Abstract
Myelodysplastic syndromes (MDS) are a group of clonal disorders arising from hematopoietic stem cells generally characterized by inefficient hematopoiesis, dysplasia in one or more myeloid cell lineages, and variable degrees of cytopenias. Most MDS patients are diagnosed in their late 60s to early 70s. The estimated incidence of MDS in the United States and in Europe are 4.3 and 1.8 per 100,000 individuals per year, respectively with lower rates reported in some Asian countries and less well estimated in other parts of the world. Evolution to acute myeloid leukemia can occur in 10-15% of MDS patients. Three drugs are currently approved for the treatment of patients with MDS: immunomodulatory agents (lenalidomide), and hypomethylating therapy [HMT (decitabine and 5-azacytidine)]. All patients will eventually lose their response to therapy, and the survival outcome of MDS patients is poor (median survival of 4.5 months) especially for patients who fail (refractory/relapsed) HMT. The only potential curative treatment for MDS is hematopoietic cell transplantation. Genomic/chromosomal instability and various mechanisms contribute to the pathogenesis and prognosis of the disease. High throughput genetic technologies like single nucleotide polymorphism array analysis and next generation sequencing technologies have uncovered novel genetic alterations and increased our knowledge of MDS pathogenesis. We will review various genetic and non-genetic causes that are involved in the pathogenesis of MDS.
Keywords: MDS, Molecular mutation, Pathogenesis
INTRODUCTION
1. Overview of myelodysplastic syndromes
Myelodysplastic syndromes (MDS) are clonal stem cell malignancies characterized by cytopenias, inefficient hematopoiesis, dysplasia in one or more myeloid cell lineages and increased risk of development of acute myeloid leukemia (AML). It is sub-classified based on percent of bone marrow (BM) and peripheral blood blasts, type/degree and number of dysplastic cell lineages, presence/absence of ring sideroblasts (RS) and presence of specific chromosomal abnormalities. The median age at the diagnosis of MDS is 71 years [1, 2]. Treatment options for MDS patients vary based on the disease severity. Transfusions, growth factors, and antibiotic therapy are part of the supportive care that is usually suggested for low-risk MDS patients. Chemotherapy regimens like hypomethylating therapy (HMT; decitabine and 5-azacytidine), immunomodulatory agents (lenalidomide), cytarabine, idarubicin, and daunorubicin are commonly used in high-risk MDS patients to delay the AML transformation. Ultimately, long term remission is achieved by using high dose chemotherapy and hematopoietic stem cell (HSC) transplantation.
Genetic defects (chromosomal aberrations, gene mutations, copy-number alterations, abnormal gene expression) are common in MDS. Clonal and recurrent cytogenetic abnormalities and their frequency are summarized in Table 1. They are often present at disease presentation; however abnormal clones can appear during the disease course and are associated with worsening conditions. Genomic instability (deletions, translocations) is important since these genetic events can encompass regions containing tumor suppressor genes (TSGs) relevant to MDS biology. Unbalanced translocations are found in ~50% of primary and 80% of therapy-related MDS (t-MDS) cases [3, 4]. Complex karyotype (3 or more defects) is usually correlated with dismal outcomes and can be seen following chemo/radiotherapy and toxic chemicals exposure. The recently published Revised International Prognostic Scoring System (R-IPSS) includes more specific cytogenetic prognostic subgroups to improve prognostic stratification in MDS [5].
Table 1.
Clonal recurrent cytogenetic abnormalities and their frequency in myelodysplastic syndrome.
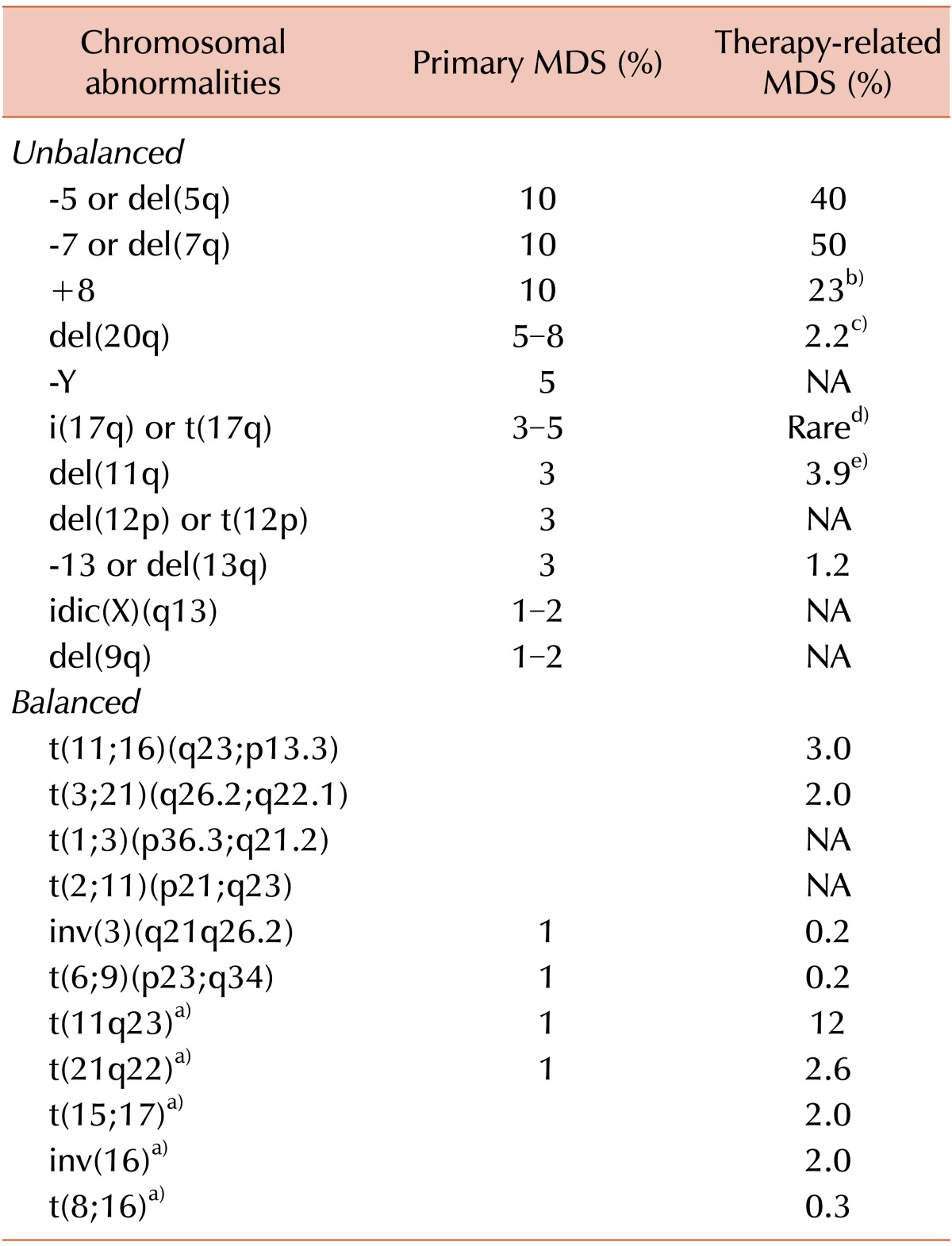
a)This frequency was reported by Smith et al. [121]. b)Data are extrapolated by Koh et al. [122]. c)The frequency was reported in Mauritzson et al. [123]. d)Abnormalities of the chromosome 17 such as 17q (del or t), 17p (del or t), -17 are detectable but rare. [124]. e)The frequency refers to 11q- in Mauritzson et al. [123]. Abbreviations: MDS, myelodysplastic syndrome; del, deletion; t, translocation; I, isochromosome; inv, inversion; idic, isodicentric; NA, not applicable.
Somatic mutations in multipotent stem cells are believed to contribute to MDS pathogenesis, even though no specific defect has been clearly identified. Genomic instability (genetic defects, mutations) increases the propensity to develop AML. It is believed that ~78% of MDS patients carry at least one somatic mutation [6]. The importance of recurrent mutations resides in their potential clinical applications specifically in prognosis, diagnosis, risk stratification, and treatment response. For example, TP53, EZH2, ETV6, RUNX1, and ASXL1 mutations are associated with poor overall survival (OS) [7, 8]. TP53 mutations predict for progression in low-risk MDS [9] and TET2, DNMT3A and SF3B1 mutations predict for response to HMT [10]. SF3B1 mutations have recently been studied as diagnostic biomarkers in the differentiation between clonal and non-clonal causes of MDS [11].
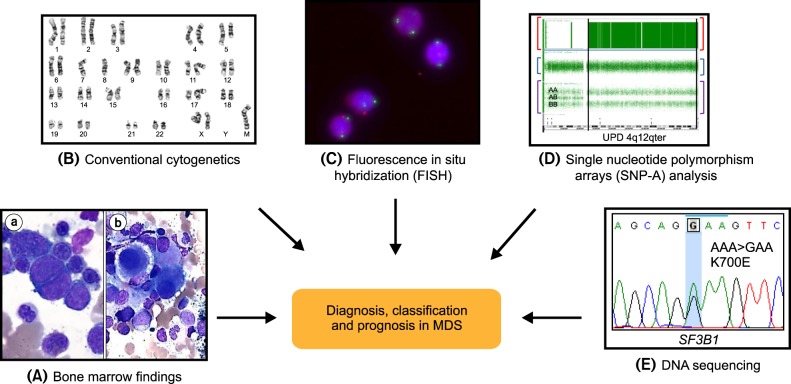
Sanger sequencing, high resolution whole genome scanning technologies [single nucleotide polymorphism arrays (SNP-A) genotyping], and high-throughput next generation sequencing [HT-NGS, whole exome/genome sequencing (WE/WGS), deep sequencing] have brought to light the presence of mutations in genes of methylation, transcription, signaling, histone modification, RNA-splicing and other pathways. Ultimately, understanding the molecular alterations of genes relevant to MDS will hold the key of targeted therapy and improvement in therapeutic outcomes. Fig. 1 shows a schema of the histopathologic, cytogenetic, and molecular genetic tools for diagnosis, classification, and prognosis assessment in MDS.
