Abstract
Objective
The complexity of psychotherapies has been a barrier to community implementation. We used the Research Domain Criteria consensus as a guide to develop Engage, a streamlined, neurobiology-based psychotherapy for late-life depression that may match the skill set of practicing clinicians. This proof of concept study tested the hypotheses that Engage is bioequivalent to Problem Solving Therapy (PST) in reducing depressive symptoms, inducing remission, and ameliorating disability.
Methods
Engage assumes that abnormal function of the positive valence systems fuels depression and uses “reward exposure” (engagement in meaningful, rewarding activities) as its principal intervention. Negativity bias, apathy, and emotional dysregulation are expressions of abnormalities in the negative valence, arousal and regulatory, and cognitive control systems respectively. Engage targets each of them with simple interventions only if they interfere with reward exposure. We treated openly with 9 weekly sessions of Engage 39 older adults with unipolar major depression. We compared their course of depression (HAM-D), remission rate (HAM-D<10), and disability (WHODAS) with those of a historical comparison group (N=97) treated with 9 weekly sessions of PST.
Results
Community social workers and research therapists required one third as much training time in Engage as in PST. Engage was non-inferior to PST in reducing HAM-D and WHODAS. Remission rates for Engage at 6 and 9 weeks were 18.2%, and 41.1%. The corresponding figures for PST were 13.7% and 35.0%.
Conclusion
These initial observations suggest that Engage has comparable efficacy with PST in reducing depressive symptoms and disability and warrants a randomized controlled trial.
Introduction
Evidence-based psychotherapies are rarely employed and sustained in the community.1,2 There are several causes of this science to service gap. One cause, specific to behavioral interventions, is the complexity of interventions and the competencies community clinicians must acquire and sustain over time in order to deliver them.3
A solution is to streamline behavioral interventions and tailor them to the settings and therapist skill level available in the community. We have suggested that neurobiological knowledge can offer biologically meaningful behavioral targets and guide the development of simplified psychotherapies.4 This view was based on the Research Domain Criteria (RDoC) Project, which reflects a current consensus on the readiness of neurobiology to guide treatment development.5 The fundamental assumption of the RDoC Project is that mental disorders are caused by brain circuit abnormalities and that biosignatures of these systems can augment the understanding and management of behavioral abnormalities. The RDoC further defined five neural systems (positive valence, negative valence, cognitive, social processes, and arousal/regulatory systems) whose dysfunction may promote psychopathology.
We theorized that dysfunction in domains of the RDoC positive valence systems is a process central to late life depression.4 This assertion is supported by animal studies demonstrating that triggers of depression influence the structure and function of circuits of reward-related, depression-like behaviors.6 Along with animal findings, depressed patients have high impulsivity and time inconsistency in tasks of gain and loss,7 suggesting a dysfunction in the positive valence systems domain of reward valuation. Deficits in reward-based decisions and high variability in action selection accompany depressive symptoms8 and are consistent with impairment in the domain of action selection/preference-based decision-making. Depressed patients have attenuated responses of the nucleus accumbens, the caudate, and other anteroventral striatum structures in response to reward paradigms.9,10 Aging impairs reward processing, influences the flexibility of adaptation to changes in reward contingencies,11 and increases sensitivity to punishment.12 These abnormalities are consistent with a dysfunction of the action selection/preference-based decision-making domain of the positive valence system.
