrounds and experience: one radiophysicist, two specialists (>25 years' experience) and two trainees in oral and maxillofacial radiology. One author extracted data from included studies, and the other authors checked the extracted data independently. Disagreement was resolved by discussion.
Figure 1.
A model presenting the steps for data extraction with different parameters important when analysing radiation dosages in cone beam CT (CBCT) of the facial skeleton. FOV, field of view; ICRP, International Commission on Radiation Protection.
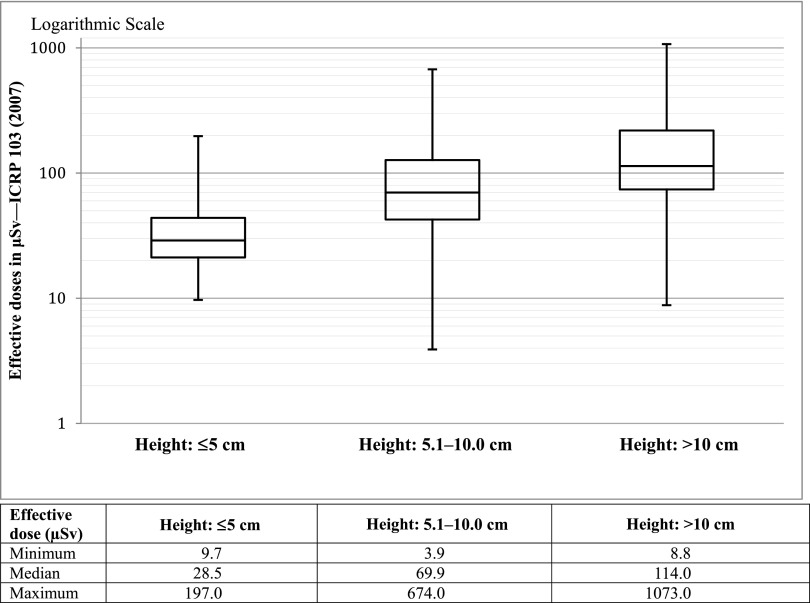
Effective doses for three heights of FOV (≤5 cm, 5.1–10.0 cm and >10.0 cm) were compiled in a spreadsheet. Median values, 25 and 75 percentiles, and range for effective dose values were calculated using software (Microsoft Office Excel® 2010; Microsoft Corporation, Redmond, WA).
RESULTS
Study selection
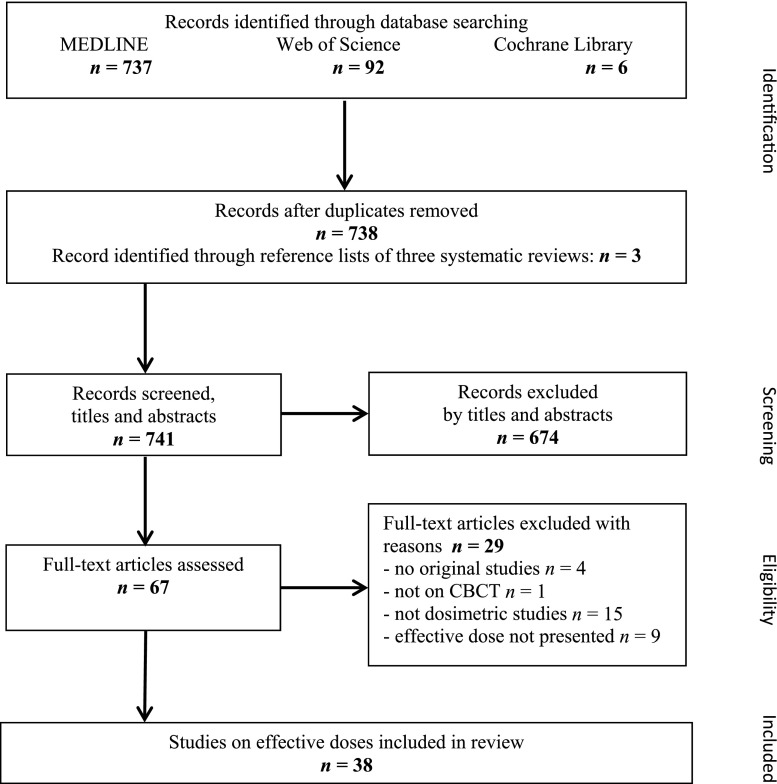
Figure 2 shows the number of publications identified, excluded and included. Of the retrieved publications, 674 were discarded because, after reviewing the abstracts, it appeared that these publications did not meet the inclusion criteria. The full text of the remaining 67 publications was examined, and 38 met the inclusion criteria. Three systematic reviews were excluded because their research question was different to that of the present review, but an additional three studies were identified and included by checking the reference lists of these reviews. Most included studies were published from 2008 onwards, the number of studies being the highest in 2008 and 2012.
Figure 2.
Flow chart according to the preferred reporting items for systematic reviews (PRISMA) statement4 presenting study selection process with number of publications identified, excluded and included for systematic review of effective dose of cone beam CT (CBCT) of the facial skeleton.