Fig. 1.
Diagram of the histopathologic, cytogenetic, and molecular genetic tools for comprehensive evaluation of diagnosis, classification and prognosis in myelodysplastic syndrome. (A) Dyserythropoiesis (a) and dysmegakaryopoiesis and dysgranulopoiesis (b) in bone marrow aspirate smears (Wright Giemsa stain ×1,000). (B) Conventional cytogenetics showing a 45,XX,del(5)(q22q35),-7,der(17)t(7;17)(p12;p11.2),-8,der(11) t(8;11)(q11.2;p11.2),+mar karyotype. (C) Fluorescence in situ hybridization detecting the deletion of the long arm of chromosome 20 with one orange signal using LSI D20S108 probe (target locus on 20q12) and two green signals using CEP 8 probe (target locus on 8p11.1-q11.1) (Abbott Molecular, Abbott Park, IL, USA). (D) Representative single nucleotide polymorphism arrays (SNP-A) analysis of loss of heterozygosity (LOH), uniparental disomy (UPD) and gain lesions. The first and top track shows LOH (red brackets), the second track shows copy number for each SNP (blue brackets) and the third track shows the genotype calls (purple brackets). Allele calls are: AA, AB, BB are indicated. Vertical lines indicate each region of the genome. (E) Chromatogram of Sanger sequencing showing the forward sequencing of SF3B1 exon 15 illustrating the most frequent missense mutation (AAA>GAA;K700E; c.2098 G>A).
2. Evolution of technologies in the detection of chromosomal defects and cryptic lesions in the diagnosis of MDS
Chromosomal abnormalities (-5/5q-, -7/7q-, +8, 20q-, +21, 12p-, 13q-, and 17p-) are detected in 40-60% of primary MDS and considered an important determinant in the prognostic scoring systems [12, 13]. However, conventional metaphase cytogenetics (MC) reaches 10% sensitivity and is informative in 46-59% of MDS patients due to limited results in non-viable cells or non-informative karyotypes [14]. Some subtle chromosomal abnormalities can be undetectable or masked [15]. Fluorescence in situ hybridization (FISH) for chromosomes 5, 7, 8, 11, 13, and 20 has complemented MC in cases of undetectable defects and no growth cases. Studies performed to compare FISH to MC have not clarified whether FISH can outperform MC [16, 17]. Recently, FISH has been combined with spectral karyotyping to improve the detection of minimal chromosomal rearrangements and monosomies [18].
The low sensitivity of MC has been overcoming using a powerful method called SNP-A karyotyping. SNP-A, which uses DNA hybridization and fluorescence technique, is currently used in clinical centers as a diagnostic tool to improve the detection rate. SNP-A can detect cryptic lesions [copy neutral-loss of heterozygosity (CN-LOH) or acquired somatic uniparental disomy] in 50% of MDS patients with normal karyotype [19, 20, 21]. Part of these lesions can be pathogenic. Studies have demonstrated the value of combining MC with SNP-A and the prognostic importance of the number of SNP lesions in MDS [20, 22, 23].
In the latest 10 years, second-generation DNA sequencing such as HT-NGS has been implemented in the discovery of genetic alterations in cancer. These technologies refer to non-Sanger DNA sequencing methods where millions of DNA strands can be massively sequenced [24]. More recently WE/WGS and deep sequencing have been helpful in discovering germ-line and somatic variants in MDS. These technologies are almost being considered as diagnostic tests compared to direct-sequencing. At the transcript level, RNA-sequencing has been used for a variety of studies (gene expression, transcript isoforms, small RNAs, TCRβ/BCR repertoires, exon usage/splicing patterns, and methylation/chromatin changes). These technologies rely on a high resolution, depth of coverage (number of times a nucleotide is sequenced) and variation/phred score (index of the quality of the variant calls) [25].
MOLECULAR GENETIC ASPECTS IN THE PATHOGENESIS OF MDS
Genetic technologies including HT-NGS have discovered several mutated genes clustered in specific pathways. We will discuss the frequency, function, and prognostic significance of the main pathways and genetic alterations in MDS (Table 2).
Table 2.
Frequency and prognostic significance of somatic molecular mutations in myelodysplastic syndrome.
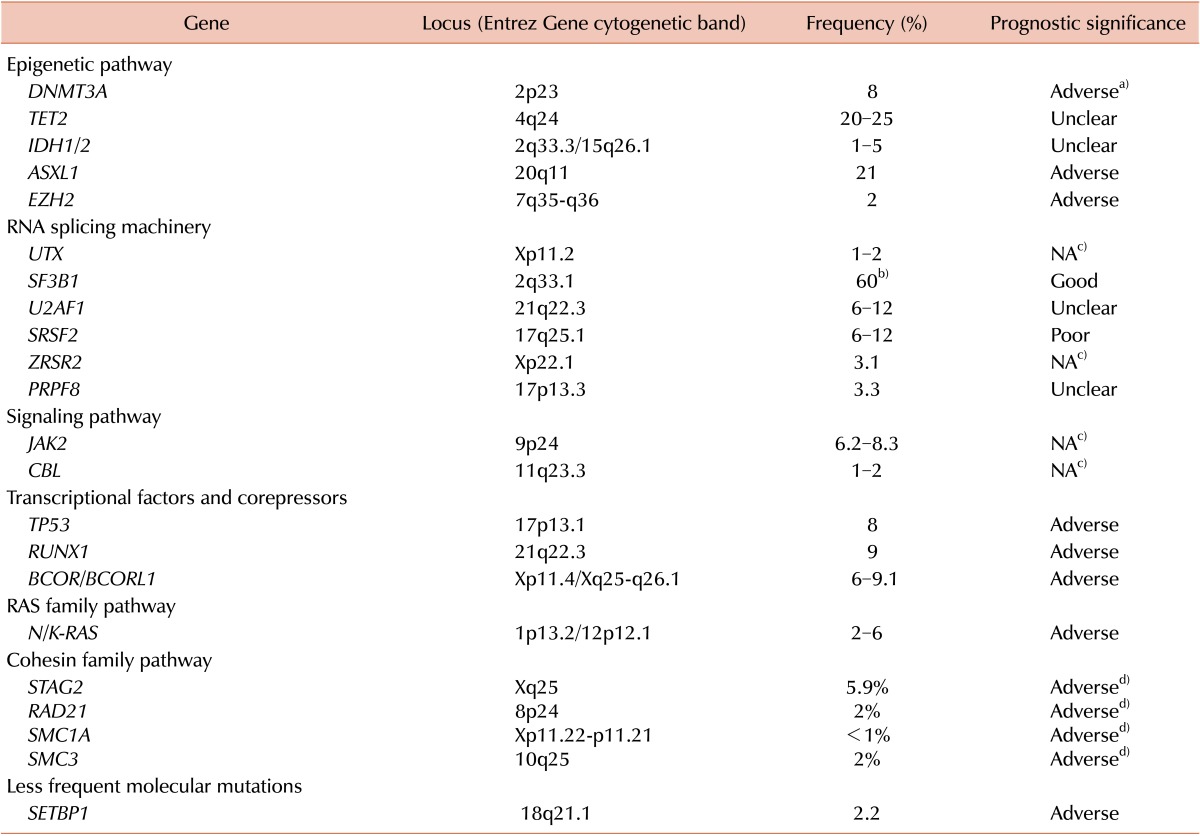
a)An adverse prognostic impact [30]. b)Indicates the frequency in refractory anemia with ring sideroblasts. c)The prognostic impact of mutations in these genes cannot be statistically assessed due to the low frequency of mutations. d)A poor overall survival was associated mainly with STAG2 mutations in MDS patients [102].
1. Epigenetic pathway: DNMT3A, TET2, IDH1/2, ASXL1, EZH2, UTX
Epigenetic regulation is one of the main mechanisms of controlling gene function. DNA methylation and histone modification are the 2 epigenetic processes that have been found to be altered in MDS. Aberrant methylation of TSG promoters is present in MDS [26]. Indeed DNA methylation (addition of a methyl-group to DNA) occurs at CpG sites (regions in which a cytosine and a guanine are linked by a phosphate). Since the CpG dinucleotides are localized in upstream regulatory regions, the methylation of the CpG leads to a silencing mechanism. DNA methyltransferases (DNMTs) such as DNMTs 1, 3a, and 3b are enzymes responsible for DNA methylation and highly expressed in AML and other myeloid neoplasms.
A somatic frameshift mutation in DNMT3A was first identified in an AML patient by WES. DNMT3A mutations were found to be recurrent in 4.1-22.1% of AML patients [27]. The most frequent mutation at position R882 was associated with dismal prognosis and reduced DNMT3A activity [28, 29]. The NH2-terminus of DNMT3A contains motifs important for the recruitment of transcriptional repressors. DNMT3A is a DNA-regulator acting as a check-point of DNA replication by keeping de novo methylation regions partially methylated. DNMT3A has been found mutated in 8% of MDS patients [30, 31] and 23.4% (23/98) of t-MDS and secondary AML (sAML) patients [32]. Moreover, heterozygous mutations occur in 3.3% of high-risk MDS. DNMT3A mutations are highly expressed in the mutated specimens regardless of blast counts, downregulate HSC differentiation, and are associated with worse prognosis and rapid progression to AML [33, 34]. The importance of DNMT3A mutations resides in the fact that HMT is considered one of the primary treatments in MDS and acts by altering the aberrant methylation through inhibition of DNMTs. We first reported that the presence of DNMT3A and TET2 mutations confer a better response to DNMT-inhibitors [10]. Itzykson et al. [35] showed that high-risk MDS patients carrying TET2 mutations have better response to 5-azacytidine.
