Abstract
Objective:
To identify independent predictors of and use recursive partitioning to develop a multivariate regression tree predicting symptom duration greater than 28 days after a sport-related concussion.
Methods:
We conducted a prospective cohort study of patients in a sports concussion clinic. Participants completed questionnaires that included the Post-Concussion Symptom Scale (PCSS). Participants were asked to record the date on which they last experienced symptoms. Potential predictor variables included age, sex, score on symptom inventories, history of prior concussions, performance on computerized neurocognitive assessments, loss of consciousness and amnesia at the time of injury, history of prior medical treatment for headaches, history of migraines, and family history of concussion. We used recursive partitioning analysis to develop a multivariate prediction model for identifying athletes at risk for a prolonged recovery from concussion.
Results:
A total of 531 patients ranged in age from 7 to 26 years (mean 14.6 ± 2.9 years). The mean PCSS score at the initial visit was 26 ± 26; mean time to presentation was 12 ± 5 days. Only total score on symptom inventory was independently associated with symptoms lasting longer than 28 days (adjusted odds ratio 1.044; 95% confidence interval [CI] 1.034, 1.054 for PCSS). No other potential predictor variables were independently associated with symptom duration or useful in developing the optimal regression decision tree. Most participants (86%; 95% CI 80%, 90%) with an initial PCSS score of <13 had resolution of their symptoms within 28 days of injury.
Conclusions:
The only independent predictor of prolonged symptoms after sport-related concussion is overall symptom burden.
Prospective cohort studies consistently show that most people who sustain sport-related concussions have resolution of their symptoms within a relatively short time period, with more than 90% of athletes recovering within a month of injury.1–3 A small proportion of athletes, however, have prolonged symptoms from their concussions. Previous investigators have studied potential predictors of prolonged recovery such as age, sex, history of previous concussion, amnesia at the time of injury, loss of consciousness at the time of injury, measures of cognitive function, individual symptoms such as headaches and dizziness, and collective symptom burden.4–12
The ability to predict which patients will have prolonged symptoms would allow clinicians to institute therapies sooner, offer anticipatory guidance, and put occupational or academic accommodations in place earlier in the course of recovery. From the patient's perspective, anticipation of a prolonged recovery would facilitate more informed decisions regarding the initiation of therapies and participation in work, school, and sports.
Using a large, prospective cohort of patients with sport-related concussions, we sought to identify independent predictors of symptom duration greater than 28 days after sport-related concussion. Furthermore, we sought to use multiple potential predictors to develop a predictive model that would estimate the probability of having prolonged symptom duration after a sport-related concussion.
METHODS
Research design and participants.
We conducted a prospective cohort study of patients who presented to the Sports Concussion Clinic at Boston Children's Hospital within 3 weeks of their injury between October 1, 2009, and July 31, 2011. We included all patients who sustained their concussions during organized sports and those who sustained their concussions as a result of mechanisms similar to sports, such as participating in gym class or falling from a standing position. Patients with more severe injury mechanisms, such as falling from a height or motor vehicle collisions, were excluded. In addition, we excluded patients with incomplete data collection forms and medical records, such that the duration of symptoms could not be reliably determined. Some participants (n = 151) were included in a previous analysis.13 Although based at Boston Children's Hospital, the Sports Concussion Clinic cares for patients of all ages, including adults.
Standard protocol approvals, registrations, and patient consents.
The study was approved by the institutional review board of Boston Children's Hospital.
Definitions.
Concussion was defined according to the definition proposed by the International Conference on Concussion in Sport.14 Therefore, athletes experiencing a rapid rotational acceleration of the head resulting in the onset of signs and symptoms included in the Post-Concussion Symptom Scale (PCSS) were diagnosed with concussion.
Assessments.
Participants completed an initial intake questionnaire and standard follow-up questionnaires developed at the clinic until they were discharged from care. Data regarding date of injury, mechanism of injury, presence of loss of consciousness or amnesia at the time of injury, sport played at time of injury, history of prior concussions, and medical history were collected on intake forms. At each follow-up clinic visit, participants whose symptoms had resolved were asked to record the date on which they last experienced symptoms. Symptoms were recorded on the PCSS that was published as part of the Sport Concussion Assessment Tool Version 2 (SCAT 2; http://www.cces.ca/files/pdfs/SCAT2%5B1%5D.pdf) developed at the 3rd International Conference on Concussion in Sport held in Zurich, Switzerland, in November 2008.14 The PCSS is a list of 22 symptoms that commonly result from concussion. Athletes rate the level they are experiencing each symptom on a scale from 0 (none) to 6 (severe). Thus, scores range from a possible 0, for athletes who are symptom-free, to 132 (6 × 22), for athletes experiencing each symptom severely. Most of the signs and symptoms included on the PCSS are nonspecific, and can result from other etiologies besides concussion. As we were only interested in symptoms attributable to their concussions, athletes were instructed to rate only those symptoms that started at the time of their injury and were still present within the 24 hours before the clinic visit.5,13 Symptom-free was defined as a PCSS score of 0.