Methods and scanning protocols used to measure and estimate radiation dosages
The methods used to measure radiation dosages varied across the studies (Table 2). The following methods were used: thermoluminescent dosemeter (TLD) 100 (25 studies), TLD-100H (8 studies), optically stimulated luminescence dosemeter (OSLD) (2 studies), radiochromic film (2 studies), ionization chamber (2 studies), magnesium orthosilicate doped with terbium (Mg2SiO4:Tb; TLD-MSO-S) (1 study), lithium borate (Li2B4O7)-TLD (1 study) and photoluminescence glass (1 study). Also, the type of phantom, the number of slices, dosemeters and exposures of each dosemeter varied across studies (Table 2). In most studies, a commercially available anthropomorphic phantom including an adult male skull was used. A phantom that included a female skull was examined in three studies and a paediatric phantom (corresponding to a person 10 years of age) in two studies. In two studies, the phantom was developed at the institution (University of Göttingen, Göttingen, Germany) where the study was performed. Only in one study40 was the phantom repositioning between scans described in enough detail to ascertain reproducibility. The method for distribution of dosemeters as described by Ludlow et al27 was applied in most studies. The number of phantom slices ranged between 7 and 10 and the number of TLDs was about 24 in most studies. The number of exposures of dosemeters ranged between 1 and 10, except for 1 study using 34 exposures.44 In seven studies, there was no information about the number of TLDs, and in one-third of the studies there was no information about the number of exposures of dosemeters.
Table 2.
Methodology for measurements and estimation of the radiation dosage in cone beam CT (CBCT) of the facial skeleton
| Study | Dosemeter |
Object |
Radiation dosage presented as: – Organ absorbed dose – Effective dose – Weighting factor to estimate effective dose (ICRP 607— 1990; ICRP 1036—2007) |
Comments | ||
|---|---|---|---|---|---|---|
| Number (n) | Exposures of each dosemeter (n) | Phantom – Type (manufacturer) – Size |
Slices used (n) | |||
| TLD-100 | ||||||
| Kim et al8 | 22 | NA | – ART head and neck phantom (Radiology Support Devices, Inc., Long Beach, CA) – Adult male |
9 | – Equivalent organ absorbed dose – Effective dose – ICRP 2007 |
Conversion coefficients from the DAP |
| Schilling and Geibel9 | 24 | – Prescan 50 – Scan 3 |
– Alderson RANDO® ART-210 (Radiology Support Devices, Inc.) – Adult male |
9 | – Organ absorbed dose – Effective dose – ICRP 1990, 2007 |
Organ absorbed dose from middle ranges for each unit |
| Rottke et al10 | 48 | 10 | – RANDO head phantom (The Phantom Laboratory, Salem, NY) | 8 | – NA – Effective dose – ICRP 2007 |
|
| Davies et al11 | 72 | 10 | – RANDO head (The Phantom Laboratory) – Adult male |
7 | – NA – Effective dose – ICRP 1990, 2007 |
|
| Grünheid et al12 | 24 | 3 | – RANDO (The Phantom Laboratory) – Adult male |
7 | – NA – Effective dose – ICRP 2007 |
|
| Jeong et al13 | 3 × 25 | NA | – ART (Radiology Support Devices, Inc.) – Adult |
16 | – Organ absorbed dose – Effective dose – ICRP 2007 |
Compared with CT with low-dose technique |
| Pauwels et al14 | 147; 152 | NA | – Two ART head and neck phantom (Radiology Support Devices, Inc.) – Adult male |
11 | – Organ absorbed dose – Effective dose – ICRP 2007 |
|
| Rampado et al15 | 50 | 10 | – RANDO head phantom (The Phantom Laboratory) | 9 | – NA – Effective dose – ICRP 2007 |
|
| Sezgin et al16 | 21 | NA | – RANDO head phantom | NA | – NA – Effective dose – ICRP 2007 |
Compared with panoramic radiography and CT |
| Librizzi et al17 | 78 | 3 | – RANDO (The Phantom Laboratory) | NA | – Organ absorbed dose – Effective dose – ICRP 2007 |
Image quality assessed as presence or absence of erosion of temporomandibular joint by two radiologists |
| Ludlow18 | 24 | 9 or 10 | – RANDO (Nuclear Associates, Hicksville, NY) – Adult |
7 | – Organ absorbed dose – Effective dose – ICRP 1990, 2007 |
Doses with and without 0.4-mm copper filtration |
