Abstract
OBJECTIVE
This study compares different non-pharmacological interventions for persons with behavioral symptoms and dementia on frequency of use and perceived efficacy in terms of change in behavior and interest.
METHODS
Participants were 89 nursing home residents from 6 Maryland nursing homes with a mean age of 85.9 years (SD=8.6). Research assistants presented interventions tailored to the participants` needs and preferences in a pre-intervention trial phase and in an intervention phase. The impact of each intervention on behavioral symptoms and on the person’s interest was rated immediately after the intervention by a research assistant.
RESULTS
The most utilized interventions in both trial and treatment phases were the social intervention of one-on-one interaction, simulated social interventions such as a lifelike doll and respite video, the theme intervention of magazine, and the sensory stimulation intervention of music. In contrast, the least utilized interventions in both phases were sewing, fabric book, and flower arrangement. Interventions with the highest impact on behavioral symptoms included one-on one social interaction, hand massage, music, video, care, and folding towels. Other high impact interventions included walking, going outside, flower arranging, food or drink, sewing, group activity, book presentation ball toss, coloring or painting, walking, and family video.
CONCLUSIONS
The results provide initial directions for choosing specific interventions for persons with dementia and also demonstrate a methodology for increasing knowledge through ongoing monitoring of practice.
Keywords: Dementia, Behavioral Symptoms, Nonpharmacological Interventions
OBJECTIVE
Behavioral symptoms in persons with dementia increase suffering of the person with dementia as well as caregivers’ burden, increase utilization of restrictive care, and are addressed by both pharmacological (1, 2) and non-pharmacological treatments (3). These behaviors have been labeled problem behaviors, disruptive behaviors, disturbing behaviors, and agitation. While several theoretical models exist for explaining behavioral symptoms in persons with dementia(4) we focus on the Unmet Needs Model.(4) According to this model, behavioral symptoms arise because of one's decreased ability to meet individual's needs and caregivers’ insufficient acknowledgment of needs that may pertain to pain/health/physical discomfort, mental discomfort (evident in affective states: depression, anxiety, frustration, boredom), the need for social contacts (loneliness), uncomfortable environmental conditions, or an inadequate level of stimulation (too low, too high, inappropriate).
Previous studies have demonstrated the efficacy of nonpharmacological interventions responding to these needs.(5) However, few compared the impact of different interventions on behavioral symptoms. In a study that compared person centered showering, the towel bath, and usual care,(6) both interventions significantly decreased behavioral symptoms and aggression, but usual caretaking did not. Snoezelen and reminiscence interventions each showed inconclusive effects on behavioral symptoms in a sample of 20 participants with dementia,(7) and activity of daily living intervention and a psychosocial interventions did not reduce behavioral symptoms.(8) In a comparison of validation therapy (VT), social contact (SC), and usual care (UC),(9) VT showed a significant reduction in physical aggressive behaviors, and both VT and SC participants demonstrated significant reductions in verbally aggressive behaviors based on nursing staff ratings. Nonparticipant observers, however, rated verbal aggression as reduced for those participating in SC but not VT and UC.(9) Finally, a comparison of one-on-one social contact, videotapes of family members, and music with usual care interventions revealed that while all interventions were more effective than usual care in reducing verbal agitation; one-on-one social contact intervention was the most effective.(10)
We found no studies comparing individually-tailored interventions that address unmet needs and cognitive and sensory limitations of persons with dementia. Therefore, this study focuses on these questions:
In the process of tailoring interventions to persons with dementia who manifest behavioral symptoms, which interventions are most often used? Who receives which intervention? What is the perceived efficacy of these interventions?
When the participants receive more than one intervention, which is related to greater perceived improvements in behavioral symptoms?
- Does the use of a trial phase improve results in the treatment phase? The hypotheses are:
- The rate of refusals will be lower in the treatment phase than in the trial phase.
- The level of success will be higher in the treatment phase than in the trial phase.
METHODS
We conducted this research as a part of a larger study on nonpharmacological interventions for behavior problems in persons with dementia.(5)
Participants and procedure
We approached 23 Maryland nursing homes located at reasonable distances (around 40 minutes drive) from the researchers` offices in Rockville, Maryland. Seven facilities refused to participate at that point in time; seven other facilities could not provide sufficient eligible participants or did not finalize the agreement by the time data collection was completed; and in two other facilities only control condition participants were enrolled (not reported in this paper). Altogether, a total of 654 eligible participants were approached for consent. Informed consent was provided by the participant, the attorney in fact, or the closest family member(11). For 231 of the residents, consent was received. Subsequently, a group of 155 residents was randomly selected to receive intervention, while the others served as control group (not reported in this paper, but described in (5)). From the participants selected for intervention, 93 met inclusion criteria. Inclusion criteria were: resident lived at the NH ≥ three weeks; nursing staff identified the resident as manifesting behavioral symptoms at least several times a day; age ≥ 60 years; diagnosis of dementia. Exclusion criteria were: life expectancy < 3 months; bipolar, schizophrenia, or mental retardation diagnosis; expected to leave the NH within 4 months; and a score on the Mini Mental Status Examination (MMSE) ≥ 25 (for more information see assessments). From the 93 participants, 4 did not receive intervention as allocated because of death. The study was conducted from June 2006 until December 2011; data collection ended in June 2011. The participants` mean age was 85.9 years (SD=8.6), 73% were female, 81% were white, 61% were widowed, and 42.7% had a college, technical school, or graduate degree. IRB approved the study protocol.
Assessments
Background data
We collected demographic data from residents` charts. Via the Minimum Data Set (MDS)(12), summing 10 items (e.g., dressing, eating), we obtained scores concerning performance of activities of daily living (ADL). Medical records provided us information on prescribed medications.
Cognitive functioning
Dementia diagnosis was taken from the chart and confirmed by a physician or nurse practitioner. The Mini-Mental Status Examination (MMSE)(13) assessed cognitive status. MMSE scores range from 0 (severe cognitive impairment) to 30 (normal cognitive functioning). Research assistants who were trained in standardized administration and scoring procedures administered the MMSE.
