Abstract
Objective
Although young women often report smoking for weight control purposes, no prospective study has tested whether smokers subsequently gain less weight over time than non-smokers. As this is an important lacuna because smoking results in greater mortality than obesity, the present study addresses this question.
Method
Female college students (N = 398; M age=18.4, SD=0.6; M BMI=23.7, SD=4.3) recruited for a body acceptance intervention trial provided data on smoking behavior and had their body mass measured at baseline and at 1-mo, 6-mo, 1-yr, and 2-yr follow-ups.
Results
Counter to the belief that smoking is an effective weight control strategy, baseline smokers (n = 29) gained significantly more weight (r = .29) than baseline non-smokers (n = 304), controlling for baseline BMI, parental obesity status, socioeconomic status, and intervention condition; over 2-yr follow-up smokers gained 2.9 kg versus 0.9 kg for non-smokers. Descriptive data indicated that weight gain was greater for young women who quit smoking during follow-up (n = 13; M = 4.8 kg) than for persistent smokers (n = 16; M = 1.4 kg), though both groups gained more weight than non-smokers.
Conclusions
Results challenge the widely held belief that smoking is an effective weight control strategy, ironically suggesting that smokers gain more weight than non-smokers during young adulthood, though non-experimental prospective studies do not establish causal relations and future research with larger representative samples is needed.
Keywords: young adults, smoking, smoking cessation, weight gain
Introduction
Although obesity is the second leading cause of premature death, smoking is the first (Hennekens & Andreotti, 2013; Mokdad, Marks, Stroup, & Gerberding, 2004). Ironically given these statistics, individuals often report smoking cigarettes for weight control purposes, particularly young women (Boles & Johnson, 2001; White, 2012). Prospective studies have confirmed that weight concerns significantly increase risk for future onset of smoking among adolescent girls (Harakeh, Engles, Monshouwer, & Hanssen, 2010; Stice & Shaw, 2003).
Prospective repeated-measures studies indicate that adults who show persistent smoking gain less weight over time than persistent non-smokers (e.g., Klesges et al., 1998; Mozaffarian, Hao, Rimm, Willett, & Hu, 2011; Rasmussen, Tynelius, & Kark, 2003), but we were unable to locate any prospective studies that tested whether baseline smokers show significantly less future weight gain than non-smokers followed over the same period. This is important because by excluding individuals who quit smoking during the follow-up, the repeated measures studies may produce misleading information about whether smoking is associated with significant reductions in future weight gain. Given that many smokers quit on a lasting or temporary basis, and smoking cessation has been consistently associated with subsequent weight gain (Dennis et al., 2000; Flegal et al., 1995; Klesges et al., 1998; Williamson et al., 1991), excluding those who quit or attempt to quit may erroneously suggest that smokers are at lower risk for future weight gain. We therefore think it important to test whether baseline smokers gain less weight over time than baseline non-smokers, as the results could have significant public health implications.
It is particularly important to investigate this research question among female college students because they are much more likely to report smoking for weight control purposes than other populations (Klesges et al., 1998), the smoking rate for college students is 66% higher than that of the general population (Centers for Disease Control and Prevention, 2009; Rigotti, Lee, & Wechsler, 2000), and few studies have investigated this population (Simmons & Brandon, 2007). Indeed, young adults aged 18-24 represent the age group with the highest smoking prevalence in the US (Freedman, Nelson, & Feldman, 2012). Thus, the aim of this report was to test whether female college students who reported smoking at baseline gained less weight over time relative to their non-smoking counterparts.