TET2 mutation was found in 20-25% of MDS patients [36, 37] and usually associated with advanced age and normal karyotype. There was no difference in terms of frequency among IPSS categories (24.5% in low/intermediate-1 and 20% in intermediate-2/high-risk MDS). Mutations are present at diagnosis and appear to be stable during disease progression. TET2 is a dioxygenase catalyzing the conversion of the 5-methylcytosine (5-mc) to 5-hydroxymethylcytosine (5-hmc) by oxidation. Indeed, methylation at the C5 position of cytosine appears to be an epigenetic modification which plays an important role in transcriptional regulation. TET2 mutations are loss-of-function and correlate with decreased 5-hmc and increased 5-mc levels leading to DNA-hypermethylation and gene silencing [38, 39]. A fraction of wild type (WT) patients also have low 5-hmc. A report correlated the low 5-hmc to the over-expression of the CXXC domain of TET2 encoding IDAX gene [38]. Further, reports have described that low 5-hmc levels are associated with DNA-hypomethylation in myeloid malignancies and DNA-hypermethylation in AML [40]. TET2 deletions lead to increased HSC proliferation and myeloid differentiation. In mice, TET2 haploinsufficiency leads to increased myeloid proliferation [41]. Recent studies showed that TET2 might be under the control of >30 microRNAs (miRNA), which inhibit TET2 activity and decrease 5-hmc. In-vivo expression of miRNAs targeting TET2 perturbs the hematopoiesis leading to myeloid cells expansion. Conversely co-expression of TET2 and miRNA restores the normal phenotypes [42]. Although the acquisition of TET2 mutations appears to be an important event in the pathogenesis and the transformation of MDS, the prognostic significance remains unclear. Some studies showed favorable prognosis, and other studies revealed no prognostic impact in MDS [43, 44].
Mutations in the isocitrate dehydrogenase 1 (IDH1) gene were discovered in ~70% of patients with gliomas through genome-wide association studies. WGS identified a somatic mutation (R132C) in an AML case. Mutations are heterozygous (R132 in IDH1 and R140 or R172 in IDH2). These 2 NADP-dependent IDH were discovered to be mutated at low frequency (~5%) in MDS. A study showed IDH1/2 mutations in 12% of MDS patients (N=277) and higher frequency in IDH2 (9%) than in IDH1 (2.9%). A higher frequency was found in high-risk MDS (23%; 8/35 RAEB-2) and 10-20% of sAML patients [45]. Mutations were associated with normal or intermediate-risk karyotype [46]. IDH1 mutations alter the catalytic activity of the enzyme producing the oncometabolite (R)-2-hydroxyglutarate (R2HG), which affects the redox state of the cells and blocks NADPH production. R2HG accumulates in AML cells. Studies have postulated that mutations (loss-of-normal allele, dominant-negative effect) might alter the mitochondrial function. Further, IDH1/2 mutations lead to DNA-hypermethylation [47]. It has been reported that serum R2HG levels can predict clinical outcomes in IDH1/2 mutant patients [48]. IDH1/2 mutant and TET2 loss-of-function cells have similar abnormal hematopoietic differentiation and methylation profiles although mutations in these genes are mutually exclusive. The presence of mutations in genes of the methylation pathway has been associated with better response to HMT [10]. This finding may help in designing novel therapeutic agents targeting specific gene mutations. Recently, primary AML cells carrying IDH1/2 mutations have been found to be sensitive to DOT1L inhibitors. DOT1L is a histone methyltransferase responsible for trimethylation of the histone 3 on lysine 79 (H3K79) [49].
ASXL1 is a member of the polycomb-group (PcG) proteins and implicated in chromatin remodeling and homeotic gene repression. ASXL1 protein is an enhancer of the trithorax- and PcG-proteins in Drosophila driving the bidirectional homeotic determination of the segments during the formation of the embryos. Truncation mutations disrupting activating domains (PDH, RARα, and SRC1) were first reported in MDS in 2009 [50]. ASXL1 monoallelic mutations have been found in 16% of high-risk MDS and ~30% of sAML with a prior MDS. ASXL1 mutations have been associated with worse OS [7]. The importance of ASXL1 resides in its genomic location (20q11.21). Indeed deletion of the long arm of chromosome 20 [del(20q)] are common in MDS. In our experience, ASXL1 mutations were found in 10% of del(20q) patients [51]. A recent meta-analysis performed on 3,311 adult AML patients has confirmed that ASXL1 mutations cluster in a specific subtype of AML with poor prognosis [52]. In another study, 16.3% (25/153) of del(20q) patients were mutated with a higher frequency in advanced MDS [53]. Mutational screening revealed the co-occurrence of ASXL1 with TET2, IDH1/2, and EZH2 mutations [54]. ASXL1 protein interacts with other PcG-proteins (SUZ12, EZH2), which have a role in histone-modification. In mice, ASXL1 depletion does not lead to impairment in the stem cells but leads to defects in the lymphoid or myeloid progenitors. Furthermore, mice do not develop MDS or leukemia most probably due to the compensation of other ASXL-members [55, 56].
Deletions of chromosome 7/7q are common in MDS and correlate with poor prognosis. EZH2 gene encodes the histone methyltransferase factor constituting the catalytic unit of the polycomb repressive complex 2 (PRC2) and promotes the repression of TSGs by depositing the histone mark H3K27me3. Point/inactivating mutations were found in 2-6% of MDS patients [57]. EZH2 forms the PRC2 with EED, SUZ12, and RBBP4 proteins. Mutations in other PRC2 genes are uncommon in MDS (<1%). In other myeloid neoplasms, SUZ12 deletions are concomitant with EZH2. Analysis of 288 low-risk MDS patients showed that EZH2 mutations were enriched in patients with worse prognosis, were associated with a hemoglobin <10 g/dL (P ≤0.008), and significantly predicted for OS after adjusting for low-risk IPSS [Hazard ratio (HR) ≥2.84] [8].
The Jumonji C (JmjC)-domain family of histone demethylases with the function of removing methyl-groups from the histone methylation site has been studied in MDS. Deletions in H3K27me2/3 (UTX/JMJD3), a demethylase on the X chromosome and in other JmjC members have been found at <1% in MDS with highest frequencies in chronic myelomonocytic leukemia (CMML) (8%) [58].
2. RNA-splicing machinery: SF3B1, U2AF1, SRSF2, ZRSR2, PRPF8
Somatic mutations in components of the RNA-splicing machinery were discovered using WE/WGS in myeloid and lymphoid disorders [59]. Splicing factor genes are mutated in almost half of the MDS patients and are generally mutually exclusive and disease-type specific. Sometimes, splicing-gene mutations can also occur with other genetic mutations primarily involved in epigenetics as in the case of SF3B1 with TET2 and DNMT3A, U2AF1 with ASXL1 and DNMT3A, and SRSF2 with TET2 and IDH1. Mutations are localized in hotspot regions [U2AF1 (S34, Q157), SRSF2 (P95) and SF3B1 (mainly K700E)]. Absence of homozygous mutations suggests a gain-of-function while occurrence of frameshift and nonsense in ZRSR2 gene suggests a loss-of-function. SF3B1 mutations are frequent in low-risk MDS and associated with RS, whereas U2AF1 and SRSF2 mutations are associated with high-risk MDS. Prognosis is favorable in SF3B1 mutants in MDS, while mutations have negative impact in lymphoid disorders [60, 61]. SF3B1 mutations occur in 68-75% of RARS and 81% of RARS-T patients [62, 63], while are rare in other diseases [64]. RARS/-T patients carrying SF3B1 mutations had a favorable clinical outcome [63]. Another study has shown no significant OS and AML transformation in 317 MDS patients [65]. SF3B1 mutants have been shown to respond better to HMT [10], and preliminary data suggest that SF3B1 mutations confer better response to erythropoiesis-stimulating agents [63].
SF3B1 mutations were associated with RS formation and recently with the higher expression level of a variant of Mitoferrin-1, a mitochondrial iron importer [66] while other studies suggested an association between SF3B1 and ABCB7, a mitochondrial gene linked to RARS pathogenesis. Nikpour et al. [67] used knock-down experiments of SF3B1 in K562 cells and induced a downregulation of ABCB7 suggesting a link between SF3B1 mutations and the down-regulation of ABCB7. In the first study investigating the relation between SF3B1 mutations and the RS phenotype in MDS, RS were increased in the BM of Sf3b1 +/- mice. We first reported a long term follow-up study of Sf3b1 +/- mice demonstrating macrocytic anemia, extramedullary hematopoiesis, and thrombocytosis. This feature was most probably correlated with the overexpression of JAK2 that has been correlated with thrombocytosis in humans [68, 69]. Subsequent other studies, focusing primarily on BM reconstitution property of the HSCs and not on the hematologic or BM phenotype, showed a compromised HSC function [70, 71].
ZRSR2 mutations were found at lower frequency in MDS with no association with RS [72] and not frequent in other BM failure syndromes [64]. Thol et al. [72] published that 6/193 (3.1%) MDS patients harbored mutations in coding-exons, while 2 patients exhibit mutations in the introns 7 and 8. Survival analysis was not performed due to the limited number of mutant patients, although 3 patients expired at 56 days, 1.4 and 3.5 years from the time of screening.
Spliceosome inhibitors have been proposed to target the mutant allele in splicing factors in MDS. Pladienolide B, Sudemycins, and Spliceostatin A derived from bacterial fermentation products and small molecules (steroids, biflavonoid natural plant, indole derivatives, protein phosphatases and benzothiazole inhibitors) showed antitumoral effect against the spliceosome [73]. In vitro data on Meayamycin, an analog of FR901464 binding to the splicing factor 3b complex and inhibiting pre-mRNA-splicing was reported in 2012 [63].
U2AF1 mutations (S34, Q157) were found in 8.7% of primary MDS patients and were associated with AML progression [74, 75]. U2AF1 mutations result in a gain-of-function and an increased exon skipping was observed when the mutant S34F cDNA was expressed in vitro [74]. U2AF1 mutations have been shown to cause missplicing and differential exon-usage in mitotic genes (CEP164, EHMT1, WAC, ATR), RNA-processing (PTBP1, STRAP, PPWD1, PABPC4, UPF3B), and G2/M checkpoint genes (CEP164) [76]. It has been also reported that mutant U2AF1 murine cells have increased sensitivity to Sudemycin [77].