Outcome measure
The Change Assessment Rating (CAR) was developed for this study and included 2 items concerning global improvement. The first item tapped behavioral symptoms change (i.e., “Did the intervention change agitation?” with agitation defined as in Cohen-Mansfield and Billig (14), and including all behaviors on the Agitation Behavior Mapping Instrument (15)). The second item tapped interest change (i.e., “Did the intervention change interest?”) with interest including all behaviors of the interest scale of the Lawton`s Modified Behavior Stream (16) as perceived by the research assistant providing the intervention. Research assistants rated the items on a 5-point scale (worse, somewhat worse, same, somewhat better, better). The CAR is comparable with other global improvement measures such as the Clinical Global Impressions (CGI) scale (17). This latter measure has good validity properties (e.g., (18, 19)). The correlation between the 2 CAR items was r=.73, p<.001 for 822 administrations in the trial phase and r=.78, p<.001 for 2428 administrations in the treatment phase.
Design
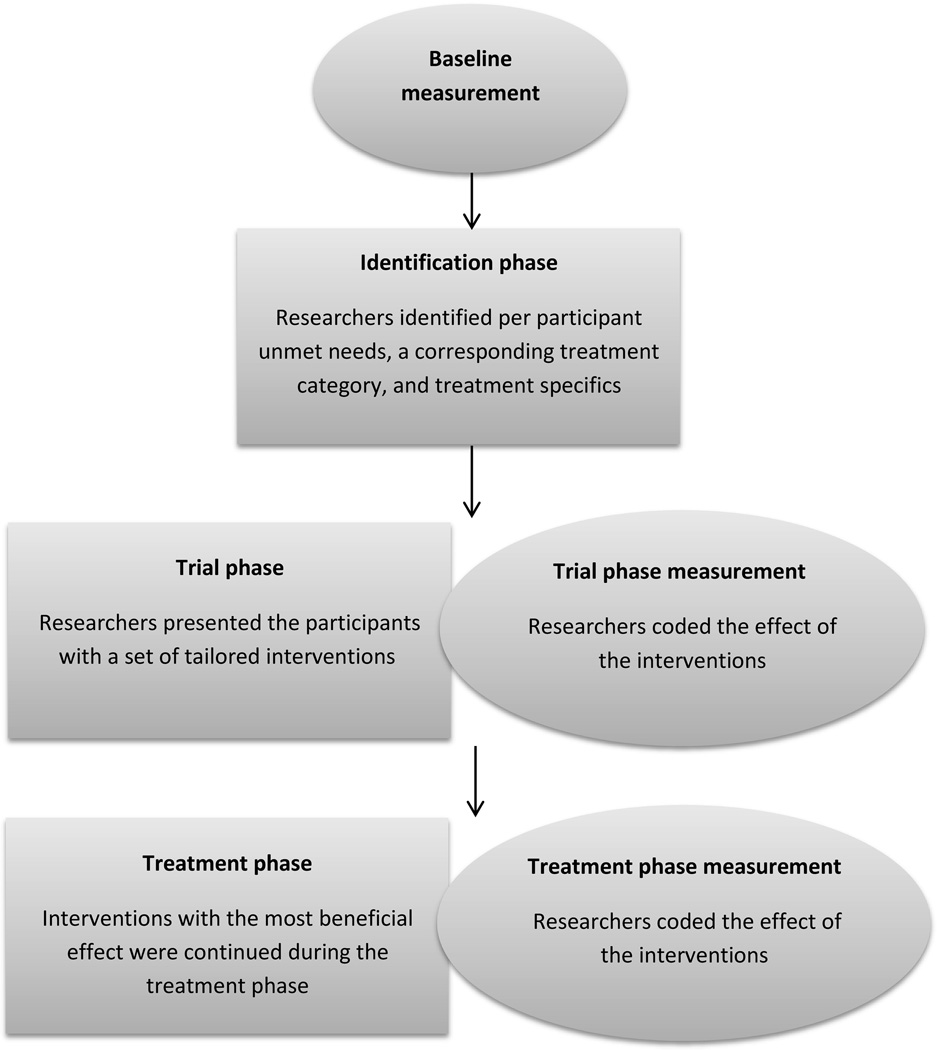
The study includes comparisons of perceived efficacy of different nonnpharmacological interventions. Two phases are included, namely trial phase and treatment phase. The design is presented in figure 1 and described in the following.
Figure 1.
Study design
Baseline measurement
After background data were obtained, a trained research assistant recorded baseline observations of behavioral symptoms and affect onto a Palm Pilot Zire31™ handheld computer (PalmOne, Inc., Milpitas, CA) via the Agitation Behavior Mapping Instrument (ABMI) (15, 20). Each participant was observed for 3 consecutive days, every half hour between 8 AM and 9 PM. Each observation lasted 3 minutes. Research assistants observed 3–5 residents per half hour, 1 resident at the time. Per resident, we recorded the mean of 69 baseline observations, and identified a 4-hour agitation peak period.
Relatives completed a questionnaire concerning participants’ medical history, self-identity, and social functioning. The treating physician completed a short form confirming the participant’s dementia diagnosis and identifying the presence of akathesia, delirium, pain, and/or depression.
Identification phase
For each intervention group participant, the Treatment Routes for Exploring Agitation (TREA) decision tree protocol (5, 21) was followed. The TREA protocol is based on a theoretical framework of unmet needs and stresses the importance of individualizing non-pharmacologic interventions to address the unmet needs of agitated persons (22). The assumption driving this theoretical framework is that interventions should be individualized according to agitation etiology, remaining abilities, level of cognitive functioning, and past/present interests. Specifically, research-assistants first collected data on the agitated person`s needs and preferences from formal caregivers (i.e., nursing home staff, physicians), informal caregivers (relatives), and direct observations. Second, the collected information was applied to systematic algorithms (i.e., decision trees) to suggest personalized interventions for lowering agitation. Examples of the decision tree contents can be found in Cohen-Mansfield (22).
Trial phase
Over the three weeks prior to the actual treatment phase, research assistants tested for each participant the specific treatments selected in the identification phase. Research assistants recorded the impact of each discrete trial, using the CAR.
