Abstract
Purpose
Coronary computed tomographic angiography (CTA) is a valuable tool for assessing coronary artery disease (CAD). Although statin use is widely recommended for persons with diabetes older than age 40, little is known about the presence and severity of CAD in younger patients with diabetes mellitus (DM). We evaluated coronary artery calcium (CAC) and coronary CTA in young persons with both DM1 and DM2 in an attempt to detect the earliest objective evidence of arteriosclerosis eligible for primary prevention.
Methods and Materials
We prospectively enrolled 40 persons with DM (25 type 1 and 15 type 2) between the ages of 19 and 35 presenting with diabetes for 5 years or longer. All patients underwent coronary CTA and CAC scans to evaluate for early atherosclerotic disease. Each plaque in the coronary artery was classified as noncalcified or calcified-mixed. We also evaluated all segments with stenosis, dividing them into mild (<50%), moderate (50–70%), and severe (>70%).
Results
The average age of the DM1 subjects were 26 ± 4 (SD) years and 30 ± 4 years for DM2 patients (P < .01), with duration of diabetes of 8 ± 5 years and average HbA1c% of 8.7 ± 1.6 (norm = 4.6–6.2). Abnormal scans were present in 57.5%, noncalcified in 35% and calcified-mixed plaque in 22.5%. Persons with DM2 had a higher prevalence of positive coronary CTA scans than DM1: 80% versus 44% (P < .03) and more positive CAC scores 53% versus 4%, (P < .01). The total segment score of 2.1 ± 3.4 (P < .01) and total plaque score 1.9 ± 2.8 (P < .01) were highly correlated to each other. Plaque was almost uniformly absent below age 25, and became increasingly common in individuals over the age of 25 years for both groups. The average radiation exposure was 2.5 ± 1.3 mSv.
Conclusion
Our study verifies that early CAD can be diagnosed with coronary CTA and minimal radiation exposure in young adults with DM. A negative CAC score was not sufficient to exclude early CAD as we observed a preponderance of noncalcified plaque in this cohort. Coronary CTA in young DM patients older than age 25 may provide earlier identification of disease than does a CAC because only non-calcified plaque is frequently present. Coronary CTA provides an opportunity to consider initiation of earlier primary CAD prevention rather than waiting for the age of 40 as currently recommended by the American Diabetes Association guidelines.
Keywords: Atherosclerosis, diabetes mellitus, cardiac computed tomography, coronary calcium
Cardiovascular disease is the leading cause of death in persons with diabetes (1,2). Cholesterol-lowering therapy has been demonstrated to reduce cardiovascular events in these patients (1–7). Current lipid management strategies in individuals with diabetes target low-density lipoprotein (LDL) lowering predominantly in those older than age 40. These strategies give way to decreasing macrovascular disease and mortality, especially in those with a history of cardiovascular events (1). Studies have shown that adults with diabetes who take statins and other lipid-lowering agents are able to reduce both coronary and cerebrovascular events (2–7). There are few data to support lipid-lowering therapy (eg, statins) use in asymptomatic persons with diabetes <40 years of age. The current guidelines state that persons with diabetes <40 years without cardiovascular disease who cannot achieve lipid goals alone with lifestyle modifications, but who are at increased risk because of other cardiovascular risk factors or duration of diabetes, should consider pharmacological therapy if LDL cholesterol is >100 mg/dL (1). Noninvasive computed tomography (CT) plaque imaging is able to identify the presence and extent of noncalcified atherosclerotic plaque in obese children (8,9). Previously, high radiation doses precluded use of coronary CT angiography (CTA) in younger patients; however, significant dose-reduction techniques have led to radiation doses that are lower than annual background radiation exposure (9). We evaluated coronary artery calcium (CAC) and coronary CTA in young persons with type 1 and 2 diabetes (DM1 and DM2) in an attempt to detect evidence of arteriosclerosis eligible for primary prevention. We also looked at lipid subfractions and its association with coronary CTA plaque prevalence in persons with diabetes.
