Abstract
AIM: To evaluate perceived risk, diagnostic testing, and acceptance of a diagnosis of irritable bowel syndrome (IBS) among the Korean laypersons.
METHODS: We designed a conceptual framework to evaluate the health-seeking behavior of subjects based on a knowledge, attitude, and practice model. We developed a vignette-based questionnaire about IBS based on a literature review and focused group interviews. The vignette described a 40-year-old woman who meets the Rome III criteria for IBS without red-flag signs. It was followed by questions about demographic characteristics, health behaviors, IBS symptoms, risk perception, perceived need for diagnostic tests, and acceptance of a positive diagnosis of IBS. We planned a nationwide survey targeting laypersons without IBS and between the ages of 20 and 69 years. Survey participants were selected by quota sampling stratified by gender, age, and nationwide location. A multivariate logistic model was constructed based on literature reviews, univariate analysis, and a stepwise selection method to investigate correlations between the perceived risk, need for diagnostic tests, and acceptance of a positive diagnosis.
RESULTS: Of 2354 eligible households, 1000 subjects completed the survey and 983 subjects were analyzed, excluding those who met symptom criteria for IBS. After reading the IBS vignette, the majority of subjects (86.8%) responded that the patient was at increased risk of severe disease. The most frequent concern was colon cancer (59.8%), followed by surgical condition (51.5%). Most subjects responded the patient needs diagnostic tests (97.2%). Colonoscopy was the most commonly required test (79.5%). Less than half of the respondents requested a stool examination (45.0%), blood test (40.7%), abdominal ultrasound (36.0%), or computed tomography (20.2%). The subjects who felt increased risk were more likely to see a need for colonoscopy [adjusted odds ratio (aOR) = 2.10, 95%CI: 1.38-3.18]. When asked about the positive diagnosis, the most frequent response was that “the patient would not be reassured” (65.7%). The increased risk perception group was less likely to be reassured by a positive diagnosis of IBS, compared to the other respondents (aOR = 0.52, 95%CI: 0.34-0.78).
CONCLUSION: For IBS diagnosis, increased risk perception is a possible barrier to the appropriate use of diagnostic tests and to the patient’s acceptance of a positive diagnosis.
Keywords: Diagnostic testing, Patient attitude, Positive diagnosis, Functional gastrointestinal disease, Irritable bowel syndrome
Core tip: To our knowledge, this is the first study to evaluate the acceptance of laypersons (as potential patients or lay consultants) with a positive diagnosis of irritable bowel syndrome (IBS). The majority of respondents showed a high perceived need for diagnostic testing (97.2%), especially colonoscopy (79.5%), and most of them were reluctant to accept a positive diagnosis of IBS (65.7%). In addition, the increased risk perception group was less likely to be reassured (adjusted odds ratio = 0.52, 95%CI: 0.34-0.78). Therefore, to help patients accept an appropriate diagnosis of IBS, the health care system must manage the perceived risk of patients.
INTRODUCTION
Irritable bowel syndrome (IBS) is a chronic condition characterized by recurrent abdominal pain and altered bowel habits without detectable organic cause. Since 2006, physicians have been encouraged to use the Rome III criteria to make a positive diagnosis of IBS[1] because of the low diagnostic yield of organic cause in patients who fulfill the diagnostic criteria[2].
However, the absence of biological markers and the possibility of overlooking organic cause can concern both patients[3] and health care providers[4]. These issues can make it difficult to accept a positive diagnosis of IBS and can lead to overuse of diagnostic tests.
Spiegel et al[5] reported that many health care providers did not follow evidence-based guidelines for IBS diagnosis. Compared with IBS experts, other health care providers - including community gastroenterologists, general internal medicine physicians, and nurse practitioners - were less likely to accept a positive diagnosis.
