Abstract
We validated the basic life support termination of resuscitation (BLS TOR) rule retrospectively using Out-of-Hospital Cardiac Arrest (OHCA) data of metropolitan emergency medical service (EMS) in Korea. We also tested it by investigating the scene time interval for supplementing the BLS TOR rule. OHCA database of Seoul (January 2011 to December 2012) was used, which is composed of ambulance data and hospital medical record review. EMS-treated OHCA and 19 yr or older victims were enrolled, after excluding cases occurred in the ambulance and with incomplete information. The primary and secondary outcomes were hospital mortality and poor neurologic outcome. After calculating the sensitivity (SS), specificity (SP), and the positive and negative predictive values (PPV and NPV), tested the rule according to the scene time interval group for sensitivity analysis. Of total 4,835 analyzed patients, 3,361 (69.5%) cases met all 3 criteria of the BLS TOR rule. Of these, 3,224 (95.9%) were dead at discharge (SS,73.5%; SP,69.6%; PPV,95.9%; NPV, 21.3%) and 3,342 (99.4%) showed poor neurologic outcome at discharge (SS, 75.2%; SP, 89.9%; PPV, 99.4%; NPV, 11.5%). The cut-off scene time intervals for 100% SS and PPV were more than 20 min for survival to discharge and more than 14 min for good neurological recovery. The BLS TOR rule showed relatively lower SS and PPV in OHCA data in Seoul, Korea.
Graphical Abstract
Keywords: Out-of-Hospital Cardiac Arrest, Cardiopulmonary Resuscitation, Decision Support Technique
INTRODUCTION
Despite many improvements in the emergency medical service (EMS) system and in the technique of cardiopulmonary resuscitation (CPR), survival rate of adult patients with out-of hospital cardiac arrests (OHCA) is still low. The survival rates are even lower for patients who have no response to basic life support (BLS) compared to the rest patients with OHCA (1, 2). However, for patients who are not likely to achieve return of spontaneous circulation (ROSC), the same amount of resources and time are used to transport these patients to the emergency department. A retrospective analysis of fatal ambulance crashes showed most crashes (202/339) and fatalities (233/405) occurred during emergency use, and most crashes resulted in at least one fatality (3). Fatal traffic accidents caused by rushing ambulances with lights and sirens hurt not only the patients and EMS personnel on board but also pedestrians and the passengers of other vehicles. Therefore, traffic accidents caused by unnecessary ambulance transport can be a potential danger to the community. To reduce the rate of hospital transport without compromising the care of potentially viable patients, many previous studies have tried to establish and validate termination of resuscitation (TOR) rules in pre-hospital OHCA situations.
The 2010 American Heart Association (AHA) resuscitation guidelines recommend that regional or local EMS authorities use the BLS TOR rule to develop protocols for the termination of resuscitative efforts by BLS providers for adult patients of cardiac arrest in areas where advanced life support (ALS) is not available or may be significantly delayed (Class I, LOE A) (4). To consider terminating BLS resuscitative attempts for adult OHCA patients, all 3 of following criteria must be present before moving the patient to the ambulance for transport: 1) arrest was not witnessed by an EMS provider or first responder; 2) there was no ROSC prior to transport; and 3) no automated electronic defibrillator (AED) shock was delivered. The recommendation was based on a clinical decision rule called the basic life support termination of resuscitation (BLS TOR) rule. The BLS TOR rule was derived by Verbeek et al. (5) through a retrospective review of case records from a large, urban EMS system where emergency medical technicians (EMTs) are trained to use an AED. The BLS TOR rule has been validated in the US, Canada, and Europe and was proven to generate high specificity and a positive predictive value (6, 7, 8, 9, 10, 11). In one study, the BLS TOR rule proved to reduce the rate of hospital transport to 37% of cardiac arrests without compromising the care of potentially viable patients (12).