Physicians determined whether or not to obtain neurocognitive testing, based on their usual practice. Therefore, not all participants underwent testing at their initial visit. When performed, computerized neurocognitive assessments were performed using ImPACT, a well-studied tool used for assessing the neurocognitive function of athletes at risk for sport-related concussions.12,15–19 The assessment consists of an initial questionnaire regarding medical history, a symptom inventory, and 6 neurocognitive modules designed to evaluate athletes' memory, attention, processing speed, and reaction time. From these data, 4 composite scores are generated: verbal memory, visual memory, visual motor speed, and reaction time. Assessments were performed while the athletes were alone in a quiet room. As we sought to develop predictors of prolonged recovery, only the data from the initial visit were analyzed.
Statistical analyses.
Previous studies have demonstrated that the majority of athletes will recover from their sport-related concussions within 4 weeks of injury.2,3,20,21 Furthermore, we do not routinely change our clinical management of concussion for the first several weeks after injury. Therefore, we sought to identify predictors of prolonged recovery beyond 28 days. Clinically, we define recovery as (1) symptom-free at rest and with exertion after discontinuing any medications started to treat concussion symptoms, (2) return to baseline measures of neurocognitive function (when available), and (3) return to baseline measures of postural stability (when available). Measures of postural stability and neurocognitive function, however, are only assessed at clinic visits; they are not performed daily. Thus, we cannot determine precisely when an athlete has recovered according to these criteria. We can only determine if he or she has recovered by the time of his or her clinic visits. Therefore, we chose symptom duration, defined as the time (days) between the date of injury and the date of last symptoms, as the main outcome variable.
Potential predictor variables were determined from the available medical literature and consisted of age, sex, initial score on symptom inventories, history of prior concussions, number of prior concussions, performance on computerized neurocognitive assessments, loss of consciousness at the time of injury, amnesia at the time of injury, history of medical treatment for headaches, self-reported history of migraine headaches, and family history of concussion.1,10,16,20,22–26 Univariate analyses of continuous variables were assessed using Student t test. Categorical variables were assessed using the χ2 test. All potential predictor variables that differed between the 2 groups (those with symptoms lasting beyond 28 days and those whose symptoms resolved within 28 days) with a statistical probability of p < 0.20 were placed into a logistic regression model in order to determine the independent effect of each variable on symptom duration, reported as an adjusted odds ratio. Any adjusted odds ratio with a 95% confidence interval that did not include 1.0 was considered statistically significant. As is common when developing logistic regression models, we used a lower threshold for significance when deciding which variables to enter into the model, since the true size and significance of the effect of certain variables may be masked by potential confounding variables.27 No inferences are drawn from these analyses; they are simply a screening to determine which independent variables are included in the model. Before entering variables into the regression model, we assessed for collinearity using variable inflation factors. When 2 variables were collinear with a variable inflation factor of >2.5, only 1 variable was included in a given regression model.
In addition, we sought to develop a multivariate prediction model for identifying athletes at risk for a prolonged recovery from concussion using recursive partitioning analysis (Classification and Regression Trees, version 7, Salford Systems, Palo Alto, CA). The advantage of this analysis is that it allows for the detection of significant patterns and relationships among predictive variables, identifying the most predictive cutoff points for each variable with predictive value.28 Recursive partitioning analysis uses the Gini method to develop a classification tree. A “parent” node is divided into “child” nodes using available candidate predictors. At each branch point of the tree, the variable that best separates parent node into the most homogenous nodes based on the binary outcome variable is used. The recursive partitioning analysis also determines the best cutpoints for continuous variables, those cutpoints that most reliably discriminate the outcome. Finally, the optimal decision tree is developed, which balances the proper identification of the outcome with the fewest branches. The software performs an internal V-fold cross-validation procedure to develop the best tree: the dataset is divided into 10 equal parts with random distribution of outcome variable, and then the model is derived with 9 parts (the learning set) and tested with 1 part (the validation set). This cross-validation is repeated 10 times, and the results are combined to develop the predictive accuracy and error rates for the tree. At the end of the analysis, all subjects are divided into high-risk and low-risk subset nodes for the outcome variable.
