Abstract
AIM: To explore the association between AT-rich interactive domain 1A (ARID1A) protein loss by immunohistochemistry and both clinicopathologic characteristics and prognosis in patients with colorectal cancer.
METHODS: We retrospectively collected clinicopathologic data and archived paraffin-embedded primary colorectal cancer samples from 209 patients, including 111 patients with colon cancer and 98 patients with rectal cancer. The tumor stage ranged from stage I to stage IV according to the 7th edition of the American Joint Committee on Cancer tumor-node-metastasis (TNM) staging system. All patients underwent resection of primary colorectal tumors. The expression of ARID1A protein in primary colorectal cancer tissues was examined by immunohistochemical staining. The clinicopathologic association and survival relevance of ARID1A protein loss in colorectal cancer were analyzed.
RESULTS: ARID1A loss by immunohistochemistry was not rare in primary colorectal cancer tumors (25.8%). There were 7.4%, 24.1%, 22.2% and 46.3% of patients with ARID1A loss staged at TNM stage I, II, III and IV, respectively, compared with 20.0%, 22.6%, 27.7% and 29.7% of patients without ARID1A loss staged at TNM stage I, II, III and IV, respectively. In patients with ARID1A loss, the distant metastasis rate was 46.3%. However, only 29.7% of patients without ARID1A loss were found to have distant metastasis. In terms of pathologic differentiation, there were 25.9%, 66.7% and 7.4% with poorly, moderately and well differentiated tumors in patients with ARID1A loss, and 14.2%, 72.3% and 13.5% with poorly, moderately and well differentiated tumors in patients without ARID1A loss, respectively. ARID1A loss was associated with late TNM stage (P = 0.020), distant metastasis (P = 0.026), and poor pathological classification (P = 0.035). However, patients with positive ARID1A had worse overall survival compared to those with negative ARID1A in stage IV colorectal cancer (HR = 2.49, 95%CI: 1.13-5.51).
CONCLUSION: ARID1A protein loss is associated with clinicopathologic characteristics in colorectal cancer patients and with survival in stage IV patients.
Keywords: AT-rich interactive domain 1A, Switching defective/sucrose non-fermenting complexes, Colorectal cancer, Clinicopathologic characteristics, Prognosis
Core tip: AT-rich interactive domain 1A (ARID1A) (BAF250A) is a member of the switching defective/sucrose non-fermenting (BAF) complexes, which remodel nucleosomes. ARID1A gene mutation and protein loss have been detected in many human cancers. However, research on their clinical association in colorectal cancer is limited and requires further exploration. We found that ARID1A loss was not rare in primary colorectal cancer tumors (25.8%), and it was associated with clinicopathologic characteristics in colorectal cancer patients and with survival in stage IV patients.
INTRODUCTION
Colorectal cancer (CRC) is the most common cancer of the digestive system. Diverse treatment strategies have been developed for better management of CRC[1,2]. Although mortality due to CRC has declined steadily during the past decades, CRC is still the second leading cause of cancer-related death in males and the third leading cause in females[3]. Patients with early stage CRC have a chance of being cured. For patients with stage IV CRC, the prognosis is poor. The tumor-node-metastasis (TNM) staging system is the most effective and commonly recognized clinical prognostic factor. However, even in the same stage, the prognoses of patients vary enormously due to molecular differences. Many prognostic biomarkers have been suggested, but only the test for RAS mutation[4] and microsatellite instability (MSI)[5,6] have become part of the routine clinical management of CRC. Other biomarkers, such as allelic imbalance at chromosome 18q[7-9], BRAF mutation[10,11], and p53 alterations[12,13], are not used in clinical practice due to the discrepancies among research reports. To better categorize CRC by biomarkers, more translational studies are warranted to identify putative biomarkers and validate them.
AT-rich interactive domain 1A (ARID1A) protein (BAF250a) is a member of the switching defective/sucrose non-fermenting (SWI/SNF) complexes, which function as ATP-dependent chromatin remodelers[14,15]. These complexes remodel nucleosomes and modulate transcription utilizing the energy of ATP hydrolysis. Inactivating mutations of several subunits of these complexes have frequently been detected in various tumors, indicating a tumor suppressor function of the SWI/SNF complexes[16-20].
Since late 2010, next-generation sequencing technologies have brought the emergence of a wide variety of cancer-associated gene mutations. Among them, inactivating mutations in ARID1A are frequently and repeatedly detected in various tumors. According to the reports, loss of ARID1A was detected in 30%-60% of ovarian clear cell and ovarian endometrioid carcinomas[18,21,22]. It was speculated that ARID1A loss mediated the transformation from endometriosis to cancer[18,23]. ARID1A loss has also been identified in some other cancers, such as endometrial cancer[24], clear cell renal cell carcinoma[25], breast cancer[26], Burkitt lymphoma[27], lung adenocarcinoma[28], neuroblastoma[29], hepatocellular carcinoma[30], and gastric cancer[31]. Related research in CRC is limited[32,33], thus we conducted this study to investigate the clinicopathologic and prognostic relevance of ARID1A loss in CRC.
MATERIALS AND METHODS
Ethics statement
All patients provided written informed consent for their information to be stored and used in the hospital database. Study approval was obtained from the independent ethics committee at the Cancer Center of Sun Yat-Sen University. The study was undertaken in accordance with the ethical standards of the World Medical Association Declaration of Helsinki.