East Asian EMS systems in Korea, Japan, and Taiwan have mostly a single-tier ambulance system, and only BLS can be provided to cardiac arrest patients before arriving to the hospital. EMTs are trained to provide BLS and use AEDs for rhythm analysis and defibrillation in the field. Unlike North America and Europe, EMTs provide CPR at the scene for a relatively short period of time and transport the patients with on-going CPR in a moving ambulance to the hospital according to their protocol. These systems do not allow EMTs to use the BLS TOR rule (13). The scene time interval (STI) is the critical period to provide high quality CPR, intubation, and fluid resuscitation in East Asian EMSs. If the STI is not enough to provide CPR before transporting patients to the emergency department (ED), the rule cannot be used or one should consider a modification of the rule components. Our purpose is to validate the BLS TOR rule retrospectively for predictive performance and perform the sensitivity analysis according to the STI.
MATERIALS AND METHODS
The study is one of Cardiac Arrest Registry and Encouragement of Excellent Resuscitation (CAREER) projects. CARRER project is a population-based emergency medical services intervention trial since 2011 in Seoul, Korea.
Study design and setting
This study was a retrospective validation of the BLS TOR rule. The setting of location was Seoul, the capital city of the Republic of Korea, with a population of approximately ten million people in 605 km2, consisting mostly of urban areas. There are 114 ambulance stations and 23 EMS agencies. One ambulance has three crewmembers: a level-1 EMT, a level-2 EMT, and a driver. The EMS service level is equivalent to an intermediate level of service in North America. EMS personnel provide CPR at the scene according to the 2010 AHA CPR guidelines, with a 30:2 compression-to-ventilation ratio and advanced airway or bag-valve-mask ventilation. They are encouraged to provide four cycles of CPR and rhythm analysis and to transport the patient to an ED, continuing CPR during ambulance transport. A public access defibrillator program was approved in 2009, and the city started a program to set up AEDs in public places in 2009. However, few cases were defibrillated by laypersons in this study period.
Data source
The dataset included all registered OHCAs from January 1, 2011, to December 31, 2012. OHCA databases were composed of EMS data from ambulance run sheets, an EMS OHCA registry completed by the attending level-1 EMT, and the hospital medical record review containing the Utstein templates. Ambulance run sheets and EMS OHCA registry are filled after transporting patients to the ED and stored at the central server of the Seoul Metropolitan Fire Department (SMFD). We extracted the cases from the database at SMFD. Hospital records for all cases were reviewed by medical record reviewers after three months by the Korea Centers for Disease Control and Prevention (KCDC) for follow-up, including the etiology, co-morbidity, and outcomes, survival to discharge and the good neurological recovery using the cerebral performance category (CPC) (where 1=good cerebral performance [conscious, alert, able to work and lead a normal life]; 2=moderate cerebral disability [conscious and able to function independently-dress, travel, prepare food-but may have hemiplegia, seizures, or permanent memory or mental changes]; 3=severe cerebral disability [conscious, dependent on others for daily support, functions only in an institution or at home with exceptional family support]; 4=coma or vegetative state; and 5=death).
Study population
EMS-treated and 19 yr old or older patients with presumed cardiac etiology were included. Patients who collapsed in the ambulance, patients with incomplete information in their registry regarding defibrillation provided by the EMS providers, presence of ROSC before ambulance transport and hospital outcomes were excluded.
Data variables
The variables collected were age, gender, response time between the initial call and the ambulance's arrival to the scene, scene time interval from arrival to departure to ED, number of witnesses, number of bystanders (EMS provider or lay person), bystander-administered CPR, use of EMS defibrillation, pre-hospital ROSC, and first ECG. The primary and secondary end-points were hospital mortality and poor neurological recovery (CPC 3, 4, or 5).
Statistical analysis
We retrospectively applied the BLS TOR rule to patients' data using AHA's three components, and calculated the predictive performance (percent and 95% confidence interval) of the rule, such as sensitivity (SS), specificity (SP), positive and negative predictive value (PPV and NPV) for hospital mortality and poor neurological recovery. We performed the sensitivity analysis on the performance value (SS, SP, PPV, and NPV) to find the cut-off value of STI for achieving 100% SP and 100% PPV for the study end-points.
