Abstract
Introduction:
Penile degloving is an important step in orthoplasty. Although its role in correcting mild curvature in distal and midshaft hypospadias has been previously reported, its impact on ventral curvature (VC) correction in proximal defects warrants further investigation. Therefore, we sought to document the effect of degloving and proximal urethral dissection on VC correction in children with proximal hypospadias.
Methods:
We retrospectively reviewed the records of 137 patients who underwent proximal hypospadias repair between 1998 and 2006. VC, defined as mild (<30%), moderate (30%–45%), and severe (>45%), was recorded before penile degloving and after erection test. Percent improvement in VC and need for further treatment (beyond degloving and proximal dissection) based on preoperative degree of curvature were assessed. ANOVA test was used to compare improvement among the 3 groups.
Results:
Mean age at repair was 14 months (range: 6–24). Penile degloving associated with proximal urethral dissection when necessary was responsible for the improvement in the degree of curvature in 7 of 9 (77%) patients with mild VC, 23 of 44 (52%) with moderate and 35 of 84 (40%) with severe VC. Additionally, degloving alone was sufficient for VC correction in 7 of 9 (77%) mild cases, 14 of 44 (30%) moderate and only 2 of 84 (2%) severe cases. The difference among these 3 groups was statistically significant (p < 0.001).
Conclusions:
Penile degloving alone can correct VC. The percentage of improvement depends on the preoperative degree of curvature, with severe VC cases showing the least improvement.
Introduction
Penile degloving is an essential first step of orthoplasty. Mettauer was one of the first physicians in 1842 to identify and highlight the importance of adequate degloving to correct ventral curvature (VC) caused by skin tethering.1 Other orthoplasty maneuvers, such as proximal ventral dissection (PVD) down to the bulbar urethra2,3 and release of lateral fibrous attachments, may be added depending on the severity of VC.
PVD has been used as an additional step of degloving to achieve further penile straightening4 before more radical maneuvers, such as urethral plate lifting, transection and corpora cavernosa grafting, are attempted.2,3 According to a recent publication, straightening of the phallus with preservation of the urethral plate can be achieved even in penoscrotal hypospadias.3 Based on these encouraging results and the lack of previous evidence on this topic, we decided to objectively document the effect of degloving and proximal ventral dissection on VC improvement in children with penoscrotal hypospadias.
Methods
Patients and selection criteria
After receiving approval from the Research Ethics Board, we retrospectively reviewed 137 consecutive patients who underwent repair of proximal hypospadias from January 1998 and December 2006. We considered proximal hypospadias as all cases whose meatal location ranged from the proximal shaft of the penis to the perineum. We excluded patients with mid-shaft defects, those who had reoperations, and cases in which the degree of curvature was not documented prior to the procedure. VC was classified as mild, moderate, or severe according to the 1999 American Academy of Pediatrics survey,5 which defined mild curvature as less than 30 degrees, moderate between 30 and 45° and severe greater than 45°. Preoperative testosterone stimulation was selectively given depending on surgeon preference and family acceptance.
Surgical technique
Dorsal plication (DP) was performed using the classic Nesbitt tuck,1 the 12 o’clock midline plication as described by Baskin,7 or displacing the neurovascular bundle in the midline and plicating directly the tunica albuginea, according to surgeon preference. When ventral penile lengthening was employed, a transverse incision was made at the point of greatest curvature through the tunica albuginea, and the defect was patched with a graft or a tunica vaginalis flap. Regardless of the procedure used to correct the VC, urethroplasty was carried out with the transverse island flap technique or one of its modifications depending on whether the plate was divided or not. Glansplasty was performed with interrupted sutures using 6-0 monocryl. Skin closure was achieved with a midline closure or with a double face onlay flap if considerable ventral skin deficiency was present. All patients were given intravenous Cefazolin before skin incision. Oral antibiotics were continued as long as a urethral stent or suprapubic tube remained in place. A compressive dressing (Coban, 3M Inc.) was wrapped around the penis for 24 to 48 hours.
Statistical analysis
Percentage of VC improvement after penile degloving was compared among mild, moderate and severe curvature cases using ANOVA test analysis, with p < 0.05 considered statistically significant. Statistical analysis was completed with the assistance of commercially available statistics software (SPSS® version 15.0, Cary, NC).
Results
Pre- and post-degloving VC data were available for 137 consecutive patients. The mean age at surgery was 18 months, ranging from 11 to 49 months, with 41% receiving preoperative testosterone. Of the 137 children who underwent repair, 18 had proximal penile hypospadias, 75 penoscrotal, 24 scrotal and 20 perineal. Patients were divided in categories based on the degree of preoperative VC ranging from mild (<30%, n = 9), moderate (30%–45%, n = 44), and severe (>45%, n = 84). Improvement in VC post-degloving alone was seen in 77%, 52%, and 40% (p < 0.01) of patients with mild, moderate, and severe VC, respectively (Table 1).
Table 1.