| Carrafiello et al19 | 42 | NA | – RANDO (Alderson Research Laboratories, Inc., New York, NY) | 10 | – NA – Effective dose – ICRP 1990 |
Subjective image quality: analysed spongy bone, teeth, surrounding structure and soft tissues Assessed on five-point scale by two observers |
| Qu et al20 | 63 | 5 | – ART phantom, model ART-210 (Radiology Support Devices, Inc.) – Adult male |
7 | – Organ absorbed dose – Effective dose – ICRP 1990, 2007 |
|
| Faccioli et al21 | 46 | NA | – RANDO (Alderson Research Laboratories, Stanford, CN) – NA |
NA | – Organ absorbed dose – Effective dose – ICRP 2007 |
Image quality assessed as high and low contrast resolution, uniformity and noise |
| Loubele et al22 | NA | 10 | – Two RANDO (Alderson Research Laboratories, NY) – Male |
20 | – NA – Effective dose – ICRP 2007 |
|
| Roberts et al23 | 72 | 10 | – RANDO – Adult |
8 | – NA – Effective dose – ICRP 1990, 2007 |
|
| Coppenrath et al24 | Unclear | NA | – RANDO | NA | – Organ absorbed dose – Effective dose – ICRP 1990 |
Compared with CT |
| Ludlow and Ivanovic25 | 24 | 3 | – RANDO (Nuclear Associates) – Adult male |
7 | – NA – Effective dose – ICRP 1990, 2007 |
Compared with CT and average panoramic dose |
| Palomo et al26 | 10 | 1 | – RANDO head phantom (The Phantom Laboratory) | 7 | – Organ absorbed dose – Effective dose – ICRP 1990, 2007 |
|
| Ludlow et al27 | 24 | 3 | – RANDO (Nuclear Associates) – Adult male |
7 | – NA – Effective dose – ICRP 1990, 2005 draft recommendations |
|
| Wörtche et al28 | NA | NA | – RANDO | NA | – NA – Effective dose – ICRP 2005 draft recommendations |
|
| Tsilakis et al29 | 25 | NA | – RANDO (Alderson Research Laboratories, CN) | NA | – NA – Effective dose – ICRP 1990, ICRP 1990 + salivary glands |
|
| Ludlow et al30 | NA | 10 | – RANDO (Nuclear Associates) – Small adult |
7 | – NA – Effective dose – ICRP 1990, ICRP 1990 + salivary glands |
|
| Mah et al31 | NA | 2 | – Humanoid, tissue-equivalent dosimetry phantom (Humanoid Systems Inc., Torrance, CA) | NA | – Organ absorbed dose – Effective dose – ICRP 1990 |
Compared with panoramic radiography and CT |
| Cohnen et al32 | 26 | 2 | – RANDO | 13 | – NA – Effective dose – NA |
Image quality assessed as mean image noise |
| TLD-100H | ||||||
| Davies et al11 | 72 | 10 | – RANDO (The Phantom Laboratory) – Male |
7 | – NA – Effective dose – ICRP 1990, 2007 |
|
| Pauwels et al14 | 147; 152 | NA | – Two ART head and neck phantom (Radiology Support Devices, Inc.) – Adult male |
11 | – Organ absorbed dose – Effective dose – ICRP 2007 |
Different numbers of TLDs used for two phantoms |
| Qu et al33 | 3 chips Positioned at 21 locations (3 × 21) |
5 | – Anthropomorphic ART-210 (Radiology Support Devices, Inc.) – Adult male |
7 | – NA – Effective dose – ICRP 2007 |
Evaluated influence of thyroid collars |
| Qu et al34 | 63 | 5 | – Anthropomorphic ART-210 (Radiology Support Devices, Inc.) – Adult male |
7 | – NA – Effective dose – ICRP 2007 |
Different oral and maxillofacial regions with and without thyroid collar |
| Theodorakou et al35 | 10 years: 104 Adolescents: 140 |
NA | – ATOM® model 702-c, 706-c (Computerized Imaging Reference System Inc., Norfolk, VA) | 10 years: 10 Adolescent: 11 |
– Organ absorbed dose – Effective dose – ICRP 2007 |
|
| Loubele et al22 | NA | 10 | – Two RANDO (Alderson Research Laboratories, NY) – Male |
20 | – NA – Effective dose – ICRP 2007 |
TLD-100H used for organs and tissues expected to receive low dose |
| Hirsch et al36 | 48 | 5 | – Anthropomorphic (developed at University of Göttingen, Göttingen, Germany) | 16 sites | – Mean absorbed dose – Effective dose – ICRP 2007 |
|
| Silva et al37 | 48 | 5 | – Anthropomorphic (developed at University of Göttingen) | NA | – NA – Effective dose – ICRP 2007 |
Compared with panoramic radiography, lateral cephalometry and CT |
| TLD-MSO-S | ||||||
| Okano et al38 | 132 | 2 | – RANDO – Female body phantom |
All | – Organ absorbed dose – Effective dose – ICRP 1990, 2007 |
|
| Lithium borate (Li2B4O7)-TLDs | ||||||
| Suomalainen et al39 | 26 | NA | – RANDO (Nuclear Associates) and RSVP Phantom™ (The Phantom Laboratory, Salem, NY) | NA | – Organ absorbed dose – Effective dose – ICRP 1990, 2007 |