Ethics statement
This study was approved by the institutional review board of Seoul National University Hospital (IRB No.1103-153-357). Informed consent was waived by the board because of the observational nature of the study.
RESULTS
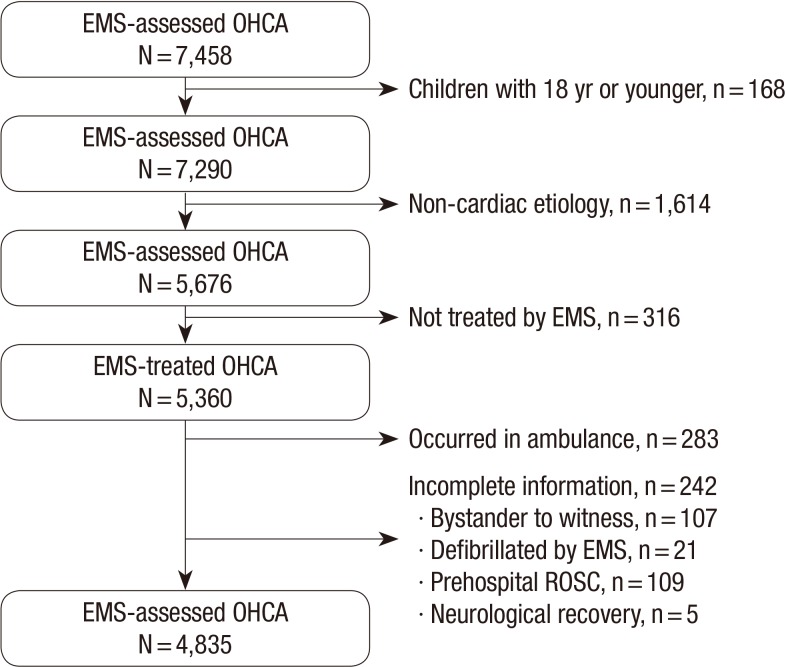
Of the 7,458 OHCA patients, we enrolled 4,835 patients. The following were excluded: children (n=168), non-cardiac etiology (n=1,641), patients not treated by EMS (n=316), occurred in ambulance (n=283) and incomplete information (n=242) (bystander to witness, n=107), defibrillation by EMS provider (n=21), prehospital ROSC (n=109), and neurological recovery (n=5) (Fig. 1). Among the enrolled 4,835 EMS-treated OHCA patients, 4,685 patients (96.9%) were not witnessed by emergency medical service personnel, 4,612 patients (95.4%) had no ROSC prior to transport, and 3,489 (72.2%) patients had no AED shock delivered (Table 1).
Fig. 1.
Patient enrollment flow. EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation.
Table 1.