Based on the assumption that abnormal function of the positive valence systems is a mechanism fueling depression, Engage uses “reward exposure”, which consists of engagement in meaningful social and physical activities, to promote the function of these systems. Negativity bias, apathy, and emotional dysregulation are clinical manifestations of depression that can serve as barriers to reward exposure. Negativity bias, consisting of selective attention to negative information, is a “cognitive vulnerability” factor for depression.13 Negativity bias can be viewed as a clinical expression of the RDoC negative valence systems' domain of loss. Negativity bias is associated with high activation of brainstem, amygdala, anterior cingulate cortex (ACC), and ventral and dorsal medial prefrontal cortex (PFC) to fear.14 Hyper-reactivity of the amygdala has been associated with sensitivity to negative stimuli15 and negative bias in the processing or interpretation of emotional stimuli.14,16 Apathy can be viewed as an expression of dysfunction in the arousal/modulation domain of the RDoC arousal and regulatory system. It occurs in conditions impairing the ventral striatum, dorsal anterior cingulate cortex (ACC), ventral globus pallidus, and medial thalamus.17 In late-life depression, apathy is accompanied by low resting functional connectivity of the nucleus accumbens (NAcc) with the amygdala, caudate, putamen, globus pallidus, and thalamus and increased connectivity with the insula and dorsomedial PFC.18 Emotional dysregulation can be considered a behavioral expression of the cognitive control domain of the RDoC cognitive systems. It may result from abnormal interaction of the ventral-rostral ACC and medial PFC, responsible for appraisal and regulation of emotional functions, and limbic subcortical circuits of emotion processing.19,20 Normal older adults react less than younger adults to negative situations,21 have lower amygdala and higher prefrontal activation in response to emotional stimuli,22 and have greater medial prefrontal control over negative input.23 However, many depressed older adults have vascular disease compromising prefrontal white matter and impairing cognitive control mechanisms of emotional regulation.22
We used the above assumptions to create Engage, a streamlined psychotherapy consisting of select psychotherapeutic components of known efficacy.4 Accordingly, the principal intervention of Engage is “reward exposure” intended to reignite the positive valence systems. Thus, Engage is personalized through a structured, stepped approach focusing on “reward exposure” and targets negativity bias (negative valence systems), apathy (arousal systems), and emotional dysregulation (cognitive control system) only if they interfere with “reward exposure”. Its psychotherapeutic components are simplified so that they can be understood by many depressed older patients and taught to large numbers of clinicians. This proof of concept study compares the time needed to train therapists in Engage and in Problem Solving Therapy (PST) and compares the efficacy of Engage to that of PST offered to a historical comparison group, part of the COPE-D Study.24,25 Unlike Engage, which focuses on exposure to meaningful and rewarding activities, PST imparts a specific problem solving method that patients may use to reconceptualize and address problems as they occur.
Methods
This is an open treatment trial of Engage. Its design was approved by the IRBs of both Cornell and UCSF.
Participants
Older adults recruited by Cornell and UCSF met the following inclusion criteria: 1) Age≥ 60 years; 2) unipolar, non-psychotic major depression (by SCID26, DSM-IV); 3) Mini-Mental State Examination (MMSE) ≥ 24; 4) off antidepressants or have been on a stable dose of an antidepressant for 12 weeks and do not intend to change the dose in the next 10 weeks; and 5) capacity to consent. Exclusion Criteria were: 1) Intent or plan to attempt suicide in the near future; 2) history or presence of psychiatric diagnoses other than unipolar, nonpsychotic major depression or generalized anxiety disorder; 3) use of psychotropic drugs or cholinesterase inhibitors other than mild doses of benzodiazepines.
Engage
“Reward exposure” (facilitation of meaningful, rewarding activities) is the principal intervention of Engage offered throughout treatment. Interventions are added only in patients with barriers impeding reward exposure. Patients and therapists develop a list of rewarding activity goals and select 2-3 activities to pursue between sessions. During sessions, they: 1. select a rewarding activity; 2. develop a list of ideas of how to meet this goal; 3. choose one of these ideas; and 4. make an “action plan” with concrete steps to address obstacles to implementation. Engage differs from PST in that it uses problem solving in the service of reward exposure rather than imparting problem solving skills to strengthen the patients' behavioral repertoire. In patients who do not engage in rewarding activities, the initial three sessions help the therapist to identify a “barrier” to reward exposure, i.e. negativity bias, apathy, or emotional dysregulation.
Strategies for negativity bias include Practicing Positivity Bias toward engagement, playing Devil's Advocate for thoughts interfering with engagement, Weighing the Evidence to motivate patients to pursue activities, writing Alternative Positive Explanations to negative thoughts interfering with engagement in rewarding activities, and learning how Positive People Respond. Strategies for apathy consist of prompts to action plans, e.g. checklists, reminders, labels, tape recorders, electronic instructions to start tasks, calls to prompt action plans, and family and friends acting as prompts. Strategies for emotional dysregulation consist of distraction, meditation, relaxation exercises, deep breathing, and imagery. Patients are taught to practice their selected strategy in session and then on their own, so that they can use it when they sense difficulties while pursuing “reward exposure.”