Patient information and tissue specimens
This study was conducted using a total of 209 archived paraffin-embedded primary CRC samples. All patients underwent resection of primary tumors between 2001 and 2009 at Sun Yat-Sen University Cancer Center. All patients received standard post-operative chemotherapy according to the National Comprehensive Cancer Network guidelines. None of the patients had preoperative chemotherapy or preoperative radiotherapy. The staging of tumors was determined according to the American Joint Committee on Cancer (AJCC) TNM staging system. Each tumor was pathologically classified according to the World Health Organization classification criteria. For survival information, patients were followed-up by the follow-up department or the outpatient department after discharge from hospital. Overall survival (OS) was defined as the interval between the date of surgery and the date of death or the last known follow-up if the patient was alive. The clinicopathologic information of the study subjects and primary tumor samples are listed in Table 1. All excised samples were obtained from tumor tissues within 1 h after surgery. For each specimen, half was placed in liquid nitrogen until analysis, and the remainder was fixed with formalin for immunohistochemistry (IHC).
Table 1.
Clinicopathologic characteristics and AT-rich interactive domain 1A expression in 209 patient samples of colorectal cancer n (%)
| Characteristics | Value |
| Gender | |
| Male | 176 (84.2) |
| Female | 33 (15.8) |
| Age (yr) | |
| Median | 55 |
| Range | 19-88 |
| Tumor location | |
| Colon | 111 (53.1) |
| Rectal | 98 (46.9) |
| TNM stage (AJCC) | |
| I | 35 (16.7) |
| II | 48 (23.0) |
| III | 55 (26.3) |
| IV | 71 (34.0) |
| T stage | |
| T1 | 10 (4.8) |
| T2 | 35 (16.7) |
| T3 | 53 (25.4) |
| T4 | 111 (53.1) |
| N stage | |
| N0 | 98 (46.9) |
| N1 | 56 (26.8) |
| N2 | 55 (26.3) |
| M stage | |
| M0 | 138 (66.0) |
| M1 | 71 (34.0) |
| Pathologic differentiation | |
| Poor | 36 (17.2) |
| Moderate | 148 (70.8) |
| Well | 25 (12.0) |
| Tumor size (cm) | |
| ≤ 5 | 136 (65.1) |
| > 5 | 73 (34.9) |
| Expression of ARID1a | |
| Negative | 54 (25.8) |
| Positive | 155 (74.2) |
AJCC: American Joint Committee on Cancer; TNM: Tumor-node-metastasis; ARID1A: AT-rich interactive domain 1A.
IHC and scoring
The protein expression levels of ARID1A were investigated in 209 primary CRC samples using IHC. The procedure used was described previously[34]. Briefly, the tissue sections were first deparaffinized, rehydrated, endogenous peroxide blocked and antigen retrieved, then incubated with ARID1A (PSG3): sc-32761 antibody (Santa Cruz Biotechnology, Inc., CA, United States) overnight at 4 °C. Next, after washing with phosphate-buffered saline Tween-20, tissue sections were treated with anti-mouse secondary antibody for 30 min, followed by further incubation with the streptavidin horseradish peroxidase complex. The sections were developed with diaminobenzidine tetrahydrochloride and then counterstained with hematoxylin.
Two independent observers who were blinded to patient clinical and pathological information reviewed and scored the immunostained sections. At least 1000 tumor cells were analyzed for each slide. The proportion of the stained cells and the extent of staining were used as the criteria for evaluation. The percentage of positive cells was scored as ≤ 10% = 0, > 10% to ≤ 25% = 1, > 25% to ≤ 50% = 2, > 50% to ≤ 75% = 3, and > 75% = 4. Nuclear immunoreactivity was considered as positive expression. The intensity of staining was scored as negative = 0, weak = 1, moderate = 2, and strong = 3. The two scores were then multiplied to calculate the final score. Based on the overall score, the immunostained sections were further divided into two groups: negative ARID1A expression group (overall score = 0) and positive ARID1A expression group (overall score ≥ 1). The positive expression group was further divided into three groups: low ARID1A expression (1 ≤ overall score ≤ 4), moderate ARID1A expression (4 < overall score ≤ 8) and high ARID1A expression group (8 < overall score ≤ 12).
Statistical analysis
All statistical analyses were performed using SPSS 13.0 statistical software. A P value < 0.05 was considered statistically significant in all cases. The association between ARID1A expression and the clinicopathological characteristics was analyzed by χ2 test or Kruskal-Wallis H test based on the type of data. Survival curves were plotted by the Kaplan-Meier method and compared using the log-rank test. Survival data were evaluated using univariate and multivariate Cox regression analyses.
RESULTS
ARID1A expression in CRC primary tumors
IHC analysis was conducted on 209 primary CRC tumor samples. Fifty-four (25.8%) primary CRC tumors had negative ARID1A expression, 107 (51.2%) tumors had low ARID1A expression, 39 (18.7%) tumors had moderate ARID1A expression, and 9 (4.3%) tumors had high ARID1A expression. Typical immunostaining of negative, low, moderate and high ARID1A expression are shown in Figure 1.
Figure 1.