Demographic findings of study population
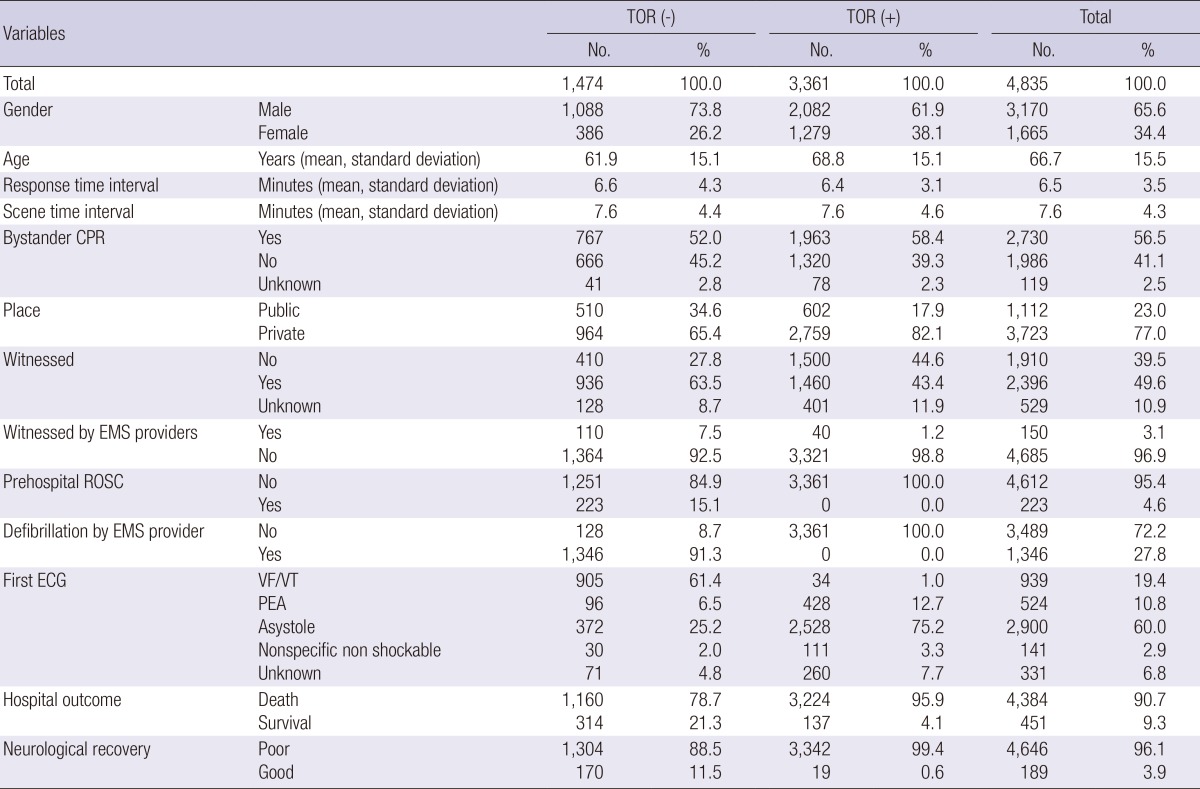
TOR, termination of resuscitation; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation; VF/VT, ventricular fibrillation/ventricular tachycardia; PEA, pulseless electrical activity.
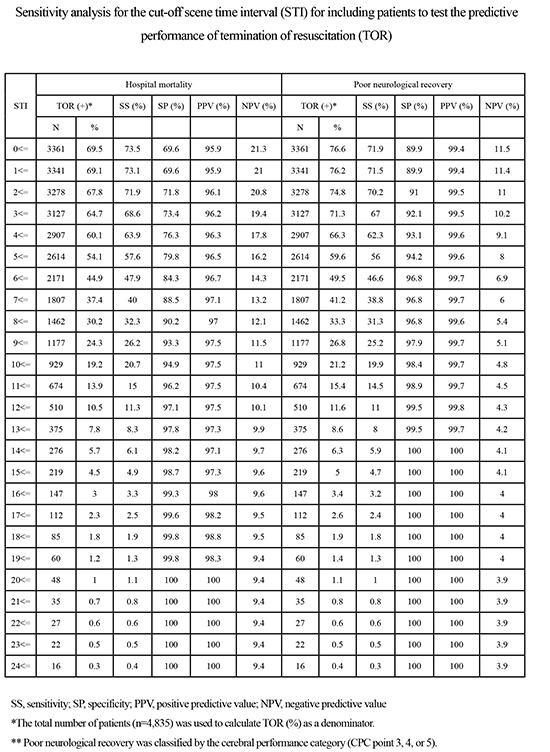
Overall, 3,361 (69.5%) patients met all 3 criteria of the BLS TOR rule, and resuscitative efforts for these patients might have been terminated before transport to the hospital if the BLS TOR rule was applied strictly. Of these, 3,224 (95.9%) were dead at discharge (SS, 73.5%; SP, 69.6%; PPV, 95.9%; NPV, 21.3%), and 3,342 (99.4%) showed poor neurologic recovery (SS, 75.2%; SP, 89.9%; PPV, 99.4%; NPV, 11.5%) (Table 2). The cut-off STIs for achieving 100% specificity and 100% positive predictive value for selecting patients were 20 min for hospital mortality with 48 cases (1.0% of all patients) and 14 min for poor neurological recovery with 276 cases (6.3%), respectively (Table 3).
Table 2.