RESULTS
A total of 1,124 patients were seen in clinic during the study period; 593 patients were excluded for presenting to clinic more than 21 days after their injury (n = 469), not having a precise date of injury recorded in the medical record or questionnaire (n = 117), or having a nonsports mechanism of injury (n = 7). Of the remaining 531 patients, 129 (24%) had computerized neurocognitive testing performed at their initial visit.
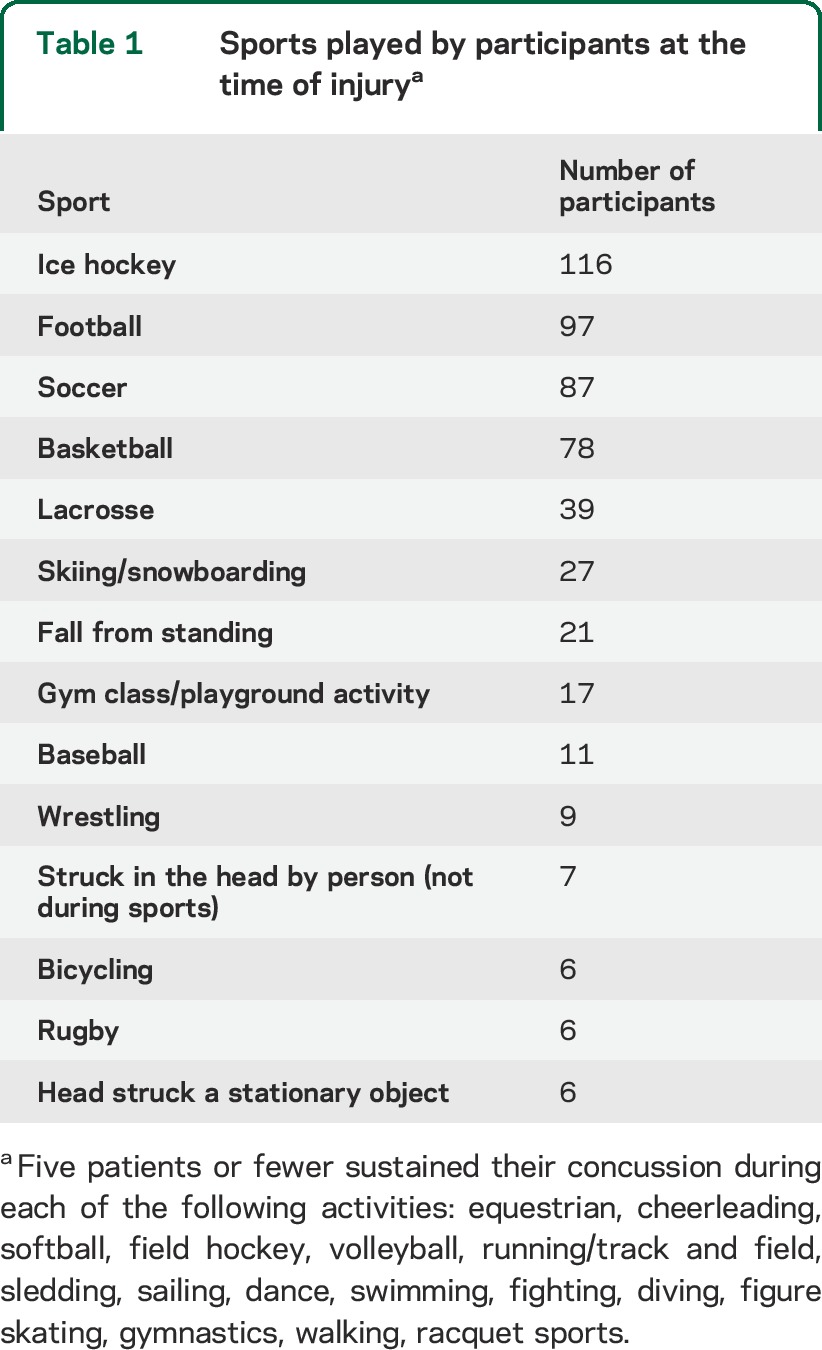
Patients ranged in age from 7 to 26 years, with a mean age of 14.6 ± 2.9 years; 61 patients were adults (>18 years old). Nearly two-thirds (62.4%) of participants were male. The mean PCSS score at the initial visit was 26 ± 26. At the time of injury, 21.1% of participants experienced a self-reported loss of consciousness, while 33.1% reported experiencing amnesia. More than one-third (34.7%) of athletes had sustained at least one previous sport-related concussion and 14.1% had sustained a prior concussion that occurred outside of sports. The mean number of prior concussions sustained by participants was 0.79 ± 1.27. Relatively few participants reported a previous diagnosis of migraine headaches (8.0%) or medical treatment for headaches (13.9%) prior to their concussion. The mean time between injury and presentation to clinic was 12.0 ± 5.3 days. The number of days between injury and initial clinic visit was weakly correlated with initial PCSS score (Spearman rho 0.251). Most patients sustained their injury during collision or contact sports (table 1).