Materials and Methods
Participants and Procedures
Participants were 398 young women (M age=18.4, SD=0.6; M BMI=23.7, SD=4.3; 83% European American, 8% Latino, 7% Asian, 2% African American) recruited from a university using mailings, flyers, and leaflets inviting freshman women with body image concerns to participate in a trial evaluating two body acceptance interventions; university enrollment, female sex, and body image concerns constituted the inclusion criteria. Potential participants were excluded if they met current diagnostic criteria for anorexia nervosa (AN), bulimia nervosa (BN), or binge eating disorder (BED) because the goal of this trial was to assess whether the Healthy Weight 2 intervention prevented eating disorder onset. The Eating Disorder Diagnostic Interview was used to assess these exclusion criteria; DSM-IV eating disorder diagnoses have shown inter-rater reliability (κ = .86), 1-week test-retest reliability (κ = .96), and sensitivity to detecting effects of eating disorder prevention programs (Stice, Mari, Shaw, & Jaconis, 2009; Stice, Rohde, Shaw, & Marti, 2012). The University of Oregon and Oregon Research Institute IRBs approved this study. Participants provided written informed consent. Participants were randomly assigned to the 4 1-hour session Healthy Weight 2 group-based eating disorder/obesity prevention program or an educational brochure control condition, providing interview and survey data at baseline and at 1-mo, 6-mo, 1-yr, and 2-yr follow-ups. See Stice and colleagues (2012) for details about random assignment, content of the Healthy Weight 2 intervention and the educational brochures, facilitator training and supervision, assessor training, quality assurance, and participant compensation.
Measures
Smoking
A smoking composite score was computed as the product of smoking frequency and smoking quantity based on items from (Johnston, O'Malley, & Bachman, 2000). Smoking frequency was assessed by an item that asked participants how many times of the past year they smoked, with the following response categories: Never, A few times, Less than monthly, 1-3 times a month, 1-2 times a week, 3-4 times a week, and 5-7 times a week. Smoking quantity was measured by an item that asked participants approximately how many cigarettes they smoked daily, with the following response options: 0, 1-2, 3-8, 9-14, 15-20, and 21 or more. Each measure was coded as an ordinal variable beginning with zero. These items have shown 1-month test retest reliability (r = .91 & .92 respectively; Stice & Shaw, 2003) and predictive validity for attenuated physical growth (Stice & Martinez, 2005). More generally, self-reported use of nicotine products in research studies has shown high agreement with serum cotinine, an indicator of nicotine exposure (e.g., < 1% reporting no nicotine use had positive test for cotinine, Yeager & Krosnick, 2010).
Parental obesity
Participants were asked whether either their biological mother or father were currently obese; the weight thresholds for obesity for women and men of average height were provided as reference points. Participants who reported that one or both of their biological parents were overweight or obese were coded as positive on this dichotomous variable (1 = yes and 0 = no). Self-report versions of these items have shown adequate temporal reliability (1-year test-retest reliability = .68) and reasonable concordance (72% overall agreement) with parental self-report of obesity (Stice, Presnell, Shaw et al., 2005).
Parental Education
Participants indicated the highest level of education for each of their parents from the following categories: grade school graduate, some high school, high school graduate, some college, college graduate, and advanced degree to serve as a proxy measure for socioeconomic status. Education levels were coded as an ordinal variable and averaged across parents.
Body mass
BMI was computed as weight in kilograms divided by meters squared. After removal of shoes and coats, weight to the nearest 0.1 kg was obtained using a digital scale and height was obtained to the nearest millimeter using a stadiometer. Two measures of height and weight were obtained at each assessment and averaged in an effort to enhance accuracy. BMI has been shown to correlate with direct measures of body fat such as dual energy x-ray absorptiometry (r = .80 – .90) and health measures such as blood pressure, adverse lipoprotein profiles, and diabetes mellitus (Pietrobelli et al., 1998). As part of a validation study (Stice, Durant, Burger, & Schoeller, 2011), a proportion of the sample provided data on weight-related constructs of estimated total daily energy intake (using doubly labeled water) and resting metabolic rate (using air displacement plethysmography [BodPod] and indirect calorimetry [TrueOne 2400 Metabolic Measurement System]).