Therapist Training
Therapists were instructed to read the Engage Manual and the trainers (PA or PR) offered two 45-minute didactics. Then, therapists had one-to-one role-play sessions in which a trainer first demonstrated a role-play, and after role-reversal, evaluated each trainee's fidelity to Engage with the Engage Adherence Scale (E-AS). Therapists were assigned “practice cases” and required to achieve E-AS scores≥ 4 on two consecutive sessions to be certified. Similar training procedures were used in the PST group.
Historical Comparison Group
We used participants of the COPE-D Study treated with PST.24,25 PST is efficacious in late-life depression24,25,27,28 and can provide therapy exposure similar to Engage. PST uses problem solving as a skill set that, once acquired, is used to address a broad range of life difficulties, reduce stress, and facilitate adaptation.
Systematic Assessment
Diagnosis was assigned in research conferences by agreement of two clinician investigators after review of clinical history and the SCID-R. All other research data were obtained by trained interviewers.
Severity of depression was assessed with the 24-item Hamilton Depression Rating Scale (HAM-D).29 Disability was quantified by the interviewer-administered World Health Organization Disability Assessment Schedule II-12 item (WHODAS).30 The WHODAS yields a composite score of disability after assessing the domains of: Understanding and communicating, getting around, self-care, getting along with others, household and work activities, and participation in society.
Overall cognitive impairment was assessed with the MMSE. Memory was assessed with the Hopkins Verbal Learning Test (HVLT). Age of onset for first episode of major depression was assessed with the SCID-R26 and neuroticism with the subscale of the NEO.31
After baseline assessment, the HAM-D and WHODAS were assessed at 6 and 9 weeks. Payment for transportation and arrangements was provided to all meetings when necessary. Compensation for time spent in assessments was offered, but not for treatment sessions.
Analysis of Data
We used mixed-effects linear regression analyses32 to compare HAM-D and WHODAS scores (baseline, weeks 6, and 9) between Engage and PST. The model included a random intercept fixed effects for treatment arm, site, time and time × treatment interaction. Age, gender, education were included as covariates and retained in the model if significant. Non-inferiority of Engage was based on the treatment difference at week 9. We concluded non-inferiority if the difference between Engage and PST fell below an assumed non-inferiority margin (M) that separated clinically meaningful from clinically negligible difference, i.e. the null hypothesis was Engage-PST≥2.25 HAM-D average points. We used a one-sided test at α=5% to compute an one-sided 95% confidence interval of the post-treatment difference (Engage-PST), and concluded non-inferiority if the upper bound of this CI was less than 2.25 HAM-D points. The effect size (Cohen's d) for end of treatment difference was based on the mixed model estimated least-square means and pooled standard deviations (raw) at week 9. Comparison of odds of remission at week 6 and 9 were studied a logistic regression model. All analyses were performed with SAS 9.3.
Results
Therapist Skill Acquisition and Fidelity to Treatment
We trained 6 community social workers (3 MSWs and 3 LCSWs) and 7 research therapists in Engage and 60 community social workers and 20 research therapists in PST. We assessed fidelity to practice sessions with review of therapists' notes and audiotapes using Adherence Forms. Both community social workers (mean: 6.92 hours, SD: 2.40 vs. 22.54, SD: 1.09; t=13.68, df=64, p<0.0001) and research therapists (mean: 5.14 hours, SD: 1.31 vs. 19.05, SD: 1.47; t=23.41, df=25, p<0.0001) required shorter total training time to be certified in Engage than in PST.
Post training fidelity to treatment manuals was examined by reviewing audiotapes of 63 Engage and 93 PST sessions. Approximately 12.7% (8/63) of Engage sessions and 36.6% (34/93) PST sessions required corrective feedback (χ2=10.87, df=1, p<.00098).
Efficacy
Engage was administered to 39 older adults with major depression (Table 1). Of these, 36 received nine sessions completed in an average 9.91 weeks (SD: 1.86, range: 7.43 to 15.00). One participant had 8 sessions, and 2 had 7 sessions. Approximately 97% (38/39) of participants completed the 6 week research assessment and 95% (37/39) completed the 9 week assessment.
Table 1.