Table 1.
Sports played by participants at the time of injurya
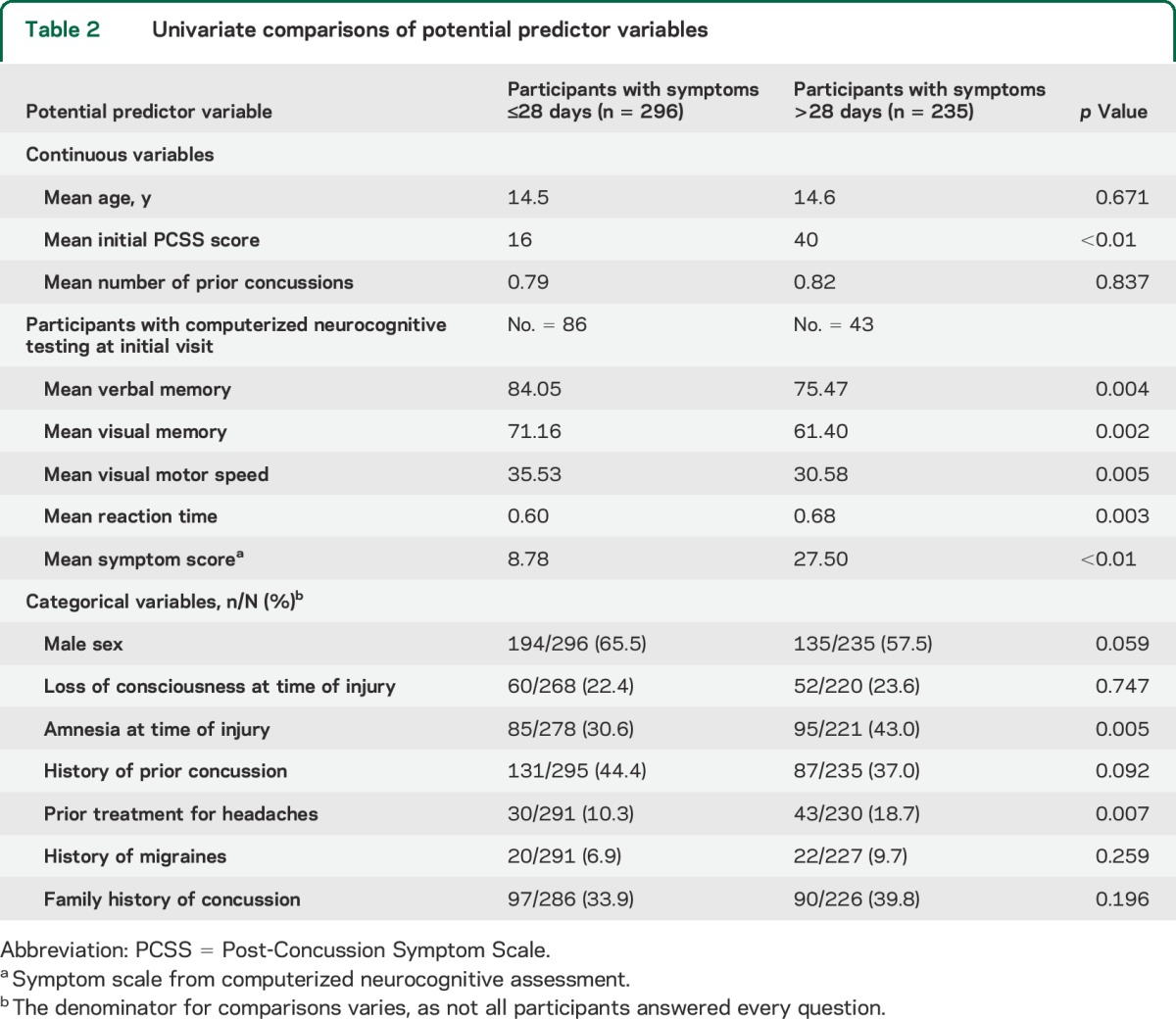
Among the continuous variables assessed, initial score on the PCSS and all composite scores on computerized neurocognitive tests met criteria for inclusion in the regression model (table 2). Of the categorical variables, sex, history of prior concussion, amnesia at the time of injury, prior treatment for headaches, and family history of concussion met criteria for inclusion in the model (table 2).