Image quality assessed as CNR and MTF |
| Optically stimulated luminescence dosemeter | ||||||
| Ludlow and Walker40 | 24 | 2–12 exposures | – ATOM Max model 711 HN and ATOM model 706 HN (Computerized Imaging Reference System Inc.) – Adult male and 10-year-old child |
9 | – Equivalent organ dose – Effective dose – ICRP 2007 |
Image quality assessed as contrast, homogeneity, CNR, MTF, polymethylmethacrylate voxel and noise, Nyqvist frequency |
| Lukat et al41 | 25 | 3 | – RANDO (Alderson Research Laboratories, CT) – Male |
7 | – Equivalent organ dose – Effective dose – ICRP 2007 |
|
| Ionization chamber | ||||||
| Vassileva and Stoyanov42 | Not applicable | NA | – NA | NA | – NA – Effective dose – ICRP 1990, 2007 |
Air kerma–area product |
| Lofthag-Hansen et al43 | Not applicable | NA | – For CTDI100: CT head dose phantom type 76-414 (Victoreen Instruments, Cleveland, OH) | NA | – NA – Effective dose – NA |
Measurement of radiation exposure Effective dose based on CTDI100 Effective dose based on DAP Patient examinations |
| Photoluminescence glass | ||||||
| Okano et al44 | 155 | 3D Accuitomo(J Morita Mfg. Corp., Kyoto, Japan): 100 CB MercuRay (Hitachi Medical Corp., Tokyo, Japan): 50 |
– RANDO (Alderson Research Laboratories, CT) – Female |
34 | – Organ absorbed dose – Effective dose – ICRP 1990, 2007 |
Compared with panoramic radiography and CT 34 slices from skull to pelvic bones |
| Radiochromic film | ||||||
| Al-Okshi et al45 | 3–4 sheets | 10–50 | – RANDO (The Phantom Laboratory) – Small adult |
6 | – Organ absorbed dose – Effective dose – CRP 2007 |
Compared with panoramic radiography |
| Rampado et al15 | 50 pieces Width, 5 mm Length, 25 mm |
10 | – RANDO (The Phantom Laboratory) | 9 | – NA – Effective dose – ICRP 2007 |
Compared TLD with Gafchromic film (International Specialty Products Corp., Wayn, NJ) |
CNR, contrast-to-noise ratio; CTDI, CT dose index; DAP, dose–area product; ICRP, International Commission on Radiation Protection; MTF, modulation transfer function; NA, information not available; TLD, thermoluminescent dosemeter.
Complete technical specifications of the CBCT unit were described in only one study.40 Supplementary information, such as the degree of rotation or trajectory arc, filtration and detector specifications, was partly accessible on the manufacturers' websites.
What are the effective doses of cone beam CT examinations of the facial skeleton?
Effective doses and individual study characteristics are presented in Supplementary Tables A–C. In seven studies, ICRP 1990 and ICRP 2007 weights were presented so that the effect of the change from 1990 weights to 2007 in effective dose calculations could be estimated. The increase of the estimated effective dose using 2007 compared with 1990 was on average 173% (range, 58–350) for FOVs with height ≤5 cm, 164% (range, 64–276) for FOVs 5.1–10.0 cm and 76% (13–180) for FOVs with height >10 cm.
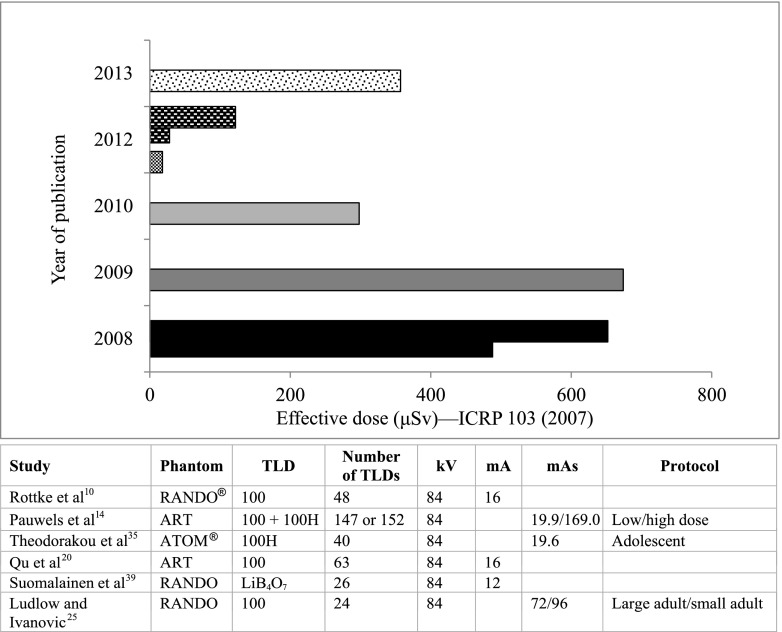
As presented in Figure 3, effective dose was influenced by the height of the FOV. The reduction of the median effective dose of FOVs with height 5.1–10.0 cm compared with that of FOVs with height >10 cm was 38%. The reduction of the median effective dose of FOVs with height ≤5 cm compared with that of FOVs with height 5.1–10.0 cm was 59%. The maximum effective dose of the smallest FOVs overlapped the median dose of the FOVs with height 5.1–10.0 cm and the same applied to the FOVs of medium and large heights (Figure 3). The ranges between the highest and lowest doses of each FOV height were wide (Figure 3). As presented in Figure 4, there was a variation in reported dose estimates for the same CBCT unit with the same FOV dimensions.10,14,20,25,35,39 As the description of technical parameters of the CBCT units examined was incomplete, it was difficult to evaluate which components of the CBCT units that produced the different results on effective doses in these studies. Besides, different phantoms, dosemeter types and number, exposure parameters and protocols were applied in these studies (Figure 4).
Figure 3.