Baseline characteristics of older participants with major depression treated with Engage and of historical controls who received Problem Solving Therapy.
|
Engage (N = 39) |
PST (N = 97) |
Mann-Whitney test | |
|---|---|---|---|
|
| |||
| Mean (SD) 71.8% | Mean (SD) 73.2% | p | |
| Female (%) | 71.8% | 73.2% | .868ˆ |
| Age | 72.8 (8.0) | 72.8 (7.7) | .895 |
| Education (years) | 16.7 (5.9) | 15.02 (2.6) | .088 |
| HAM-D* | 20.4 (4.9) | 23.6 (4.0) | .001 |
| WHODAS II** | 27.3 (7.6) | 27.2 (7.6) | .879 |
| Age of Depression Onset | 44.3 (24.6) | 57.8 (21.3) | .005 |
| Charlson Comorbidity Index | 2.5 (1.8) | 2.1 (1.8) | .309 |
| Mini-Mental State Examination | 28.8 (1.2) | 27.8 (1.7) | .001 |
| HVLT+ Learning Trials | 23.1 (5.6) | 21.1 (4.8) | .445 |
| HVLT Recall | 7.8 (3.1) | 8.3 (6.2) | .371 |
| NEO-N++ | 14.4 (5.2) | 14.9 (5.4) | .719 |
Chi-squared test (1 degree of freedom)
Hamilton Depression Rating Scale-24 items
World Health Organization Disability Assessment Schedule II
Hopkins Verbal Learning Test
Neuroticism-Extroversion-Openness Personality Inventory (NEO), Neuroticism Domain
The efficacy of Engage (N=39) was compared to that of with a historical comparison group treated with PST (N=97) over 9 weeks at UCSF and Cornell.24,25 There were no demographic or clinical differences at baseline between the two study sites. At entry, Engage participants had lower severity of depression and less cognitive impairment than PST participants (Table 1). Approximately 26% of Engage participants and 27% of PST participants were taking antidepressants at entry. There were no statistically significant differences in demographics, depression severity, cognitive impairment, medical burden, or disability at baseline among participants who were taking antidepressant medication and those who were not.
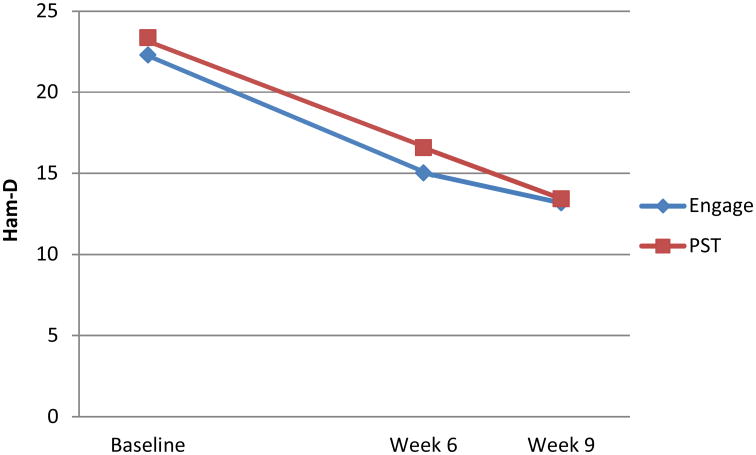
Depression Severity
A linear mixed effects model consisting of treatment (Engage N=39 vs. PST N=97), site (Cornell vs. UCSF), week (0, 6, 9), and week x treatment showed that both treatments reduced HAM-D; the effects of week was F2,254=125.72, p < 0.0001. After controlling for site (F1,254=4.73, p=0.0305), the week treatment (Engage vs. PST) interaction was not significant (F2,254=0.74, p=0.4770) suggesting that Engage and PST did not significantly differ in their depression trajectory. However, HAM-D was significantly different between the two treatment groups at baseline (PST-Engage=2.78 (95% CI: 0.52-5.05), t254=2.42, p = 0.02).