Table 2.
Univariate comparisons of potential predictor variables
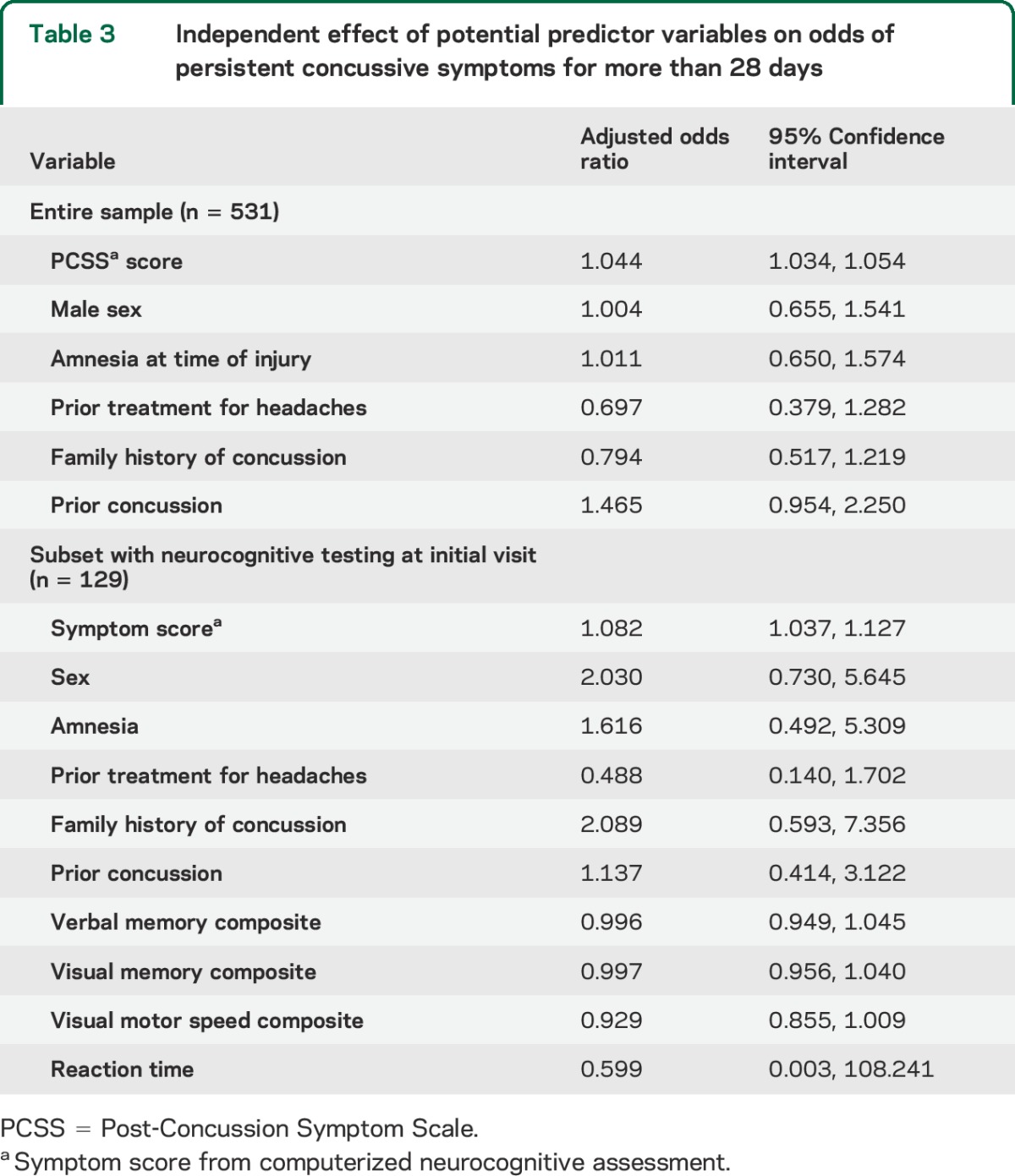
When regression analyses were performed on the entire sample, only total symptom burden as recorded on the PCSS at the time of initial visit was independently associated with symptom duration of greater than 28 days (table 3). When regression analyses were repeated on the sample of patients that had computerized neurocognitive testing at the time of their initial visit, again, only symptom burden was independently associated with symptoms lasting longer than 28 days (table 3).