METHODS AND MATERIALS
We prospectively enrolled 40 volunteers with diabetes (25 type 1 and 15 type 2) between the ages of 19 and 35 presenting with diabetes for 5 years or longer in the South Los Angeles area. Patients were recruited from the diabetes clinic at Harbor-UCLA Medical Center and the offices of Cardiovascular Medical Group of Southern California, Beverly Hills California, after signed informed consent. All patients underwent coronary CTA and CAC scans to evaluate for early atherosclerotic disease. Lipid subfractions and CAC scores were determined for each patient. The average radiation exposure was 2.48 ± 1.3 mSv.
CAC Scanning
A 64-row multidetector CT (LightSpeed VCT, General Electric Medical System, Milwaukee, WI) was used for CAC Scanning.
64-multidetector CT Imaging Procedure
The settings of the multidetector CTwere 80 to 120kVp, 430 mA, 350 ms/per rotation with 227 ms per scan temporal resolution with 2.5-mm slice thicknesses. Electrocardiographic triggering was employed so that each image was obtained at the same point in diastole, corresponding to 75% of the RR interval. Complete coronary artery visualization was obtained without contrast medium injection, and at least 35 consecutive images were obtained at 2.5-mm intervals beginning 1 cm below the carina and progressing caudally to include the distal coronary arteries. Total radiation exposure using this technique was 0.9 mSev per patient.
CT Angiography Image Acquisition
All coronary CTA studies were performed with a 64-detector row Lightspeed VCT scanner (GE Healthcare, Milwaukee, WI). All patients were in normal sinus rhythm at the time of the coronary CTA scan. Individuals with heart rates above 65 pre-treated with up to 100 mg of metoprolol several hours before the procedure and were also administered intravenous metoprolol at 5-mg increments to a total possible dose of 25 mg in order to achieve a resting heart rate <65 beats/min. All patients eligible for coronary CTA were scanned, irrespective of whether the goal <65 beats/min heart rate was achieved.
After a scout radiograph of the chest, a timing bolus was performed to detect time to optimal contrast opacification in the axial image at a level immediately superior to the ostium of the left main artery. During coronary CTA acquisition, 60 mL of iodinated contrast (Visipaque, GE Healthcare, Milwaukee, WI) was injected using a triple-phase contrast protocol: 40 mL iodixanol, followed by 40 mL of a 50:50 mixture of iodixanol and saline, followed by a 50-mL saline flush. Prospective electrocardiogram-triggered contrast-enhanced CTA was performed, with scan initiation 20 mm above the level of the left main artery to 20 mm below the inferior myocardial apex. The scan parameters were 64 × 0.625-mm collimation, tube voltage 100–120 mV and effective mA 350–780 mA (depending on body habitus).
Coronary CTA Interpretation
CTA images were interpreted by one reader (M.B.) blinded to all patient characteristics. All CT angiography images were evaluated on three-dimensional image analysis workstation (GE Advantage Workstation, GE Healthcare, Milwaukee, WI) as previously described (10). CTA reader was permitted to use any or all of available postprocessing image reconstruction algorithms, including two-dimensional axial, or three-dimensional maximal intensity projection, multiplanar reformat, cross-sectional analysis, or volume-rendered technique. Coronary arteries were scored using a 15-segment AHA coronary artery classification. An overall assessment of image quality and coronary supply dominance was performed on the subject level. A semiquantitative scale was employed by coronary CTA readers to grade degree of luminal stenosis as a percentage of the vessel diameter. Stenosis severity was recorded in the following manner: no stenosis; ≤29% stenosis; 30% to 49% stenosis; 50% to 69% stenosis; 70% to 100% stenosis.
Plaque Severity Score
All images were used to evaluate each segment on the basis of plaque type, amount of plaque, and severity of stenosis (10). Plaque was evaluated from both axial source images and multi-planar reformat images of the long axis at each segment of the coronary arteries. A total plaque score was developed to semi-quantitate the plaque in each participant with the use of the 15-segment AHA SCCT model of the coronary arteries. Each plaque was assigned a score of 1 when plaque volume was small, 2 for medium plaque volume, and 3 for large plaque volume. The total plaque severity score per person was determined by summing the number of interpretable coronary segments (maximum of 18 segments) with individual plaque scores (range 1–3).
