Abstract
Intestinal obstruction is a common clinical entity encountered in surgical practice. The objective of this report is to corroborate an atypical scenario of intestinal obstruction in a Chinese patient and to focus on the diagnosis and treatment. A 27-year-old male presented with a history of gastric pain combined with nausea and abdominal distension that had been present for 5 d. The presence of a foreign body was detected by computed tomography and observed as an abnormal density within the stomach. A diospyrobezoar was revealed during gastroscopy, the extraction of which was prevented due to its size and firmness. An endoscopic holmium laser joined with a snare was used to fragment the obstruction, which was followed by management with a conservative “sandwich” treatment strategy involving intestinal decompression with an ileus tube and Coca-Cola lavage between endoscopic lithotripsy fragmentation procedures. This strategy resulted in the successful removal of the diospyrobezoar along with multiple small bowel obstructions. The patient was discharged after abatement of symptoms. The case presented here demonstrates the implementation of a conservative, yet successful, treatment as an alternative to conventional surgical removal of intestinal obstructions.
Keywords: Small bowel obstruction, Diospyrobezoar, Ileus tube, Holmium laser, Endoscopy
Core tip: This case report presents the treatment of an intestinal obstruction using a conservative alternative to surgical therapy. A patient presented with signs of intestinal obstruction, which was confirmed by radiography. A diospyrobezoar was revealed during gastroscopy that was not extractable due to its size and firmness. The obstruction was successfully managed following holium laser fragmentation using a “sandwich” strategy of ileal tube decompression and Coca-Cola lavage between two endoscopic lithotripsy procedures. This treatment strategy should therefore be considered in place of surgical intervention for the treatment of intestinal obstructions.
INTRODUCTION
Bezoars are calculi or other hard types of matter found within the gastrointestinal tract and are commonly accompanied by delayed gastric emptying in individuals who have undergone stomach surgery[1]. There are numerous etiological aspects related to bezoar formation, including sparse chewing, high-fiber diets, and long-term constipation, which are common in elderly patients with inadequate food intake[2]. Moreover, prior surgical stomach procedures, such as reduced acid secretion after vagotomy[3], are considered to be pathogenic factors for bezoar formation. Diospyrobezoars, formed from undigested persimmons, are stiffer than other classes of phytobezoars, and can be resistant to medications, requiring endoscopic or surgical removal[4,5]. The case presented here describes the diagnosis and treatment of a Chinese patient with a rare intestinal diospyrobezoar obstruction.
CASE REPORT
A 27-year-old male presented to our emergency room with a 5-d history of upper abdominal pain. The patient had experienced nausea and distension that worsened with ingestion of any type of food. He reported no loss of weight or appetite, though his bowel habits were altered, with no signs of rectal bleeding. The patient reported excessive ingestion of persimmons two weeks prior.
On physical examination, the patient was mildly dehydrated with a blood pressure of 108/74 mmHg and a heartbeat of 103 beats/min. Abdominal distension coupled with pain on diffuse palpation without signs of peritoneal irritation were witnessed. Bowel sounds were active, and no palpable mass was present upon rectal examination. Abnormal laboratory values included a white blood cell count of 10.8 × 103 cells/μL and glucose level of 120 mg/dL. An abdominal radiograph revealed two substantially dilated small bowel curls with gas-fluid levels and fold thickening on the left side of the abdomen (Figure 1A), and an obstruction was located in the pelvic jejunum by computed tomography (Figure 1B). The radiologist confirmed the presence of a gastrolith by the abnormal density within the stomach together with the clinical indications for intestinal obstruction.
Figure 1.
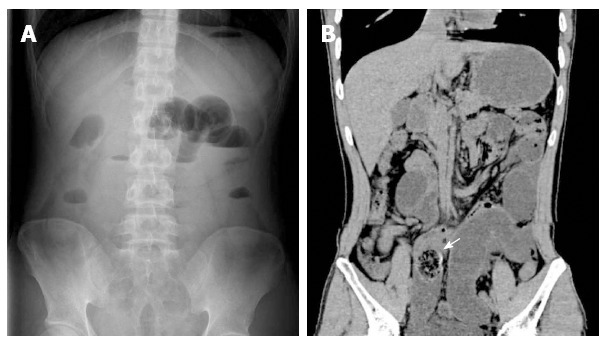
Radiologic findings. A: Plain abdominal radiograph showed gas-fluid levels on left side of the abdomen; B: Computed tomography scan revealed a low intestinal obstruction (white arrow).
A gastroscopy was performed and revealed a greenish, semisolid mass, 5 cm × 6 cm in size (Figure 2A). An initial attempt to extract the gastrolith failed due to its size and firmness. Endoscopy with a holmium:yttrium-aluminum-garnet (Ho:YAG) laser with a snare was then employed with the patient under anesthesia. The stomach was filled with normal saline until the bezoar was submerged, and the Ho:YAG laser was applied to the outer layer of the bezoar. An endoscopic trap was subsequently embedded through the accessory hole to extract the fragmented part. At the end of the procedure, 30 mL of Coca-Cola (Coca-Cola Co., Shanghai, China) was imbued to the mass at intervals. A 3 m CLINY ileus tube (Create Medic, Tokyo, Japan) was positioned through the biopsy forceps into the jejunum to decompress the intestine. The endoscopic procedure lasted approximately 60 min with no complications.