Treatment phase
Activities with the most beneficial effect during the trials were subsequently used in the 2-week treatment phase. A research assistant provided interventions during 4 hours a day, those hours which had been identified at baseline as having the highest levels of behavioral symptoms for that individual. The interventions were delivered for 5 working days a week for two weeks. The amount and duration of interventions depended on various parameters, such as how long the participant was engaged with each intervention and how much of the time the participant was awake and available. Again, research assistants rated the impact of each discrete intervention using the CAR.
Interventions
Twenty four interventions were used, divided into 9 categories (Tables 1 and 2). The categories included care (activities concerning residents comfort, such as taking person to bathroom or bringing a blanket), theme (reading or video materials), manipulative (activities that require moving objects such as puzzle or toss ball), sensory stimulation (hand massage, provision of a fabric book, and music) movement activities (walking and going outside), artistic activities, and work-like activities. The simulated social category included videos of family members talking to the participant, life-like baby doll, a robotic animal, and a respite video, i.e., a commercially available generic video of someone talking to the participant or singing to and with him/her. The social category included group activities on the unit or in the nursing home and one-on-one interaction with the research assistant. In this paper we do not analyze interventions administered at lower frequencies, such as provision of family pictures, stuffed animals, or aromatherapy.
Table 1.
Utilization and Impact of Different Interventions in the Trial Phase
| Intervention | # of sessions |
# persons |
Proportion refused sessions |
Impact on behavioral symptoms1 |
Interest with interventiona |
Male % |
MMSE2 | ||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) by | Mean (SD) by | ||||||||
| Session | Person | Session | Person | ||||||
| Care | |||||||||
| Care | 158 | 71 | 0.01 | 4.29(0.86) | 4.36(0.73) | 4.29(0.84) | 4.41(0.74) | 17 | 10.12(7.10) |
| Food or drink | 16 | 14 | 0.06 | 4.40(0.70) | 4.44(0.73) | 4.55(0.69) | 4.55(0.69) | 00 | 9.21(5.47) |
| Theme | |||||||||
| Book | 19 | 16 | 0.00 | 4.11(0.93) | 4.06(0.94) | 4.21(0.89) | 4.29(0.75) | 17 | 10.36(7.31) |
| Magazine | 112 | 80 | 0.20 | 3.81(0.78) | 3.83(0.75) | 3.94(0.90) | 3.89(0.86) | 30 | 7.18(6.13) |
| Video | 69 | 47 | 0.03 | 3.76(0.76) | 3.89(0.72) | 3.84(0.84) | 3.92(0.83) | 40 | 5.98(5.88) |
| Manipulative | |||||||||
| Ball Toss (balloon, tetherball) |
48 | 40 | 0.19 | 3.82(1.14) | 3.93(1.03) | 4.03(1.07) | 4.13(0.93) | 43 | 8.07(7.04) |
| Puzzle | 61 | 54 | 0.05 | 3.42(0.98) | 3.45(0.93) | 3.43(0.89) | 3.43(0.89) | 27 | 6.77(6.24) |
| Squeeze Ball | 56 | 53 | 0.14 | 3.81(0.82) | 3.83(0.82) | 3.73(0.74) | 3.79(0.73) | 30 | 6.14(5.40) |
| Artisitic | |||||||||
| Coloring/painting | 83 | 68 | 0.19 | 3.84(1.05) | 3.86(1.06) | 3.96(1.07) | 3.95(1.06) | 23 | 7.25(6.36) |
| Sewing | 9 | 15 | 0.12 | 4.38(0.92) | 4.38(0.92) | 4.64(0.67) | 4.64(0.67) | 09 | 7.45(5.84) |
| Flower Arranging |
12 | 10 | 0.17 | 4.50(1.00) | 4.50(1.00) | 4.44(0.88) | 4.44(0.88) | 22 | 3.33(3.61) |
| Work-like | |||||||||
| Sorting | 30 | 27 | 0.10 | 3.56(0.73) | 3.57(0.73) | 3.92(0.93) | 3.92(0.93) | 46 | 10.65(6.66) |
| Folding Towels | 56 | 48 | 0.11 | 4.00(0.81) | 4.03(0.81) | 4.13(0.94) | 4.15(0.92) | 17 | 6.32(5.92) |
| Movement | |||||||||
| Walk | 17 | 15 | 0.06 | 4.88(0.35) | 4.88(0.35) | 4.60(0.70) | 4.60(0.70) | 60 | 3.19(2.24) |
| Outside | 33 | 29 | 0.18 | 4.73(0.46) | 4.71(0.47) | 4.50(0.79) | 4.47(0.80) | 35 | 7.24(6.33) |
| Simulated social | |||||||||
| Family Video | 65 | 59 | 0.05 | 3.96(1.24) | 4.00(1.24) | 4.24(1.15) | 4.27(1.14) | 32 | 9.13(6.97) |
| Real Looking Doll |
99 | 83 | 0.16 | 3.92(0.91) | 3.96(0.92) | 4.22(0.91) | 4.26(0.90) | 25 | 7.14(6.34) |
| Robotic Animal | 111 | 84 | 0.19 | 3.74(0.95) | 3.75(0.94) | 3.96(0.98) | 4.02(0.90) | 30 | 7.43(6.32) |
| Respite Video | 99 | 88 | 0.09 | 4.02(0.85) | 4.02(0.84) | 4.02(0.95) | 4.04(0.96) | 30 | 7.15(6.35) |
| Social | |||||||||
| Group activity | 56 | 45 | 0.16 | 4.13(0.90) | 4.09(0.90) | 4.53(0.79) | 4.47(0.82) | 23 | 10.12(5.92) |
| One-on-one interaction |
101 | 80 | 0.06 | 4.09(0.79) | 4.13(0.72) | 4.35(0.76) | 4.40(0.67) | 26 | 7.82(6.38) |
|
Sensory stimulation |
|||||||||
| Hand massage | 36 | 33 | 0.06 | 4.30(0.76) | 4.32(0.72) | 4.58(0.86) | 4.64(0.57) | 32 | 2.31(3.07) |
| Fabric Book | 9 | 7 | 0.11 | 3.40(0.89) | 3.50(1.00) | 3.80(0.84) | 3.80(0.84) | 20 | 2.56(3.96) |
| Music | 97 | 76 | 0.11 | 4.14(0.74) | 4.14(0.73) | 4.16(0.76) | 4.20(0.72) | 26 | 7.02(6.00) |
Scale: 1=worse to 5=better
Scale: 0=severe cognitive impairment to 30=normal cognitive functioning
Table 2.