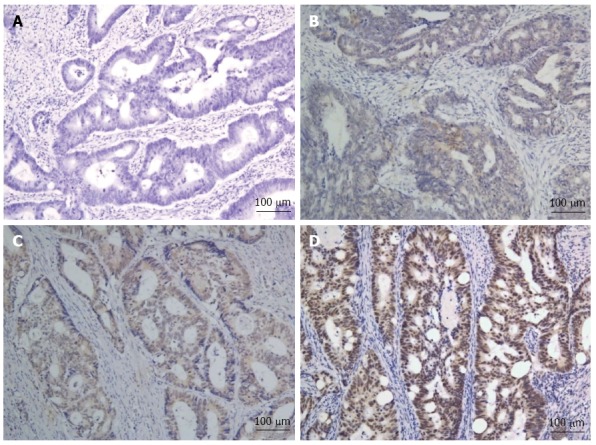
Typical immunohistochemical staining of AT-rich interactive domain 1A (× 100). A: Negative AT-rich interactive domain 1A (ARID1A) expression; B: Low ARID1A expression; C: Moderate ARID1A expression; D: High ARID1A expression.
Loss of ARID1A expression was associated with clinicopathological features of CRC
All 209 primary CRC tumors were included in this analysis. Fifty-four (25.8%) had negative ARID1A expression, and 155 (74.2%) cases had positive ARID1A expression. The correlations between ARID1A expression (negative/positive) and clinicopathological features of CRC are listed in Table 2. As shown in Table 2, loss of ARID1A expression was not associated with gender (male/female), age (≤ 55/> 55 years), tumor location (colon/rectal), T stage (T1/T2/T3/T4), N stage (N0/N1/N2), or tumor size (≤ 5/> 5 cm). However, the associations between ARID1A expression and TNM (AJCC) stage, M stage and pathologic differentiation were all statistically significant (P = 0.020, P = 0.026, and P = 0.035, respectively). Loss of ARID1A expression was significantly associated with late TNM stage, distant metastasis, and poor pathologic differentiation.
Table 2.
Correlation between AT-rich interactive domain 1A expression and clinicopathologic characteristics of colorectal cancer patients n (%)
| Characteristics |
ARID1a |
P value | |
| Negative | Positive | ||
| Gender | 0.132 | ||
| Male | 42 (77.8) | 134 (86.5) | |
| Female | 12 (22.2) | 21 (13.5) | |
| Age (yr) | 0.409 | ||
| ≤ 55 | 30 (55.6) | 76 (49.0) | |
| > 55 | 24 (44.4) | 79 (51.0) | |
| Tumor location | 0.293 | ||
| Colon | 32 (59.3) | 79 (51.0) | |
| Rectal | 22 (40.7) | 76 (49.0) | |
| TNM stage (AJCC) | 0.020 | ||
| I | 4 (7.4) | 31 (20.0) | |
| II | 13 (24.1) | 35 (22.6) | |
| III | 12 (22.2) | 43 (27.7) | |
| IV | 25 (46.3) | 46 (29.7) | |
| T stage | 0.771 | ||
| T1 | 1 (1.9) | 9 (5.8) | |
| T2 | 6 (11.1) | 29 (18.7) | |
| T3 | 20 (37.0) | 33 (21.3) | |
| T4 | 27 (50.0) | 84 (54.2) | |
| N stage | 0.638 | ||
| N0 | 23 (42.6) | 75 (48.4) | |
| N1 | 17 (31.5) | 39 (25.1) | |
| N2 | 14 (25.9) | 41 (26.5) | |
| M stage | 0.026 | ||
| M0 | 29 (53.7) | 109 (70.3) | |
| M1 | 25 (46.3) | 46 (29.7) | |
| Pathologic differentiation | 0.035 | ||
| Poor | 14 (25.9) | 22 (14.2) | |
| Moderate | 36 (66.7) | 112 (72.3) | |
| Well | 4 (7.4) | 21 (13.5) | |
| Tumor size (cm) | 0.170 | ||
| ≤ 5 | 31 (57.4) | 105 (67.7) | |
| > 5 | 23 (42.6) | 50 (32.3) | |
AJCC: American Joint Committee on Cancer; TNM: Tumor-node-metastasis; ARID1A: AT-rich interactive domain 1A.
Association between ARID1A loss and CRC survival
Kaplan-Meier analysis was used for the initial analysis of the influence of ARID1A loss on OS in CRC patients. ARID1A expression (negative/positive) was not associated with OS in all 209 CRC patients (P = 0.538). However, when the population was split by TNM stage, ARID1A expression (negative/positive) was significantly associated with OS in stage IV patients (P = 0.027, Figure 2), but a significant relationship was not observed in stage I-III patients. Thus, we further analyzed the association between ARID1A expression (negative/positive) and OS in stage IV patients. The results of univariate and multivariate analyses are listed in Table 3.
Figure 2.
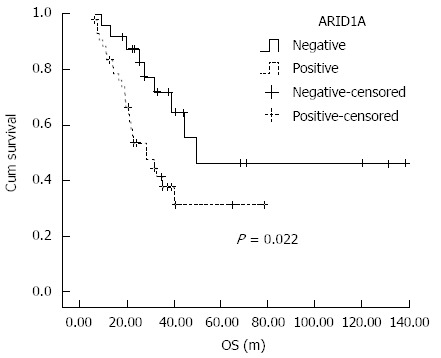
Kaplan-Meier curves. Kaplan-Meier curves with univariate analyses (log-rank) for stage IV patients with negative AT-rich interactive domain 1A (ARID1A) expression vs positive ARID1A expression.