Percentage improvement after penile degloving
| Type of VC (degrees) | Preoperative (before degloving) (n = 137) | After degloving | n | Percentage improvement |
|---|---|---|---|---|
| Mild (<30) | 9 | No VC | 7 | 77.3% |
| Mild | 2 | |||
| Moderate (30–45) | 44 | No VC | 13 | 52.4% |
| Mild | 10 | |||
| Moderate | 21 | |||
| Severe (>45) | 84 | No VC | 2 | 40.4% |
| Mild | 2 | |||
| Moderate | 31 | |||
| Severe | 49 |
VC: ventral curvature.
A satisfactory straight penis (no VC) was achieved with complete penile degloving only in 77%, 29.5%, and 2% (p < 0.001) of children with mild, moderate and severe VC, respectively (Table 2).
Table 2.
Percentage of patients with no ventral curvature after penile degloving
| Type of VC (degrees) | Preoperative (before degloving) (n = 137) | After degloving | n | Percentage with no VC post-degloving | p |
|---|---|---|---|---|---|
| Mild (<30) | 9 | No VC | 7 | 77.3% | |
| Mild | 2 | ||||
| Moderate (30–45) | 44 | No VC | 13 | 29.5% | |
| Mild | 10 | p <0.001 | |||
| Moderate | 21 | ||||
| Severe (>45) | 84 | No VC | 2 | 2.4% | |
| Mild | 2 | ||||
| Moderate | 31 | p <0.001 | |||
| Severe | 49 |
VC: ventral curvature.
Of the 9 boys who initially had mild VC, 2 had persistent curvature following degloving alone and underwent dorsal plication. Of the 44 patients who had moderate VC, 21 continued to have persistent moderate VC after degloving. Of these 21 patients, 18 had DP, 2 with VPL, and 1 lifting of the urethral plate. Of the 84 boys who initially had severe VC, 49 continued to have severe VC post degloving. VPL was undertaken in 29, DP in 19 and PVD in 1 patient. Tunica vaginalis flap was used in 23 of 38 patients who underwent VPL, while grafts (dural-4, dermal-3, bovine perocardium-7, and porcine collagen-1) were employed in the remaining 15 children (Fig. 1).
Fig. 1.
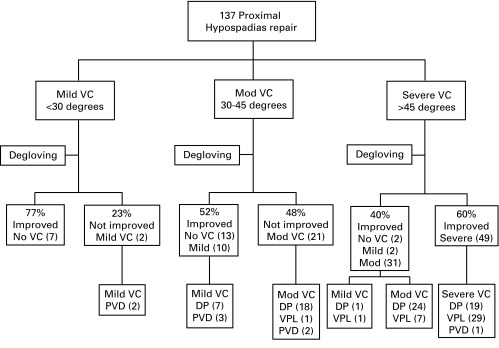
Outcome of 137 patients with proximal hypospadias.
Discussion
VC correction in proximal hypospadias remains a challenging and controversial topic among pediatric urologists. Distinct from distal and mid-shaft repairs, in which dorsal plication and penile degloving are widely accepted and employed to correct penile bending, several techniques have been described to correct VC in proximal hypospadias. Unfortunately, none has emerged as clearly superior in regards to complications and effectiveness.
The role played by skin deficiency in the formation of curvature seems especially striking in the manipulation of the penis without an artificial erection in patients with proximal hypospadias. It is very easy to pull the skin downward and create considerable ventral curvature. Artificial erection was first described by Gittes and McLaughlin in 1974,6 which was a very significant contribution to orthoplasty. Although the description “orthoplasty” is more commonly referred to as “release of chordee,” this implies that the bend is caused by fibrous bands. However, multiple independent authors have found histologically increased vascularity in ventral dartos and spongiosum tissue without fibrous scar.7–9 Therefore, we have adopted the term “ventral curvature,” which more accurately expresses underlying pathology. Most patients with mild (<30 degrees) VC preoperatively had straight phallus after degloving on artificial erection test. In more severe cases (>45 degrees), degloving was not effective to correct the VC as 98% of these patients required more than degloving to obtain a straight penis.
Significant variability exists for preferred technique for proximal hypospadias and curvature correction.10 Even in the most severe hypospadias, the urethral plate may not require division to produce a straight penis.2–4 Snodgrass and colleagues3 recently reported that mobilization of the urethral plate in proximal hypospadias cases with greater than 30-degree ventral curvature after penile degloving reduced the need for urethral plate transection. The evolution of this concept required numerous experiences of dividing the urethral plate and performing extensive ventral corporeal dissection, only to have significant penile curvature persist with artificial erection.11,12 Our results show that if the preoperative VC is less than 45 degrees, significant improvement should be expected after degloving and about 30% will convert to a straight penis. Even patients with proximal hypospadias and severe VC have a 40% chance of improving after degloving and a 2% chance of requiring no further treatment. As mentioned by Hadidi13 we also suggest there are 2 types of VC associated with proximal hypospadias. The first type is VC associated with superficial subcutaneous skin tethering, proximal to the meatus that can be corrected with degloving. The second type of VC, presented in more severe cases, is usually intrinsic and deeply located. The residual curvature may be corrected by many different techniques and can only be revealed after degloving. Nevertheless, some cases still require division of the urethral plate, particularly when it is poorly developed. Yet, we have concern with early division of the urethral plate prior to degloving as described in some techniques since the true degree of VC has not been assessed.14
An important limitation of our study is that post-degloving assessment of VC was determined with an artificial erection test which did not represent a natural clinical scenario. Additionally, in patients with proximal defects and more severe ventral curvature there was an inherent higher likelihood of the dissection broadly labeled as degloving, including proximal release of the ventral aspect of the penis into the scrotum and peri-bulbar region in comparison with more distal defects.