Since Engage participants (N=39) had lower baseline HAM-D than PST participants (N=97), we repeated the above analysis in Engage and PST participants with baseline HAM-D ranging from 16 to 36 (common range of Engage and PST participants), i.e. 33 Engage and 95 PST participants with statistically indistinguishable HAM-D at baseline (PST-Engage=1.1, 95% CI (-1.21, 3.37), t238 = 0.93, p=0.3537). After controlling for site (F1,238=5.66, p=0.0182), there was a significant effect of week (F2,238=120.30, p<0.0001) suggesting, as before, that both treatments reduced HAM-D significantly (Figure 1). The progression of HAM-D over time was also similar between the two group (treatment x week F2,238=0.52, p = 0.60). At week 9 (end of therapy), Engage lowered HAM-D more than PST by 0.25 HAM-D points (estimated from the mixed model was 0.25 HAM-D).This difference was not significant (t238=0.21, p=0.83), Cohen's d = 0.04 (95% CI: -0.36, 0.43). Choosing a non-inferiority margin (M) of 2.25 HAM-D points for the difference at 9 weeks, Engage was found non-inferior to PST at an alpha of 5%.
Figure 1.
24-item Hamilton Depression Rating Scale (HAM-D) Least Square Means of 33 Older Participants with Major Depression Treated with Engage and of 95 Historical Controls Treated with Problem Solving Therapy (PST).
Participants included in the Engage vs. PST comparison had HAM-D scores within the same range (16-36).
Components of Engage
All participants treated with Engage received “reward exposure”, but 35.1% of participants had reward exposure alone, 37.8% required additional interventions for negativity bias, 18.9% required additional interventions for apathy, and 8.1% required additional interventions for emotional dysregulation. Mixed effects showed no significant differences in the course of depression (HAM-D) among these four groups (F6,67 = 1.35, p = 0.25).
Remission of Depression
Remission rates (HAM-D<10) for Engage at 6 and 9 weeks (N=33) were 18.2%, and 41.1%. The corresponding figures for PST (N=95) were 13.7% and 35.0%. Logistic regression model comparing odds of remission between PST and Engage after adjusting for site showed no difference in odds at week 6 (OR = 0.67, 95% CI (0.25,1.83), Wald's χ2(1)=0.60, p = 0.44) and at week 9 (OR = 0.90, 95% CI (0.40,2.1), Wald's, χ2(1)=0.06, p = 0.81).
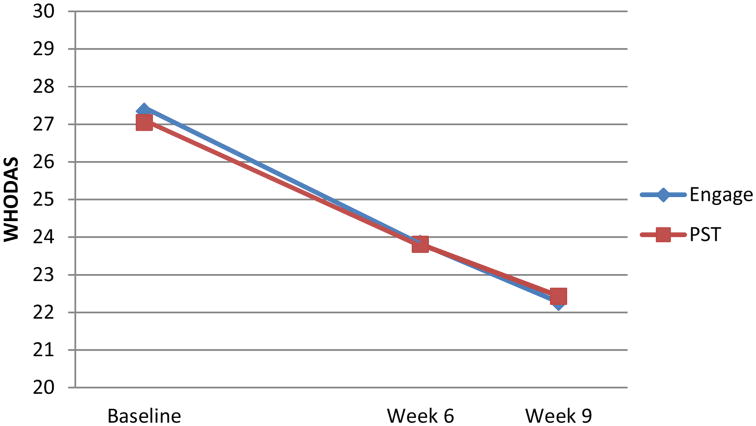
Disability
There was no significant difference in disability (WHODAS) at baseline between Engage (N=39) and PST (N=97) treated participants (Table 1). For this reason all Engage (N=39) and PST (N=97) participants were included in disability comparisons. A linear mixed effects model consisting of treatment (Engage vs. PST), site, week (0, 6, 9) and week x treatment indicated that both treatments reduced WHODAS; the effect of week was F2,234=35.73, p < 0.0001 (Figure 2). The week x treatment interaction was not significant (F2,234=0.08, p=0.9274). The difference between PST and Engage (after controlling for other variables) at week 9 was 0.16 WHODAS points (t234=0.11, p=0.9141) with a Cohen's d=0.02 (95% CI: -0.35, 0.39).
Figure 2.
World Health Organization Disability Assessment Schedule II (WHODAS) LS Means of 39 Older Participants with Major Depression Treated with Engage and of 97 Historical Controls Treated with Problem Solving Therapy (PST).