Segment Stenosis Scoring
Segments were graded as normal (no stenosis), stenosis 1%–29%, 30%–49%, 50%–69%, ≥70% by visual semiquantification method, with assignment of scores of 0, 1, 2, 3, or 4, respectively. Stenosis was not measured when the vessel diameter was ≥2 mm. Segment stenosis score per person was calculated by summing all the 15 individual segments with a possible score ranging from 0 to 60.
RESULTS
Persons with DM1 were younger than those with DM2 (26 ± 4 [SD] years vs. 30 ± 4 years, P < .01). The average HbA1c% was 8.7 ± 1.6 (norm = 4.6–6.2) and average duration of diabetes was 8 ± 5 years. Abnormal scans were present in 23 persons with diabetes, noncalcified in 14 and calcified-mixed plaque in 9. Plaque prevalence by coronary CTA was higher among DM2 vs. DM1 (80% vs. 44%, P < .03) and more DM2 had positive CAC scores (53% vs. 4%, P < .01). The total segment score of 2.1 ± 3.4 units (P < .01) and total plaque score 1.9 ± 2.8 units (P < .01) were highly correlated to each other (r = 0.99). Plaque was seen in 8% of those younger than age 25 was seen in 50% of those diabetes patients older than age of 25 years. High-density lipoprotein subfraction 2, triglycerides, very-low density lipoprotein 3, and C-reactive protein were all significantly higher among persons with DM2 versus DM1 (Table 1). Using advanced lipid testing, we analyzed patterns of cholesterol. The LDL subfraction pattern with increased levels of the small dense LDL (type B), whereas the less atherogenic larger particle predominance was described as type A. Among DM1, only 7 (28%) were type B LDL pattern on advanced lipid testing, whereas 11/15 (73%) were type B among DM2 (P < .01). There was a significant increase in the presence of any CAD (odds ratio 3.3, confidence interval 1.31 to 8.13, P < .05) and obstructive CAD (=50%, odds ratio 2.9, confidence interval 1.16 to 7.28, P < .05) in the group with increased triglyceride level and waist circumference (Table 1).
TABLE 1.
Demographics of Study Population in Relation to Type I and II Diabetes
| Variable | Type I Diabetes (n = 25) | Type II Diabetes (n = 15) | P Value |
|---|---|---|---|
| Age | 26 ± 4 y | 30 ± 4 yrs | <.01 |
| Glucose | 206.9 ± 86.7 mg/dL | 175.3 ± 85.8 mg/dL | >.01 |
| HgA1c% | 9.0 ± 1.3% | 7.9 ± 2.1% | >.01 |
| Triglycerides | 107.2 ± 107.6 mg/dL | 192.5 ± 165.1 mg/dL | <.06 |
| HDL2 | 14.5 ± 9.2 mg/dL | 9.5 ± 5.1 mg/dL | <.05 |
| VLDL3 | 10.5 ± 2.4 mg/dL | 13.0 ± 4.1 mg/dL | <.05 |
| Hs-CRP | 3.6 ± 7.1 mg/L | 19.3 ± 27.0 mg/L | <.05 |
HDL, high-density lipoprotein; HsCRP, high-sensitivity C-reactive protein; HgAIC, hemoglobin A1c; VLDL, very low density lipoproteins.
DISCUSSION
Our study was able to identify plaque in 50% of persons with diabetes using coronary CTA, especially DM2 over the age of 25. Several studies have been conducted studying the effects of diabetes on the cardiovascular system, but very few have been done in patients younger than 35 years of age. A study conducted in Nova Scotia concluded that changes in the heart and blood vessels to adapt to exercise may be impaired early after the onset of DM2. Magnetic resonance imaging scans revealed that during exercise, the hearts of teens with DM2 exhibited filling abnormalities (11). Most available data on coronary plaque are based on studies in patients older than 40 years old. These studies demonstrate that plaque is much more common in persons with DM and that the amount of plaque (both calcified or noncalcified) is significantly greater than in the general population (12–15). A study by Scholte et al showed that shown that noncalcified plaques were the most common type of plaque found in asymptomatic DM patients who underwent CTAs (16). In another study by Lin et al consisting of 1024 subjects, 135 had diabetes, and 334 had metabolic syndrome. These subjects with diabetes and those with metabolic syndrome had a higher prevalence of noncalcified, calcified, and mixed-type plaques and stenosed coronary segments than the subjects with neither condition (P < .05). The odds ratios for diabetes and the presence of any plaque, mixed plaque, calcified plaque, and stenosed segment compared with neither metabolic syndrome nor diabetes were 2.89, 3.63, 2.10, and 2.04, respectively, all of which were significant (P < .05) (17). A study by Makino et al showed similar results, also in older DM patients. Calcified plaques were more frequent in patients with hypertension (P = .02), and patients with calcified plaques also had significantly lower low-density lipoprotein cholesterol levels (P < .001). Soft plaques (Fig 1) were more frequent in patients with dyslipidemia (P < .001). Patients with soft plaques had significantly higher low-density lipoprotein cholesterol levels (P = .02) and lower high-density lipoprotein cholesterol levels (P < .001) (18).