Figure 2.
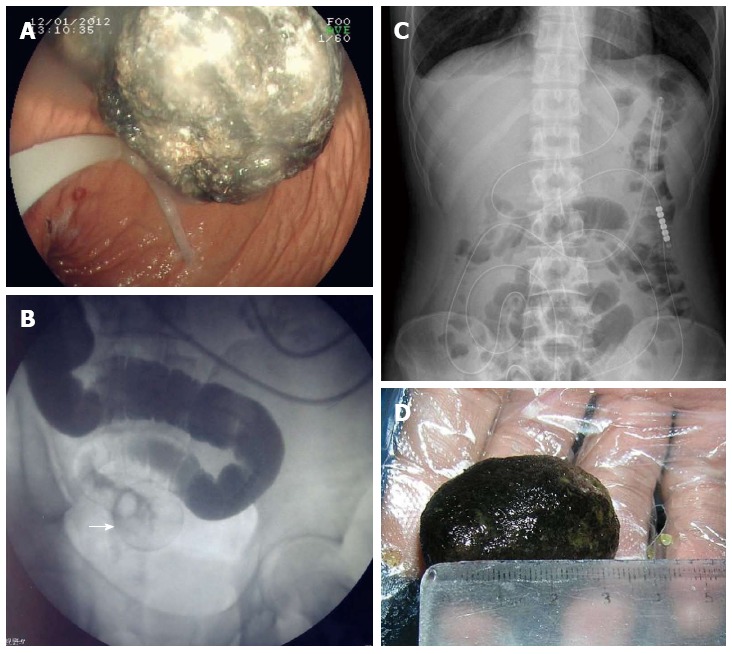
Treatment procedures. A: A greenish, semisolid mass in the stomach observed on gastroscopy; B: Imaging revealed slight expansion of the intestine and dislodgement at a round point (white arrow); C: No air-fluid level was observed on plain abdominal radiograph two days later; D: Image of the discharged diospyrobezoar.
Over the following 2 d, the patient’s symptoms resolved. After 48 h, imaging of the small intestine with gastrografin via the long tube revealed slight expansion of the intestine (Figure 2B). Coca-Cola (50 mL) was then administered through the drainage hole of the tube every 6 h according to the method described by Kato et al[6]. 2 d later, no air-fluid level was observed on a plain abdominal X-ray (Figure 2C). The next day, before the tube was pulled, the patient discharged a hard 3.5 cm × 2.5 cm stone in the stool (Figure 2D).
The patient was advised to maintain a liquid diet with plenty of fluids following the procedure, including a can of Coca-Cola with meals. The phytobezoar remnant was entirely eliminated through an endoscopic trap, which was observed during the second gastroscopy examination one week later. The patient was discharged following complete cessation of symptoms and urged to avoid future ingestion of food items that can lead to phytobezoar formation.
DISCUSSION
The patient in the present case presented with an intestinal obstruction following ingestion of persimmons, which are known to cause diospyrobezoars. Laser destruction via an endoscope and endoscopically-directed suction removal has been demonstrated as beneficial in dealing with phytobezoars and diospyrobezoars[7,8]. Moreover, gastric lavage utilizing NaHCO3 highlights a mucolytic effect for the management of diospyrobezoars, and penetration of CO2 bubbles can aid in their digestion[9]. Remarkably, nasogastric lavage with Coca-Cola has been reported as an effective strategy for treatment of gastric diospyrobezoars[6]. Although the mechanism is not clear, the carbonic and phosphoric acidity of Coca-Cola (pH 2.6) resembles gastric acid, which is considered vital for dietary fiber digestion[10]. Two studies of 5 patients have found no signs of recurrence by endoscopic evaluation after 3 to 15 mo following the preliminary therapy with Coca-Cola[11-13].
A conservative treatment with close monitoring was implemented in the present case to avoid potential catastrophic events. The bezoars in the stomach were first split using a Ho:YAG laser, and gradual fragmentation of these segments was accomplished by endoscopic trap to acquire tiny remnants (about nine fragments of 0.5-1 cm2) that might effortlessly pass along the intestinal tract. The small bowel obstructions in our case also appeared to be caused by migration of gastric bezoars. The diospyrobezoars were successfully dealt with by endoscopic injection of Coca-Cola with a long tube providing intestinal decompression “sandwiched” in between two endoscopic lithotripsy processes. This method proved to be easy, efficient and economical, and thus should be considered as a conservative approach for bezoar removal rather than surgical intervention.
Patients may be treated by surgical resections utilizing either open or laparoscopic strategy when entangled with small bowel obstructions, gastric perforation or stomach hemorrhage. Endoscopic techniques can be remunerative and reliable for treatment of bezoar-induced small bowel obstructions in comparison to a conventional approach[10]. However, the “sandwich” strategy described here is a useful way to avoid operative intervention if the endoscopic approach is not successful. The case presented herein describes an effective “sandwich” treatment comprised of integrated endoscopic fragmentation plus intestinal decompression with an ileus tube and Coca-Cola lavage. Our results foster an interest for supplemental prospective evaluation of this strategy in place of conventional treatments such as surgery.