Utilization and Impact of Different Interventions in the Treatment Phase
| Intervention | # of sessions |
# of persons |
proportion refused sessions |
Impact on behavioral symptoms3 |
Interest with interventiona |
% Male |
MMSE4 | ||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) by | Mean (SD) by | ||||||||
| Session | Person | Session | Person | ||||||
| Care | |||||||||
| Care | 65 | 25 | 0.00 | 4.69(0.86) | 4.66(0.92) | 4.62(0.68) | 4.55(0.65) | 19 | 7.81(5.91) |
| Food or drink | 54 | 19 | 0.02 | 4.37(0.92) | 4.41(0.81) | 4.47(0.79) | 4.52(0.66) | 11 | 9.50(7.64) |
| Theme | |||||||||
| Book | 42 | 7 | 0.05 | 4.54(0.79) | 4.03(1.37) | 4.48(0.64) | 4.30(0.65) | 14 | 8.43(6.73) |
| Magazine | 376 | 62 | 0.04 | 4.11(0.79) | 3.95(0.64) | 4.15(0.78) | 3.98(0.64) | 31 | 8.05(6.32) |
| Video | 191 | 49 | 0.02 | 4.00(0.76) | 3.94(0.61) | 3.95(0.82) | 3.87(0.64) | 31 | 7.71(6.78) |
| Manipulative | |||||||||
| Ball toss | 55 | 21 | 0.07 | 4.63(0.66) | 4.41(0.85) | 4.63(0.66) | 4.56(0.63) | 55 | 8.69(7.22) |
| Puzzle | 80 | 21 | 0.15 | 4.02(0.85) | 3.81(0.71) | 4.13(0.86) | 3.84(0.73) | 37 | 7.35(8.10) |
| Squeeze ball | 57 | 28 | 0.07 | 3.89(0.93) | 3.84(0.85) | 3.86(0.80) | 3.78(0.75) | 41 | 6.34(5.43) |
| Artisitic | |||||||||
| Coloring/painting | 92 | 32 | 0.18 | 4.45(0.76) | 4.39(0.67) | 4.47(0.74) | 4.27(0.65) | 19 | 6.94(6.59) |
| Sewing | 21 | 6 | 0.14 | 4.36(0.93) | 4.33(0.77) | 4.39(0.92) | 4.45(0.63) | 0 | 6.80(6.65) |
| Flower arranging | 38 | 11 | 0.05 | 4.32(0.77) | 4.14(0.84) | 4.34(0.73) | 4.36(0.67) | 9 | 3.86(3.51) |
| Work-like | |||||||||
| Sorting | 54 | 20 | 0.04 | 4.35(0.86) | 4.17(0.86) | 4.37(0.80) | 4.15(0.72) | 35 | 9.75(5.31) |
| Folding towels | 135 | 40 | 0.06 | 4.39(0.78) | 4.33(0.57) | 4.40(0.77) | 4.36(0.48) | 13 | 7.61(6.22) |
| Movement | |||||||||
| Walk | 59 | 22 | 0.10 | 4.38(0.81) | 4.38(0.74) | 4.49(0.74) | 4.47(0.62) | 33 | 6.30(6.16) |
| Outside | 18 | 13 | 0.06 | 4.43(0.85) | 4.41(0.80) | 4.76(0.56) | 4.74(0.60) | 31 | 6.69(6.05) |
| Simulated social | |||||||||
| Family video | 97 | 28 | 0.03 | 4.26(0.88) | 4.23(0.76) | 4.35(0.86) | 4.29(0.72) | 29 | 7.92(7.16) |
| Real looking doll | 369 | 64 | 0.07 | 4.12(0.83) | 4.12(0.68) | 4.25(0.78) | 4.23(0.60) | 20 | 6.47(5.55) |
| Robotic animal | 190 | 50 | 0.12 | 3.84(0.93) | 3.76(0.87) | 3.94(0.86) | 3.89(0.69) | 29 | 6.19(5.82) |
| Respite video | 209 | 58 | 0.04 | 3.80(0.81) | 3.81(0.63) | 4.00(0.81) | 3.98(0.60) | 30 | 7.29(5.91) |
| Social | |||||||||
| Group activity | 57 | 19 | 0.05 | 4.14(1.25) | 4.09(1.20) | 4.29(1.04) | 4.23(1.01) | 17 | 11.17(6.76) |
| One-on-one interaction |
547 | 77 | 0.02 | 4.07(0.80) | 4.11(0.59) | 4.26(0.76) | 4.29(0.47) | 25 | 8.05(6.28) |
|
Sensory stimulation |
|||||||||
| Hand massage | 50 | 17 | 0.08 | 4.18(0.84) | 4.13(0.71) | 4.10(0.86) | 4.02(0.78) | 35 | 3.74(5.46) |
| Fabric book | 37 | 10 | 0.08 | 3.88(0.91) | 3.75(0.78) | 3.94(0.89) | 4.19(0.80) | 33 | 4.35(4.72) |
| Music | 335 | 51 | 0.01 | 3.74(0.75) | 3.85(0.52) | 3.76(0.76) | 3.81(0.55) | 28 | 7.36(6.87) |
Scale: 1=worse to 5=better
Scale: 0=severe cognitive impairment to 30=normal cognitive functioning
Scale: 1=worse to 5=better
Scale: 0=severe cognitive impairment to 30=normal cognitive functioning
Statistical analysis
We performed all analyses separately for the trial and treatment phase. We included data for interventions used for at least 10 persons. For each intervention, we calculated the percent of sessions in which participants refused the intervention and the mean CAR for behavioral symptoms and for interest both for all sessions in which we used the intervention, and as an average of all the persons who received the intervention. In the latter analysis, the score for each participant was the average of all the sessions in which the participant received the intervention. We also calculated the mean MMSE score and the gender distribution of participants who received each intervention.