Data analysis
We implemented linear mixed effects models, which accommodate multilevel data structures, using HLM 6.06 with robust standard errors (Raudenbush et al., 2004) to examine change in BMI across the follow-up period. Linear mixed models also accommodate unevenly spaced longitudinal data (Hox, 2010) and missing data by precision weighting the impact of participants relative to the number of observations they provide (Raudenbush & Bryk, 2002). We fit the model following recommendations for longitudinal model building from Singer and Willett (2003). We initially examined the best model of longitudinal change by comparing linear and nonlinear models of BMI change, ultimately determining that the linear model, in which time was coded as the number of months from the baseline assessment, was equivalent to or better than log-linear and quadratic models of change using criteria for evaluating model Akaike Information Criterion (AIC) following recommendations from Burnham and Anderson (2002). After establishing the model of longitudinal change, we added person-level covariates, including intervention condition, parental obesity, parental education, race (dummy coded as Hispanic, Native American, Asian American or Pacific Islander, African American versus European American), and baseline BMI, as well as the effects of greatest theoretical interest: baseline smoking composite and the interaction between the baseline smoking composite and time. The model contained a random intercept that reflects the variability in BMI at baseline. Models included only participants that indicated that they had non-zero values for both smoking quantity and smoking frequency (n = 29) and participants that did not smoke at baseline, 1-year, and 2-year follow-ups (n = 304); participants that initiated smoking after baseline (n = 18) or did not respond to smoking items (n = 47) were excluded from all analyses.
We assessed the possibility that individual participants exerted disproportionate influence by computing Cook's distance for each participant with the requirement that values should be less that the 50th percentile of the F distribution (Kutner, Nachtsheim, Neter, & Li, 2005). We estimated effect sizes for terms in the model by converting t values to Pearson's r (Lipsey & Wilson, 2001). We also tested the possibility that baseline smoking status moderated the effects of the obesity prevention program on change in outcomes by adding a time x condition x baseline smoking status interaction and all implied lower order terms for all outcomes.
Results
There were 29 smokers included in the analysis. Among baseline smokers, 17% reported smoking less than weekly, 34% reported smoking more than weekly, and 48% reported smoking daily or near daily; 55% reported usage of 1-2 cigarettes per smoking day, 24% reported 3-8 cigarettes per smoking day, and 21% reported 9 cigarettes or more per smoking day. Baseline smokers exhibited higher baseline BMIs (M = 25.07, [SD = 5.80]) than non-smokers (M = 23.47, [SD = 3.94]) (t[331] = 2.00, p = .047). Resting metabolic rate obtained from the BodPod, which exhibited strong agreement with resting metabolic rate obtained from a metabolic cart in a subsample (r = .82, p < .001, n = 68), was higher for baseline smokers (M = 1262.4 [SD = 180.6], n = 20) than baseline non-smokers (M = 1193.8 [SD = 152.0], n = 243), though the difference was only a marginal trend (t [261] = 1.91, p = .057, d = 0.41). A comparison of doubly labeled water estimated total daily energy intake in a randomly selected subsample indicated that baseline smokers (M = 2454.4 [SD = 507.0], n = 6) and baseline non-smokers (M = 2576.0 [SD = 455.6], n = 68) did not exhibit significant differences (t [72] = 0.62, p = .536, d = −0.11). There were no differences in the number of smokers in each arm of the trial (χ2[1] = 0.39, p = .349).
Model results are reported in Table 1. There was a significant effect for the parameter of primary interest, the smoking-by-months interaction (t[1508] = 2.12, p = .034, r = .12), which represented a small effect size. Unexpectedly, the positive effect indicated that greater levels of smoking were associated with larger increases in BMI over the 2-year follow-up period. Assessment of the model indicated that all participants fell below the outlier criterion and random intercepts, evaluated using a QQ plot, adhered to a normal distribution. On average smokers gained 1.1 BMI units (SD = 3.0, 95% CI [−0.1, 2.2]) and 2.9 kg (SD = 7.9, 95% CI [0.0, 5.8]) over follow-up. In contrast, baseline non-smokers gained 0.2 BMI units (SD = 1.6, 95% CI [0.0, 0.4]) and 0.9 kg (SD = 4.3, 95% CI [0.4, 1.4]) over follow-up. Examination of smoking as a moderator of intervention effects indicated that there was not a significant time x condition x smoking interaction for BMI (t[1505] = 1.28, p = .203).
Table 1.