Discussion
The principal observation of this proof of concept study is that Engage has comparable efficacy to that of problem solving therapy (PST) in reducing depressive symptoms and signs, promoting remission of depression, and improving disability in late-life major depression. PST is an efficacious treatment for late-life depression based on studies showing greater reduction of depression and disability than that of supportive therapy in patients without28 and with executive dysfunction.24,25 Both community-based social workers and research therapists achieved competence in Engage and PST, but they required one third as much training time in Engage as in PST.
This is the first report of efficacy of this novel, streamlined psychotherapy. Engage's innovations consist of focus on “reward “exposure”, the structured timing and targeting of biologically-based barriers to reward exposure, and the selection and simplification of behavioral interventions aimed to increase “reward exposure” and target its “barriers”. Engage is the first psychotherapy using RDoC concepts as a guide to simplification. Accordingly, Engage targets core aspects of depression as suggested by the IOM Report: Bridging Disciplines in the Brain, Behavioral, and Clinical Sciences.33 The stepped, systematic personalization of Engage is a departure from other methods of personalized therapies (e.g., modular, preference matching) because it makes personalization part of the treatment structure itself. The focus of “Engage” on behaviors related to the positive valence systems may have implications for suicide prevention in depressed elders, a population with a high suicide risk.34
The structure of Engage, with its step-wise targeting of specific barriers to reward exposure, may serve as a template for interventions of younger adults suffering from depression or related disorders. Its stepped approach allows personalization, so that if young patients have different barriers than older adults they can be approached within the Engage framework. Studies exploring “why does Engage works” and “for whom Engage works” may guide the choice of intervention targets in patients with mental health problems other than depression. For example, if patients with emotional dysregulation only benefit from reward exposure when they use strategies to control their emotions, this observation can be introduced in therapies for patients in whom emotional dysregulation is their principal manifestation, e.g., anxiety disorders or PTSD.
The main limitations of this preliminary study are its small sample and its open treatment design. The absence of a randomized control group may have contributed to the statistical differences in overall cognitive impairment, severity of depression, and age of onset between Engage and PST participants. The 0.98 point difference of means in Mini-Mental Status Examination may not have been clinically significant. Engage is based on the theory that it reduces depression through “reward exposure”, which improves the function of the positive valence systems. However, this preliminary study lacks data on these relationships and this question will have to be tested by a subsequent randomized controlled trial (RCT). Further, the Engage and PST groups had no psychiatric comorbidity other than generalized anxiety disorder. For this reason, no conclusions can be drawn about the suitability of Engage in depressed elders with additional psychiatric diagnoses. Comparisons of participants with severity of depression (HAM-D) within the same range in both treatment arms offers information about the comparative efficacy of Engage to PST in reducing depression. However, the well-characterized historical comparison group receiving PST was part of another RCT24,25 unrelated to Engage. Therefore, they can only serve as a point of reference for evaluating the efficacy of Engage in reducing depression and disability. For this reason, this paper should be viewed as a “proof of concept” study of the efficacy of Engage that needs to be tested by an RCT.
Arguably, Engage has potential for implementation in the community. Although we used neurobiological concepts to identify its behavioral targets, its interventions are simplified to match the skill set of social workers offering mental health services in the community. Moreover, the streamlined, stepped structure of Engage offers explicit guidance on the selection and timing of its interventions. The six community-based social workers were certified in Engage after training for an average of 6.92 hours (SD: 2.40). Although further study is required, this preliminary observation suggests that community therapists may be able to administer Engage after short training.
Community implementation of a treatment is a complex process requiring buy-in and organizational changes. Classical35 and recent models36 of innovation diffusion indicate that key attributes of interventions affecting implementation are effectiveness, reimbursement by the current system, client acceptability, simplicity (ease of use by clinicians), cost (time to learn and routinize), compatibility with routine care, observability (observable use and outcomes), and trialability (can be tested in an organization and dropped at low cost). Engage was designed after long interactions and input by community clinicians with the goal of meeting criteria for simplicity, cost, compatibility with routine care, and trialability. It was designed to meet the time constraints of community therapy (nine 40-min sessions) and operationalized for “ease of use” in training and supervision time. If its efficacy is confirmed, it may be used in the large number of depressed older patients who rarely have access to structured psychotherapy.