In contrast, there are few reports about the reaction to positive diagnosis among laypersons. Only a few studies have investigated the knowledge and anxieties of patients with IBS[3,6]. However, the overuse of diagnostic tests can be driven by patients’ wishes[7], as well as those of health care providers[8]. Patients are often in active positions[9] as consumers of health care services, particularly following the increase of health information available through the media and the improvement of accessibility to health care services[7,10,11]. In addition, patient wishes can be influenced by a lay consultation network including caregivers, family members, or neighborhood residents[12-14]. This is especially true for chronic conditions[14]. Therefore, this study aimed to describe the perceived risk, desire for diagnostic tests, and acceptance of a positive diagnosis of IBS among laypersons (as potential patients or lay consultants) and to investigate correlations between these factors.
MATERIALS AND METHODS
Conceptual framework
We designed a conceptual framework based on the knowledge, attitude and practice (KAP) model to quantitatively evaluate the health-seeking behavior of study subjects. The KAP model looks at what is known, believed, and done in relation to a particular topic[15]. The scope of this study included the knowledge and attitudes of laypersons about IBS. We investigated two hypotheses: (1) high perception of risk could lead to inappropriate diagnostic tests; and (2) high perception of risk could be a barrier to accepting a positive diagnosis (Figure 1).
Figure 1.
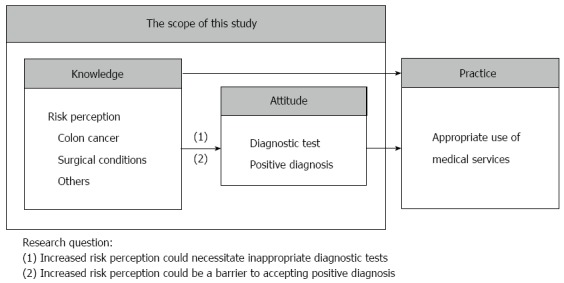
Conceptual framework of the study hypothesis: Increased risk perception about irritable bowel syndrome could influence perceived need for diagnostic tests and acceptance of a positive diagnosis.
Sampling frame
We planned a nationwide survey targeting laypersons between the ages of 20 and 69 years without IBS. To secure representativeness, survey participants were selected by quota sampling from 100 areas stratified by gender, age, and location using the latest database from the Korean National Statistical Office as a sampling frame.
Trained interviewers conducted person-to-person interviews using questionnaires between August and September of 2012. They visited households in various time zones to ensure the diversity of respondents in gender, age, and job. Interviewers aimed to interview 10 respondents in each of 100 regions. Subjects received educational material about IBS for completing the survey. The Institutional Review Board of Seoul National University Hospital approved this study.
Vignette-based questionnaire
We developed a vignette-based questionnaire about IBS based on a literature review and a focused group interview of physicians and patients with functional gastrointestinal disorders, including IBS and functional dyspepsia. The vignette described a 40-year-old woman who meets the Rome III criteria for IBS without red-flag signs. It was followed by questions about demographic characteristics, health behaviors, symptoms of IBS, risk perception, needs for diagnostic tests, and acceptance of the positive diagnosis of IBS.
Measurement of risk perception
The question on risk perception of IBS was phrased as follows: “Based upon the information provided at this point, do you believe that this patient is at increased risk of the following conditions?” Respondents had five multiple choice options: (1) colon cancer; (2) nutritional deficit; (3) surgical condition; (4) shorter life span; or (5) nothing relevant. They were classified into the “concerned group” if they selected one or more of the first four options (colon cancer, nutritional deficit, surgical condition, or shorter life span) and classified into the “not concerned group” if they selected the last option (nothing relevant).
Measurement of perceived need for diagnostic testing
The perception of need for diagnostic testing was assessed by the following question: “In your opinion, the patient needs to be diagnosed by ¡ (choose everything appropriate).” Respondents had six multiple choice options: (1) blood test; (2) stool examination; (3) colonoscopy; (4) abdominal ultrasound; (5) computed tomography; or (6) don’t need any tests.
Measurement of acceptance of a positive diagnosis
Acceptance of a positive diagnosis of IBS was assessed as follows: “If a doctor diagnoses her (as having) irritable bowel syndrome without any kind of diagnostic test, she would be ¡ (choose only one answer).” Respondents had four options for how the patient would feel about the diagnosis: (1) reassured; (2) still worried; (3) impatient with the uncertainty; or (4) have no idea. Respondents were classified into the “reassured group” if they selected the first option (reassured) and classified into the “not reassured group” if they selected either of the next two options (still worried or impatient of uncertainty).