Box and whisker diagram of effective doses (µSv) of cone beam CT units with three heights of fields of view. ICRP, International Commission on Radiation Protection.
Figure 4.
Effective doses (µSv) of different versions of the same cone beam CT unit with the field of view of 8 × 8 cm2 presented in studies published 2008–13. ART, Radiology Support Devices Inc., A Carson, CA; ATOM®, Computerized Imaging Reference System, Norfolk, VA. ICRP, International Commission on Radiation Protection; TLD, thermoluminescent dosemeter.
In addition to the size, the positioning of the FOV influenced the effective dose. The dose of FOVs of <10 cm was higher for examination of the lower jaw than for the upper jaw23,30 and for examinations with the FOV positioned on the posterior part of the lower jaw than for the anterior part of the upper jaw.14,38,45 The effective dose was reduced by 43% when 0.4-mm copper filtration was added in examinations with FOV heights 9 and 18 cm.18
Effective dose was related to image quality in six studies (Table 2) expressed as objective image quality21,32,39,40 or subjective image quality.17,19 As presented in Table 2, the effective dose of CBCT was compared with those of other imaging modalities in eight studies: CT,13,16,24,25,37,44 panoramic radiography16,25,31,37,44,45 and cephalometry.37 Risk estimations were presented in eight studies12,18,23,25,27,30,35,45 mostly as comparisons with background radiation.
DISCUSSION
This systematic review revealed that key methodological details of measurement methods and scanning protocols were missing. We did not implement any quality evaluation in this systematic review, as there is no validated tool for this publication type, as is the case for quality evaluation of diagnostic studies. If the model proposed in Figure 1 had been used as a quality tool, all but one study40 would have been excluded, as technical data of the CBCT units was insufficiently described.
TLD-100 was used in most studies, probably owing to the fact that TLD-100 is not only used in the field of dosimetry but also for monitoring personnel radiation doses, which means that the method is a well established clinical routine. The main advantages of the TLD-100 are good sample-to-sample uniformity, nearly tissue equivalent and simple calibration procedures using common radionuclide sources. According to Al Najjar et al,46 TLDs may be less accurate in the lower dose range than OSLDs, which were used in two recent studies.40,41 The results of the study by Ludlow and Walker40 showed, however, that TLDs and OSLDs yielded differences of <2% in the calculation of effective dose in CBCT. Radiochromic film, used in two studies,15,45 is, compared with TLDs, easier to adjust on the phantom in relation to the radiation field and present a continuous “analog”-like dose distribution, where the limit for spatial resolution is set by the pixel size when digitizing the image in the flatbed scanner.45 CT dose index (CTDI) or the dose–area product (DAP) in combination with a conversion factor was used in one study.47 When used for CBCT dosimetry, both CTDI and DAP have been criticized. CTDI underestimates the dose by failing to measure scatter radiation to tissues outside the scan region.25 DAP value represents only the surface dose and effective doses based on DAP conversion factor have been found to be inaccurate for small FOVs.43 As revealed by this review, radiation dosages have been measured and estimated with dosimetric methods used in conventional dental radiography, such as intraoral and panoramic radiography, and in CT. There are, however, significant differences between these imaging modalities, for example, dose distribution and scanning geometry, which entail a different approach to measurements of the radiation for CBCT. The shortcoming of the CTDI concept is well known, and the International Atomic Energy Agency48 and American Association of Physicists in Medicine49 have proposed recommendations on new CTDI type measurements but, as of yet, there is not any new dosimetry standard established.
The nature and size of the phantom, number of sections and the position and extension of the organs inside the phantom varied across the studies. In most studies, an adult RANDO® anthropomorphic phantom was used but the attenuation varies as each RANDO phantom is constructed around a real human skull or synthetic bone material. A specific phantom has been developed (SedentexCT IQ CBCT Phantom; Leeds Test Object Ltd, Boroughbridge, UK) that has been shown to be valid for assessment of image quality parameters.50 There were only two studies using a paediatric phantom corresponding to patients aged 10 years.35,40 This is notable as CBCT is increasingly replacing two-dimensional imaging modalities, such as cephalometry and panoramic radiography, in adolescents aged 10–18 years undergoing orthodontic treatment. As the justification for an increased dose to this young patient group is unclear,1 there is an urgent need to estimate effective doses in relation to diagnostic tasks when examining these patients.
One known factor influencing effective dose is the dimension of the FOV. If all other factors affecting the dose remain constant, a larger FOV results in a higher dose. The dose range for the same FOV height was wide, which is in line with the results presented in the review by Bornstein et al51 and overlapped for different FOV heights indicating that several factors influence the effective dose. This was further highlighted in our synthesis of the results of six studies of the same CBCT unit with the same FOV dimensions.10,14,20,25,35,39 The positioning of FOV with heights ≤10 cm was shown to influence dose such that exposure of the posterior part of the lower jaw resulted in higher effective dose than did the anterior part of the upper jaw,14,38,45 because salivary gland and thyroid tissues receive little exposure when the FOV is centred on the anterior upper jaw.