Model coefficients
| B | SE | df | t | p | r | |
|---|---|---|---|---|---|---|
| Intercept | 0.35 | 0.46 | 299 | 0.76 | .449 | .04 |
| Baseline BMI | 0.98 | 0.02 | 299 | 56.16 | <.001 | .95 |
| Healthy Weight intervention | 0.00 | 0.08 | 299 | 0.02 | .986 | .00 |
| Parental obesity | −0.04 | 0.12 | 299 | −0.35 | .729 | −.02 |
| Parental education | 0.04 | 0.04 | 299 | 0.90 | .368 | .05 |
| Hispanic | 0.30 | 0.17 | 299 | 1.75 | .080 | .10 |
| Native American | −0.53 | 0.18 | 299 | −2.88 | .005 | −.16 |
| Asian or Pacific Islander | 0.17 | 0.22 | 299 | 0.76 | .450 | .04 |
| African American | −0.25 | 0.56 | 299 | −0.45 | .650 | −.03 |
| Baseline smoking | 0.00 | 0.01 | 299 | 0.13 | .895 | .01 |
| Months | 0.01 | 0.00 | 1508 | 1.47 | .142 | .08 |
| Baseline smoking × months | 0.01 | 0.00 | 1508 | 2.12 | .034 | .12 |
Given that the direction of the effect was opposite of what would be expected if smoking were an effective weight control procedure, we examined whether this effect was driven by excess weight gain exhibited by the subset of baseline smoking participants who quit smoking during the follow-up, as cessation has been associated with subsequent weight gain. Because of the small cell sizes involved, we present these data for descriptive purposes, and refrained from conducting inferential tests. Figure 1 displays BMI for non-smokers and among baseline smokers that we classified as either persistent smokers (n = 16) if they smoked at all three time points or quitters (n = 13) if they reported not smoking at either 1-year or 2-year follow-up. Smokers who quit smoking gained 4.8 kg (SD = 9.4, 95% CI [−0.4, 9.9]), relative to smokers who did not quit, who gained 1.4 kg (SD = 6.4, 95% CI [−1.7, 4.5]), and non-smokers, who gained 0.9 kg (SD = 4.3, 95% CI [0.4, 1.4]).
Figure 1.
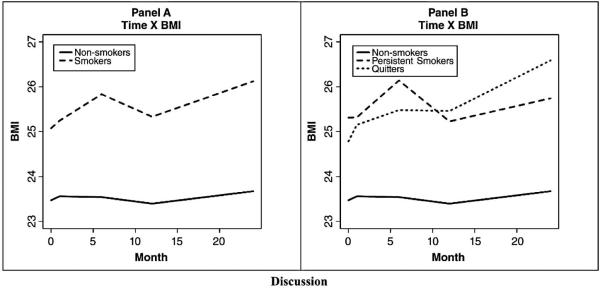
In panel A, raw values of BMI for non-smokers and baseline smokers; In panel B, raw values of BMI at each measurement occasion for (a) non-smokers, (b) persistent smokers, and (c) participants who quit at some point after baseline.
Discussion
Contrary to the notion that cigarette smoking is an effective weight control strategy, results suggested that smokers gained significantly more weight over 2-year follow-up than non-smokers (M = 2.9 kg vs. M = 0.9 kg, respectively). Although descriptive data suggested that baseline smokers who quit gained more weight than those who persisted in their smoking (M = 4.8 kg vs. M = 1.4 kg respectively), both groups gained more weight than baseline non-smokers (M = 0.9 kg), though small cell sizes prevented us from estimating inferential tests. The fact that smokers who quit gained more weight than those who did not in the present sample converges with repeated-measures studies that have found that adults who quit smoking gain more weight over follow-up than persistent smokers (Dennis et al., 2000; Flegal et al., 1995; Klesges et al., 1998; Williamson et al., 1991), implying that our findings from this sample of young women with body image concerns may generalize more broadly. One novel aspect of the present data is that the average frequency and quantity of smoking was relatively low, as has been observed in other studies of college student smokers (Simmons & Brandon, 2007), suggesting that even relatively light smoking may be associated with subsequent weight gain.