Table 3.
Univariate and multivariate analyses of various prognostic parameters in stage IV patients with colorectal cancer using Cox-regression analysis n (%)
| Characteristics |
Univariate analysis |
Multivariate analysis |
|||
| P value | HR | 95%CI | P value | ||
| Gender | 0.258 | ||||
| Male | 40 (56.3) | ||||
| Female | 31 (43.7) | ||||
| Age (yr) | 0.934 | ||||
| ≤ 55 | 39 (54.9) | ||||
| > 55 | 32 (45.1) | ||||
| ARID1a expression | 0.027 | 2.49 | 1.13-5.51 | 0.024 | |
| Negative | 25 (35.2) | ||||
| Positive | 46 (64.8) | ||||
| T stage | 0.038 | 2.01 | 1.08-3.75 | 0.029 | |
| T1 | 1 (1.4) | ||||
| T2 | 5 (7.0) | ||||
| T3 | 43 (60.6) | ||||
| T4 | 22 (31.0) | ||||
| N stage | 0.929 | ||||
| N0 | 12 (16.9) | ||||
| N1 | 27 (38.0) | ||||
| N2 | 32 (45.1) | ||||
| Pathologic differentiation | 0.458 | ||||
| Poor | 17 (23.9) | ||||
| Moderate | 51 (71.8) | ||||
| Well | 3 (4.3) | ||||
| Tumor size (cm) | 0.261 | ||||
| ≤ 5 | 43 (60.6) | ||||
| > 5 | 28 (39.4) | ||||
| Metastatic site | 0.806 | ||||
| Single | 52 (73.2) | ||||
| Multiple | 19 (26.8) | ||||
| Metastasis limited to the liver | 0.519 | ||||
| No | 37 (52.1) | ||||
| Yes | 34 (47.9) | ||||
| Resection of metastatic tumors1 | 0.002 | 0.33 | 0.16-0.67 | 0.002 | |
| No | 21 (29.6) | ||||
| Yes | 50 (70.4) | ||||
Resection of metastasis: Including R0 and R1 resection of all metastatic tumors. ARID1A: AT-rich interactive domain 1A.
In stage IV CRC patients, potential prognostic factors, including N stage (N0/N1/N2), pathologic differentiation (poor/moderate/well), tumor size (≤ 5/> 5 cm), metastatic site (single/multiple), and metastasis limited to the liver (no/yes) were not found to be significantly prognostic. However, ARID1A expression (negative/positive), T stage (T1/T2/T3/T4) and resection of metastatic tumors (no/yes) were found to be significant prognostic factors in univariate analyses (P = 0.027, P = 0.038, and P = 0.002, respectively, Table 3). Factors significantly prognostic in univariate analysis were included in multivariate analysis. All three of the above factors were independent prognostic factors in multivariate analysis. Positive ARID1A expression was significantly and independently associated with worse OS in stage IV CRC patients compared with negative ARID1A expression (HR = 2.49, 95%CI: 1.13-5.51, Table 3). The Kaplan-Meier survival curves of ARID1A (negative/positive) for patients with stage IV CRC are shown in Figure 2.
DISCUSSION
In the present study, we demonstrated that loss of ARID1A expression was associated with late TNM stage, distant metastasis and poor pathologic differentiation. These findings indicated that ARID1A may play an important role in the progression of CRC. In addition, the survival analyses also indicated that loss of ARID1A protein expression was a prognostic factor for better OS in stage IV CRC.
Epigenetic regulators modulate gene expression, and thereby influence cell function. Alterations in epigenetic regulators have been shown to be one of the key characteristics in tumorigenesis[35]. Of these epigenetic regulators, the SWI/SNF chromatin remodeling complexes have been demonstrated to be repeatedly mutated in a wide range of carcinomas[36]. These complexes consist of several highly related multiunit complexes, and the occurrence of specific inactivating mutations in subunits were frequently authenticated, including the SNF5, BAF 180, BRM/SWI2-related gene 1, as well as ARID1A[36]. Functionally, ARID1A is required for nucleosome substrate binding and occupancy by SWI/SNF complexes[37]. Knockdown of ARID1A abrogates normal cell cycle arrest in osteoblasts cells, indicating the potential tumor suppressor function of ARID1A as well as the relevance of ARID1A loss and tumorigenesis[14]. In addition, Dykhuizen et al[38] discovered that SWI/SNF complexes were essential for the binding of topoisomerase IIalpha to approximately 12000 sites across the genome by directly interacting with topoisomerase IIalpha through ARID1A protein, which resulted in decatenation defects.
The tumor suppressor function of ARID1A has been verified in a wide variety of carcinomas, with significant research in gynecological carcinomas. There are few investigations regarding ARID1A in CRC, which requires further clarification. The mutation rate of ARID1A reported in CRC is low, and was reported by Jones et al[39] to be 10% and Kim et al[40] found no mutations. Thus, the importance of ARID1A loss in CRC may be underestimated. In our study, loss of ARID1A protein by IHC occurred in 25.8% of primary CRC tumors, with an even higher proportion of 35.2% in stage IV CRC, suggesting that loss of ARID1A was not uncommon in CRC. Moreover, loss of ARID1A was of clinicopathological significance.