Comparing the trial phase to the treatment phase, we compared intervention refusal rates in the trial phase to that of the treatment phase using the Wilcoxon Signed Rank Test. Similarly, we conducted paired t-tests comparing the CAR ratings of each intervention in the trial phase to those in the treatment phase, using the mean of the CAR ratings per intervention separately.
Subsequently, we compared the efficacy of interventions for behavioral symptoms. We included only pairs of interventions that were presented to at least 10 participants, and conducted paired comparisons of the CAR. We reported comparisons for interventions that were significantly associated with at least two other interventions (at .05 two tailed level, and in the same direction).
RESULTS
The mean MMSE score was 7.6 (SD=6.3), and the mean ADL functional difficulties index 2.7 (SD=0.8). Participants received on average 8.8 (SD=2.1) medications.
Trial phase – utilization, impact, and associations with background characteristics
Table 1 presents trial phase interventions` utilization and their perceived impact by session and by person. The main findings by person are presented next.
Utilization
The most common interventions were respite video, followed by robotic animal, one-on-one interaction, real looking doll, magazine, and music. The least common interventions were fabric book, flower arranging, walking, food or drink, and sewing.
Impact on behavioral symptoms
On average, the level of impact on behavioral symptoms was highest for interventions involving walking, going outside, flower arranging, food or drink, sewing, care, hand massage, music, one-on-one interaction, group activity and book presentation. On average, impact on behavioral symptoms was the lowest, although still positive, for puzzle, fabric book, and sorting.
Impact on interest
Participants, on average, were most interested in sewing and hand massage, walk, food and drink, going outside, and group activity. On average, interest was lowest for puzzle, squeeze ball, fabric book, magazine, and sorting.
Relationship with gender
Walking, sorting, and ball toss interventions, were predominantly used with men, whereas provision of food or drink and sewing were predominantly with women.
Relationship with cognitive function
Interventions used with participants with the highest levels of cognitive functioning (note, the highest average is 10.65 on a scale of 0–30, with 26–30 indicating normal functioning) were: sorting, book, care, group activity, and food and drink. Interventions used with participants with the lowest levels of cognitive functioning were: hand massage, fabric book, walk, and flower arranging.
Treatment phase – utilization, impact, and associations with background characteristics
Table 2 presents intervention utilization and perceived impact in the treatment phase. We summarize the main results by person below.
Utilization
The most highly utilized interventions were (by order of number of persons with whom intervention was tried): one-on-one interaction, real looking doll, magazine, respite video, and music. The least often used were: sewing, book, fabric book, flower arranging, and going outside.
Impact on behavioral symptoms
The most highly rated interventions were: care, ball toss, food or drink, going outside, coloring or painting, walking, folding towels, sewing, and family video. Other interventions with a relatively high rating were sorting, flower arranging, hand massage, real looking doll, one-on-one interaction, group activity, and book. Ratings were lowest for fabric book and robotic animal interventions.
Impact on interest
The most highly rated interventions were: going outside, ball toss, care, food or drink, walk, sewing, folding towels, flower arranging, book, family video, one-on-one interaction, coloring/painting, real looking doll, and group activity. Squeeze ball and music had the lowest average impact.
Relationship with gender
Ball toss, squeeze ball, and puzzle had the highest utilization rate with males, whereas sewing and flower arranging had the highest rates of female participants.
Relationship with cognitive function
Interventions whose participants had the highest level of cognitive functioning were: group activity, sorting, food or drink, ball toss, book, and magazine. Those receiving hand massage, flower arranging, and fabric book had the lowest level of cognitive functioning.
Refusal rates
Refusal rates were highest for magazine, ball toss, coloring/painting, robotic animal and going outside in the trial phase and for coloring/painting, puzzle, sewing, robotic animal, and walking in the treatment phase (Tables 1 and 2).
Comparison of trial phase and treatment phase
Refusal rates during the trial phase (mean=0.108, SD=0.061) were significantly higher than the rates during the treatment phase (mean=0.065, SD=0.0457), related samples Wilcoxon Signed Rank Test p=.003, two tailed.
We compared the mean CAR ratings for each treatment during the trial phase to ratings during the treatment phase, for mean ratings by session and by person and for behavioral symptoms and for interest. Mean CAR ratings were consistently higher in the treatment phase than in the trial phase. However, the difference was statistically significant only for mean ratings by session for behavioral symptoms: 4.21 (SD=0.27) during treatment as compared to 4.04 (SD=0.37) for the trial phase, t(23)=1.78, p=.044, one tailed.
Comparison of interventions
Trial phase
For the majority of comparisons, either the sample size was too small (i.e., < 10 participants) or there were no significant differences between interventions. We therefore report only those interventions that were either superior or inferior to others in more than one comparison. Interventions superior to others included one-on-one interaction, music, and hand massage. Specifically, one-on-one interaction was significantly more effective than sorting (t(12)=2.94; p=.012), robotic animal (t(41)=2.28; p=.028), magazine (t(37)=1.99; p=.054), and puzzle (t(33)=2.71; p=.011). Music was more effective than sorting (t(11)=3.56 ; p=.004), robotic animal (t(38)=2.78; p=.008), squeeze ball (t(25)=2.06; p=.050), and puzzle (t(31)=4.30; p<.001). Hand massage was more effective than magazine (t(12)=−3.63; p=.003), real looking doll (t(16)=−2.61; p=.019), coloring\painting (t(10)=−3.19; p=.010), and folding towels (t(10)=-2.28 ; p=.05). Interventions which were inferior to others were puzzle and robotic animal. Specifically, puzzle was inferior to one-on-one interaction (t(33)=2.71 ; p=.011), music (t(31)=4.30; p<.001), video (t(16)=2.49 ; p=.024), respite video (t(32)=4.71 ; p<.001), and real looking doll (t(31)=2.79; p=.009). Robotic animal was inferior to one-on-one interaction (t(41)=2.28; p=.028) and music (t(38)=2.28; p=.008).