Despite the fact that this study used a prospective design, which permits firmer inferences than cross-sectional studies because temporal precedence is established, it is always possible that some confound explains the relation between the independent and the dependent variable. Interestingly, the present results extend prior prospective studies that have found that people who engage in a variety of weight control behaviors, such as dietary restriction of caloric intake, appetite suppressant/laxative use, vomiting for weight control, and exercise for weight control show greater future weight gain than those who do not engage in these behaviors (e.g., Chaput, Leblanc, Perusse, Despres, Bouchard, & Tremblay, 2009; Field et al., 2003; Stice, Cameron, Killen, Hayward, & Taylor, 1999). This broader pattern of findings imply that it is possible that individuals who struggle with weight control may resort to various behaviors to curb overeating, but that these behaviors are not able to offset the effects of overeating on future weight gain. Regardless, the evidence that smokers gain more weight over a 2-year follow-up period than non-smokers may help debunk the unhealthy belief that smoking is an effective weight control strategy, which is vital given that smoking is still responsible for more preventable deaths than obesity (Mokdad et al., 2004).
The evidence that smokers had significantly higher body mass at baseline than non-smokers is generally consistent with the notion that many of the participants may have been engaging in smoking for weight control purposes, though we did not directly assess smoking intentions. It could also be that smokers are less healthy in multiple regards relative to non-smokers. In this context it is important to note that because we controlled for baseline BMI, it is unlikely that elevated initial body mass is a third variable that explains the positive relation between baseline smoking status and elevated future weight gain.
Detractors may argue that the finding that smokers who quit gained more weight than those who did not suggests that smoking is an effective weight control strategy. Indeed, epidemiologic studies on the predictors of weight gain indicate that smoking cessation is often the most potent predictor of future weight gain (Kahn et al., 1997; Koh-Banerjee et al., 2003; Mozaffarian et al., 2011; O'Hara et al., 1998). However, the fact that smokers who did not quit gained more weight than non-smokers, and certainly did not lose weight, offers little support for this interpretation. It is important from a public health standpoint to note that 45% of the smokers at baseline reported quitting over the 2-year follow-up in the present sample. In aggregate, the present findings imply that young women who smoke, potentially for weight control purposes, will weigh more than those who do not smoke several years later. The present data suggest that if a young woman starts smoking in adolescence, she will tend to gain 2.9 kg in college over a 2-year period instead of 0.9 kg, and she has a 45% chance of quitting smoking.
It is important to consider the limitations of this study when interpreting the findings. First and foremost, it will be vital to replicate the present findings using data from larger more representative samples. Nevertheless, the model's results appear to be stable in the present sample as evidenced by the fact that we used robust estimation for all models, numerous covariates that could viably account for weight gain did not impact the finding, and there was no evidence that outliers disproportionately influenced the model. Second, the present sample was composed solely of female college students with body dissatisfaction, which limits generalizability of the findings. However, the fact that we were able to replicate previous evidence that smoking cessation was associated with greater weight gain than persistent smoking suggests that the findings may generalize. Third, lack of data on smoking intentions was a limitation to study interpretations, although the requirement that participants have body dissatisfaction may have increased the likelihood that smokers were doing so for weight control purposes. Fourth, only 17% of the present sample reported being from minority ethnic groups, suggesting that findings should be generalized with care to more ethnically diverse populations. Fifth, because we did not confirm smoking status and non-smoking status biologically, it is possible that some individuals who reported not smoking did actually smoke and vice versa, which would have reduced the magnitude of effects. Finally, as noted, because smoking status was not manipulated experimentally, no causal inferences from these data are possible, as some confound may explain the prospective relations, such as psychiatric comorbidity.
Conclusions
The present findings challenge the widely held belief that smoking is an effective weight control strategy, instead suggesting that after 2-years, young women who smoke will weigh more than those who do not. Although the present data suggest that baseline smokers who quit gained more weight than baseline smokers who did not, descriptive data imply that both gained more weight than non-smoking young women. The finding that a high proportion of this sample of young adult smokers quit over a 2-year period implies that many young women who smoke may experience marked weight gain secondary to subsequent quit attemps, suggesting that it is ill advised to turn to smoking for weight control purposes.
Highlights.
Conducted first prospective test of whether smokers gain less weight over time
Baseline smokers actually gained more weight over 2-year follow-up than non-smokers
45% of baseline smokers quit, which was associated with the greatest weight gain
However, even persistent smokers gained somewhat more weight than non-smokers
Findings may help deter young women from smoking for weight control purposes
Acknowledgments
This study was supported by grant (DK072932) from the National Institutes of Health.