SRSF2 mutations were found in 12.4% of MDS patients with higher ranges in CMML (28.4-47%) [72]. The most common mutations are missense at P95 position. Rare deletions [P95_R102del (c.284_307del), P95_D97del (c.283_291del)] have been also described [78]. Given that studies in Srsf2 -/- mice demonstrated increased apoptosis and no hematopoietic cells, SRSF2 is essential for hematopoiesis during embryonic development and induces alternative splicing of hematopoietic genes. Since MDS patients are usually heterozygous, studies using Srsf2 +/- mice revealed alternative splicing of hematopoietic genes but no obvious hematopoietic defect [79]. SRSF2 mutations have been correlated with older age, anemia, and normal karyotype. Some studies have shown no impact on OS while others poor outcomes. SRSF2 mutant had outcomes similar to WT patients in a cohort that underwent allogeneic HSC transplantation suggesting that transplant is able to compensate for the negative impact [80].
PRPF8 is a component of the catalytic core of the spliceosome and forms interactions with the 3' and 5' splice, the branch point, and the excised introns. Two mutant cases were reported by Makishima et al. and Gomez-Segui et al. [75, 81, 82]. In a larger cohort (N=447) the authors found mutations in 15/447 (3.3%) patients [83]. Mutations were found along the gene, and D1598 was the most common amino acid change. A higher frequency was found in primary and sAML. In total, 60% of the patients appeared to have RS. Due to the genomic mapping of PRPF8 (17p13.3) and TP53 (17p13.1), the authors described that some cases with del(17p) also involved the TP53 locus. Gene expression of TCGA database found that PRPF8 may regulate mitochondrial respiratory chain genes (NDUFAF6, SFXN2, SLC25A19). Knock-down of PRPF8 in K562 cell line, whole BM and CD34+ cells of healthy subjects leads to increased cell proliferation. Cells with PRPF8 mutant were more sensitive than normal BM cells to Meayamycin [83]. In a model of zebrafish carrying a premature stop codon, an impaired myeloid differentiation and a decreased expression of myeloid compared to erythroid markers were observed. Further, PRPF8 seems to be able to auto-regulate his own pre-mRNA-splicing. Indeed PRPF8 splicing in this zebrafish model is defective [84].
3. Signaling pathway: JAK2, CBL
JAK2 is a member of the Janus kinase family (JAK1, JAK3, TYK2) proteins, which are intracellular non-receptor tyrosine kinases with a function in cell proliferation and survival of HSC. JAK2 mutations are hallmark of myeloproliferative neoplasms (MPN). The most common mutation at position 617 (V617F) induces autophosphorylation, gene transcription, and in vitro kinase activity. In JAK2 mutant MPN patients, JAK2 phosphorylates the arginine methyltransferase PRMT5 reducing the methylation to histone substrates and promoting the MPN-like phenotype. CD34+ cells of JAK2 mutant MPN patients with decreased PRMT5 expression showed an increased erythroid differentiation and colonies in vitro [85]. A gain-of-function mutation in exon 12 is detected in 3-5% of JAK2 WT patients. Compared to V617F mutation, mutations in exon 12 produce increased ligand-independent signaling and phosphorylation through JAK2. JAK2 mutations have been reported at frequency of 6.2% in 97 MDS patients carrying isolated del(5q) [86] and in 8.3% (1/12) where the unique mutant patient carried a del(20q) abnormality [87]. In the first study, mutant tended to have elevated platelet count compared to WT patients (475 vs. 250 × 109/L; P=0.15). A higher prevalence of JAK2V617F was found in patients with RARS-T. Szpurka et al. [88] showed that in a group of 9 RARS-T patients, 6 patients carried JAK2V617F mutation and 1 WT patient had increased phospho-STAT5 staining. The features of RARS-T resemble more MDS patients in terms of degree of anemia and survival outcomes. It is believed that RARS patients may acquire JAK2 mutations during the disease course [89]. On the contrary, a study found JAK2 mutation only at the time of development of myelofibrosis (MF) in 2/6 MDS patients, but not in MDS patients without MF (N=38) [90].
CBL gene encodes for a cytosolic protein, which downregulates the tyrosine kinase signaling trigged by E3 ubiquitin ligase leading to lysosomal/proteosomal degradation and modulates JAK2 and MPL downstream signals. CBL mutations seem to trigger an oncogenic phenotype and cell proliferation by activating the RAS-pathway. In mice CBL haploinsufficiency leads to MPN-like features (splenomegaly, cell proliferation, sensitivity to growth factors). Mutations in c-CBL, CBL-b, and CBL-c are rare in MDS (1%) while are more frequent (8.1%) in MDS/MPN, specifically in CMML (15-20%) [91]. The mutations are missense or in-frame deletions and coexist with JAK2, TP53, FLT3, and RUNX1 mutations.
4. Transcriptional factors and corepressors: RUNX1, TP53, BCOR/BCORL1
RUNX1 [AML1 or core-binding factor-α (CBFA)] is a DNA core-binding factor regulating the transcription of genes important in HSC formation. Indeed, RUNX1-/- mice die in utero without achieving complete hematopoiesis. RUNX1 mutations have been associated with translocations [t(8;21), t(3;21), t(12;21)]. It has been reported that RUNX1 mutations are present in 12% (16/132) of MDS patients at diagnosis, and they remain unchanged during the disease course. In this study, 2/45 serially available samples acquired RUNX1 mutations (one at the time of progression to AML and another at relapse and AML transformation after HSC transplantation) [92]. RUNX1 mutations are associated with high-risk MDS. Steensma et al. [93, 94] reported a frequency of 9.6% (5/52) in MDS and higher frequency in RAEB-2 (4/7; 57%).
TP53 is a TSG that regulates the cell cycle progression and the apoptosis. The coexistence of MDS features like cytopenias and hypercellular BM has been correlated with the increased apoptosis in the HSCs. Mutations in TP53 were detected early at MDS presentation, suggesting a primary event in the disease manifestation and were associated with certain cytogenetic changes including isolated del(5q), -5/5q-, 17p- and complex karyotypes. A study of 318 MDS patients found a mutational frequency of 9.4% (30/318) with 8.1% in primary MDS patients. TP53 mutations were correlated with complex karyotype and -5/5q- (72%), IPSS intermediate-2/high, and higher blast count. TP53 mutant had higher leukemic transformation, shorter median OS and progression free survival (PFS) compared to WT patients [8, 96]. TP53 was also the most commonly mutated gene in t-MDS (21%; 8/38), where TP53 mutant carried dismal survival compared to WT patients (8.8 vs. 37.4 months; P =0.0035) [95]. Some TP53 mutant patients were also mutated for other genes like U2AF1, RUNX1, ASXL1, TET2, DNMT3A, and IDH1. TP53 mutant clones reduced in patients responding to 5-azacytidine [96]. A study showed that targeting suppression of p53 protein may be beneficial to del(5q) MDS patients, who are resistant to lenalidomide [97].
BCOR and BCORL1 are 2 transcriptional co-repressors located on chromosome X. BCOR protein has a BCL6 binding domain and acts as corepressor of BCL6. BCORL1 is a transcriptional corepressor binding to class II histone deacetylases to interact with the CTBP1 corepressor inducing E-cadherin repression. They were first discovered in AML by WES. Mutational analysis showed that BCOR/BCORL1 mutations are found in 4.2% and 0.8% in MDS with higher frequency (6-9.1%) in AML or t-MDS patients [98]. BCOR mutations are associated with shorter survival (HR, 3.3; 95% CI, 1.4-8.1; P =0.008) [99].
5. RAS family pathway
Activating oncogenic mutations are rare in MDS. N/K-RAS were reported at 2-6% and associated with disease progression and shorter OS. RAP1, a member of the Ras family of small G proteins, were found mutated at low frequencies in MDS. One patient with high-risk MDS [RAEB with del(7q)] harbored 2 RAP1B mutations (G12R, K42E) [100]. GNAS (R201) was reported at 0.7% (3/439) in MDS [7]. Genetic abnormalities (mutations and amplification) in Ras-like-without-CAAX-1 (RIT1; 1q22) gene have been detected in high-risk MDS (8.4%) and in sAML (3.9%) [82].
6. Cohesin family
Genome-wide mapping clarified the cohesin complex structure and identified its role in chromosome condensation in Saccharomyces cerevisiae [101]. The structure of this complex resembles a ring constituted by 4 subunits (Scc1, Scc3, Smc1, Smc3) with the Smc1 and Smc3 being elements of the structural maintenance of chromosome family. Cohesins control that sister chromatids are connected during metaphase and segregate into right directions during cell division. Cohesins are important also in DNA-replication, DNA double-strand breaks repair, and chromosome condensation. Mutations in the cohesin complex (STAG2, RAD21, SMC1A, SMC3) have been found in 8.0% (18/224) of MDS, 12.1% (19/157) of AML, 10.2% (9/88) of CMML, and 6.3% (4/64) of chronic myeloid leukemia (CML). The role of cohesin in mitosis has been established, but its role in leukemogenesis is unclear. In 386 MDS cases, cohesin mutations were mainly enriched in trisomy 8 patients rather than in normal or complex karyotype. Mutations co-occur with RUNX1, Ras-family, BCOR, and ASXL1. STAG2/RAD21 mutant responded better to HMT compared to WT patients (79% vs. 47%; P =0.04). Cohesin mutant patients had shorter OS compared to WT patients. (27.2 vs. 39.9 months; P =0.023) [102].
7. Less frequent molecular mutations
Genetic alterations in SETBP1, a gene associated with Schinzel-Giedion syndrome, were first found in 24% (17/70) of atypical CML patients [103] and then discovered in MDS. Somatic hererozygous mutations (Asp868, Ser869, Gly870, Ile871, Asp880) were detected in 17% of sAML and 15% of CMML [104]. SETBP1 mutations are rare (2.2%) in MDS [105]. A study of 944 AML patients found 10 mutant patients (6 MDS; 4 sAML from MDS) [106]. SETBP1 mutations are frequent in patients with myeloid neoplasms carrying i(17)(q10) and are associated with SRSF2 mutations. SETBP1 mutations tended to be associated with worse prognosis. Mutants were older and had higher monocyte counts compared to WT patients. Morphologycally, the cohort had prominent dysgranulopoiesis with hypo-/non-segmented nuclei [107]. A subsequent study conducted in 1,130 cases also found an association of SETBP1 with i(17)(q10) and -7 abnormalities correlating SETBP1 mutations with 2 other negative prognostic mutations (ASXL1, CBL) [108]. Mutations in U2AF65, SF1, SRSF1, SF3A1, PRF40B, and LUC7L2 are infrequent [75].