Statistical analysis
Descriptive data about respondents’ characteristics, perceived risk, perceived need for diagnostic tests, and acceptance of a positive diagnosis were presented as frequency and proportion. We compared characteristics between two groups using t tests for continuous variables and the chi-square test for categorical variables. To evaluate the correlation between perceived risk or perceived need for diagnostic tests and acceptance of a positive diagnosis, a multivariate logistic model was constructed based on literature reviews[8,16], univariate analysis, and the stepwise selection method. We calculated odds ratios (ORs) and 95% confidence intervals (CIs) adjusting for sex, age, area of residency, number of comorbidities, and presence of problem drinking. We used STATA version 12.0 (STATA Corp., Houston, TX), with statistical significance defined as P ≤ 0.05.
RESULTS
Out of 2354 contacts, 1000 subjects completed the survey, giving a response rate of 42.5%. A total of 983 subjects were included in the final analysis excluding 17 subjects who meet Rome III diagnostic criteria for IBS.
Characteristics of study subjects
The mean age of the respondents was 42.71 years (± 12.65 years). Most of them had no comorbid disease (79.2%), and 7.2% had more than two comorbid diseases. The majority of respondents (78.8%) visited a hospital five or fewer times per year. Subjects who reported that the patient had an increased risk were more likely to live in urban area (54.3% vs 44.6%, P = 0.040) and to report problem drinking (10.8% vs 19.1%, P = 0.021) compared with the control group. However, there were no statistically significant differences in age, gender, marital status, educational status, household income, hospital visitor smoking status between the two groups (Table 1).
Table 1.
Characteristics of respondents by risk perception of irritable bowel syndrome n (%)
|
Increased risk perception (colon cancer, nutritional deficit, surgical condition, or shorter life span) (n = 983) |
|||
| No (n = 130) | Yes (n = 853) | P value1 | |
| Characteristics | |||
| Age (yr) | |||
| mean ± SD | 42.55 ± 13.50 | 42.74 ± 12.53 | 0.871 |
| 29-39 | 54 (41.5) | 371 (43.5) | |
| 40-59 | 62 (47.7) | 377 (44.2) | |
| ≥ 60 | 14 (10.8) | 105 (12.3) | 0.730 |
| Sex | 0.908 | ||
| Male | 67 (51.5) | 435 (51.0) | |
| Female | 63 (48.5) | 418 (49.0) | |
| Marital status | 0.403 | ||
| Married | 92 (70.8) | 645 (75.6) | |
| Widowed/separated/divorced | 1 (0.8) | 10 (1.2) | |
| Single | 37 (28.4) | 198 (23.2) | |
| Educational status (yr) | 0.617 | ||
| ≥ 13 | 45 (34.6) | 331 (38.8) | |
| 10-12 | 74 (56.9) | 447 (52.4) | |
| ≤ 9 | 11 (8.5) | 75 (8.8) | |
| Household income (monthly) | 0.712 | ||
| ≥ $4000 | 21 (16.2) | 153 (17.9) | |
| $2000-3999 | 81 (62.3) | 499 (58.5) | |
| < $2000 | 28 (21.5) | 201 (23.6) | |
| Region | 0.040 | ||
| Urban | 58 (44.6) | 463 (54.3) | |
| Rural | 72 (55.4) | 390 (45.7) | |
| Hospital visit (/yr) | |||
| mean ± SD | 4.68 ± 5.94 | 4.24 ± 4.86 | 0.343 |
| 0-5 | 96 (73.8) | 679 (79.6) | |
| 6-10 | 24 (18.5) | 104 (12.2) | |
| ≥ 11 | 10 (7.7) | 70 (8.2) | 0.141 |
| No. of comorbidity | |||
| mean ± SD | 0.28 ± 0.57 | 0.35 ± 0.94 | 0.403 |
| 0 | 100 (76.9) | 679 (79.6) | |
| 1 | 26 (20.0) | 107 (12.5) | |
| ≥ 2 | 4 (3.1) | 67 (7.9) | 0.016 |
| Smoking | 0.969 | ||
| None | 77 (59.2) | 500 (58.6) | |
| Past | 15 (11.5) | 105 (12.3) | |
| Current | 38 (29.2) | 248 (29.1) | |
| Problem drinking2 | 0.021 | ||
| No | 116 (89.2) | 690 (80.9) | |
| Yes | 14 (10.8) | 163 (19.1) | |
P values calculated from t-test for continuous variables and the chi-square test for categorical variables;
For men, seven or more drinks on an occasion and more than two times per week; for women, five or more drinks on an occasion and more than two times per week. IBS: Irritable bowel syndrome.