There are a large number of reports on the relevance of ARID1A mutation or protein loss to survival in several carcinomas. However, there is controversy regarding the results of these studies. Some studies found that ARID1A mutation or protein loss was a predictor of worse survival in cervical cancer[41], and gastric cancer[42]. Others suggested no association between ARID1A mutation or protein loss and survival in clear cell carcinoma of the endometrium[43], and ovarian clear cell adenocarcinomas[22]. There are also reports indicating that ARID1A mutation or protein loss was related to a survival advantage in endometrial carcinoma[44] and gastric cancer[31]. Our study is the first to explore the influence of ARID1A loss on CRC survival. It was found that ARID1A loss predicted superior OS in stage IV CRC. ARID1A loss was also related to microsatellite instability (MSI) in endometrial cancer[45]. Previous research demonstrated that ARID1A mutation occurred more frequently in CRC with high MSI (MSI-H) compared with those with microsatellite stable CRC[32,40]. It was shown that MSI-H predicts better survival in early stage CRC[46]. In stage IV CRC, Liang et al[5] reported that MSI-H predicted better chemosensitivity to high-dose 5-fluorouracil plus leucovorin chemotherapy for stage IV sporadic colorectal cancer after palliative bowel resection. In our study, all stage IV patients underwent resection of primary CRC tumors. Thus, the survival advantage in patients with ARID1A loss may be partially explained by its association with MSI-H. However, one limitation of our study was that the status of MSI was not tested. Another was that the association between ARID1A loss and chemosensitivity in stage IV patients was not explored as only 21 (29.6%) cases did not receive metastatic tumor resection and had evaluable lesions. These associations need to be verified and the mechanisms clarified in future investigations.
Other limitations in our study were as follows: All stage IV patients underwent resection of primary tumors, thus those with a heavy tumor burden or poor performance status were not included. Therefore, the finding that ARID1A loss predicted better OS in stage IV CRC patients could only be applied to those with good performance status or low tumor burden. In addition, patients with early stage CRC and metastatic CRC received different drug regimens. The duration of our study was nine years from 2001-2009. During this period, the results of some clinical trials contributed to changes in clinical practice. Thus, even for patients with the same stage, their treatment was different. For these reasons, the associations between ARID1A loss and the effects of the chemotherapy and radiotherapy were not analyzed in this study.
In conclusion, ARID1A loss was not rare in CRC. It was associated with late TNM stage, distant metastasis, and poor pathologic differentiation. In addition, stage IV patients with ARID1A protein loss in primary tumors had longer survival than those with ARID1A positive tumors. ARID1A may be a candidate prognostic biomarker in CRC. In addition, considering that epigenetic alterations are potentially reversible, CRC patients with ARID1A loss may benefit from therapeutics which target chromatin-modifying enzymes.
ACKNOWLEDGMENTS
We thank Professor Liu Qing in the Epidemiology Department for his suggestions on the statistical analysis; and all the staff members in our department for their support and suggestions in this study.
COMMENTS
Background
AT-rich interactive domain 1A (ARID1A), a member of the switching defective/sucrose non-fermenting (SWI/SNF) complexes, has been shown to be mutated in many human cancers. However, studies on their clinical association in colorectal cancer are limited. The identification of new biomarkers is warranted to direct the categorization and treatment of colorectal cancer.
Research frontiers
ARID1A gene mutation has been repeatedly detected in many cancers, particularly in ovarian clear cell and ovarian endometrioid carcinomas. ARID1A loss is considered to be an important early event in the tumorigenic transformation from endometriosis to cancer. It was also found to be associated with microsatellite instability in endometrial cancer. ARID1A gene mutation was detected in colorectal cancer in previous studies, however, the association between ARID1A protein loss by immunohistochemistry and both clinicopathologic characteristics and prognosis in colorectal cancer is unclear.
Innovations and breakthroughs
The authors found that ARID1A loss was not rare in primary colorectal cancer tumors (25.8%), and was associated with late TNM stage, distant metastasis, and poor pathological classification in patients with colorectal cancer. However, ARID1A loss predicted better overall survival in stage IV patients.
Applications
This study indicated an important role for ARID1A protein loss in colorectal cancer. ARID1A protein loss was found to be associated with late TNM stage, distant metastasis and poor pathological differentiation, suggesting that it might play a role in the progression of colorectal cancer. However, in stage IV patients, ARID1A loss was found to predict better survival. This could partially be explained by its association with microsatellite instability. Further studies are needed to clarify the detailed mechanisms involved.
Terminology
ARID1A, also known as BAF250a, is a member of the SWI/SNF complexes, which function as ATP-dependent chromatin remodelers. The SWI/SNF complexes remodel nucleosomes and modulate transcription utilizing the energy of ATP hydrolysis.
Peer review
This study demonstrated the clinical association of ARID1A protein loss by immunohistochemistry in colorectal cancer. ARID1A protein loss was found to be related with late TNM stage, distant metastasis and poor pathological differentiation. In addition, it was found to predict better survival in stage IV patients.