Figure 1.
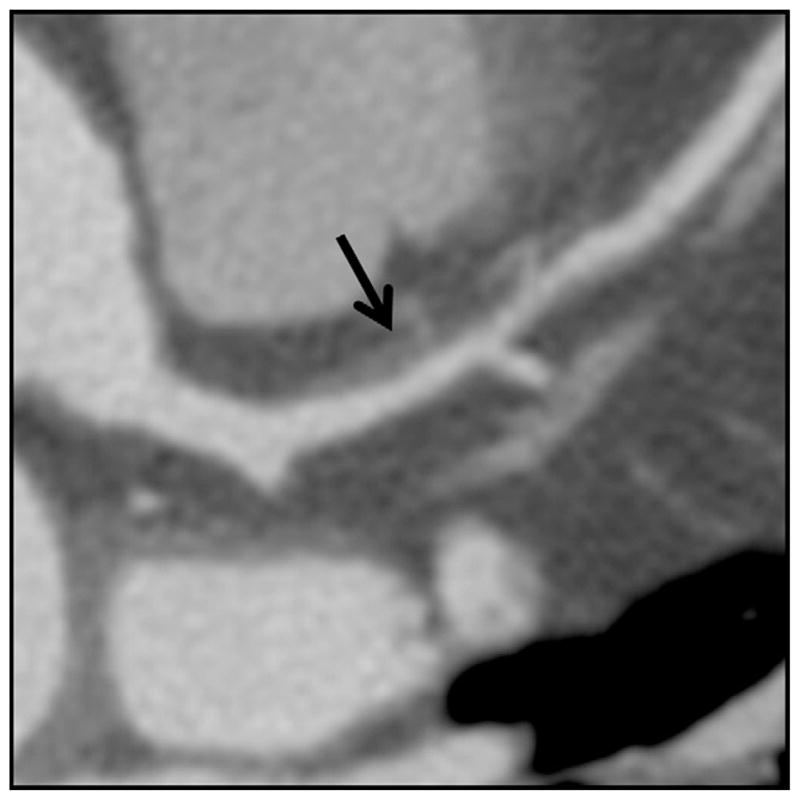
A large noncalified plaque (arrow) in the proximal left anterior descending artery.
It is important to note that these plaques generally begin to form at such a young age and can go undetected for many years before becoming symptomatic or causing injury. This may be exacerbated among persons with DM2, because silent ischemia is thought to be a considerable challenge. A study by Rivera et al. studied 906 individuals with and without DM (mean age 49 ± 9 years, 62% males); 19 and 9% of the population had any and two or more segments with coronary plaque, respectively. Unadjusted analysis showed a positive association between increasing levels of HbA1c and the number of coronary segments with any (P < .001) and with mixed coronary plaques (P < .0001). The association persisted even when traditional risk factors were taken into account (19). In a study by de Graaf et al, the researchers found a relationship between increased waist circumference and increased plasma triglyceride levels and the number of noncalcified and mixed plaques (20). Most of the risk factors found to predict coronary CTA defined plaque as amenable to lifestyle or pharmacologic therapy. Because medical management can aid in the prevention of plaque progression and cardiovascular events, early detection is key (21–23).