Since effective dose was related to image quality in few studies, it is difficult to assess how the dose can be reduced and still achieve the diagnostic aims of a CBCT examination. Image quality of rotation of 180° and 360° was compared in examinations of the posterior parts of the jaws, and it was concluded that “a rotation of 180° gave good subjective image quality, hence a substantial dose reduction can be achieved without loss of diagnostic information”.52 It remains, however, to produce more evidence on how the reduction of the scan arc from 360° to 180° in combination with other factors will influence image quality for different diagnostic tasks. As stated by Ludlow and Walker,40 “As optimization and dose reduction become more of a focus for CBCT manufacturers, the effect on image quality will need close attention.”
Our review has limitations. Although the literature search was performed with some language limitation and only in databases, not in reference lists of included studies, some studies were probably missed. However, the search was in accordance with assessment of multiple systematic reviews (AMSTAR),53 which proposes a search of at least two electronic sources. As the definition of facial skeleton in MeSH guided the study selection, studies of the soft tissues and surrounding regions of the facial skeleton were excluded. Key methodological data of measurement methods and scanning protocols were missing, which made data extraction difficult and might have induced bias. Heterogeneity between how effective doses were measured and calculated in the included studies is likely to have an effect on our calculations of the median values for different FOV heights.
In conclusion, although there were many studies on effective dose of CBCT of the facial skeleton, the quality of the evidence is low on how different diagnostic tasks and appropriate image quality should be matched with different scanning protocols to accord with the ALADA principle. According to grading of recommendations assessment, development and evaluation (GRADE),54 the quality of evidence is low when there is a limitation to the study quality, important inconsistency of estimates of effects across studies and an uncertainty about important consequences. As this is the case for effective dose in CBCT, further research is very likely to have an impact on our confidence in the estimates of effective doses. For estimations, and in particular comparisons of effective doses of different CBCT units and scanning protocols, a more complete reporting is required. A minimum data, as presented in the model presented in Figure 1, has to be reported in future studies on optimization and image quality of CBCT examinations.
REFERENCES
- 1.European Commission. Radiation protection no. 172: cone beam CT for dental and maxillofacial radiology. Evidence based guidelines. A report prepared by the SEDENTEXCT project. Luxembourg: European Commission; 2011. [Cited 27 November 2014.] Available from: http://ec.europa.eu/energy/nuclear/radiation_protection/doc/publication/172.pdf [Google Scholar]
- 2.Nemtoi A, Czink C, Haba D, Gahleitner A. Cone beam CT: a current overview of devices. Dentomaxillofac Radiol 2013; 42: 20120443. doi: 10.1259/dmfr.20120443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bushberg JT. Science, radiation protection, and the NCRP: building on the past, looking to the future. In: NCRP Fiftieth Annual Meeting Program; 10–11 March 2014; Bethesda, MD. Bethesda, MD: National Council on Radiation Protection and Measurements. pp. 5–7.
- 4.Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8: 336–41. doi: 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 5.Akers J, Aguiar-Ibáñez R, Baba-Akbari Sari A, Beynon S, Booth A, Burch J, et al. Systematic reviews: CRD's guidance for undertaking reviews in health care. Vol. III. York, UK: Centre for Reviews and Dissemination; 2009. pp. 294. [Google Scholar]
- 6.International Commission on Radiation Protection. The 2007 recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 2007; 37: 1–332. [DOI] [PubMed] [Google Scholar]
- 7.International Commission on Radiological Protection. The 1990 recommendations of the International Commission on Radiological Protection. ICRP publication 60. Ann ICRP 1991; 21: 1–201. [PubMed] [Google Scholar]
- 8.Kim DS, Rashsuren O, Kim EK. Conversion coefficients for the estimation of effective dose in cone-beam CT. Imaging Sci Dent 2014; 44: 21–9. doi: 10.5624/isd.2014.44.1.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schilling R, Geibel MA. Assessment of the effective doses from two dental cone beam CT devices. Dentomaxillofac Radiol 2013; 42: 20120273. doi: 10.1259/dmfr.20120273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rottke D, Patzelt S, Poxleitner P, Schulze D. Effective dose span of ten different cone beam CT devices. Dentomaxillofac Radiol 2013; 42: 20120417. doi: 10.1259/dmfr.20120417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davies J, Johnson B, Drage N. Effective doses from cone beam CT investigation of the jaws. Dentomaxillofac Radiol 2012; 41: 30–6. doi: 10.1259/dmfr/30177908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grünheid T, Kolbeck Schieck JR, Pliska BT, Ahmad M, Larson BE. Dosimetry of a cone-beam computed tomography machine compared with a digital x-ray machine in orthodontic imaging. Am J Orthod Dentofacial Orthop 2012; 141: 436–43. doi: 10.1016/j.ajodo.2011.10.024 [DOI] [PubMed] [Google Scholar]