Treatment phase
As in the case with the trial phase, most comparisons that either did not have a sufficient number of participants or were not significant, were not reported. More effective interventions included one-on-one interaction, hand massage, topic video, care, and folding towels. One-on-one interaction was superior to robotic animal (t(28)=2.40; p=.022), respite video (t(44)=2.73; p=.009), and squeeze ball (t(18)=2.91; p=.009). Hand massage was superior to one-on-one interaction (t(11)=−2.49; p=.030) and respite video (t(10)=−3.36; p=.009). Topic video was superior to puzzle (t(10)=2.21; p=.051) and squeeze ball (t(11)=3.38; p=.006). Care was superior to one-on-one interaction (t(16)=−3.76; p=.002) and robotic animal (t(10)=-3.00; p=.013). Folding towels was superior to one-on-one interaction (t(32)=−2.01; p=.053), robotic animal (t(18)=−2.38; p=.028), respite video (t(22)=−2.70; p=.013), and music (t(13)=2.81; p=.015). Less effective interventions were robotic animal, respite video, and squeeze ball. Robotic animal was inferior to one-on-one interaction (t(38)=2.40;p=.022), real looking doll (t(34)=−3.15; p=.003), folding towels (t(18)=−2.38; p=.028), music (t(20)=−2.45; p=.024), and care (t(10)=−3.00; p=.013); respite video was inferior to family video (t(16)=−3.96; p=.001), folding towels (t(22)=−2.70; p=.013), hand massage (t(10)=−3.36; p=.007), and walking (t(15)=−4.55; p<.001); squeeze ball was inferior to topic video (t(11)=3.38; p=.006) and one-on-one interaction (t(18)=2.91; p=.009).
CONCLUSIONS
This is the first study to systematically examine the immediate impact of tailored interventions for people with dementia. It highlights issues concerning the relative impact of various interventions, the utility of a trial phase to determine use of interventions, and patterns of intervention individualization.
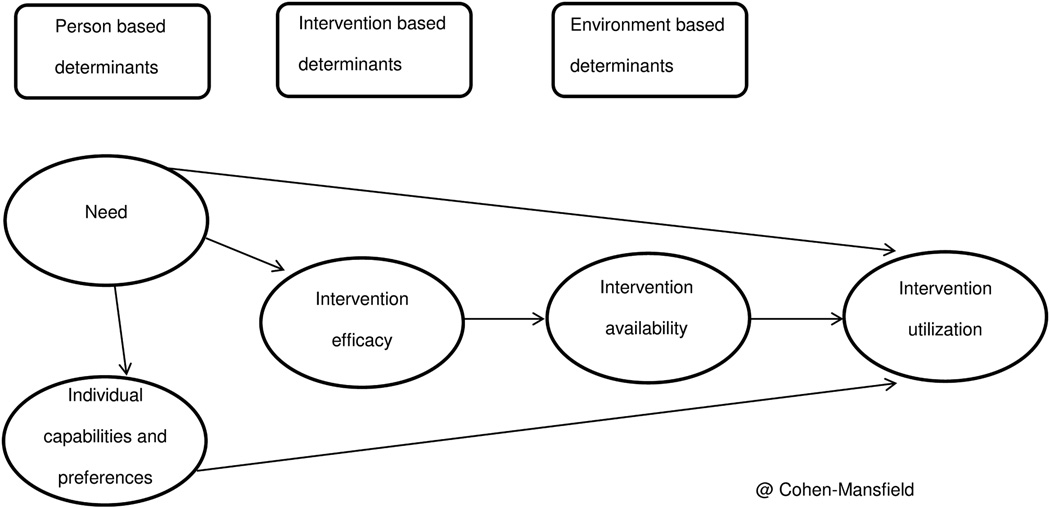
Intervention utilization
Efficacy seems to affect utilization. For example, past research has shown the potency of social interventions in preventing behavioral symptoms.(23) Yet, other factors were also involved. For example, sewing was one of the most highly rated interventions in terms of impact on behavioral symptoms, yet it was one of the least utilized. Tailoring a sewing activity for a participant requires that the person with dementia has adequate cognitive ability and reasonably good dexterity, which may not have been present in most of our sample. While female gender was associated with utilizing sewing, this association did not impede utilization in our sample of 73% females. For persons with very limited abilities, a narrower range of interventions is available. The fabric book was one of the interventions appropriate for persons with very low cognitive function, but the low utilization rates of this intervention may be accounted for by its relatively low efficacy. Availability of interventions may also affect their utilization. For example, in our study, appropriate group activities were often not available in the nursing home, and one-on-one interaction was more feasible than setting up new groups. Figure 2 summarizes the factors affecting intervention utilization. Accordingly, interventions will have low utilization if they require abilities not present for most participants, if they are not efficacious, or if they are not available for other reasons, such as resource allocation. While availability is a modifiable factor, future research needs to expand the current findings by examining the utilization and efficacy of other interventions. It should also investigate what factors may make an intervention better fitted to the persons’ abilities or more efficacious. For example, in previous research we noted that the more socially acceptable the intervention, the lower the refusal rates (24). Additional parameters affecting use and efficacy should be examined.
Figure 2.
Factors affecting intervention utilization
Note. Some unmet needs have a direct effect on intervention utilization, such as request for food or drink. Other needs are best catered to by the most efficacious intervention for those needs, e.g., direct social interaction for a social need, but utilization is then affected by intervention availability. In the current study, intervention availability was high for one-on-one interaction and low for group activities. Some needs such as for activity or for meaning can be addressed by specific interventions, such as sewing, the utilization of which is determined by their match to participants’ individual capabilities and preferences.
Efficacy of intervention
The use of tailored interventions does not lend itself to proper comparison of interventions, as efficacy is a function not only of the intervention but also of the person receiving it. The high efficacy rates of some of the interventions in both trial and treatment phases, such as walking, going outside, or sewing, may reflect the combination of intervention efficacy and selection of participants. The high efficacy of care activities intervention in both phases may result from the direct impact of responding to a clear need, such as going to the bathroom. Interestingly, hand massage, used with those with the lowest cognitive functioning, was still rated as more than somewhat effective. In contrast, fabric book, presented to the same group, had low efficacy rates, either because of intervention or recipient effects. Most of the intervention comparisons yielded no results (i.e., the combined sample was too small) or non- significant differences. In line with this, nonpharmacological interventions` comparable efficacy (or lack of efficacy) has been previously reported (6, 8, 9). The lack of significant differences in nonpharmacological interventions` efficacy may be even more evident in this study because interventions were chosen to fit the participants receiving them. However, it also should be considered that the small sample size (n=10 using the same intervention) did not provide sufficient power for comparison.