NON-MOLECULAR ASPECTS OF MDS
Although molecular mutations are frequent in MDS, the consequences of these mutations have not been clarified. Other non-genetic mechanisms including BM-microenvironment factors, apoptosis, cytokines, immunoregulation, T-cell repertoire and telomere length (TL) have been largely studied. In supporting to the involvement of apoptotic pathways, death receptors (Fas, TRAIL), mitochondrial pathways and caspase activation have been found modulated in MDS cells. Indeed, MDS precursors overexpress Fas and TRAIL receptors, which seem to induce death signaling. Tumor necrosis factor alpha (TNF-α) also seems to be released by cytotoxic T-cells inducing apoptosis. Cytochrome c release is observed in low-risk MDS patients while caspase-9 activity is increased. Recently, it was reported that SF3B1 mutant RARS/-T patients overexpress a specific variant of Mitoferrin-1, a mitochondrial iron importer [66]. The pro-apoptotic BCL2 protein has been found up-regulated in high-risk MDS and may explain the increased cellular proliferation [109]. Drugs (EPO, G-CSF) that target the apoptosis pathway improve the anemia in low-risk MDS.
Abnormalities in suppressive cytokines [TNF-α, tumor growth factor-β (TGF-β), interferon-γ (IFN-γ), interleukins-3, 6, and 8, thrombopoietin (TPO)] have been described in MDS. Overactivation of TGF-β depends on a family of proteins called Sma- and Mad-related (SMAD). SMAD2, a downstream regulator of TGF-β receptor I kinase activation, is constitutively activated in MDS CD34+ cells, while SMAD7, a negative regulator, seems to be decreased in MDS cells [110]. Multiplex-analysis of cytokines/chemokines showed similarity between MDS and AML cells with a higher expression of the VEGF in MDS. High levels of TNF-α have been correlated with worse OS in MDS [111]. Higher levels of TPO and G-CSF, and lower levels of CD40L, CCL5, CCL11, VEGF, CXCL5, EGF, and CXCL11 were found by comparing plasma cytokines between aplastic anemia and MDS patients. Differences between low- and high-risk MDS were described with decreased CXCL5, CCL5, CD40L, EGF, and VEGF, and increased CCL4 in high-risk MDS [112]. HSCs in high-risk MDS patients are believed to proliferate bypassing the immune system. Differences in immune-complexes were found between low- and high-risk MDS and attributable to clonal progression. Cytotoxicity of BM cells in low-risk MDS has been associated with high numbers of NK cells, Th17, and macrophages releasing IFN-γ. CD4+FOXP3+-regulatory T cells have been correlated with immune response suppression and found elevated in high-risk MDS patients. The BM failure of MDS patients has been related to autoimmunity. In trisomy 8 MDS, spectratyping of T-cell receptor β-chain variable (Vβ) families revealed that CD8+ T-lymphocytes are oligoclonal and selectively cytotoxic against trisomy 8 clones. Trisomy 8 clones seem to be resistant to the T-cell immune attack by up-regulating survivin. Microarray showed increased expression of WT1 in trisomy 8 CD34+ cells [113].
Cellular senescence in MDS has been related to telomere shortening. BM MDS cells appear to have erosive telomeric repeats without changes in telomerase activity. Southern blot showed a variability in TL in MDS with a lower TL correlating with leukemic progression and complex cytogenetics [114]. Using multiplex-quantitative RT-PCR in 307 MDS patients, TL in BM cells was lower in MDS compared to healthy subjects with no correlation with age or gender. TL seems to be negatively correlated with IPSS, transfusion dependence, BM blasts and complex karyotype [115, 116]. Telomerase mutations/polymorphisms are sporadic in MDS. One patient with MDS and del(5q) harbored a TERC mutation [nucleotide 322 (G/A)] within the conserved region (CR) 4-CR5 domain, while 2 MDS patients carried polymorphisms [nucleotide 58 (G/A)] [117]. Mutations were found in the TERC and TERT genes in familial MDS/AML. The mutations affected the telomerase activity in vitro, and mutant patients had short telomeres [118]. Recently, a germline mutation (A377G) in the H box of the TERC gene was found in a young MDS patient with short telomeres [119].
Aberrant methylation is another important mechanism in MDS. Hypermethylation of promoter-CpG island of TSGs is a silencing mechanism and contributes to clonal evolution in MDS. Level of methylation also correlated with survival outcomes. One study showed that MDS patients with higher levels of aberrant CpG methylation in relatively common genes had a shorter median OS and PFS (OS: 12.3 vs. 17.5 months; P =0.04; PFS: 6.4 vs.14.9 months; P =0.009) compared to MDS patients with lower level of methylation [120].
CONCLUSION
MDS is a heterogeneous clonal disease with multifactorial causes. Molecular mutations in several pathways have been identified. Almost 78% of MDS patients carry at least one mutation in one gene. The presence of mutations has been associated with disease phenotypes and response to therapies. The use of NGS technologies has almost being implemented in clinical practice, although large clinical studies are needed to validate the possibility to use mutations as predictors of diagnosis, prognosis, and treatment response. Functional studies aim to decipher how genetic alterations may lead to the clinical phenotypes and whether targeting specific pathways or genes will be beneficial for MDS patients.
Footnotes
No potential conflicts of interest relevant to this article were reported.
References
- 1.Ma X, Does M, Raza A, Mayne ST. Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007;109:1536–1542. doi: 10.1002/cncr.22570. [DOI] [PubMed] [Google Scholar]
- 2.Sekeres MA. Epidemiology, natural history, and practice patterns of patients with myelodysplastic syndromes in 2010. J Natl Compr Canc Netw. 2011;9:57–63. doi: 10.6004/jnccn.2011.0006. [DOI] [PubMed] [Google Scholar]
- 3.Sole F, Espinet B, Sanz GF, et al. Incidence, characterization and prognostic significance of chromosomal abnormalities in 640 patients with primary myelodysplastic syndromes. Grupo Cooperativo Español de Citogenética Hematológica. Br J Haematol. 2000;108:346–356. doi: 10.1046/j.1365-2141.2000.01868.x. [DOI] [PubMed] [Google Scholar]
- 4.Le Beau MM, Albain KS, Larson RA, et al. Clinical and cytogenetic correlations in 63 patients with therapy-related myelodysplastic syndromes and acute nonlymphocytic leukemia: further evidence for characteristic abnormalities of chromosomes no. 5 and 7. J Clin Oncol. 1986;4:325–345. doi: 10.1200/JCO.1986.4.3.325. [DOI] [PubMed] [Google Scholar]
- 5.Greenberg PL, Tuechler H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–2465. doi: 10.1182/blood-2012-03-420489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papaemmanuil E, Gerstung M, Malcovati L, et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 2013;122:3616–3627. doi: 10.1182/blood-2013-08-518886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bejar R, Stevenson K, Abdel-Wahab O, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364:2496–2506. doi: 10.1056/NEJMoa1013343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bejar R, Stevenson KE, Caughey BA, et al. Validation of a prognostic model and the impact of mutations in patients with lower-risk myelodysplastic syndromes. J Clin Oncol. 2012;30:3376–3382. doi: 10.1200/JCO.2011.40.7379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jadersten M, Saft L, Smith A, et al. TP53 mutations in low-risk myelodysplastic syndromes with del(5q) predict disease progression. J Clin Oncol. 2011;29:1971–1979. doi: 10.1200/JCO.2010.31.8576. [DOI] [PubMed] [Google Scholar]
- 10.Traina F, Visconte V, Elson P, et al. Impact of molecular mutations on treatment response to DNMT inhibitors in myelodysplasia and related neoplasms. Leukemia. 2014;28:78–87. doi: 10.1038/leu.2013.269. [DOI] [PubMed] [Google Scholar]
- 11.Visconte V, Tabarroki A, Gerace CJ, et al. Screening for SF3B1 mutations is a useful tool to differentiate between acquired clonal and non-clonal sideroblastic anemia. Leuk Lymphoma. 2014:1–3. doi: 10.3109/10428194.2014.976821. [DOI] [PubMed] [Google Scholar]
- 12.Bejar R. Prognostic models in myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2013;2013:504–510. doi: 10.1182/asheducation-2013.1.504. [DOI] [PubMed] [Google Scholar]
- 13.Estephan F, Tiu RV. Current and novel therapeutic approaches in myelodysplastic syndromes. J Community Support Oncol. 2014;12:236–249. doi: 10.12788/jcso.0057. [DOI] [PubMed] [Google Scholar]
- 14.Tiu RV, Visconte V, Traina F, Schwandt A, Maciejewski JP. Updates in cytogenetics and molecular markers in MDS. Curr Hematol Malig Rep. 2011;6:126–135. doi: 10.1007/s11899-011-0081-2. [DOI] [PubMed] [Google Scholar]
- 15.Flactif M, Lai JL, Preudhomme C, Fenaux P. Fluorescence in situ hybridization improves the detection of monosomy 7 in myelodysplastic syndromes. Leukemia. 1994;8:1012–1018. [PubMed] [Google Scholar]
- 16.Bernasconi P, Cavigliano PM, Boni M, et al. Is FISH a relevant prognostic tool in myelodysplastic syndromes with a normal chromosome pattern on conventional cytogenetics? A study on 57 patients. Leukemia. 2003;17:2107–2112. doi: 10.1038/sj.leu.2403108. [DOI] [PubMed] [Google Scholar]