- 13.Jeong DK, Lee SC, Huh KH, Yi WJ, Heo MS, Lee SS, et al. Comparison of effective dose for imaging of mandible between multi-detector CT and cone-beam CT. Imaging Sci Dent 2012; 42: 65–70. doi: 10.5624/isd.2012.42.2.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 2012; 81: 267–71. doi: 10.1016/j.ejrad.2010.11.028 [DOI] [PubMed] [Google Scholar]
- 15.Rampado O, Bianchi SD, Peruzzo Cornetto A, Rossetti V. Ropolo R. Radiochromic films for dental CT dosimetry: a feasibility study. Phys Med 2014; 30: 18–24. doi: 10.1016/j.ejmp.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 16.Sezgin ÖS, Kayipmaz S, Yasar D, Yilmaz AB, Ozturk MH. Comparative dosimetry of dental cone beam computed tomography, panoramic radiography, and multislice computed tomography. Oral Radiol 2012; 28: 32–7. [Google Scholar]
- 17.Librizzi ZT, Tadinada AS, Valiyaparambil JV, Lurie AG, Mallya SM. Cone-beam computed tomography to detect erosions of the temporomandibular joint: effect of field of view and voxel size on diagnostic efficacy and effective dose. Am J Orthod Dentofacial Orthop 2011; 140: e25–30. doi: 10.1016/j.ajodo.2011.03.012 [DOI] [PubMed] [Google Scholar]
- 18.Ludlow JB. A manufacturer's role in reducing the dose of cone beam computed tomography examinations: effect of beam filtration. Dentomaxillofac Radiol 2011; 40: 115–22. doi: 10.1259/dmfr/31708191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carrafiello G, Dizonno M, Colli V, Strocchi S, Pozzi Taubert S, Leonardi A, et al. Comparative study of jaws with multislice computed tomography and cone-beam computed tomography. [In Italian.] Radiol Med 2010; 115: 600–11. doi: 10.1007/s11547-010-0520-5 [DOI] [PubMed] [Google Scholar]
- 20.Qu XM, Li G, Ludlow JB, Zhang ZY, Ma XC. Effective radiation dose of ProMax 3D cone-beam computerized tomography scanner with different dental protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 770–6. doi: 10.1016/j.tripleo.2010.06.013 [DOI] [PubMed] [Google Scholar]
- 21.Faccioli N, Barillari M, Guariglia S, Zivelonghi E, Rizzotti A, Cerini R, et al. Radiation dose saving through the use of cone-beam CT in hearing-impaired patients. Radiol Med 2009; 114: 1308–18. doi: 10.1007/s11547-009-0462-y [DOI] [PubMed] [Google Scholar]
- 22.Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 2009; 71: 461–8. doi: 10.1016/j.ejrad.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 23.Roberts JA, Drage NA, Davies J, Thomas DW. Effective dose from cone beam CT examinations in dentistry. Br J Radiol 2009; 82: 35–40. doi: 10.1259/bjr/31419627 [DOI] [PubMed] [Google Scholar]
- 24.Coppenrath E, Draenert F, Lechel U, Veit R, Meindl T, Reiser M, et al. Cross-sectional imaging in dentomaxillofacial diagnostics: dose comparison of dental MSCT and NewTom 9000 DVT. [In German.] Fortschr Röntgenstr 2008; 180: 396–401. doi: 10.1055/s-2008-1027142 [DOI] [PubMed] [Google Scholar]
- 25.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 106–14. doi: 10.1016/j.tripleo.2008.03.018 [DOI] [PubMed] [Google Scholar]
- 26.Palomo JM, Rao PS, Hans MG. Influence of CBCT exposure conditions on radiation dose. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105: 773–82. doi: 10.1016/j.tripleo.2007.12.019 [DOI] [PubMed] [Google Scholar]
- 27.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006; 35: 219–26. [DOI] [PubMed] [Google Scholar]
- 28.Wörtche R, Hassfeld S, Lux CJ, Mussig E, Hensley FW, Krempien R, et al. Clinical application of cone beam digital volume tomography in children with cleft lip and palate. Dentomaxillofac Radiol 2006; 35: 88–94. [DOI] [PubMed] [Google Scholar]
- 29.Tsilakis K, Donta C, Gavala S, Karayianni K, Kamenopoulou V, Hourdakis CJ. Dose reduction in maxillofacial imaging using low dose cone beam CT. Eur J Radiol 2005; 56: 413–17. [DOI] [PubMed] [Google Scholar]
- 30.Ludlow JB, Davies-Ludlow LE, Brooks SL. Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. Dentomaxillofac Radiol 2003; 32: 229–34. [DOI] [PubMed] [Google Scholar]
- 31.Mah JK, Danforth RA, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 508–13. [DOI] [PubMed] [Google Scholar]
- 32.Cohnen M, Kemper J, Möbes O, Pawelzik J, Mödder U. Radiation dose in dental radiology. Eur Radiol 2002; 12: 634–7. [DOI] [PubMed] [Google Scholar]