We thank project research assistants Cara Bohon, Shelley Durant, Erica Marchand, Janet Ng, and Alex Stanton, as well as the undergraduates who volunteered to participate in this trial.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Boles S, Johnson P. Gender, weight concerns, and adolescent smoking. Journal of Addictive Diseases. 2001;20:5–14. doi: 10.1300/J069v20n02_02. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson D. Model selection and multi-model inference: A practical information-theoretic approach. Springer; New York, NY: 2002. [Google Scholar]
- Centers for Disease Control and Prevention Tobacco use among adults-United States, 2005. Morbidity and Mortality Weekly Report. 2009;55:1145–1148. [PubMed] [Google Scholar]
- Chaput J, Leblanc C, Perusse L, Despres J, Bouchard C, Tremblay A. Risk factors for adult overweight and obesity in the Quebec Family Study: Have we been barking up the wrong tree? Obesity. 2009;17:1964–1970. doi: 10.1038/oby.2009.116. doi: 10.1038/oby.2009.116. [DOI] [PubMed] [Google Scholar]
- Dennis B, Pajak A, Pardo B, Davis C, Williams O, Piotrowski W. Weight gain and its correlates in Poland between 1983 and 1993. International Journal of Obesity. 2000;24:1507–1513. doi: 10.1038/sj.ijo.0801435. [DOI] [PubMed] [Google Scholar]
- Field et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112:900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- Flegal K, Troiano R, Pamuk E, Kuczmarski R, Campbell S. The influence of smoking cessation on the prevalence of overweight in the United States. New England Journal of Medicine. 1995;333:1165–1170. doi: 10.1056/NEJM199511023331801. [DOI] [PubMed] [Google Scholar]
- Freedman K, Nelson N, Feldman L. Smoking initiation among young adults in the United States and Canada, 1998-2010; A systematic review. Preventing Chronic Disease. 2012;9:E05. [PMC free article] [PubMed] [Google Scholar]
- Harakeh Z, Engles R, Monshouwer K, Hanssen P. Adolescent's weight concerns and the onset of smoking. Substance Use and Misuse. 2010;45:1847–1860. doi: 10.3109/10826081003682149. [DOI] [PubMed] [Google Scholar]
- Hennekens C, Andreotti F. Leading avoidable cause of premature deaths worldwide: Case for obesity. American Journal of Medicine. 2013;126:97. doi: 10.1016/j.amjmed.2012.06.018. [DOI] [PubMed] [Google Scholar]
- Hox J. Multilevel Analysis: Techniques and Applications. Taylor & Francis; New York, NY: 2010. [Google Scholar]
- Johnston L, O'Malley P, Bachman J. Secondary school students. Vol. 1. National Institute on Drug Abuse; Rockville, MD: 2000. Monitoring the Future National Survey Results on Drug Use, 1975-1999. [Google Scholar]
- Kahn H, Tatham L, Rodriguez C, Calle E, Thun M, Heath C. Stable behaviors associated with adults’ 10-year change in body mass index and likelihood of gain at the waist. American Journal of Public Health. 1997;87:747–754. doi: 10.2105/ajph.87.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klesges R, Ward K, Ray J, Cutter G, Jacobs D, Wagenknecht L. The prospective relationships between smoking and weight in a young, biracial cohort: The coronary artery risk development in young adults study. Journal of Consulting and Clinical Psychology. 1998;66:987–993. [PubMed] [Google Scholar]
- Koh-Banerjee P, Chu N, Spiegelman D, Rosner B, Colditz G, Willet W, et al. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16587 men. American Journal of Clinical Nutrition. 2003;78:719–727. doi: 10.1093/ajcn/78.4.719. [DOI] [PubMed] [Google Scholar]
- Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied linear statistical models. McGraw-Hill; New York, NY: 2005. [Google Scholar]
- Lipsey M, Wilson D. Practical meta-analysis. Sage Publications; Thousand Oaks, CA: 2001. [Google Scholar]
- Mokdad A, Marks J, Stroup D, Gerberding J. Actual causes of death in the United States 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Hao T, Rimm E, Willett W, Hu F. Changes in diet and lifestyle and long-term weight gain in women and men. New England Journal of Medicine. 2011;364:2394–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Hara P, Connett J, Lee W, Nides M, Murray R, Wise R. Early and late weight gain following smoking cessation in the Lung Health Study. American Journal of Epidemiology. 1998;148:821–830. doi: 10.1093/oxfordjournals.aje.a009706. [DOI] [PubMed] [Google Scholar]