Acknowledgments
Source of Funding: This paper was supported by P30 MH085943 (Alexopoulos), R01 MH064099 (Alexopoulos), K24 MH074717 (Arean), R01 MH075900 (Arean) and the Sanchez Foundation. Dr. Alexopoulos has served on the speakers' bureaus of Astra Zeneca, Novartis, Sunovion, and Takeda-Lundbeck.
Footnotes
Conflicts of Interest: No other authors report conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chambers DA. Advancing the science of implementation: a workshop summary. Adm Policy Ment Health. 2008 Mar;35(1-2):3–10. doi: 10.1007/s10488-007-0146-7. [DOI] [PubMed] [Google Scholar]
- 2.Goldman HH, Azrin ST. Public policy and evidence-based practice. Psychiatr Clin North Am. 2003 Dec;26(4):899–917. doi: 10.1016/s0193-953x(03)00068-6. [DOI] [PubMed] [Google Scholar]
- 3.Mellman LA, Beresin E. Psychotherapy competencies: development and implementation. Acad Psychiatry. 2003 Fall;27(3):149–153. doi: 10.1176/appi.ap.27.3.149. [DOI] [PubMed] [Google Scholar]
- 4.Alexopoulos GS, Arean P. A model for streamlining psychotherapy in the RDoC era: the example of ‘Engage’. Mol Psychiatry. 2014 Jan;19(1):14–19. doi: 10.1038/mp.2013.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. The American journal of psychiatry. 2010 Jul;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 6.Russo SJ, Nestler EJ. The brain reward circuitry in mood disorders. Nature reviews Neuroscience. 2013 Sep;14(9):609–625. doi: 10.1038/nrn3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takahashi T, Oono H, Inoue T, et al. Depressive patients are more impulsive and inconsistent in intertemporal choice behavior for monetary gain and loss than healthy subjects--an analysis based on Tsallis' statistics. Neuro endocrinology letters. 2008 Jun;29(3):351–358. [PubMed] [Google Scholar]
- 8.Kunisato Y, Okamoto Y, Ueda K, et al. Effects of depression on reward-based decision making and variability of action in probabilistic learning. Journal of behavior therapy and experimental psychiatry. 2012 Dec;43(4):1088–1094. doi: 10.1016/j.jbtep.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 9.Robinson OJ, Cools R, Carlisi CO, Sahakian BJ, Drevets WC. Ventral striatum response during reward and punishment reversal learning in unmedicated major depressive disorder. The American journal of psychiatry. 2012 Feb;169(2):152–159. doi: 10.1176/appi.ajp.2011.11010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pizzagalli DA, Holmes AJ, Dillon DG, et al. Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. The American journal of psychiatry. 2009 Jun;166(6):702–710. doi: 10.1176/appi.ajp.2008.08081201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eppinger B, Hammerer D, Li SC. Neuromodulation of reward-based learning and decision making in human aging. Annals of the New York Academy of Sciences. 2011 Oct;1235:1–17. doi: 10.1111/j.1749-6632.2011.06230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dombrovski AY, Siegle GJ, Szanto K, Clark L, Reynolds CF, Aizenstein H. The temptation of suicide: striatal gray matter, discounting of delayed rewards, and suicide attempts in late-life depression. Psychological medicine. 2012 Jun;42(6):1203–1215. doi: 10.1017/S0033291711002133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beck AT. The evolution of the cognitive model of depression and its neurobiological correlates. The American journal of psychiatry. 2008 Aug;165(8):969–977. doi: 10.1176/appi.ajp.2008.08050721. [DOI] [PubMed] [Google Scholar]
- 14.Williams LM, Gatt JM, Schofield PR, Olivieri G, Peduto A, Gordon E. ‘Negativity bias’ in risk for depression and anxiety: brain-body fear circuitry correlates, 5-HTT-LPR and early life stress. NeuroImage. 2009 Sep;47(3):804–814. doi: 10.1016/j.neuroimage.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Munafo MR, Brown SM, Hariri AR. Serotonin transporter (5-HTTLPR) genotype and amygdala activation: a meta-analysis. Biological psychiatry. 2008 May 1;63(9):852–857. doi: 10.1016/j.biopsych.2007.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Monk CS, Klein RG, Telzer EH, et al. Amygdala and nucleus accumbens activation to emotional facial expressions in children and adolescents at risk for major depression. The American journal of psychiatry. 2008 Jan;165(1):90–98. doi: 10.1176/appi.ajp.2007.06111917. [DOI] [PubMed] [Google Scholar]