Sensitivity, specificity, positive predictive value, and negative predictive value of termination of resuscitation rule (TOR) for hospital mortality and poor neurological outcome at discharge
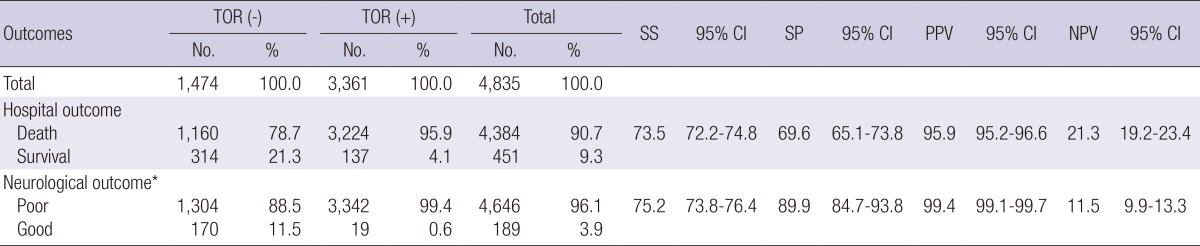
13.395% CI, 95% confidence interval. *Good neurological outcome was classified by the cerebral performance category with good (1 and 2) and poor (3, 4, or 5). SS, sensitivity; SP, specificity; PPV, positive predictive value; NPV, negative predictive value.
Table 3.
Sensitivity analysis for the cut-off scene time interval (STI) for including patients to test the predictive performance of termination of resuscitation (TOR)
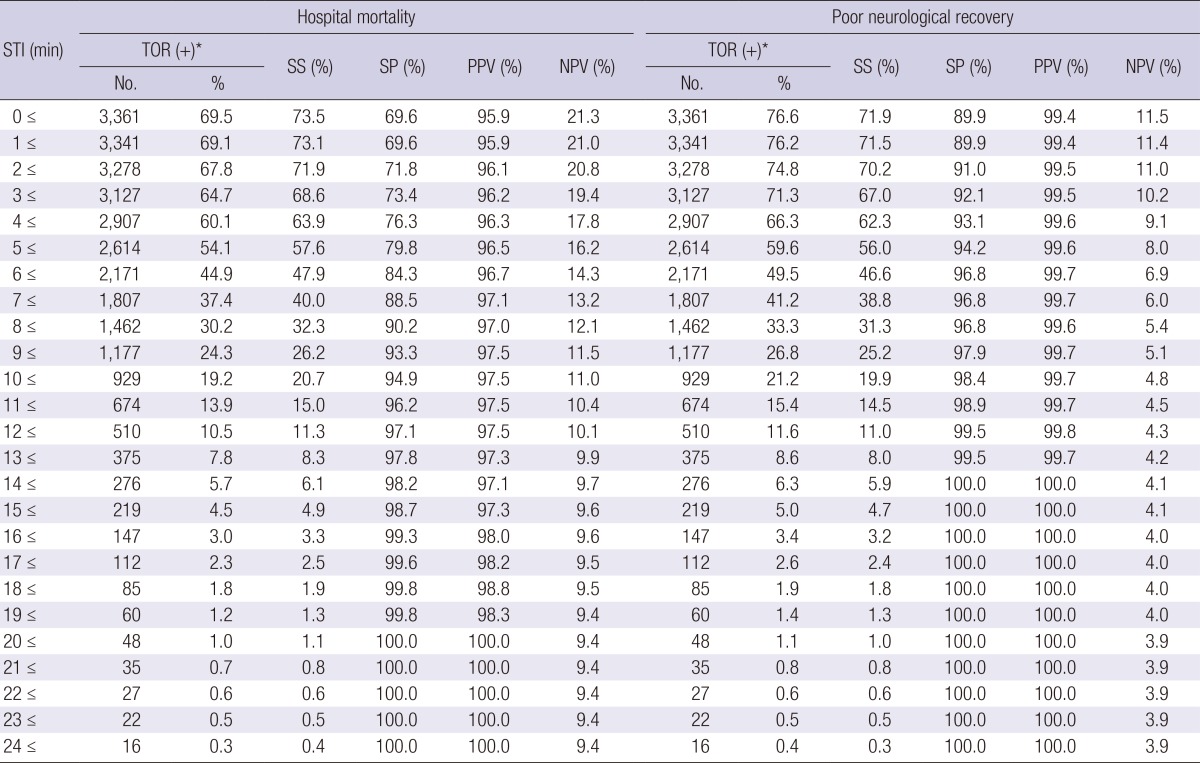
*The total number of patients (n=4,835) was used to calculate TOR (%) as a denominator. SS, sensitivity; SP, specificity; PPV, positive predictive value; NPV, negative predictive value.