Footnotes
Supported by National High Technology Research and Development Program of China (863 Program), No. 2012AA02A506; National Natural Science Foundation of China, No. 81372570; the Science and Technology Foundation of Guangdong Province, China, No. 2012B031800088; and the Science and Technology Foundation of Guangdong Province, China, No. C2011019
P- Reviewer: de Bree E, De Re V, Patanè S S- Editor: Gou SX L- Editor: Webster JR E- Editor: Wang CH
References
- 1.Mellas N, Benbrahim Z, El Mesbahi O. Colorectal cancer: new developments after the 2013 ECCO/ESMO congress. Chin J Cancer. 2014;33:218–221. doi: 10.5732/cjc.013.10203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang DZ, Kumar V, Ma Y, Li K, Kopetz S. Individualized therapies in colorectal cancer: KRAS as a marker for response to EGFR-targeted therapy. J Hematol Oncol. 2009;2:18. doi: 10.1186/1756-8722-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 4.Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem J, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369:1023–1034. doi: 10.1056/NEJMoa1305275. [DOI] [PubMed] [Google Scholar]
- 5.Liang JT, Huang KC, Lai HS, Lee PH, Cheng YM, Hsu HC, Cheng AL, Hsu CH, Yeh KH, Wang SM, et al. High-frequency microsatellite instability predicts better chemosensitivity to high-dose 5-fluorouracil plus leucovorin chemotherapy for stage IV sporadic colorectal cancer after palliative bowel resection. Int J Cancer. 2002;101:519–525. doi: 10.1002/ijc.10643. [DOI] [PubMed] [Google Scholar]
- 6.Hemminki A, Mecklin JP, Järvinen H, Aaltonen LA, Joensuu H. Microsatellite instability is a favorable prognostic indicator in patients with colorectal cancer receiving chemotherapy. Gastroenterology. 2000;119:921–928. doi: 10.1053/gast.2000.18161. [DOI] [PubMed] [Google Scholar]
- 7.Jen J, Kim H, Piantadosi S, Liu ZF, Levitt RC, Sistonen P, Kinzler KW, Vogelstein B, Hamilton SR. Allelic loss of chromosome 18q and prognosis in colorectal cancer. N Engl J Med. 1994;331:213–221. doi: 10.1056/NEJM199407283310401. [DOI] [PubMed] [Google Scholar]
- 8.Ogino S, Nosho K, Irahara N, Shima K, Baba Y, Kirkner GJ, Meyerhardt JA, Fuchs CS. Prognostic significance and molecular associations of 18q loss of heterozygosity: a cohort study of microsatellite stable colorectal cancers. J Clin Oncol. 2009;27:4591–4598. doi: 10.1200/JCO.2009.22.8858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carethers JM, Hawn MT, Greenson JK, Hitchcock CL, Boland CR. Prognostic significance of allelic lost at chromosome 18q21 for stage II colorectal cancer. Gastroenterology. 1998;114:1188–1195. doi: 10.1016/s0016-5085(98)70424-x. [DOI] [PubMed] [Google Scholar]
- 10.Ogino S, Nosho K, Kirkner GJ, Kawasaki T, Meyerhardt JA, Loda M, Giovannucci EL, Fuchs CS. CpG island methylator phenotype, microsatellite instability, BRAF mutation and clinical outcome in colon cancer. Gut. 2009;58:90–96. doi: 10.1136/gut.2008.155473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bardelli A, Siena S. Molecular mechanisms of resistance to cetuximab and panitumumab in colorectal cancer. J Clin Oncol. 2010;28:1254–1261. doi: 10.1200/JCO.2009.24.6116. [DOI] [PubMed] [Google Scholar]
- 12.Munro AJ, Lain S, Lane DP. P53 abnormalities and outcomes in colorectal cancer: a systematic review. Br J Cancer. 2005;92:434–444. doi: 10.1038/sj.bjc.6602358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iacopetta B, Russo A, Bazan V, Dardanoni G, Gebbia N, Soussi T, Kerr D, Elsaleh H, Soong R, Kandioler D, et al. Functional categories of TP53 mutation in colorectal cancer: results of an International Collaborative Study. Ann Oncol. 2006;17:842–847. doi: 10.1093/annonc/mdl035. [DOI] [PubMed] [Google Scholar]
- 14.Nagl NG, Patsialou A, Haines DS, Dallas PB, Beck GR, Moran E. The p270 (ARID1A/SMARCF1) subunit of mammalian SWI/SNF-related complexes is essential for normal cell cycle arrest. Cancer Res. 2005;65:9236–9244. doi: 10.1158/0008-5472.CAN-05-1225. [DOI] [PubMed] [Google Scholar]
- 15.Wang X, Nagl NG, Wilsker D, Van Scoy M, Pacchione S, Yaciuk P, Dallas PB, Moran E. Two related ARID family proteins are alternative subunits of human SWI/SNF complexes. Biochem J. 2004;383:319–325. doi: 10.1042/BJ20040524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Versteege I, Sévenet N, Lange J, Rousseau-Merck MF, Ambros P, Handgretinger R, Aurias A, Delattre O. Truncating mutations of hSNF5/INI1 in aggressive paediatric cancer. Nature. 1998;394:203–206. doi: 10.1038/28212. [DOI] [PubMed] [Google Scholar]