Perceived risk of IBS
The majority of respondents (86.8%) responded that the presented case is at increased risk of severe disease, whereas only 13.2% of respondents reported no increased risk. The most frequent concern was colon cancer (59.8%), followed by surgical condition (51.5%). Less than half of the respondents chose nutritional deficit (20.4%) or shorter life span (11.5%) (Table 2).
Table 2.
Perceived risk of irritable bowel syndrome among laypersons1 n (%)
| The patient is at increased risk of…(choose EVERYTHING appropriate) | No | Yes |
| Colon cancer | 395 (40.2) | 588 (59.8) |
| Nutritional deficit | 782 (79.6) | 201 (20.4) |
| Surgical condition | 477 (48.5) | 506 (51.5) |
| Shorter life span | 870 (88.5) | 113 (11.5) |
| Nothing relevant | 853 (86.8) | 130 (13.2) |
| Union of answers | 130 (13.2) | 853 (86.8) |
1The respondents were asked: "Based upon the information provided at this point, do you believe that this patient is at increased risk of following conditions? (choose EVERYTHING appropriate)".
Need for diagnostic tests
Most of the subjects (97.2%) responded that a diagnostic test is necessary for the patient. Colonoscopy was the most commonly requested test (79.5%). The increased risk perception group was more likely than other respondents to respond that colonoscopy was needed [adjusted odds ratio (aOR) = 2.10, 95%CI: 1.38-3.18]. Less than half of the respondents requested a stool examination (45.0%), blood test (40.7%), abdominal ultrasound (36.0%), or computed tomography (20.2%). The increased risk perception group was also more likely than other respondents to request these tests. Only 28 subjects (2.8%) responded that diagnostic tests are not necessary (Table 3).
Table 3.
Needs of diagnostic tests by risk perception of irritable bowel syndrome1 n (%)
| The patient needs to be diagnosed by …(choose EVERYTHING appropriate) |
Increased risk perception (colon cancer, nutritional deficit, surgical condition, or shorter life span) |
|||
| No (n = 130) | Yes (n = 853) | OR2 (95%CI) | aOR3 (95%CI) | |
| Blood test (n = 400) | 30 (23.1) | 370 (43.4) | 2.55 (1.66-3.92) | 2.66 (1.72-4.11) |
| Stool examination (n = 442) | 40 (30.8) | 402 (47.1) | 2.01 (1.35-2.98) | 2.12 (1.42-3.17) |
| Colonoscopy (n = 781) | 89 (68.5) | 692 (81.1) | 1.98 (1.32-2.98) | 2.10 (1.38-3.18) |
| Abdominal ultrasound (n = 354) | 25 (19.2) | 329 (38.6) | 2.64 (1.67-4.17) | 2.70 (1.70-4.28) |
| Computed tomography (n = 199) | 10 (7.7) | 189 (22.2) | 3.42 (1.76-6.64) | 3.33 (1.71-6.51) |
| Don't need any test (n = 28) | 19 (14.6) | 9 (1.1) | 0.06 (0.03-0.14) | 0.05 (0.02-0.11) |
1The question was "In your opinion, the patient needs to be diagnosed by… (choose EVERYTHING appropriate);
Odds ratio of "yes" referenced by "no";
Adjusted by sex, age, area of residency, number of comorbidity, and problem drinking. CI: Confidence interval; OR: Odds ratio; aOR: Adjusted odds ratio.
Acceptance of a positive diagnosis
When asked about the positive diagnosis, the most frequent response was that “the patient would not be reassured” (65.7%). The increased risk perception group was less likely to be reassured (aOR = 0.52, 95%CI: 0.34-0.78) by a positive diagnosis compared with the control group (Table 4).