DISCUSSION
We validated the basic life support termination of resuscitation (BLS TOR) rule retrospectively using OHCA data of Seoul metropolitan EMS in Korea. We also tested it by investigating the scene time interval for supplementing the BLS TOR rule.
There were several previous studies suggesting the TOR rule in the BLS system, and a few guidelines for TOR have been proposed by researchers (5, 14, 15). Verbeek et al. (5) reviewed 700 cases in which the BLS defibrillator system was used and found that ROSC, defibrillation, and arrest witnessed by EMS to have the strongest association with survival. From these factors, they proposed the BLS TOR rule. Our study also showed significant differences between the following 3 factors and hospital mortality: witnessed by EMS provider (P=0.007), pre-hospital ROSC (P<0.001), and pre-hospital defibrillation (P<0.001). Our study, however showed, when the BLS TOR rule was applied to the Seoul EMS data, the survival rate of OHCA patients who the BLS TOR rule suggested termination was 4.1% (Table 2). Generally, in clinical rule validation studies, 1% or less survival rate was suggested as reflective of medical futility (16). Because our validation results did not satisfy the medical futility limits, the BLS TOR rule should not be implemented without modification, or a new rule that has a better ability to predict performance should be developed.
Although the BLS TOR rule was validated in other countries and been proven to show high specificity and a positive predictive value (6, 7, 8, 9, 10, 11), our study showed a much lower specificity and positive predictive value than other previous validation studies on the same BLS TOR rule. Compared to other previous validation studies with higher specificity, there was a much higher portion of patients who satisfied each criteria of the BLS TOR rule. The reason for this finding was not clear. One of the reasons could be the difference in EMS performance. One of the criteria of the BLS TOR rule is whether a patient had gained ROSC prior to transport. The original rule did not specify a time limit before achieving ROSC at the scene (scene time interval). Because of this vagueness, the TOR rule would produce different results because local EMS systems have different BLS protocols or algorithms for transporting OHCA patients. Therefore, the 2010 AHA guidelines expand on this and recommend applying the TOR rule after three full rounds of CPR and AED analysis (4). Regardless, we still found a low specificity (84.3%) and positive predictive value (96.7%) for hospital mortality when we tested the performance for patients excluding those with STI less than 6 min (Table 3), considering 1 cycle of CPR takes 2 min. For this cut-off STI, 1,190 (35.4%) patients would be excluded. This may imply that Korean EMS tends to be more focused on faster transfer to a designated ED rather than longer in-field procedures such as several cycles of CPR or defibrillation.
Unlike an STI of 20 min in the United States (17, 18), the 7 min of median STI (mean 7.6 min) in our TOR(+) group (median of 9 min of STI even though STI less than 6 min and unresponsive patients were excluded) was too short to achieve ROSC prior to transport or to pronounce death. Our study proposes that the TOR rule should be modified or revised to reflect these CPR protocols. We compare the study results with previous studies performed in Japan and Singapore in Appendix 1 (19, 20). Specificity of the BLS TOR rule in all 3 studies is lower than 0.9, which demonstrates a lower specificity result from previous validation studies performed in North America. A lower specificity of the BLS TOR rule in Asia could imply that the BLS TOR rule could misjudge possible survivors of OHCA or recommend TOR in these patients before they are transported to hospitals.