- 17.Varela I, Tarpey P, Raine K, Huang D, Ong CK, Stephens P, Davies H, Jones D, Lin ML, Teague J, Bignell G, Butler A, Cho J, Dalgliesh GL, Galappaththige D, Greenman C, Hardy C, Jia M, Latimer C, Lau KW, Marshall J, McLaren S, Menzies A, Mudie L, Stebbings L, Largaespada DA, Wessels LF, Richard S, Kahnoski RJ, Anema J, Tuveson DA, Perez-Mancera PA, Mustonen V, Fischer A, Adams DJ, Rust A, Chan-on W, Subimerb C, Dykema K, Furge K, Campbell PJ, Teh BT, Stratton MR, Futreal PA. Exome sequencing identifies frequent mutation of the SWI/SNF complex gene PBRM1 in renal carcinoma. Nature. 2011;469:539–542. doi: 10.1038/nature09639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiegand KC, Shah SP, Al-Agha OM, Zhao Y, Tse K, Zeng T, Senz J, McConechy MK, Anglesio MS, Kalloger SE, et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010;363:1532–1543. doi: 10.1056/NEJMoa1008433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong AK, Shanahan F, Chen Y, Lian L, Ha P, Hendricks K, Ghaffari S, Iliev D, Penn B, Woodland AM, et al. BRG1, a component of the SWI-SNF complex, is mutated in multiple human tumor cell lines. Cancer Res. 2000;60:6171–6177. [PubMed] [Google Scholar]
- 20.Reisman DN, Sciarrotta J, Wang W, Funkhouser WK, Weissman BE. Loss of BRG1/BRM in human lung cancer cell lines and primary lung cancers: correlation with poor prognosis. Cancer Res. 2003;63:560–566. [PubMed] [Google Scholar]
- 21.Maeda D, Mao TL, Fukayama M, Nakagawa S, Yano T, Taketani Y, Shih IeM. Clinicopathological significance of loss of ARID1A immunoreactivity in ovarian clear cell carcinoma. Int J Mol Sci. 2010;11:5120–5128. doi: 10.3390/ijms11125120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yamamoto S, Tsuda H, Takano M, Tamai S, Matsubara O. PIK3CA mutations and loss of ARID1A protein expression are early events in the development of cystic ovarian clear cell adenocarcinoma. Virchows Arch. 2012;460:77–87. doi: 10.1007/s00428-011-1169-8. [DOI] [PubMed] [Google Scholar]
- 23.Yamamoto S, Tsuda H, Takano M, Tamai S, Matsubara O. Loss of ARID1A protein expression occurs as an early event in ovarian clear-cell carcinoma development and frequently coexists with PIK3CA mutations. Mod Pathol. 2012;25:615–624. doi: 10.1038/modpathol.2011.189. [DOI] [PubMed] [Google Scholar]
- 24.Liang H, Cheung LW, Li J, Ju Z, Yu S, Stemke-Hale K, Dogruluk T, Lu Y, Liu X, Gu C, et al. Whole-exome sequencing combined with functional genomics reveals novel candidate driver cancer genes in endometrial cancer. Genome Res. 2012;22:2120–2129. doi: 10.1101/gr.137596.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lichner Z, Scorilas A, White NM, Girgis AH, Rotstein L, Wiegand KC, Latif A, Chow C, Huntsman D, Yousef GM. The chromatin remodeling gene ARID1A is a new prognostic marker in clear cell renal cell carcinoma. Am J Pathol. 2013;182:1163–1170. doi: 10.1016/j.ajpath.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Mamo A, Cavallone L, Tuzmen S, Chabot C, Ferrario C, Hassan S, Edgren H, Kallioniemi O, Aleynikova O, Przybytkowski E, et al. An integrated genomic approach identifies ARID1A as a candidate tumor-suppressor gene in breast cancer. Oncogene. 2012;31:2090–2100. doi: 10.1038/onc.2011.386. [DOI] [PubMed] [Google Scholar]
- 27.Love C, Sun Z, Jima D, Li G, Zhang J, Miles R, Richards KL, Dunphy CH, Choi WW, Srivastava G, et al. The genetic landscape of mutations in Burkitt lymphoma. Nat Genet. 2012;44:1321–1325. doi: 10.1038/ng.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imielinski M, Berger AH, Hammerman PS, Hernandez B, Pugh TJ, Hodis E, Cho J, Suh J, Capelletti M, Sivachenko A, et al. Mapping the hallmarks of lung adenocarcinoma with massively parallel sequencing. Cell. 2012;150:1107–1120. doi: 10.1016/j.cell.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sausen M, Leary RJ, Jones S, Wu J, Reynolds CP, Liu X, Blackford A, Parmigiani G, Diaz LA, Papadopoulos N, et al. Integrated genomic analyses identify ARID1A and ARID1B alterations in the childhood cancer neuroblastoma. Nat Genet. 2013;45:12–17. doi: 10.1038/ng.2493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fujimoto A, Totoki Y, Abe T, Boroevich KA, Hosoda F, Nguyen HH, Aoki M, Hosono N, Kubo M, Miya F, et al. Whole-genome sequencing of liver cancers identifies etiological influences on mutation patterns and recurrent mutations in chromatin regulators. Nat Genet. 2012;44:760–764. doi: 10.1038/ng.2291. [DOI] [PubMed] [Google Scholar]