Notwithstanding the above limitations, comparisons did yield significant findings:
-
Interventions found to be superior to others:
One-on-one interaction was often better than nonsocial (e.g., squeeze ball) or simulated social (e.g., robotic animal) interventions. This is supported by previous research showing live social intervention to be superior to other approaches in preventing behavioral symptoms(25) or showing one-on-one social contact to be superior to music, family video, or usual care in its impact on verbal agitation.(10)-
◦Hand massage was superior to simulated social interventions (doll in trial phase, respite video in treatment phase) and to some nonsocial interventions (in the trial phase) as well as to one-on-one interaction in the treatment phase. This may be because hand massage was used with very low cognitive functioning participants, and because this intervention combines one-on-one social interaction with sensory stimulation.
-
◦Music was superior to several other interventions in the trial phase, but it was only superior to robotic animal in the treatment phase.
-
◦Topic video, care, and folding towels were better than other interventions in the treatment phase but not in the trial phase. This could be related to smaller sample sizes in the trial phase or to different combinations of participants in trial and treatment phases.
-
◦
- Interventions found to be inferior to others:
-
◦Puzzle was inferior to several interventions in the trial phase, but in the more tailored treatment phase, it was inferior to only the video intervention.
-
◦Robotic animal was inferior to human direct or simulated social interaction, reinforcing the importance of human contact found in a study of engagement of persons with dementia(23), and to music.
-
◦Differences with the respite video and the squeeze ball were only significant in the treatment phase. Both findings reinforce the importance of social contact gradations, i.e., a respite video, in which a stranger talks to the person with dementia, is less effective than a family video, or to a hand massage, involving live human touch. Similarly a squeeze ball activity is less effective than social contact activities, such as one-on-one interaction.
-
◦
Inevitably this study has limitations, pointing out the need for further research. First, it includes a small sample size for specific interventions. Future research should include larger sample sizes, providing greater power to detect differences in the comparisons and allowing the study of interventions that are used less frequently. In addition, when including a larger sample one should control for family wise type I error (multiple comparisons). In this study we did not do so given its exploratory and descriptive nature which made us search for trends rather than precise differences. Second, interventions were chosen and delivered (or initiated, e.g., for nursing interventions) by the same research assistant who completed the CAR, raising questions about possible bias. However, there was no a-priori suggestion that any intervention would prove better than another. Indeed, the comparison among interventions was not the original goal of the study. It was clear to all that different participants would respond differently to different interventions, and the goal of the CAR was descriptive. Therefore we believe that the research assistants did not have any consistent bias in their rating. Indeed, we believe that such evaluation of treatment emulates well the process of intervention during clinical work. A third limitation is that single participants were provided with multiple interventions. Further research should investigate whether our significant results were caused by independent effects, or interaction/cumulative effects between the different interventions.
While we hope that these comparisons will guide caregivers in their choice of stimuli and intervention, we acknowledge their limitations in providing practice guidelines, as (1) the different comparisons involved different subgroups of participants and (2) specific circumstances of unmet needs guided the choice of intervention. Also, it is impossible to determine the impact of the specific exemplars used for each category, e.g., different types of robotic animals or of real looking dolls.
In this study, research assistants decided which interventions to implement and then implemented them. Translating this procedure to the daily nursing home practice would mean that the nursing staff would be responsible for these tasks. We believe nursing staff would obtain similar results. Apart from practical issues such as time demand, the need for training and mentoring, and organizational support for the effort, nursing staff should be able to follow the TREAs protocol in order to decide on tailored interventions and evaluate the effects of interventions. Another option for promoting nonpharmacological interventions in practice involves dedicating a specialized person to implement and evaluate these interventions (such as a medicine aid is available for pharmacological interventions). Regardless of who implements the intervention, including an immediate evaluation of the intervention, as with the CAR would likely increase thoughtful reflection and systematic consistent practice in the nursing home.
The high refusal rates of robotic animals and real looking dolls may be related to their low social acceptability(26). To better ascertain the factors that affect refusals, future research should control for interventions` social value and appropriateness, the amount of involvement required, and the cognitive level of participants. The fact that refusal rates were significantly lower in the treatment phase than in the trial phase, and that there was a trend for better efficacy in the treatment phase, suggests that utilization of a trial phase is useful in the process of optimizing sets of nonpharmacological stimuli to match the needs, abilities and preferences of persons with dementia and behavioral symptoms.
In addition to providing new information on the utilization of nonpharmacological interventions and comparing them, this paper sets an example of how ongoing clinical data can be utilized to improve our understanding of caring for persons with dementia. Using a similar approach to classify interventions and systematically record their use and impact, nursing homes can clarify the very important issues of utilization including who receives what intervention, and what is the interventions` efficacy? This provides an opportunity to compare interventions` efficacy, and thus provide avenues for improvement. Although the rating may not be ‘objective’ because the same person delivers, and rates multiple interventions to multiple people, that becomes less important. Furthermore, through their continued contact with participants, the caregivers delivering interventions can also become more sensitive to the nuances of participants` responses. Such ongoing monitoring can offer a substantial tool for improving care and sensitivity in long term care.
ACKNOWLEDGMENTS
Source of Funding: This study was supported by National Institutes of Health grant AG010172 and by the Minerva-Stiftung Foundation Grant number 31583295000. The funders had no role in the research study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: There are no conflicts of interest.
Author Contributions: Jiska Cohen-Mansfield directed the study, contributed to the data collection and was involved in data analysis, interpretation of data and write up. Marcia S. Marx contributed to the conceptualization of the study, was involved in overseeing the data collection and participated in the interpretation of the data and write-up. Maha Dakheel-Ali was involved in data collection and data analysis. Khin Thein was involved in the coordination of data collection, data collection, data checks and organization.
Sponsor`s Role: None.