Table 3.
Independent effect of potential predictor variables on odds of persistent concussive symptoms for more than 28 days
Our recursive partitioning analysis found that PCSS score at the time of initial visit was the variable that best predicted symptom duration, with only one branch point (PCSS cutoff point of 13) included in the optimal decision tree (figure 1). Additional analyses using only those patients who had computerized neurocognitive assessment performed at the time of their initial visit again revealed that PCSS score at the time of initial visit was the variable that best predicted symptom duration with only one branch point (PCSS cutoff point of 11) included in the optimal decision tree (figure 2).
Figure 1. Optimal classification and regression tree for all participants.
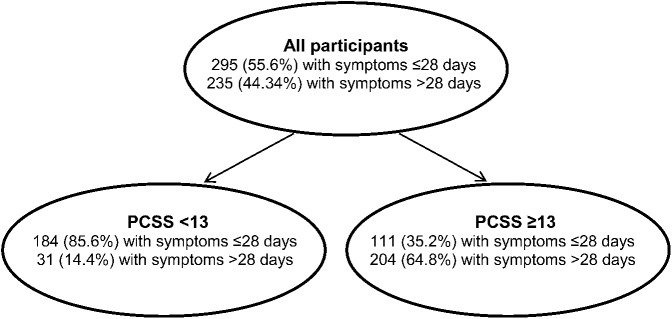
The most useful variable for distinguishing patients who had symptoms for longer than 28 days from those with shorter recoveries was Post-Concussion Symptom Scale (PCSS) score at the time of the initial visit with an optimal cutoff point of 13; those with a PCSS score of 13 or higher at their initial visit were more likely to have symptoms that lasted beyond 28 days.
Figure 2. Optimal classification and regression tree for participants who had computerized neurocognitive testing during initial visit.

The 129 patients who underwent computerized neurocognitive testing were analyzed separately to determine any added value of such testing in predicting symptom duration. Again, the most useful variable for distinguishing patients who had symptoms for longer than 28 days from those with shorter recoveries was Post-Concussion Symptom Scale (PCSS) score at the time of the initial visit. The optimal cutoff point changed slightly in this population, such that those with a PCSS score of 11 or higher at their initial visit were more likely to have symptoms that lasted beyond 28 days.
DISCUSSION
We hoped that by using multiple variables we could develop a clinical model for predicting which athletes who sustain sport-related concussions are at highest risk for prolonged symptoms beyond 28 days. Our study suggests, however, that the best predictor of prolonged symptoms after sport-related concussion is simply total symptom burden at the time of presentation. Although the cutoff point changed slightly when those participants who underwent neurocognitive testing were assessed separately, the best predictor of prolonged symptoms remained total symptom burden at the time of presentation, with computerized neurocognitive test scores having no independent association with duration of symptoms. None of the other potential predictor variables was independently associated with prolonged symptom duration. In addition, the optimal decision tree for predicting prolonged recovery did not include any other potential predictor variables. Age, amnesia, sex, history of previous concussions, and computerized neurocognitive test scores were neither independently associated with prolonged symptom duration nor useful in addition to total symptom burden for developing a predictive model.
Our study adds further evidence suggesting that the variable most important for predicting prolonged symptoms from concussion is total symptom burden. In our population, the majority (86%) of patients with a PCSS score <13 at presentation had symptoms that resolved within 28 days. In contrast, 65% of athletes with a PCSS score ≥13 at the time of their first visit had prolonged symptoms, lasting more than 28 days, compared to only 14% of those with a lower score (figure 1). When planning for the care of athletes with sport-related concussions, clinicians might provide anticipatory guidance and consider earlier introduction of therapies for those athletes with a PCSS score of 13 or higher.
Our findings are consistent with our prior work. In a smaller study, we found only initial symptom burden was independently associated with symptom duration of greater than 28 days.13 In addition, Chrisman et al.4 conducted a retrospective cohort study of athletes participating in the High School Reporting Information Online injury surveillance system. They showed that athletes who reported 4 or more symptoms after sport-related concussion had more than double the risk of having symptoms for longer than 1 week. Their results also suggested that several other variables, such as history of prior concussions, amnesia, dizziness, nausea, and difficulties with concentration, were associated with symptom duration lasting longer than 1 week for certain athletes. McCrea et al.9 also sought to determine variables associated with symptoms lasting greater than 7 days by conducting a retrospective analysis of 3 prospectively collected datasets. Their results suggested that loss of consciousness, amnesia, and higher symptom severity levels were all associated with symptoms lasting longer than 7 days postinjury. Other investigators have found that subjective fogginess, amnesia at the time of injury, dizziness at the time of injury, and neurocognitive test scores were associated with a prolonged duration of symptoms, with varying definitions for prolonged, ranging from longer than 7 days to longer than 21 days.4,9,11,12,18,29 We chose 28 days as our outcome, as have other investigators,13,30 for 2 main reasons: (1) the vast majority of athletes who sustain sport-related concussions will be symptom-free by the end of 4 weeks2,3,20,21; and (2) when athletes' symptoms persist beyond 4 weeks without substantial improvement, we start to consider changes to their management.