- 17.Broseus J, Alpermann T, Wulfert M, et al. Age, JAK2(V617F) and SF3B1 mutations are the main predicting factors for survival in refractory anaemia with ring sideroblasts and marked thrombocytosis. Leukemia. 2013;27:1826–1831. doi: 10.1038/leu.2013.120. [DOI] [PubMed] [Google Scholar]
- 18.Imataka G, Arisaka O. Chromosome analysis using spectral karyotyping (SKY) Cell Biochem Biophys. 2012;62:13–17. doi: 10.1007/s12013-011-9285-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tiu RV, Gondek LP, OKeefe CL, et al. Prognostic impact of SNP array karyotyping in myelodysplastic syndromes and related myeloid malignancies. Blood. 2011;117:4552–4560. doi: 10.1182/blood-2010-07-295857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gondek LP, Tiu R, O'Keefe CL, Sekeres MA, Theil KS, Maciejewski JP. Chromosomal lesions and uniparental disomy detected by SNP arrays in MDS, MDS/MPD, and MDS-derived AML. Blood. 2008;111:1534–1542. doi: 10.1182/blood-2007-05-092304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jerez A, Gondek LP, Jankowska AM, et al. Topography, clinical, and genomic correlates of 5q myeloid malignancies revisited. J Clin Oncol. 2012;30:1343–1349. doi: 10.1200/JCO.2011.36.1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gondek LP, Tiu R, Haddad AS, et al. Single nucleotide polymorphism arrays complement metaphase cytogenetics in detection of new chromosomal lesions in MDS. Leukemia. 2007;21:2058–2061. doi: 10.1038/sj.leu.2404745. [DOI] [PubMed] [Google Scholar]
- 23.Mohamedali A, Gaken J, Twine NA, et al. Prevalence and prognostic significance of allelic imbalance by single-nucleotide polymorphism analysis in low-risk myelodysplastic syndromes. Blood. 2007;110:3365–3373. doi: 10.1182/blood-2007-03-079673. [DOI] [PubMed] [Google Scholar]
- 24.Grada A, Weinbrecht K. Next-generation sequencing: methodology and application. J Invest Dermatol. 2013;133:e11. doi: 10.1038/jid.2013.248. [DOI] [PubMed] [Google Scholar]
- 25.Metzker ML. Sequencing technologies - the next generation. Nat Rev Genet. 2010;11:31–46. doi: 10.1038/nrg2626. [DOI] [PubMed] [Google Scholar]
- 26.Itzykson R, Fenaux P. Epigenetics of myelodysplastic syndromes. Leukemia. 2014;28:497–506. doi: 10.1038/leu.2013.343. [DOI] [PubMed] [Google Scholar]
- 27.Ley TJ, Ding L, Walter MJ, et al. DNMT3A mutations in acute myeloid leukemia. N Engl J Med. 2010;363:2424–2433. doi: 10.1056/NEJMoa1005143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yamashita Y, Yuan J, Suetake I, et al. Array-based genomic resequencing of human leukemia. Oncogene. 2010;29:3723–3731. doi: 10.1038/onc.2010.117. [DOI] [PubMed] [Google Scholar]
- 29.Shivarov V, Gueorguieva R, Stoimenov A, Tiu R. DNMT3A mutation is a poor prognosis biomarker in AML: results of a meta-analysis of 4500 AML patients. Leuk Res. 2013;37:1445–1450. doi: 10.1016/j.leukres.2013.07.032. [DOI] [PubMed] [Google Scholar]
- 30.Thol F, Winschel C, Ludeking A, et al. Rare occurrence of DNMT3A mutations in myelodysplastic syndromes. Haematologica. 2011;96:1870–1873. doi: 10.3324/haematol.2011.045559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jankowska AM, Makishima H, Tiu RV, et al. Mutational spectrum analysis of chronic myelomonocytic leukemia includes genes associated with epigenetic regulation: UTX, EZH2, and DNMT3A. Blood. 2011;118:3932–3941. doi: 10.1182/blood-2010-10-311019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fried I, Bodner C, Pichler MM, et al. Frequency, onset and clinical impact of somatic DNMT3A mutations in therapy-related and secondary acute myeloid leukemia. Haematologica. 2012;97:246–250. doi: 10.3324/haematol.2011.051581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Challen GA, Sun D, Jeong M, et al. Dnmt3a is essential for hematopoietic stem cell differentiation. Nat Genet. 2011;44:23–31. doi: 10.1038/ng.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walter MJ, Ding L, Shen D, et al. Recurrent DNMT3A mutations in patients with myelodysplastic syndromes. Leukemia. 2011;25:1153–1158. doi: 10.1038/leu.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Itzykson R, Kosmider O, Cluzeau T, et al. Impact of TET2 mutations on response rate to azacitidine in myelodysplastic syndromes and low blast count acute myeloid leukemias. Leukemia. 2011;25:1147–1152. doi: 10.1038/leu.2011.71. [DOI] [PubMed] [Google Scholar]
- 36.Jankowska AM, Szpurka H, Tiu RV, et al. Loss of heterozygosity 4q24 and TET2 mutations associated with myelodysplastic/myeloproliferative neoplasms. Blood. 2009;113:6403–6410. doi: 10.1182/blood-2009-02-205690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Langemeijer SM, Kuiper RP, Berends M, et al. Acquired mutations in TET2 are common in myelodysplastic syndromes. Nat Genet. 2009;41:838–842. doi: 10.1038/ng.391. [DOI] [PubMed] [Google Scholar]
- 38.Ko M, An J, Bandukwala HS, et al. Modulation of TET2 expression and 5-methylcytosine oxidation by the CXXC domain protein IDAX. Nature. 2013;497:122–126. doi: 10.1038/nature12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ponnaluri VK, Maciejewski JP, Mukherji M. A mechanistic overview of TET-mediated 5-methylcytosine oxidation. Biochem Biophys Res Commun. 2013;436:115–120. doi: 10.1016/j.bbrc.2013.05.077. [DOI] [PubMed] [Google Scholar]
- 40.Ko M, Huang Y, Jankowska AM, et al. Impaired hydroxylation of 5-methylcytosine in myeloid cancers with mutant TET2. Nature. 2010;468:839–843. doi: 10.1038/nature09586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moran-Crusio K, Reavie L, Shih A, et al. Tet2 loss leads to increased hematopoietic stem cell self-renewal and myeloid transformation. Cancer Cell. 2011;20:11–24. doi: 10.1016/j.ccr.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng J, Guo S, Chen S, et al. An extensive network of TET2-targeting MicroRNAs regulates malignant hematopoiesis. Cell Rep. 2013;5:471–481. doi: 10.1016/j.celrep.2013.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith AE, Mohamedali AM, Kulasekararaj A, et al. Next-generation sequencing of the TET2 gene in 355 MDS and CMML patients reveals low-abundance mutant clones with early origins, but indicates no definite prognostic value. Blood. 2010;116:3923–3932. doi: 10.1182/blood-2010-03-274704. [DOI] [PubMed] [Google Scholar]
- 44.Kihara R, Nagata Y, Kiyoi H, et al. Comprehensive analysis of genetic alterations and their prognostic impacts in adult acute myeloid leukemia patients. Leukemia. 2014;28:1586–1595. doi: 10.1038/leu.2014.55. [DOI] [PubMed] [Google Scholar]
- 45.Patnaik MM, Hanson CA, Hodnefield JM, et al. Differential prognostic effect of IDH1 versus IDH2 mutations in myelodysplastic syndromes: a Mayo Clinic study of 277 patients. Leukemia. 2012;26:101–105. doi: 10.1038/leu.2011.298. [DOI] [PubMed] [Google Scholar]
- 46.Schnittger S, Haferlach C, Ulke M, Alpermann T, Kern W, Haferlach T. IDH1 mutations are detected in 6.6% of 1414 AML patients and are associated with intermediate risk karyotype and unfavorable prognosis in adults younger than 60 years and unmutated NPM1 status. Blood. 2010;116:5486–5496. doi: 10.1182/blood-2010-02-267955. [DOI] [PubMed] [Google Scholar]
- 47.Figueroa ME, Abdel-Wahab O, Lu C, et al. Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype, disrupt TET2 function, and impair hematopoietic differentiation. Cancer Cell. 2010;18:553–567. doi: 10.1016/j.ccr.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DiNardo CD, Propert KJ, Loren AW, et al. Serum 2-hydroxyglutarate levels predict isocitrate dehydrogenase mutations and clinical outcome in acute myeloid leukemia. Blood. 2013;121:4917–4924. doi: 10.1182/blood-2013-03-493197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sarkaria SM, Christopher MJ, Klco JM, Ley TJ. Primary acute myeloid leukemia cells with IDH1 or IDH2 mutations respond to a DOT1L inhibitor in vitro. Leukemia. 2014;28:2403–2406. doi: 10.1038/leu.2014.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gelsi-Boyer V, Trouplin V, Adelaide J, et al. Mutations of polycomb-associated gene ASXL1 in myelodysplastic syndromes and chronic myelomonocytic leukaemia. Br J Haematol. 2009;145:788–800. doi: 10.1111/j.1365-2141.2009.07697.x. [DOI] [PubMed] [Google Scholar]
- 51.Tabarroki A, Zhang L, Visconte V, et al. Impact of cytogenetics and molecular genetics in the clinical outcomes of patients with deletion (20)q diagnosed with MDS and other myeloid malignancies. 4th International Bone Marrow Failure Disease Scientific Symposium 2014. ( http://www.aamds.org/node/2472)
- 52.Shivarov V, Gueorguieva R, Ivanova M, Tiu RV. ASXL1 mutations define a subgroup of AML patients with distinct gene expression profile and poor prognosis: a meta-analysis of 3311 adult AML patients. Leuk Lymphoma. 2014:1–11. doi: 10.3109/10428194.2014.974596. [DOI] [PubMed] [Google Scholar]
- 53.Bacher U, Haferlach T, Schnittger S, et al. Myelodysplastic syndromes (MDS) with 20q deletion show a high frequency of associated cytogenetic and molecular lesions with an association to U2AF1, SRSF2, and prognostically adverse ASXL1 mutations. Blood. 2013;122(ASH Annual Meeting):abst 657. [Google Scholar]