Limitations
Some of the limitations to our study are the small sample size. Our study is biased toward the young diabetes patients with severe disease as characterized by duration of disease, early onset and the HaIc. Similar studies are needed to be conducted across less severe disease and also across various ethnic and socioeconomic groups of similar age ranges to further validate these results. Although safety and low radiation doses have been well established for coronary CTA (24–26), technical limitations that preclude use of coronary CTA include inadequate heart rate control (atrial fibrillations, premature ventricular complexes), heavy calcification making segments uninterpretable, and need for contrast in patients with renal insufficiency although newer techniques are challenging these limitations.
CONCLUSION
Our study identifies that a significant number of persons with DM1 and DM2 below the age of 40 have identifiable plaque and that coronary CTA can be employed safely and with minimal radiation exposure in young persons with diabetes. Although a negative CAC score implies a very low event rate, in this young population CAC did not exclude early arteriosclerosis as we observed a preponderance of non-calcified plaque in this cohort (23). Coronary CTA in young persons with DM provides earlier identification of disease than does a CAC scan, because isolated noncalcified plaque is present in approximately one third of these young patients. A positive coronary CTA in young persons with diabetes provides an opportunity to consider earlier initiation of primary CAD prevention (eg, lifestyle management, aspirin use, statin therapy) rather than waiting for the age of 40 as is currently recommended.
Acknowledgments
This study was supported by an unrestricted grant from the Cardiovascular Research Foundation of Southern California, Beverly Hills, California (CVRF).
References
- 1.Position statements. Diabetes Care. 2010;33:S100. [Google Scholar]
- 2.Pyorala K, Pedersen TR, Kjekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) Diabetes Care. 1997;20:614–620. doi: 10.2337/diacare.20.4.614. [DOI] [PubMed] [Google Scholar]
- 3.Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 4.Collins R, Armitage J, Parish S, et al. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet. 2003;361:2005–2016. doi: 10.1016/s0140-6736(03)13636-7. [DOI] [PubMed] [Google Scholar]
- 5.Frick MH, Elo O, Haapa K, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987;317:1237–1245. doi: 10.1056/NEJM198711123172001. [DOI] [PubMed] [Google Scholar]
- 6.Rubins HB, Robins SJ, Collins D, et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial Study Group. N Engl J Med. 1999;341:410–418. doi: 10.1056/NEJM199908053410604. [DOI] [PubMed] [Google Scholar]
- 7.Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 8.Hausleiter J, Meyer T, Hadamitzky M, et al. Prevalence of noncalcified coronary plaques by 64-slice computed tomography in patients with an intermediate risk for significant coronary artery disease. J Am Coll Cardiol. 2006;48:312–318. doi: 10.1016/j.jacc.2006.02.064. [DOI] [PubMed] [Google Scholar]
- 9.Hoffmann U, Butler J. Noninvasive detection of coronary atherosclerotic plaque by multidetector row computed tomography. Int J Obes (Lond) 2005;29(Suppl 2):S46–S53. doi: 10.1038/sj.ijo.0803083. [DOI] [PubMed] [Google Scholar]
- 10.Pagali SR, Madaj P, Gupta M, et al. Interobserver variations of plaque severity score and segment stenosis score in coronary arteries using 64 slice multidetector computed tomography: a substudy of the ACCURACY trial. J Cardiovasc Comput Tomogr. 2010;4:312–318. doi: 10.1016/j.jcct.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Berry C, Sattar N. Stressed hearts in children with obesity and diabetes: a cause for concern? Diabetologia. 2011;54:715–718. doi: 10.1007/s00125-010-2041-0. [DOI] [PubMed] [Google Scholar]
- 12.Aldrovandi A, Maffei E, Seitun S, et al. Major adverse cardiac events and the severity of coronary atherosclerosis assessed by computed tomography coronary angiography in an outpatient population with suspected or known coronary artery disease. J Thorac Imaging. 2012;27:23–28. doi: 10.1097/RTI.0b013e3181f55d0d. [DOI] [PubMed] [Google Scholar]