REFERENCES
- 1.Woodward MR, Harper DG, Stolyar A, et al. Dronabinol for the treatment of agitation and aggressive behavior in acutely hospitalized severely demented patients with noncognitive behavioral symptoms. The American Journal of Geriatric Psychiatry. 2013 doi: 10.1016/j.jagp.2012.11.022. [DOI] [PubMed] [Google Scholar]
- 2.Herrmann N, Black SE, Chow T, et al. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. The American Journal of Geriatric Psychiatry. 2012;20(9):789–797. doi: 10.1097/JGP.0b013e31823033f3. [DOI] [PubMed] [Google Scholar]
- 3.Brodaty H, Burns K. Nonpharmacological management of apathy in dementia: A systematic review. The American Journal of Geriatric Psychiatry. 2012;20(7):549–564. doi: 10.1097/JGP.0b013e31822be242. [DOI] [PubMed] [Google Scholar]
- 4.Cohen-Mansfield J. Theoretical frameworks for behavioral problems in dementia. Alzheimer’s Care Today. 2000;1(4):8–21. [Google Scholar]
- 5.Cohen-Mansfield J, Thein K, Marx MS, et al. Efficacy of nonpharmacologic interventions for agitation in advanced dementia: a randomized, placebo-controlled trial. J Clin Psychiatry. 2012;73(9):61–1255. doi: 10.4088/JCP.12m07918. [DOI] [PubMed] [Google Scholar]
- 6.Sloane PD, Hoeffer B, Mitchell CM, et al. Effect of person-centered showering and the towel bath on bathing-associated aggression, agitation, and discomfort in nursing home residents with dementia: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(11):1795–1804. doi: 10.1111/j.1532-5415.2004.52501.x. [DOI] [PubMed] [Google Scholar]
- 7.Baillon S, Van Diepen E, Prettyman R, et al. A comparison of the effects of Snoezelen and reminiscence therapy on the agitated behaviour of patients with dementia. Int J Geriatr Psychiatry. 2004;19(11):1047–1052. doi: 10.1002/gps.1208. [DOI] [PubMed] [Google Scholar]
- 8.Beck CK, Vogelpohl TS, Rasin JH, et al. Effects of behavioral interventions on disruptive behavior and affect in demented nursing home residents. Nurs Res. 2002;51(4):219–228. doi: 10.1097/00006199-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Toseland RW, Diehl M, Freeman K, et al. The impact of validation group therapy on nursing home residents with dementia. J Appl Gerontol. 1997;16(1):31–50. [Google Scholar]
- 10.Cohen-Mansfield J, Werner P. Management of verbally disruptive behaviors in nursing home residents. J Gerontol A Biol Sci Med Sci. 1997;52(6):369–377. doi: 10.1093/gerona/52a.6.m369. [DOI] [PubMed] [Google Scholar]
- 11.Cohen-Mansfield J, Kerin P, Pawlson G, et al. Informed consent for research in a nursing home: Processes and issues. The Gerontologist. 1988;28(3):355–360. doi: 10.1093/geront/28.3.355. [DOI] [PubMed] [Google Scholar]
- 12.Morris J, Hawes C, Murphy K, et al. MDS resident assessment. Natick, MA: Eliot Press; 1991. [Google Scholar]
- 13.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state" A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 14.Cohen-Mansfield J, Billig N. Agitated behaviors in the elderly: I. A conceptual review. J Am Geriatr Soc. 1986 doi: 10.1111/j.1532-5415.1986.tb04302.x. [DOI] [PubMed] [Google Scholar]
- 15.Cohen-Mansfield J, Werner P, Marx MS. An observational study of agitation in agitated nursing home residents. Int Psychogeriatr. 1989;1(02):153–165. doi: 10.1017/s1041610289000165. [DOI] [PubMed] [Google Scholar]
- 16.Lawton MP, Van Haitsma K, Klapper J. Observed affect in nursing home residents with Alzheimer's disease. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1996;51(1):P3–P14. doi: 10.1093/geronb/51b.1.p3. [DOI] [PubMed] [Google Scholar]
- 17.Guy W. Clinical global impression scale. The ECDEU Assessment Manual for Psychopharmacology-Revised Volume DHEW Publ No ADM 76. 1976;338:218–222. [Google Scholar]
- 18.Fieve R, Goodnick P, Peselow E, et al. Pattern analysis of antidepressant response to fluoxetine. The Journal of clinical psychiatry. 1986;47(11):560–562. [PubMed] [Google Scholar]
- 19.Sato TL, Turnbull CD, Davidson JR, et al. Depressive illness and placebo response. The International Journal of Psychiatry in Medicine. 1984;14(3):171–179. [Google Scholar]
- 20.Cohen-Mansfield J. Instruction Manual for the Cohen-Mansfield Agitation Inventory (CMAI) Research Institute of the Hebrew Home of Greater Washington; 1991. [Google Scholar]
- 21.Cohen-Mansfield J. Nonpharmacological management of behavioral problems in persons with dementia: The TREA model. Alzheimer’s Care Today. 2000;1(4) 22&hyhen. [Google Scholar]
- 22.Cohen-Mansfield J. Theoretical frameworks for behavioral problems in dementia. Alzheimer’s Care Today. 2000;1(4) 8&hyhen. [Google Scholar]
- 23.Cohen-Mansfield J, Thein K, Dakheel-Ali M, et al. The value of social attributes of stimuli for promoting engagement in persons with dementia. J Nerv Ment Dis. 2010;198(8):586–592. doi: 10.1097/NMD.0b013e3181e9dc76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen-Mansfield J, Marx MS, Freedman LS, et al. The comprehensive process model of engagement. The American Journal of Geriatric Psychiatry. 2011;19(10):859–870. doi: 10.1097/JGP.0b013e318202bf5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen-Mansfield J, Marx MS, Dakheel-Ali M, et al. Can agitated behavior of nursing home residents with dementia be prevented with the use of standardized stimuli? J Am Geriatr Soc. 2010;58(8):1459–1464. doi: 10.1111/j.1532-5415.2010.02951.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen-Mansfield J, Marx MS, Dakheel-Ali M, et al. Can persons with dementia be engaged with stimuli? Am J Geriatr Psychiatry. 2010;18(4):351. doi: 10.1097/jgp.0b013e3181c531fd. [DOI] [PMC free article] [PubMed] [Google Scholar]