Our findings must be considered in light of their limitations. Our study population consisted of patients cared for in a dedicated sports concussion clinic at an academic teaching hospital. There is likely a difference between the concussions referred to such a center and those cared for in other settings such as primary care offices. This likely explains, in part, the higher proportion of patients in our sample who had symptoms beyond a month than has been observed in studies using more general samples.
The only independent predictor of prolonged symptoms after sport-related concussion appears to be overall symptom burden. For those athletes with higher symptom scale scores after a concussion, clinicians should consider anticipatory guidance and early initiation of treatment. Future models to more accurately predict the likelihood of prolonged symptoms after concussion should focus on symptom burden.
Supplementary Material
GLOSSARY
- PCSS
Post-Concussion Symptom Scale
Footnotes
Editorial, page 2196
AUTHOR CONTRIBUTIONS
Dr. Meehan contributed to the concept of the study, design of the study, data collection, data analysis, interpretation, and manuscript preparation. Dr. Mannix contributed to the concept of the study, design of the study, data analysis, interpretation, and manuscript preparation. Michael Monuteaux contributed to the design of the study, data analysis, interpretation, and manuscript preparation. Dr. Stein contributed to the data collection, data analysis, interpretation, and manuscript preparation. Dr. Bachur contributed to the concept of the study, design of the study, data analysis, interpretation, and manuscript preparation.
STUDY FUNDING
Funded by the NIH T32 HD040128-06A (Dr. Meehan) and the NFL Players Association (Dr. Meehan).
DISCLOSURE
W. Meehan receives royalties from ABC-Clio for the sale of his book, Kids, Sports, and Concussion: A Guide for Coaches and Parents and royalties from Wolters Kluwer for working as an author for UpToDate. R. Mannix, M. Monuteaux, and C. Stein report no disclosures relevant to the manuscript. R. Bachur receives royalties from Wolters Kluwer for his work as an editor for UpToDate and from Lippincott Williams & Wilkins for his work as editor of Textbook of Pediatric Emergency Medicine. His research on biomarkers for appendicitis receives industry sponsorship from Astute Medical. Go to Neurology.org for full disclosures.
REFERENCES
- 1.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA 2003;290:2556–2563. [DOI] [PubMed] [Google Scholar]
- 2.Meehan WP, III, d'Hemecourt P, Comstock RD. High school concussions in the 2008-2009 academic year: mechanism, symptoms, and management. Am J Sports Med 2010;38:2405–2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meehan WP, III, d'Hemecourt PA, Collins CL, Comstock RD. Assessment and management of sport-related concussions in United States high schools. Am J Sports Med 2011;39:2304–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chrisman SP, Rivara FP, Schiff MA, Zhou C, Comstock RD. Risk factors for concussive symptoms 1 week or longer in high school athletes. Brain Inj 2013;27:1–9. [DOI] [PubMed] [Google Scholar]
- 5.Babcock L, Byczkowski T, Wade SL, Ho M, Mookerjee S, Bazarian JJ. Predicting postconcussion syndrome after mild traumatic brain injury in children and adolescents who present to the emergency department. JAMA Pediatr 2013;167:156–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dischinger PC, Ryb GE, Kufera JA, Auman KM. Early predictors of postconcussive syndrome in a population of trauma patients with mild traumatic brain injury. J Trauma 2009;66:289–296; discussion 296–287. [DOI] [PubMed] [Google Scholar]
- 7.Eisenberg MA, Andrea J, Meehan W, Mannix R. Time interval between concussions and symptom duration. Pediatrics 2013;132:8–17. [DOI] [PubMed] [Google Scholar]
- 8.Faux S, Sheedy J, Delaney R, Riopelle R. Emergency department prediction of post-concussive syndrome following mild traumatic brain injury: an international cross-validation study. Brain Inj 2011;25:14–22. [DOI] [PubMed] [Google Scholar]