- 33.Qu X, Li G, Sanderink G, Zhang ZY, Ma XC. Dose reduction of cone beam CT scanning for the entire oral and maxillofacial regions with thyroid collars. Dentomaxillofacial Radiol 2012; 41: 373–8. doi: 10.1259/dmfr/30200901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qu X, Li G, Zhang Z, Ma X. Thyroid shields for radiation dose reduction during cone beam computed tomography scanning for different oral and maxillofacial regions. Eur J Radiol 2012; 81: e376–80. doi: 10.1016/j.ejrad.2011.11.048 [DOI] [PubMed] [Google Scholar]
- 35.Theodorakou C, Walker A, Horner K, Pauwels R, Bogaerts R, Jacobs R, et al. Estimation of paediatric organ and effective doses from dental cone beam CT using anthropomorphic phantoms. Br J Radiol 2012; 85: 153–60. doi: 10.1259/bjr/19389412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hirsch E, Wolf U, Heinicke F, Silva MA. Dosimetry of the cone beam computed tomography Veraviewepocs 3D compared with the 3D Accuitomo in different fields of view. Dentomaxillofac Radiol 2008; 37: 268–73. doi: 10.1259/dmfr/23424132 [DOI] [PubMed] [Google Scholar]
- 37.Silva MA, Wolf U, Heinicke F, Bumann A, Visser H, Hirsch E. Cone-beam computed tomography for routine orthodontic treatment planning: a radiation dose evaluation. Am J Orthod Dentofacial Orthop 2008; 133: 640.e1–5. doi: 10.1016/j.ajodo.2007.11.019 [DOI] [PubMed] [Google Scholar]
- 38.Okano T, Matsuo A, Gotoh K, Yokoi M, Hirukawa A, Okumura S, et al. Comparison of absorbed and effective dose from two dental cone beam computed tomography scanners. [In Japanese.] Nihon Hoshasen Gijutsu Gakkai Zasshi 2012; 68: 216–25. [DOI] [PubMed] [Google Scholar]
- 39.Suomalainen A, Kiljunen T, Käser Y, Peltola J, Kortesniemi M. Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofac Radiol 2009; 38: 367–78. doi: 10.1259/dmfr/15779208 [DOI] [PubMed] [Google Scholar]
- 40.Ludlow JB, Walker C. Assessment of phantom dosimetry and image quality of i-CAT FLX cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2013; 144: 802–17. doi: 10.1016/j.ajodo.2013.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lukat TD, Wong JC, Lam EW. Small field of view cone beam CT temporomandibular joint imaging dosimetry. Dentomaxillofac Radiol 2013; 42: 20130082. doi: 10.1259/dmfr.20130082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vassileva J, Stoyanov D. Quality control and patient dosimetry in dental cone beam CT. Radiat Prot Dosimetry 2010; 139: 310–12. doi: 10.1093/rpd/ncq011 [DOI] [PubMed] [Google Scholar]
- 43.Lofthag-Hansen S, Thilander-Klang A, Ekestubbe A, Helmrot E, Gröndahl K. Calculating effective dose on a cone beam computed tomography device: 3D Accuitomo and 3D Accuitomo FPD. Dentomaxillofac Radiol 2008; 37: 72–9. doi: 10.1259/dmfr/60375385 [DOI] [PubMed] [Google Scholar]
- 44.Okano T, Harata Y, Sugihara Y, Sakaino R, Tsuchida R, Iwai K, et al. Absorbed and effective doses from cone beam volumetric imaging for implant planning. Dentomaxillofac Radiol 2009; 38: 79–85. doi: 10.1259/dmfr/14769929 [DOI] [PubMed] [Google Scholar]
- 45.Al-Okshi A, Nilsson M, Petersson A, Wiese M, Lindh C. Using GafChromic film to estimate the effective dose from dental cone beam CT and panoramic radiography. Dentomaxillofac Radiol 2013; 42: 20120343. doi: 10.1259/dmfr.20120343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al Najjar A, Colosi D, Dauer LT, Prins R, Patchell G, Branets I, et al. Comparison of adult and child radiation equivalent doses from 2 dental cone-beam computed tomography units. Am J Orthod Dentofacial Orthop 2013; 143: 784–92. doi: 10.1016/j.ajodo.2013.01.013 [DOI] [PubMed] [Google Scholar]
- 47.Lofthag-Hansen S, Thilander-Klang A, Gröndahl K. Evaluation of subjective image quality in relation to diagnostic task for cone beam computed tomography with different fields of view. Eur J Radiol 2011; 80: 483–8. doi: 10.1016/j.ejrad.2010.09.018 [DOI] [PubMed] [Google Scholar]
- 48.International Atomic Energy Agency. Status of computed tomography dosimetry for wide cone beam scanners. IAEA human health reports no. 5. Vienna, Austria: International Atomic Energy Agency; 2011. [Google Scholar]
- 49.American Association of Physicists in Medicine, Task Group III. Comprehensive methodology for the evaluation of radiation dose in X-ray computed tomography. AAPM report no. III. College Park, MD: American Association of Physicists in Medicine; 2010. [Google Scholar]
- 50.Bamba J, Araki K, Endo A, Okano T. Image quality assessment of three cone beam CT machines using the SEDENTEXCT CT phantom. Dentomaxillofac Radiol 2013; 42: 20120445. doi: 10.1259/dmfr.20120445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risk. Int J Oral Maxillofac Implants 2014; 29: 55–77. doi: 10.11607/jomi.2014suppl.g1.4 [DOI] [PubMed] [Google Scholar]
- 52.Lofthag-Hansen S. Cone beam computed tomography radiation dose and image quality assessments. Swed Dent J Suppl 2010: 4–55. [PubMed] [Google Scholar]
- 53.Shea B, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007; 7: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. ; GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004; 328: 1490. [DOI] [PMC free article] [PubMed] [Google Scholar]