- Pietrobelli A, Faith M, Allison D, Gallagher D, Chiumello G, Heymsfield S. Body mass index as a measure of adiposity among children and adolescents: A validation study. Journal of Pediatrics. 1998;132:204–210. doi: 10.1016/s0022-3476(98)70433-0. [DOI] [PubMed] [Google Scholar]
- Rasmussen F, Tynelius P, Kark M. Importance of smoking habits for longitudinal and age-matched changes in body mass index: A cohort study of Swedish men and women. Preventive Medicine. 2003;37:1–9. doi: 10.1016/s0091-7435(03)00043-4. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk AS, Cheong YF, Congdon RT, du Toit M. HLM 6: Hierarchical linear and nonlinear modeling. Scientific Software International; Lincolnwood, IL: 2004. [Google Scholar]
- Rigotti N, Lee J, Wechsler H. US college students’ use of tobacco products: Results of a national survey. Journal of the American Medical Association. 2000;284:699–705. doi: 10.1001/jama.284.6.699. doi:10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- Rasmussen F, Tynelius P, Kark M. Importance of smoking habits for longitudinal and age-matched changes in body mass index: A cohort study of Swedish men and women. Preventive Medicine. 2003;37:1–9. doi: 10.1016/s0091-7435(03)00043-4. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A. Hierarchical linear models: Applications and data analysis methods. SAGE Publications; London: 2002. [Google Scholar]
- Simmons V, Brandon T. Secondary smoking prevention in a university setting: A randomized comparison of an experimental, theory-based intervention and a standard didactic intervention for increasing cessation motivation. Health Psychology. 2007;26:268–277. doi: 10.1037/0278-6133.26.3.268. doi:10.1037/0278-6133.26.3.268. [DOI] [PubMed] [Google Scholar]
- Singer J, Willett J. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press, USA.; New York, NY: 2003. [Google Scholar]
- Stice E, Cameron R, Killen JD, Hayward C, Taylor CB. Naturalistic weight reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. Journal of Consulting and Clinical Psychology. 1999;67:967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- Stice E, Durant S, Burger KS, Schoeller DA. Weight suppression and risk of future increases in body mass: effects of suppressed resting metabolic rate and energy expenditure. American Journal of Clinical Nutrition. 2011;94:7–11. doi: 10.3945/ajcn.110.010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of Abnormal Psychology. 2009;118:587–597. doi: 10.1037/a0016481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Martinez E. Cigarette smoking prospectively predicts retarded physical growth during adolescence. Journal of Adolescent Health. 2005;37:363–370. doi: 10.1016/j.jadohealth.2004.10.017. [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Marti CN. Efficacy trial of a selective prevention program targeting both eating disorder symptoms and unhealthy weight gain among female college students. Journal of Consulting and Clinical Psychology. 2012;80:164–-170. doi: 10.1037/a0026484. doi: 10.1037/a0026484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H. Prospective relations of body image, eating, and affective disturbances to smoking onset in adolescent girls: How Virginia slims. Journal of Consulting and Clinical Psychology. 2003;71:129–135. doi: 10.1037//0022-006x.71.1.129. [DOI] [PubMed] [Google Scholar]
- White M. Smoking for weight control and its associations with eating disorder symptomatology. Comprehensive Psychiatry. 2012;53:403–407. doi: 10.1016/j.comppsych.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson D, Madans J, Anda R, Kleinman J, Giovino G, Byers T. Smoking cessation and severity of weight gain in a national cohort. New England Journal of Medicine. 1991;324:739–745. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- Yeager DS, Krosnick JA. The validity of self-reported nicotine product use in the 2001-2008 National Health and Nutrition Examination survey. Medical Care. 2010;48:1128–1132. doi: 10.1097/MLR.0b013e3181ef9948. [DOI] [PubMed] [Google Scholar]