- 9.McCrea M, Guskiewicz K, Randolph C, et al. Incidence, clinical course, and predictors of prolonged recovery time following sport-related concussion in high school and college athletes. J Int Neuropsychol Soc 2013;19:22–33. [DOI] [PubMed] [Google Scholar]
- 10.Lau B, Lovell MR, Collins MW, Pardini J. Neurocognitive and symptom predictors of recovery in high school athletes. Clin J Sport Med 2009;19:216–221. [DOI] [PubMed] [Google Scholar]
- 11.Lau BC, Collins MW, Lovell MR. Sensitivity and specificity of subacute computerized neurocognitive testing and symptom evaluation in predicting outcomes after sports-related concussion. Am J Sports Med 2011;39:1209–1216. [DOI] [PubMed] [Google Scholar]
- 12.Lau BC, Collins MW, Lovell MR. Cutoff scores in neurocognitive testing and symptom clusters that predict protracted recovery from concussions in high school athletes. Neurosurgery 2012;70:371–379. [DOI] [PubMed] [Google Scholar]
- 13.Meehan WP, III, Mannix RC, Stracciolini A, Elbin RJ, Collins MW. Symptom severity predicts prolonged recovery after sport-related concussion, but age and amnesia do not. J Pediatr 2013;163:721–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCrory P, Meeuwisse W, Johnston K, et al. Consensus Statement on Concussion in Sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Br J Sports Med 2009;43(suppl 1):i76–i90. [DOI] [PubMed] [Google Scholar]
- 15.Collins MW, Field M, Lovell MR, et al. Relationship between postconcussion headache and neuropsychological test performance in high school athletes. Am J Sports Med 2003;31:168–173. [DOI] [PubMed] [Google Scholar]
- 16.Collins MW, Iverson GL, Lovell MR, McKeag DB, Norwig J, Maroon J. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med 2003;13:222–229. [DOI] [PubMed] [Google Scholar]
- 17.Iverson GL, Lovell MR, Collins MW. Interpreting change on ImPACT following sport concussion. Clin Neuropsychol 2003;17:460–467. [DOI] [PubMed] [Google Scholar]
- 18.Iverson GL, Gaetz M, Lovell MR, Collins MW. Relation between subjective fogginess and neuropsychological testing following concussion. J Int Neuropsychol Soc 2004;10:904–906. [DOI] [PubMed] [Google Scholar]
- 19.Van Kampen DA, Lovell MR, Pardini JE, Collins MW, Fu FH. The “value added” of neurocognitive testing after sports-related concussion. Am J Sports Med 2006;34:1630–1635. [DOI] [PubMed] [Google Scholar]
- 20.Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA 2003;290:2549–2555. [DOI] [PubMed] [Google Scholar]
- 21.Makdissi M, Darby D, Maruff P, Ugoni A, Brukner P, McCrory PR. Natural history of concussion in sport: markers of severity and implications for management. Am J Sports Med 2010;38:464–471. [DOI] [PubMed] [Google Scholar]
- 22.Erlanger D, Kaushik T, Cantu R, et al. Symptom-based assessment of the severity of a concussion. J Neurosurg 2003;98:477–484. [DOI] [PubMed] [Google Scholar]
- 23.Gronwall D, Wrightson P. Cumulative effect of concussion. Lancet 1975;2:995–997. [DOI] [PubMed] [Google Scholar]
- 24.Lovell MR, Collins MW, Iverson GL, et al. Recovery from mild concussion in high school athletes. J Neurosurg 2003;98:296–301. [DOI] [PubMed] [Google Scholar]
- 25.Field M, Collins MW, Lovell MR, Maroon J. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. J Pediatr 2003;142:546–553. [DOI] [PubMed] [Google Scholar]
- 26.Gordon KE, Dooley JM, Wood EP. Is migraine a risk factor for the development of concussion? Br J Sports Med 2006;40:184–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sperandi S. Understanding logistic regression analysis. Biochem Med 2013;24:12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dawson B, Trapp RG. Statistical Methods for Multiple Variables: Basic and Clinical Biostatistics, 4th ed New York: McGraw-Hill; 2004. [Google Scholar]
- 29.Lau BC, Kontos AP, Collins MW, Mucha A, Lovell MR. Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players? Am J Sports Med 2011;39:2311–2318. [DOI] [PubMed] [Google Scholar]
- 30.Zemek RL, Farion KJ, Sampson M, McGahern C. Prognosticators of persistent symptoms following pediatric concussion: a systematic review. JAMA Pediatr 2013;167:259–265. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