- 17.Bonelli RM, Cummings JL. Frontal-subcortical circuitry and behavior. Dialogues in clinical neuroscience. 2007;9(2):141–151. doi: 10.31887/DCNS.2007.9.2/rbonelli. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexopoulos GS, Hoptman MJ, Yuen G, et al. Functional connectivity in apathy of late-life depression: A preliminary study. Journal of affective disorders. 2013 Jul;149(1-3):398–405. doi: 10.1016/j.jad.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Etkin A, Egner T, Kalisch R. Emotional processing in anterior cingulate and medial prefrontal cortex. Trends in cognitive sciences. 2011 Feb;15(2):85–93. doi: 10.1016/j.tics.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maier S, Szalkowski A, Kamphausen S, et al. Clarifying the Role of the Rostral dmPFC/dACC in Fear/Anxiety: Learning, Appraisal or Expression? PloS one. 2012;7(11):e50120. doi: 10.1371/journal.pone.0050120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mather M. The emotion paradox in the aging brain. Annals of the New York Academy of Sciences. 2012 Mar;1251:33–49. doi: 10.1111/j.1749-6632.2012.06471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roalf DR, Pruis TA, Stevens AA, Janowsky JS. More is less: emotion induced prefrontal cortex activity habituates in aging. Neurobiology of aging. 2011 Sep;32(9):1634–1650. doi: 10.1016/j.neurobiolaging.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williams LM, Brown KJ, Palmer D, et al. The mellow years?: neural basis of improving emotional stability over age. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2006 Jun 14;26(24):6422–6430. doi: 10.1523/JNEUROSCI.0022-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alexopoulos GS, Raue PJ, Kiosses DN, et al. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction: effect on disability. Archives of general psychiatry. 2011 Jan;68(1):33–41. doi: 10.1001/archgenpsychiatry.2010.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arean PA, Raue P, Mackin RS, Kanellopoulos D, McCulloch C, Alexopoulos GS. Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction. The American journal of psychiatry. 2010 Nov;167(11):1391–1398. doi: 10.1176/appi.ajp.2010.09091327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.First MB, Spitzer RL, Williams JBW, Gibbon M. Structured clinical interview for DSM-IV - patient version (SCID-P) Washington: American Psychiatric Press; 1995. [Google Scholar]
- 27.Alexopoulos GS, Raue P, Arean P. Problem-solving therapy versus supportive therapy in geriatric major depression with executive dysfunction. Am J Geriatr Psychiatry. 2003 Jan-Feb;11(1):46–52. [PubMed] [Google Scholar]
- 28.Arean PA, Perri MG, Nezu AM, Schein RL, Christopher F, Joseph TX. Comparative effectiveness of social problem-solving therapy and reminiscence therapy as treatments for depression in older adults. J Consult Clin Psychol. 1993 Dec;61(6):1003–1010. doi: 10.1037//0022-006x.61.6.1003. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton M. A rating scale for depression. Journal of neurology, neurosurgery, and psychiatry. 1960 Feb;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Epping-Jordan JA, Ustun TB. The WHODAS-II: leveling the playing field for all disorders. WHO Mental Health Bulletin. 2000;6:5–6. [Google Scholar]
- 31.Costa PT, McCrae RR. NEO PI-R Professional Manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 32.Laird N, Ware J. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 33.Institute of Medicine. Bridging Disciplines in the Brain, Behavioral, and Clinical Sciences. Washington, DC: Academies Press; 2000. [PubMed] [Google Scholar]
- 34.Arean P, Hegel M, Vannoy S, Fan MY, Unuzter J. Effectiveness of problem-solving therapy for older, primary care patients with depression: results from the IMPACT project. Gerontologist. 2008 Jun;48(3):311–323. doi: 10.1093/geront/48.3.311. [DOI] [PubMed] [Google Scholar]
- 35.Rogers E. Diffusion of Innovation. 4th. New York: Free Press; 1995. [Google Scholar]
- 36.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]