Table 4.
Acceptance of a positive diagnosis by risk perception of irritable bowel syndrome1 n (%)
| The patient would be…(choose ONLY ONE answer) |
Increased risk perception (colon cancer, nutritional deficit, surgical condition, or shorter life span) |
|||
| No (n = 130) | Yes (n = 853) | OR2 (95%CI) | aOR3 (95%CI) | |
| Reassured (n = 288) | 50 (38.5) | 238 (27.9) | 0.49 (0.33-0.73) | 0.52 (0.34-0.78) |
| Not reassured (n = 646) | 60 (46.2) | 586 (68.7) | 2.05 (1.37-3.07) | 1.94 (1.29-2.93) |
| Still worried (n = 417) | 33 (25.4) | 384 (45.0) | NA | NA |
| Impatient of uncertainty (n = 229) | 27 (20.8) | 202 (23.7) | NA | NA |
| Have no idea (n = 49) | 20 (15.4) | 29 (3.4) | NA | NA |
1The question was "If a doctor diagnoses her (as) irritable bowel syndrome without any kind of diagnostic test, she would be… (choose ONLY ONE answer)";
Odds ratio of "yes" referenced by "no";
Adjusted by sex, age, area of residency, number of comorbidity, and problem drinking. CI: Confidence interval; OR: Odds ratio; aOR: Adjusted odds ratio; NA: Not applicable.
DISCUSSION
To our knowledge, this is the first study about laypersons’ acceptance of a positive diagnosis of IBS in the context of the KAP model. A few qualitative[17] and quantitative studies[3,6,18] have investigated knowledge and anxiety about IBS among patients with IBS. They reported serious concern about organic disease[3,6] and strong expectation of diagnostic tests[3,17,18] among IBS patients. However, none of these studies measured whether patients could accept the standard diagnostic process and whether such acceptance is correlated with their knowledge about IBS.
In this study, we surveyed a representative sample of the national population as potential patients or lay consultants. When questioned about a typical IBS vignette, the majority of respondents showed increased risk perception about IBS (86.8%). Concern about colon cancer (59.8%) was the most prevalent and was three times larger than that found in previous reports from the United States and Lebanon, although direct comparison should be made with care[3,6]. Those studies reported that concern about inflammatory bowel disease[3] or colitis[6] was double that for cancer. The difference between those studies and our own is likely mainly a result of differences in the epidemiology of inflammatory bowel disease between Korea and the United States[19]. We did not ask about concern about inflammatory bowel disease in this study because its prevalence is still low in Korea. Concern about serious disease tends to be higher among IBS patients compared to the healthy population, as recently reported for women and men in Sweden[20].
The most important observation in this study was that the majority of respondents showed a high perceived necessity for diagnostic testing (97.2%), especially colonoscopy (79.5%). Two thirds of respondents (65.7%) found it hard to accept a positive diagnosis of IBS. In addition, increased risk perception was correlated with the perceived need for colonoscopy (aOR = 2.10, 95%CI: 1.38-3.18) and with difficulty in accepting a positive diagnosis of IBS (aOR = 0.52, 95%CI: 0.34-0.78). Several reports have pointed out that the need for reassurance is a key factor in seeking medical consultation among patients with functional gastrointestinal disorders[21-23] and that such patients expect diagnostic tests beyond what is usually recommended by physicians[3,17,18]. As a result, both patients and doctors frequently experience frustration, dissatisfaction, and feelings of stigmatization[24,25]. However, Spiegel et al[21] reported that a negative colonoscopy finding was not associated with reassurance or improved health-related quality of life in IBS patients. In a literature review, Koloski et al[16] even suggested that abnormal attitudes and beliefs about illness are more important than symptom severity or knowledge about illness in patients’ actions to seek health care. Such results might partly reflect differences between health care systems, including low cost of diagnostic tests, quality of medical facilities, and popularized private or public screening programs for colon cancer[26].