Conclusion
This study is the first in the literature to objectively document the effect of degloving in proximal hypospadias surgery. We found penile degloving alone can correct VC with the percentage of improvement dependent on preoperative degree of curvature, with severe VC cases showing the least improvement and requiring additional management.
Footnotes
Competing interests: Dr. Weber, Dr. Braga, Dr. Patel, Dr. Pippi Salle, Dr. Bägli, Dr. Khoury and Dr. Lorenzo declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Mettauer J. Practical observations on those malformations of the male urethra and penis, termed hypospadias and epispadias, and epispadias, with an anomalous case. Am J Med Sci. 1842;4:42. doi: 10.1097/00000441-184207000-00003. [DOI] [Google Scholar]
- 2.Bhat A. Extended urethral mobilization in incised plate urethroplasty for severe hypospadias: A variation in technique to improve chordee correction. J Urol. 2007;178:1031–5. doi: 10.1016/j.juro.2007.05.074. [DOI] [PubMed] [Google Scholar]
- 3.Snodgrass W, Prieto J. Straightening ventral curvature while preserving the urethral plate in proximal hypospadias repair. J Urol. 2009;182:1720–5. doi: 10.1016/j.juro.2009.02.084. [DOI] [PubMed] [Google Scholar]
- 4.Baker LA, Mathews RI, Docimo SG. Radical bulbar dissection to correct severe chordee and proximal hypospadias. J Urol. 2000;164:1347–9. doi: 10.1016/S0022-5347(05)67194-7. [DOI] [PubMed] [Google Scholar]
- 5.Bologna RA, Noah TA, Nasrallah PF, et al. Chordee: Varied opinions and treatments as documented in a survey of the American Academy of Pediatrics, Section of Urology. Urology. 1999;53:608–12. doi: 10.1016/S0090-4295(98)00656-6. [DOI] [PubMed] [Google Scholar]
- 6.Gittes RF, McLaughlin AP., 3rd Injection technique to induce penile erection. Urology. 1974;4:473–4. doi: 10.1016/0090-4295(74)90025-9. [DOI] [PubMed] [Google Scholar]
- 7.Baskin LS, Erol A, Li YW, et al. Anatomical studies of hypospadias. J Urol. 1998;160:1108–15. doi: 10.1016/S0022-5347(01)62711-3. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan GW, Lamm DL. Embryogenesis of chordee. J Urol. 1975;114:769–72. doi: 10.1016/s0022-5347(17)67140-4. [DOI] [PubMed] [Google Scholar]
- 9.Snodgrass W, Patterson K, Plaire JC, et al. Histology of the urethral plate implications for hypospadias repair. J Urol. 2000;164:988–9. doi: 10.1016/S0022-5347(05)67233-3. [DOI] [PubMed] [Google Scholar]
- 10.Cook A, Khoury AE, Neville C, et al. A multicenter evaluation of technical preferences for primary hypospadias repair. J Urol. 2005;174:2354–7. doi: 10.1097/01.ju.0000180643.01803.43. [DOI] [PubMed] [Google Scholar]
- 11.Elder JS, Duckett JW, Snyder HM. Onlay island flap in the repair of mid and distal penile hypospadias without chordee. J Urol. 1987;138:376–9. doi: 10.1016/s0022-5347(17)43152-1. [DOI] [PubMed] [Google Scholar]
- 12.Hollowell JG, Keating MA, Snyder HM, 3rd, et al. Preservation of theurethral plate in hypospadias repair: Extended applications and further experience with the onlay island flap urethroplasty. J Urol. 1990;143:98–100. doi: 10.1016/s0022-5347(17)39878-6. [DOI] [PubMed] [Google Scholar]
- 13. Hypospadias-Surgery.com. Hypospadias Surgery. 2012. http://www.hypospadias-surgery.com/index.html. Accessed November 27, 2014.
- 14.Nonomura K, Kovanagi T, Imanaka K, et al. One-stage total repair of severe hypospadias with scrotal transposition: Experience in 18 cases. J Pediatr Surg. 1988;23:177–80. doi: 10.1016/S0022-3468(88)80152-0. [DOI] [PubMed] [Google Scholar]