- 54.Shih AH, Abdel-Wahab O, Patel JP, Levine RL. The role of mutations in epigenetic regulators in myeloid malignancies. Nat Rev Cancer. 2012;12:599–612. doi: 10.1038/nrc3343. [DOI] [PubMed] [Google Scholar]
- 55.Abdel-Wahab O, Gao J, Adli M, et al. Deletion of Asxl1 results in myelodysplasia and severe developmental defects in vivo. J Exp Med. 2013;210:2641–2659. doi: 10.1084/jem.20131141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fisher CL, Pineault N, Brookes C, et al. Loss-of-function additional sex combs like 1 mutations disrupt hematopoiesis but do not cause severe myelodysplasia or leukemia. Blood. 2010;115:38–46. doi: 10.1182/blood-2009-07-230698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Makishima H, Jankowska AM, Tiu RV, et al. Novel homo- and hemizygous mutations in EZH2 in myeloid malignancies. Leukemia. 2010;24:1799–1804. doi: 10.1038/leu.2010.167. [DOI] [PubMed] [Google Scholar]
- 58.Bejanyan N, Tiu RV, Raza A, et al. A phase 2 trial of combination therapy with thalidomide, arsenic trioxide, dexamethasone, and ascorbic acid (TADA) in patients with overlap myelodysplastic/myeloproliferative neoplasms (MDS/MPN) or primary myelofibrosis (PMF) Cancer. 2012;118:3968–3976. doi: 10.1002/cncr.26741. [DOI] [PubMed] [Google Scholar]
- 59.Visconte V, Selleri C, Maciejewski JP, Tiu RV. Molecular pathogenesis of myelodysplastic syndromes. Transl Med UniSa. 2014;8:19–30. [PMC free article] [PubMed] [Google Scholar]
- 60.Malcovati L, Papaemmanuil E, Bowen DT, et al. Clinical significance of SF3B1 mutations in myelodysplastic syndromes and myelodysplastic/myeloproliferative neoplasms. Blood. 2011;118:6239–6246. doi: 10.1182/blood-2011-09-377275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Quesada V, Ramsay AJ, Lopez-Otin C. Chronic lymphocytic leukemia with SF3B1 mutation. N Engl J Med. 2012;366:2530. doi: 10.1056/NEJMc1204033. [DOI] [PubMed] [Google Scholar]
- 62.Papaemmanuil E, Cazzola M, Boultwood J, et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011;365:1384–1395. doi: 10.1056/NEJMoa1103283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jerez A, Sugimoto Y, Makishima H, et al. Loss of heterozygosity in 7q myeloid disorders: clinical associations and genomic pathogenesis. Blood. 2012;119:6109–6117. doi: 10.1182/blood-2011-12-397620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Visconte V, Tabarroki A, Rogers HJ, et al. SF3B1 mutations are infrequently found in non-myelodysplastic bone marrow failure syndromes and mast cell diseases but, if present, are associated with the ring sideroblast phenotype. Haematologica. 2013;98:e105–e107. doi: 10.3324/haematol.2013.090506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patnaik MM, Hanson CA, Sulai NH, et al. Prognostic irrelevance of ring sideroblast percentage in World Health Organization-defined myelodysplastic syndromes without excess blasts. Blood. 2012;119:5674–5677. doi: 10.1182/blood-2012-03-415356. [DOI] [PubMed] [Google Scholar]
- 66.Visconte V, Avishai N, Mahfouz R, et al. Distinct iron architecture in SF3B1-mutant myelodysplastic syndrome patients is linked to an SLC25A37 splice variant with a retained intron. Leukemia. 2014 doi: 10.1038/leu.2014.170. doi: 10.1038/leu.2014.170. [DOI] [PubMed] [Google Scholar]
- 67.Nikpour M, Scharenberg C, Liu A, et al. The transporter ABCB7 is a mediator of the phenotype of acquired refractory anemia with ring sideroblasts. Leukemia. 2013;27:889–896. doi: 10.1038/leu.2012.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Visconte V, Rogers HJ, Tabarroki A, et al. Splicing factor 3b subunit 1 (SF3B1) heterozygous mice manifest a hematologic phenotype similar to low risk myelodysplastic syndromes with ring sideroblasts. Blood. 2013;122(ASH Annual Meeting):abst 259. [Google Scholar]
- 69.Visconte V, Tabarroki A, Zhang L, et al. Splicing factor 3b subunit 1 (Sf3b1) haploinsufficient mice display features of low risk Myelodysplastic syndromes with ring sideroblasts. J Hematol Oncol. 2014;7:89. doi: 10.1186/s13045-014-0089-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Matsunawa M, Yamamoto R, Sanada M, et al. Haploinsufficiency of Sf3b1 leads to compromised stem cell function but not to myelodysplasia. Leukemia. 2014;28:1844–1850. doi: 10.1038/leu.2014.73. [DOI] [PubMed] [Google Scholar]
- 71.Wang C, Sashida G, Saraya A, et al. Depletion of Sf3b1 impairs proliferative capacity of hematopoietic stem cells but is not sufficient to induce myelodysplasia. Blood. 2014;123:3336–3343. doi: 10.1182/blood-2013-12-544544. [DOI] [PubMed] [Google Scholar]
- 72.Thol F, Kade S, Schlarmann C, et al. Frequency and prognostic impact of mutations in SRSF2, U2AF1, and ZRSR2 in patients with myelodysplastic syndromes. Blood. 2012;119:3578–3584. doi: 10.1182/blood-2011-12-399337. [DOI] [PubMed] [Google Scholar]
- 73.Bonnal S, Vigevani L, Valcarcel J. The spliceosome as a target of novel antitumour drugs. Nat Rev Drug Discov. 2012;11:847–859. doi: 10.1038/nrd3823. [DOI] [PubMed] [Google Scholar]
- 74.Graubert TA, Shen D, Ding L, et al. Recurrent mutations in the U2AF1 splicing factor in myelodysplastic syndromes. Nat Genet. 2011;44:53–57. doi: 10.1038/ng.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Makishima H, Visconte V, Sakaguchi H, et al. Mutations in the spliceosome machinery, a novel and ubiquitous pathway in leukemogenesis. Blood. 2012;119:3203–3210. doi: 10.1182/blood-2011-12-399774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Przychodzen B, Jerez A, Guinta K, et al. Patterns of missplicing due to somatic U2AF1 mutations in myeloid neoplasms. Blood. 2013;122:999–1006. doi: 10.1182/blood-2013-01-480970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tripathi M, Lunn CL, Okeyo-Owuor T, Walter MJ, Webb TR, Graubert T. Sudemycin selectively inhibits growth of primary murine hematopoietic cells expressing mutant U2AF1. Blood. 2012;120(ASH Annual Meeting):abst 554. [Google Scholar]
- 78.Wu SJ, Kuo YY, Hou HA, et al. The clinical implication of SRSF2 mutation in patients with myelodysplastic syndrome and its stability during disease evolution. Blood. 2012;120:3106–3111. doi: 10.1182/blood-2012-02-412296. [DOI] [PubMed] [Google Scholar]
- 79.Komeno Y, Qiu J, Lin L, et al. SRSF2 is essential for hematopoiesis and its mutations dysregulate alternative RNA splicing in MDS. Blood. 2013;122(ASH Annual Meeting):abst 261. [Google Scholar]
- 80.Hamilton BK, Tabarroki A, Elson P, et al. Impact of allogeneic hematopoietic stem cell transplant (HSCT) on patients harboring the spliceosome mutation SRSF2. J Clin Oncol. 2013;31(Suppl):abst 7008. [Google Scholar]
- 81.Kurtovic Kozaric A, Makishima H, Przychodzen BP, et al. PRPF8 defects cause missplicing in myeloid malignancies. Blood. 2013;122(ASH Annual Meeting):abst 2838. doi: 10.1038/leu.2014.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gomez-Segui I, Makishima H, Jerez A, et al. Novel recurrent mutations in the RAS-like GTP-binding gene RIT1 in myeloid malignancies. Leukemia. 2013;27:1943–1946. doi: 10.1038/leu.2013.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kurtovic-Kozaric A, Przychodzen B, Singh J, et al. PRPF8 defects cause missplicing in myeloid malignancies. Leukemia. 2014 doi: 10.1038/leu.2014.144. doi: 10.1038/leu.2014.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Keightley MC, Crowhurst MO, Layton JE, et al. In vivo mutation of pre-mRNA processing factor 8 (Prpf8) affects transcript splicing, cell survival and myeloid differentiation. FEBS Lett. 2013;587:2150–2157. doi: 10.1016/j.febslet.2013.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu F, Zhao X, Perna F, et al. JAK2V617F-mediated phosphorylation of PRMT5 downregulates its methyltransferase activity and promotes myeloproliferation. Cancer Cell. 2011;19:283–294. doi: 10.1016/j.ccr.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ingram W, Lea NC, Cervera J, et al. The JAK2 V617F mutation identifies a subgroup of MDS patients with isolated deletion 5q and a proliferative bone marrow. Leukemia. 2006;20:1319–1321. doi: 10.1038/sj.leu.2404215. [DOI] [PubMed] [Google Scholar]
- 87.Jekarl DW, Han SB, Kim M, et al. JAK2 V617F mutation in myelodysplastic syndrome, myelodysplastic syndrome/myeloproliferative neoplasm, unclassifiable, refractory anemia with ring sideroblasts with thrombocytosis, and acute myeloid leukemia. Korean J Hematol. 2010;45:46–50. doi: 10.5045/kjh.2010.45.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Szpurka H, Tiu R, Murugesan G, et al. Refractory anemia with ringed sideroblasts associated with marked thrombocytosis (RARS-T), another myeloproliferative condition characterized by JAK2 V617F mutation. Blood. 2006;108:2173–2181. doi: 10.1182/blood-2006-02-005751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hellstrom-Lindberg E, Cazzola M. The role of JAK2 mutations in RARS and other MDS. Hematology Am Soc Hematol Educ Program. 2008:52–59. doi: 10.1182/asheducation-2008.1.52. [DOI] [PubMed] [Google Scholar]