- 13.Choi EK, Chun EJ, Choi SI, et al. Assessment of subclinical coronary atherosclerosis in asymptomatic patients with type 2 diabetes mellitus with single photon emission computed tomography and coronary computed tomography angiography. Am J Cardiol. 2009;104:890–896. doi: 10.1016/j.amjcard.2009.05.026. [DOI] [PubMed] [Google Scholar]
- 14.Maffei E, Seitun S, Nieman K, et al. Assessment of coronary artery disease and calcified coronary plaque burden by computed tomography in patients with and without diabetes mellitus. Eur Radiol. 2011;21:944–953. doi: 10.1007/s00330-010-1996-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chu ZG, Yang ZG, Dong ZH, et al. Characteristics of coronary artery disease in symptomatic type 2 diabetic patients: evaluation with CT angiography. Cardiovasc Diabetol. 2010;9:74. doi: 10.1186/1475-2840-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scholte AJ, Schuijf JD, Kharagjitsingh AV, et al. Prevalence of coronary artery disease and plaque morphology assessed by multi-slice computed tomography coronary angiography and calcium scoring in asymptomatic patients with type 2 diabetes. Heart. 2008;94:290–295. doi: 10.1136/hrt.2007.121921. [DOI] [PubMed] [Google Scholar]
- 17.Lin T, Liu JC, Chang LY, et al. Association of metabolic syndrome and diabetes with subclinical coronary stenosis and plaque subtypes in middle-aged individuals. Diabet Med. 2011;28:493–499. doi: 10.1111/j.1464-5491.2010.03213.x. [DOI] [PubMed] [Google Scholar]
- 18.Makino K, Yoshitama T, Kanda S, et al. Relation of coronary plaque composition determined by 64-slice multidetector computed tomography in patients with suspected coronary heart disease. Am J Cardiol. 2011;107:1624–1629. doi: 10.1016/j.amjcard.2011.01.047. [DOI] [PubMed] [Google Scholar]
- 19.Rivera JJ, Choi EK, Yoon YE, et al. Association between increasing levels of hemoglobin A1c and coronary atherosclerosis in asymptomatic individuals without diabetes mellitus. Coron Artery Dis. 2010;21:157–163. doi: 10.1097/MCA.0b013e328337ff9b. [DOI] [PubMed] [Google Scholar]
- 20.de Graaf FR, Schuijf JD, Scholte AJ, et al. Usefulness of hypertriglyceridemic waist phenotype in type 2 diabetes mellitus to predict the presence of coronary artery disease as assessed by computed tomographic coronary angiography. Am J Cardiol. 2010;106:1747–1753. doi: 10.1016/j.amjcard.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 21.Price HC, Tucker L, Griffin SJ, et al. The impact of individualised cardiovascular disease (CVD) risk estimates and lifestyle advice on physical activity in individuals at high risk of CVD: a pilot 2 x 2 factorial understanding risk trial. Cardiovasc Diabetol. 2008;7:21. doi: 10.1186/1475-2840-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Budoff MJ, Nasir K, Katz R, et al. Thoracic aortic calcification and coronary heart disease events: the multi-ethnic study of atherosclerosis (MESA) Atherosclerosis. 2011;215:196–202. doi: 10.1016/j.atherosclerosis.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Budoff MJ, McClelland RL, Nasir K, et al. Cardiovascular events with absent or minimal coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Am Heart J. 2009;158:554–561. doi: 10.1016/j.ahj.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi TY, Malpeso J, Li D, et al. Radiation dose reduction with increasing utilization of prospective gating in 64-multidetector cardiac computed tomography angiography. J Cardiovasc Comp Tomogr. 2011;5:264–270. doi: 10.1016/j.jcct.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 25.Gopal A, Mao SS, Karlsberg D, et al. Radiation reduction with prospective ECG-triggering acquisition using 64-multidetector computed tomographic angiography. Int J Cardiovasc Imaging. 2009;25:405–416. doi: 10.1007/s10554-008-9396-z. [DOI] [PubMed] [Google Scholar]
- 26.Bell GW, Edwardes M, Dunning AM, et al. Periprocedural safety of 64-detector row coronary computed tomographic angiography: results from the prospective multicenter ACCURACY trial. J Cardiovasc Comput Tomogr. 2010;4:375–380. doi: 10.1016/j.jcct.2010.08.003. [DOI] [PubMed] [Google Scholar]