Patient expectations are an important issue as many countries attempt to reduce the overuse of health care services. Several factors contribute to overuse, including defensive treatment by the physician, patient wishes, inappropriate financially motivated factors, health system factors, industry, and the media[7]. Among these factors, patient wishes become more important as expectations about medical technology increase and health care services become more accessible. Although it is not clear how much patient wishes contribute to the overuse of diagnostic tests, it would be no surprise if they play a major role[7]. Patient expectations would be hard to control in the presence of large amounts of unverified health information, a surplus of medical resources, and health care providers with little motivation to control the overuse of diagnostic tests[10,11]. That is the case in Korea, where there is a flood of health information from mass media and Internet sources, a wealth of health care facilities, very low medical costs, and a fee-for-service national health insurance.
Therefore, to alleviate the need for diagnostic tests and to help patients accept a positive diagnosis, the health care system must manage the perceived risk itself instead of performing unnecessary tests. Further study is needed to determine the strength of the causality involved and how physicians and the government can effectively intervene through medical practice and the health care system.
Strengths of this study include the use of a nationwide sampling frame and person-to-person interviews. Study subjects were selected using proportionate quota sampling stratified by age, gender, and location in South Korea, as mentioned in the Methods section. Trained interviewers prevented respondents from misunderstanding questions or giving invalid answers.
An important consideration is that the subjects of this study were laypersons without IBS. However, they are potential lay consultants such as caregivers, family members, and neighborhood members[12]. Therefore, compared with surveys of IBS patients, our study provides additional information about the diagnosis of IBS[3,21].
One limitation of our study is the possibility of selection bias. The response rate (42.5%) was not lower than those of previous studies (reported as 38%[6] to 39.3%[3]), even though we could not review the characteristics of non-respondents.
Another limitation is that data from a KAP survey do not provide an explanation about causality. This cross-sectional finding needs further study to determine the causality between risk perception and attitude toward a positive diagnosis.
Furthermore, our conceptual framework is based on a strong hypothesis that knowledge can change the attitudes and practice of laypersons. Even though knowledge is an important target in clinical practice, it is also a contributing factor to the overuse of diagnostic tests, as mentioned above[27]. Therefore, a longitudinal study is needed to evaluate whether improved knowledge can control the overuse of tests and change attitudes about positive diagnosis in practice.
Despite these limitations, this study’s results suggest that for most laypersons, it is hard to accept a positive diagnosis of IBS. High risk perception can be a barrier to the control of overuse of diagnostic tests and to acceptance of a positive diagnosis of IBS. Therefore, it is important to manage perceived risk by providing information about the natural course of IBS and the efficacy of diagnostic testing in IBS.
Clinical vignette
A 40-year-old woman visited a local clinic with a longstanding history of abdominal pain. Her pain started when she was young and recurred frequently. The pain often worsened within 10 min after a meal and was relieved by defecation. Sometimes she had urgent loose stool passage several times a day. Sometimes there was no bowel movement for three to four days. She frequently had to avoid eating to prevent urgent bowel movement. She denied weight loss, fever, and other symptoms. She did not take medication or imbibe excess alcohol.
COMMENTS
Background
It has been reported that many health care providers do not follow evidence-based guidelines for irritable bowel syndrome (IBS) diagnosis despite the low diagnostic yield of organic cause in patients who fulfill the diagnostic criteria. Unnecessary diagnostic testing can be driven not only by health care providers but also by patients themselves, and it can be influenced by a lay consultation network including caregivers, family members, or neighbors. However, there are few reports about the knowledge and attitude of laypersons as potential patients or lay consultants.
Research frontiers
The absence of biological markers and the possibility of overlooking organic cause can concern both patients and health care providers. In the area of IBS diagnosis, the research hotspot is how to improve both the accuracy of and the adherence to the evidence-based diagnostic criteria.
Innovations and breakthroughs
There are a few reports about health care providers’ adherence to the evidence-based diagnostic criteria of IBS. It is difficult, however, to find reports about how the attitudes of the patients themselves, or medical consumers, may affect medical diagnoses and decisions. Based on the insight that most medical decisions are the result of interactions between health care providers and the patients, in this study, we focused on the patient side of the medical decision equation.