- 31.Wang K, Kan J, Yuen ST, Shi ST, Chu KM, Law S, Chan TL, Kan Z, Chan AS, Tsui WY, et al. Exome sequencing identifies frequent mutation of ARID1A in molecular subtypes of gastric cancer. Nat Genet. 2011;43:1219–1223. doi: 10.1038/ng.982. [DOI] [PubMed] [Google Scholar]
- 32.Cajuso T, Hänninen UA, Kondelin J, Gylfe AE, Tanskanen T, Katainen R, Pitkänen E, Ristolainen H, Kaasinen E, Taipale M, et al. Exome sequencing reveals frequent inactivating mutations in ARID1A, ARID1B, ARID2 and ARID4A in microsatellite unstable colorectal cancer. Int J Cancer. 2014;135:611–623. doi: 10.1002/ijc.28705. [DOI] [PubMed] [Google Scholar]
- 33.Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–337. doi: 10.1038/nature11252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teng KY, Qiu MZ, Li ZH, Luo HY, Zeng ZL, Luo RZ, Zhang HZ, Wang ZQ, Li YH, Xu RH. DNA polymerase η protein expression predicts treatment response and survival of metastatic gastric adenocarcinoma patients treated with oxaliplatin-based chemotherapy. J Transl Med. 2010;8:126. doi: 10.1186/1479-5876-8-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 36.Wilson BG, Roberts CW. SWI/SNF nucleosome remodellers and cancer. Nat Rev Cancer. 2011;11:481–492. doi: 10.1038/nrc3068. [DOI] [PubMed] [Google Scholar]
- 37.Chandler RL, Brennan J, Schisler JC, Serber D, Patterson C, Magnuson T. ARID1a-DNA interactions are required for promoter occupancy by SWI/SNF. Mol Cell Biol. 2013;33:265–280. doi: 10.1128/MCB.01008-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dykhuizen EC, Hargreaves DC, Miller EL, Cui K, Korshunov A, Kool M, Pfister S, Cho YJ, Zhao K, Crabtree GR. BAF complexes facilitate decatenation of DNA by topoisomerase IIα. Nature. 2013;497:624–627. doi: 10.1038/nature12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones S, Li M, Parsons DW, Zhang X, Wesseling J, Kristel P, Schmidt MK, Markowitz S, Yan H, Bigner D, et al. Somatic mutations in the chromatin remodeling gene ARID1A occur in several tumor types. Hum Mutat. 2012;33:100–103. doi: 10.1002/humu.21633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim MS, Je EM, Yoo NJ, Lee SH. Loss of ARID1A expression is uncommon in gastric, colorectal, and prostate cancers. APMIS. 2012;120:1020–1022. doi: 10.1111/j.1600-0463.2012.02930.x. [DOI] [PubMed] [Google Scholar]
- 41.Cho H, Kim JS, Chung H, Perry C, Lee H, Kim JH. Loss of ARID1A/BAF250a expression is linked to tumor progression and adverse prognosis in cervical cancer. Hum Pathol. 2013;44:1365–1374. doi: 10.1016/j.humpath.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 42.Wang DD, Chen YB, Pan K, Wang W, Chen SP, Chen JG, Zhao JJ, Lv L, Pan QZ, Li YQ, et al. Decreased expression of the ARID1A gene is associated with poor prognosis in primary gastric cancer. PLoS One. 2012;7:e40364. doi: 10.1371/journal.pone.0040364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fadare O, Gwin K, Desouki MM, Crispens MA, Jones HW, Khabele D, Liang SX, Zheng W, Mohammed K, Hecht JL, et al. The clinicopathologic significance of p53 and BAF-250a (ARID1A) expression in clear cell carcinoma of the endometrium. Mod Pathol. 2013;26:1101–1110. doi: 10.1038/modpathol.2013.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Allo G, Bernardini MQ, Wu RC, Shih IeM, Kalloger S, Pollett A, Gilks CB, Clarke BA. ARID1A loss correlates with mismatch repair deficiency and intact p53 expression in high-grade endometrial carcinomas. Mod Pathol. 2014;27:255–261. doi: 10.1038/modpathol.2013.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bosse T, ter Haar NT, Seeber LM, v Diest PJ, Hes FJ, Vasen HF, Nout RA, Creutzberg CL, Morreau H, Smit VT. Loss of ARID1A expression and its relationship with PI3K-Akt pathway alterations, TP53 and microsatellite instability in endometrial cancer. Mod Pathol. 2013;26:1525–1535. doi: 10.1038/modpathol.2013.96. [DOI] [PubMed] [Google Scholar]
- 46.Gavin PG, Colangelo LH, Fumagalli D, Tanaka N, Remillard MY, Yothers G, Kim C, Taniyama Y, Kim SI, Choi HJ, et al. Mutation profiling and microsatellite instability in stage II and III colon cancer: an assessment of their prognostic and oxaliplatin predictive value. Clin Cancer Res. 2012;18:6531–6541. doi: 10.1158/1078-0432.CCR-12-0605. [DOI] [PMC free article] [PubMed] [Google Scholar]