- 90.Ohyashiki K, Aota Y, Akahane D, et al. The JAK2 V617F tyrosine kinase mutation in myelodysplastic syndromes (MDS) developing myelofibrosis indicates the myeloproliferative nature in a subset of MDS patients. Leukemia. 2005;19:2359–2360. doi: 10.1038/sj.leu.2403989. [DOI] [PubMed] [Google Scholar]
- 91.Makishima H, Jankowska AM, McDevitt MA, et al. CBL, CBLB, TET2, ASXL1, and IDH1/2 mutations and additional chromosomal aberrations constitute molecular events in chronic myelogenous leukemia. Blood. 2011;117:e198–e206. doi: 10.1182/blood-2010-06-292433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen CY, Lin LI, Tang JL, et al. RUNX1 gene mutation in primary myelodysplastic syndrome-the mutation can be detected early at diagnosis or acquired during disease progression and is associated with poor outcome. Br J Haematol. 2007;139:405–414. doi: 10.1111/j.1365-2141.2007.06811.x. [DOI] [PubMed] [Google Scholar]
- 93.Steensma DP, Gibbons RJ, Mesa RA, Tefferi A, Higgs DR. Somatic point mutations in RUNX1/CBFA2/AML1 are common in high-risk myelodysplastic syndrome, but not in myelofibrosis with myeloid metaplasia. Eur J Haematol. 2005;74:47–53. doi: 10.1111/j.1600-0609.2004.00363.x. [DOI] [PubMed] [Google Scholar]
- 94.Harada H, Harada Y, Niimi H, Kyo T, Kimura A, Inaba T. High incidence of somatic mutations in the AML1/RUNX1 gene in myelodysplastic syndrome and low blast percentage myeloid leukemia with myelodysplasia. Blood. 2004;103:2316–2324. doi: 10.1182/blood-2003-09-3074. [DOI] [PubMed] [Google Scholar]
- 95.Shih AH, Chung SS, Dolezal EK, et al. Mutational analysis of therapy-related myelodysplastic syndromes and acute myelogenous leukemia. Haematologica. 2013;98:908–912. doi: 10.3324/haematol.2012.076729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kulasekararaj AG, Smith AE, Mian SA, et al. TP53 mutations in myelodysplastic syndrome are strongly correlated with aberrations of chromosome 5, and correlate with adverse prognosis. Br J Haematol. 2013;160:660–672. doi: 10.1111/bjh.12203. [DOI] [PubMed] [Google Scholar]
- 97.Caceres G, McGraw K, Yip BH, et al. TP53 suppression promotes erythropoiesis in del(5q) MDS, suggesting a targeted therapeutic strategy in lenalidomide-resistant patients. Proc Natl Acad Sci U S A. 2013;110:16127–16132. doi: 10.1073/pnas.1311055110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tiacci E, Grossmann V, Martelli MP, Kohlmann A, Haferlach T, Falini B. The corepressors BCOR and BCORL1: two novel players in acute myeloid leukemia. Haematologica. 2012;97:3–5. doi: 10.3324/haematol.2011.057901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Damm F, Chesnais V, Nagata Y, et al. BCOR and BCORL1 mutations in myelodysplastic syndromes and related disorders. Blood. 2013;122:3169–3177. doi: 10.1182/blood-2012-11-469619. [DOI] [PubMed] [Google Scholar]
- 100.Gyan E, Frew M, Bowen D, et al. Mutation in RAP1 is a rare event in myelodysplastic syndromes. Leukemia. 2005;19:1678–1680. doi: 10.1038/sj.leu.2403882. [DOI] [PubMed] [Google Scholar]
- 101.Glynn EF, Megee PC, Yu HG, et al. Genome-wide mapping of the cohesin complex in the yeast Saccharomyces cerevisiae. PLoS Biol. 2004;2:E259. doi: 10.1371/journal.pbio.0020259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Thota S, Viny AD, Makishima H, et al. Genetic alterations of the cohesin complex genes in myeloid malignancies. Blood. 2014;124:1790–1798. doi: 10.1182/blood-2014-04-567057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Piazza R, Valletta S, Winkelmann N, et al. Recurrent SETBP1 mutations in atypical chronic myeloid leukemia. Nat Genet. 2013;45:18–24. doi: 10.1038/ng.2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Makishima H, Yoshida K, Nguyen N, et al. Somatic SETBP1 mutations in myeloid malignancies. Nat Genet. 2013;45:942–946. doi: 10.1038/ng.2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Damm F, Itzykson R, Kosmider O, et al. SETBP1 mutations in 658 patients with myelodysplastic syndromes, chronic myelomonocytic leukemia and secondary acute myeloid leukemias. Leukemia. 2013;27:1401–1403. doi: 10.1038/leu.2013.35. [DOI] [PubMed] [Google Scholar]
- 106.Thol F, Suchanek KJ, Koenecke C, et al. SETBP1 mutation analysis in 944 patients with MDS and AML. Leukemia. 2013;27:2072–2075. doi: 10.1038/leu.2013.145. [DOI] [PubMed] [Google Scholar]
- 107.Visconte V, Tabarroki A, Zhang L, et al. Clinicopathologic and molecular characterization of myeloid neoplasms harboring isochromosome 17(q10) Am J Hematol. 2014;89:862. doi: 10.1002/ajh.23755. [DOI] [PubMed] [Google Scholar]
- 108.Meggendorfer M, Bacher U, Alpermann T, et al. SETBP1 mutations occur in 9% of MDS/MPN and in 4% of MPN cases and are strongly associated with atypical CML, monosomy 7, isochromosome i(17)(q10), ASXL1 and CBL mutations. Leukemia. 2013;27:1852–1860. doi: 10.1038/leu.2013.133. [DOI] [PubMed] [Google Scholar]
- 109.Kerbauy DB, Deeg HJ. Apoptosis and antiapoptotic mechanisms in the progression of myelodysplastic syndrome. Exp Hematol. 2007;35:1739–1746. doi: 10.1016/j.exphem.2007.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhou L, McMahon C, Bhagat T, et al. Reduced SMAD7 leads to overactivation of TGF-beta signaling in MDS that can be reversed by a specific inhibitor of TGF-beta receptor I kinase. Cancer Res. 2011;71:955–963. doi: 10.1158/0008-5472.CAN-10-2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kornblau SM, McCue D, Singh N, Chen W, Estrov Z, Coombes KR. Recurrent expression signatures of cytokines and chemokines are present and are independently prognostic in acute myelogenous leukemia and myelodysplasia. Blood. 2010;116:4251–4261. doi: 10.1182/blood-2010-01-262071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Feng X, Scheinberg P, Wu CO, et al. Cytokine signature profiles in acquired aplastic anemia and myelodysplastic syndromes. Haematologica. 2011;96:602–606. doi: 10.3324/haematol.2010.030536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sloand EM, Melenhorst JJ, Tucker ZC, et al. T-cell immune responses to Wilms tumor 1 protein in myelodysplasia responsive to immunosuppressive therapy. Blood. 2011;117:2691–2699. doi: 10.1182/blood-2010-04-277921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Boultwood J, Fidler C, Kusec R, et al. Telomere length in myelodysplastic syndromes. Am J Hematol. 1997;56:266–271. doi: 10.1002/(sici)1096-8652(199712)56:4<266::aid-ajh12>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 115.Jiang J, Kulasekararaj AG, Krishnamurthy P, et al. Telomere length in MDS patients bone marrow is highly correlated with complex cytogenetics, IPSS risk groups and transfusion dependency. Blood. 2011;118(ASH Annual Meeting):abst 3826. [Google Scholar]
- 116.Sieglova Z, Zilovcova S, Cermak J, et al. Dynamics of telomere erosion and its association with genome instability in myelodysplastic syndromes (MDS) and acute myelogenous leukemia arising from MDS: a marker of disease prognosis? Leuk Res. 2004;28:1013–1021. doi: 10.1016/j.leukres.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 117.Yamaguchi H, Baerlocher GM, Lansdorp PM, et al. Mutations of the human telomerase RNA gene (TERC) in aplastic anemia and myelodysplastic syndrome. Blood. 2003;102:916–918. doi: 10.1182/blood-2003-01-0335. [DOI] [PubMed] [Google Scholar]
- 118.Kirwan M, Vulliamy T, Marrone A, et al. Defining the pathogenic role of telomerase mutations in myelodysplastic syndrome and acute myeloid leukemia. Hum Mutat. 2009;30:1567–1573. doi: 10.1002/humu.21115. [DOI] [PubMed] [Google Scholar]
- 119.Ueda Y, Calado RT, Norberg A, et al. A mutation in the H/ACA box of telomerase RNA component gene (TERC) in a young patient with myelodysplastic syndrome. BMC Med Genet. 2014;15:68. doi: 10.1186/1471-2350-15-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shen L, Kantarjian H, Guo Y, et al. DNA methylation predicts survival and response to therapy in patients with myelodysplastic syndromes. J Clin Oncol. 2010;28:605–613. doi: 10.1200/JCO.2009.23.4781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Smith SM, Le Beau MM, Huo D, et al. Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood. 2003;102:43–52. doi: 10.1182/blood-2002-11-3343. [DOI] [PubMed] [Google Scholar]
- 122.Koh Y, Kim I, Bae JY, et al. Prognosis of secondary acute myeloid leukemia is affected by the type of the preceding hematologic disorders and the presence of trisomy 8. Jpn J Clin Oncol. 2010;40:1037–1045. doi: 10.1093/jjco/hyq097. [DOI] [PubMed] [Google Scholar]
- 123.Mauritzson N, Albin M, Rylander L, et al. Pooled analysis of clinical and cytogenetic features in treatment-related and de novo adult acute myeloid leukemia and myelodysplastic syndromes based on a consecutive series of 761 patients analyzed 1976-1993 and on 5098 unselected cases reported in the literature 1974-2001. Leukemia. 2002;16:2366–2378. doi: 10.1038/sj.leu.2402713. [DOI] [PubMed] [Google Scholar]
- 124.Third MIC Cooperative Study Group. Recommendations for a morphologic, immunologic, and cytogenetic (MIC) working classification of the primary and therapy-related myelodysplastic disorders. Report of the workshop held in Scottsdale, Arizona, USA, on February 23-25, 1987. Cancer Genet Cytogenet. 1988;32:1–10. [PubMed] [Google Scholar]