Applications
Most laypersons are reluctant to accept a positive diagnosis of IBS. High risk perception can be a barrier to controlling the overuse of diagnostic tests and to acceptance of a positive diagnosis of IBS. Therefore, to help patients accept an appropriate diagnosis of IBS, the health care system must manage patients’ risk perceptions.
Peer review
This study included a laborious analysis of the data with correct methodology. The results are interesting and lead to the idea of health education for the laypersons, which alone can change perceptions about IBS. The concern of a large number of respondents for certainty in the diagnosis of IBS without conducting additional examinations may also be a message for the medical world that a more precise definition of the criteria for the diagnosis of IBS is needed (an improvement of the Rome III criteria).
Footnotes
Supported by Korea Centers for Disease Control and Prevention, No. 800-20120075
P- Reviewer: Mihaila RG, Zouiten-Mekki L S- Editor: Ding Y L- Editor: A E- Editor: Wang CH
References
- 1.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 2.Cash BD, Schoenfeld P, Chey WD. The utility of diagnostic tests in irritable bowel syndrome patients: a systematic review. Am J Gastroenterol. 2002;97:2812–2819. doi: 10.1111/j.1572-0241.2002.07027.x. [DOI] [PubMed] [Google Scholar]
- 3.Lacy BE, Weiser K, Noddin L, Robertson DJ, Crowell MD, Parratt-Engstrom C, Grau MV. Irritable bowel syndrome: patients’ attitudes, concerns and level of knowledge. Aliment Pharmacol Ther. 2007;25:1329–1341. doi: 10.1111/j.1365-2036.2007.03328.x. [DOI] [PubMed] [Google Scholar]
- 4.Spiegel BM. Do physicians follow evidence-based guidelines in the diagnostic work-up of IBS? Nat Clin Pract Gastroenterol Hepatol. 2007;4:296–297. doi: 10.1038/ncpgasthep0820. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel BM, Farid M, Esrailian E, Talley J, Chang L. Is irritable bowel syndrome a diagnosis of exclusion?: a survey of primary care providers, gastroenterologists, and IBS experts. Am J Gastroenterol. 2010;105:848–858. doi: 10.1038/ajg.2010.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halpert A, Dalton CB, Palsson O, Morris C, Hu Y, Bangdiwala S, Hankins J, Norton N, Drossman D. What patients know about irritable bowel syndrome (IBS) and what they would like to know. National Survey on Patient Educational Needs in IBS and development and validation of the Patient Educational Needs Questionnaire (PEQ) Am J Gastroenterol. 2007;102:1972–1982. doi: 10.1111/j.1572-0241.2007.01254.x. [DOI] [PubMed] [Google Scholar]
- 7.Rehani B. Imaging overutilisation: Is enough being done globally? Biomed Imaging Interv J. 2011;7:e6. doi: 10.2349/biij.7.1.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spiegel BM, Kanwal F, Naliboff B, Mayer E. The impact of somatization on the use of gastrointestinal health-care resources in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:2262–2273. doi: 10.1111/j.1572-0241.2005.00269.x. [DOI] [PubMed] [Google Scholar]
- 9.Encyclopedia WTF. [updated 29 August 2013 22: 48 UTC; cited 2013 16 October] Medicalization: Wikimedia Foundation Inc; 2013. Available from: http://en.wikipedia.org/wiki/Medicalization. [Google Scholar]
- 10.Emanuel EJ, Fuchs VR. The perfect storm of overutilization. JAMA. 2008;299:2789–2791. doi: 10.1001/jama.299.23.2789. [DOI] [PubMed] [Google Scholar]
- 11.Fuchs VR. Eliminating «waste» in health care. JAMA. 2009;302:2481–2482. doi: 10.1001/jama.2009.1821. [DOI] [PubMed] [Google Scholar]
- 12.Halpert A, Dalton CB, Palsson O, Morris C, Hu Y, Bangdiwala S, Hankins J, Norton N, Drossman DA. Patient educational media preferences for information about irritable bowel syndrome (IBS) Dig Dis Sci. 2008;53:3184–3190. doi: 10.1007/s10620-008-0280-4. [DOI] [PubMed] [Google Scholar]
- 13.Stoller EP, Wisniewski AA. The structure of lay consultation networks: managing illness in community settings. J Aging Health. 2003;15:482–507. doi: 10.1177/0898264303253504. [DOI] [PubMed] [Google Scholar]
- 14.Vassilev I, Rogers A, Sanders C, Kennedy A, Blickem C, Protheroe J, Bower P, Kirk S, Chew-Graham C, Morris R. Social networks, social capital and chronic illness self-management: a realist review. Chronic Illn. 2011;7:60–86. doi: 10.1177/1742395310383338. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Advocacy, communication and social control for TB control. A guide to developing knolwedge, attitude and practice survey 2008. Available from: http://www.stoptb.org/assets/documents/resources/publications/acsm/ACSM_KAP GUIDE.pdf.