COMMENTS
Case characteristics
The patient presented with abdominal distension with pain on diffuse palpation without peritoneal irritation.
Clinical diagnosis
Intestinal obstruction due to phytobezoar.
Differential diagnosis
Intestinal obstruction.
Laboratory diagnosis
Laboratory values included a white blood cell count of 10.8 × 103 cells/µL and a glucose level of 120 mg/dL. Other standard blood results were within the normal ranges.
Imaging diagnosis
A low intestinal obstruction due to foreign body was revealed by computed tomography. The presence of a gastrolith was confirmed by the abnormal density within the stomach observed on radiology coupled with the clinical signs indicative of intestinal obstruction.
Treatment
Endoscopic fragmentation with a holmium:yttrium-aluminum-garnet laser followed by a “sandwich” strategy comprised of intestinal decompression with an ileus tube and Coca-Cola lavage between endoscopic lithotripsy procedures.
Experiences and lessons
Phytobezoars can be conservatively treated using integrated techniques, such as the laser fragmentation, ileal tube decompression and Coca-Cola lavage described in this case.
Peer review
In this case, the authors describe the successful use of a conservative “sandwich” technique to remove a large diospyrobezoar from the small intestine. This case demonstrates that conventional surgical approaches may be replaced by an easy, efficient and economical treatment for intestinal obstruction.
Footnotes
Supported by Projects of Administration of Traditional Chinese Medicine of Zhejiang Province, No. 2012ZA084
P- Reviewer: Vasilescu A S- Editor: Nan J L- Editor: A E- Editor: Wang CH
References
- 1.Cifuentes Tebar J, Robles Campos R, Parrilla Paricio P, Lujan Mompean JA, Escamilla C, Liron Ruiz R, Pellicer Franco EM. Gastric surgery and bezoars. Dig Dis Sci. 1992;37:1694–1696. doi: 10.1007/BF01299861. [DOI] [PubMed] [Google Scholar]
- 2.Verstandig AG, Klin B, Bloom RA, Hadas I, Libson E. Small bowel phytobezoars: detection with radiography. Radiology. 1989;172:705–707. doi: 10.1148/radiology.172.3.2772176. [DOI] [PubMed] [Google Scholar]
- 3.Delpre G, Neeman A, Kadish U. Postoperative bezoars (persimmon and others): further considerations. Gastroenterology. 1983;85:1456. [PubMed] [Google Scholar]
- 4.Rozen P, Gilat T. Enzymatic softening and endoscopic destruction of a phytobezoar in an unoperated stomach. Am J Gastroenterol. 1975;64:397–399. [PubMed] [Google Scholar]
- 5.Walker-Renard P. Update on the medicinal management of phytobezoars. Am J Gastroenterol. 1993;88:1663–1666. [PubMed] [Google Scholar]
- 6.Kato H, Nakamura M, Orito E, Ueda R, Mizokami M. The first report of successful nasogastric Coca-Cola lavage treatment for bitter persimmon phytobezoars in Japan. Am J Gastroenterol. 2003;98:1662–1663. doi: 10.1111/j.1572-0241.2003.07563.x. [DOI] [PubMed] [Google Scholar]
- 7.Naveau S, Poynard T, Zourabichvili O, Poitrine A, Chaput JC. Gastric phytobezoar destruction by Nd: YAG laser therapy. Gastrointest Endosc. 1986;32:430–431. doi: 10.1016/s0016-5107(86)71938-x. [DOI] [PubMed] [Google Scholar]
- 8.Blam ME, Lichtenstein GR. A new endoscopic technique for the removal of gastric phytobezoars. Gastrointest Endosc. 2000;52:404–408. doi: 10.1067/mge.2000.108407. [DOI] [PubMed] [Google Scholar]
- 9.Saeed ZA, Rabassa AA, Anand BS. An endoscopic method for removal of duodenal phytobezoars. Gastrointest Endosc. 1995;41:74–76. doi: 10.1016/s0016-5107(95)70282-2. [DOI] [PubMed] [Google Scholar]
- 10.McCloy RF, Greenberg GR, Baron JH. Duodenal pH in health and duodenal ulcer disease: effect of a meal, Coca-Cola, smoking, and cimetidine. Gut. 1984;25:386–392. doi: 10.1136/gut.25.4.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol. 2002;14:801–803. doi: 10.1097/00042737-200207000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Lin CS, Tung CF, Peng YC, Chow WK, Chang CS, Hu WH. Successful treatment with a combination of endoscopic injection and irrigation with coca cola for gastric bezoar-induced gastric outlet obstruction. J Chin Med Assoc. 2008;71:49–52. doi: 10.1016/S1726-4901(08)70073-X. [DOI] [PubMed] [Google Scholar]
- 13.Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis I. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther. 2013;37:169–173. doi: 10.1111/apt.12141. [DOI] [PubMed] [Google Scholar]