- 16.Koloski NA, Talley NJ, Boyce PM. Predictors of health care seeking for irritable bowel syndrome and nonulcer dyspepsia: a critical review of the literature on symptom and psychosocial factors. Am J Gastroenterol. 2001;96:1340–1349. doi: 10.1111/j.1572-0241.2001.03789.x. [DOI] [PubMed] [Google Scholar]
- 17.Casiday RE, Hungin AP, Cornford CS, de Wit NJ, Blell MT. Patients’ explanatory models for irritable bowel syndrome: symptoms and treatment more important than explaining aetiology. Fam Pract. 2009;26:40–47. doi: 10.1093/fampra/cmn087. [DOI] [PubMed] [Google Scholar]
- 18.Bijkerk CJ, de Wit NJ, Stalman WA, Knottnerus JA, Hoes AW, Muris JW. Irritable bowel syndrome in primary care: the patients’ and doctors’ views on symptoms, etiology and management. Can J Gastroenterol. 2003;17:363–368; quiz 405-406. doi: 10.1155/2003/532138. [DOI] [PubMed] [Google Scholar]
- 19.Ponder A, Long MD. A clinical review of recent findings in the epidemiology of inflammatory bowel disease. Clin Epidemiol. 2013;5:237–247. doi: 10.2147/CLEP.S33961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faresjö Å, Grodzinsky E, Hallert C, Timpka T. Patients with irritable bowel syndrome are more burdened by co-morbidity and worry about serious diseases than healthy controls--eight years follow-up of IBS patients in primary care. BMC Public Health. 2013;13:832. doi: 10.1186/1471-2458-13-832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spiegel BM, Gralnek IM, Bolus R, Chang L, Dulai GS, Naliboff B, Mayer EA. Is a negative colonoscopy associated with reassurance or improved health-related quality of life in irritable bowel syndrome? Gastrointest Endosc. 2005;62:892–899. doi: 10.1016/j.gie.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 22.Delaney BC. Why do dyspeptic patients over the age of 50 consult their general practitioner? A qualitative investigation of health beliefs relating to dyspepsia. Br J Gen Pract. 1998;48:1481–1485. [PMC free article] [PubMed] [Google Scholar]
- 23.Howell S, Talley NJ. Does fear of serious disease predict consulting behaviour amongst patients with dyspepsia in general practice? Eur J Gastroenterol Hepatol. 1999;11:881–886. doi: 10.1097/00042737-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Dhaliwal SK, Hunt RH. Doctor-patient interaction for irritable bowel syndrome in primary care: a systematic perspective. Eur J Gastroenterol Hepatol. 2004;16:1161–1166. doi: 10.1097/00042737-200411000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Dixon-Woods M, Critchley S. Medical and lay views of irritable bowel syndrome. Fam Pract. 2000;17:108–113. doi: 10.1093/fampra/17.2.108. [DOI] [PubMed] [Google Scholar]
- 26.Kim Y, Jun JK, Choi KS, Lee HY, Park EC. Overview of the National Cancer screening programme and the cancer screening status in Korea. Asian Pac J Cancer Prev. 2011;12:725–730. [PubMed] [Google Scholar]
- 27.Hausmann-Muela S, Ribera JM, Nyamong I. DCPP Working Paper No. 14. Health-seeking behaviour and the health system response, August 2003. Available from: http://www.dcp2.org/file/29/wp14.pdf.