Our study had a number of limitations. First, our study was a retrospective validation of an existing rule. If we used the rule to validate prospectively, we may have obtained different results. However, it was too hard to validate this TOR rule in the EMS setting due to ethical issues. Second, we excluded a number of patients due to incomplete information which could lead to bias for performance. Third, although a recent study performed in Korea and Japan showed a positive association between intermediate STI from 8 to 16 min and good neurological outcomes after OHCA (21), inclusion of STI in TOR rule could be a controversy because there was only few study regarding relation between STI and patients' outcome. Moreover there is no specific comment in 2010 AHA guideline regarding optimal scene treatment time for EMS personnel providing CPR in the scene. Additionally our study used STI instead of the real treatment time interval, which could reflect the other time frame such as vertical response time. Therefore, the real treatment time interval would be shorter than STI.
In conclusion, the BLS TOR rule showed a relatively low specificity and positive predictive value when retrospectively validated with OHCA data from Seoul, Korea. With additional sensitivity analysis, an STI longer than 20 min for hospital mortality and 14 min for poor neurological recovery was derived to achieve 100% performance of each for a very select group of patients. Further efforts of modifying and validating BLS TOR rule to fit into Korean EMS system is needed in the future based on our study results.
Appendix 1
Comparison of validation studies on basic life support (BLS) termination of resuscitation (TOR) rule in Asian countries for out-of-hospital cardiac arrest
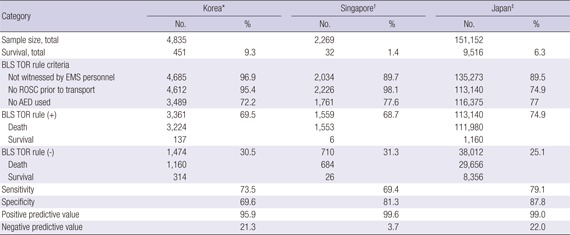
*Korea, current study; †Ong ME, Tan EH, Ng FS, Yap S, Panchalingham A, Leong BS, Ong VY, Tiah L, Lim SH, Venkataraman A. Comparison of termination-of-resuscitation guidelines for out-of-hospital cardiac arrest in Singapore EMS. Resuscitation 2007; 75: 244-51. (Reference 19); ‡Kajino K, Kitamura T, Iwami T, Daya M, Ong ME, Hiraide A, Shimazu T, Kishi M, Yamayoshi S. Current termination of resuscitation (TOR) guidelines predict neurologically favorable outcome in Japan. Resuscitation 2013; 84: 54-9. (Reference 20). EMS, emergency medical service; ROSC, return of spontaneous circulation.
Footnotes
The study was financially supported by the Korea Centers for Disease Control and Prevention (2012E3301000).
All authors have no potential conflicts of interest to disclose in this study.
Conceived and designed the experiments: SD Shin, TH Kim. Performed the experiments: TH Kim, YJ Kim, CH Kim. Analyzed the data: TH Kim, JE Kim. Contributed reagents/materials/analysis tools: CH Kim, YJ Kim. Wrote the first draft of the manuscript: TH Kim, SD Shin. Wrote the paper: TH Kim, YJ Kim, CH Kim, SD Shin. ICMJE criteria for authorship read and met: TH Kim, SD Shin. Agree with manuscript results and conclusions: TH Kim, SD Shin, YJ Kim, CH Kim, JE Kim.
References
- 1.Stiell IG, Wells GA, Spaite DW, Nichol G, O'Brien B, Munkley DP, Field BJ, Lyver MB, Luinstra LG, Dagnone E, et al. OPALS Study Group. The Ontario Prehospital Advanced Life Support (OPALS) study Part II: Rationale and methodology for trauma and respiratory distress patients. Ann Emerg Med. 1999;34:256–262. doi: 10.1016/s0196-0644(99)70241-6. [DOI] [PubMed] [Google Scholar]
- 2.Finlay I, Dallimore D. Your child is dead. BMJ. 1991;302:1524–1525. doi: 10.1136/bmj.302.6791.1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahn CA, Pirrallo RG, Kuhn EM. Characteristics of fatal ambulance crashes in the United States: an 11-year retrospective analysis. Prehosp Emerg Care. 2001;5:261–269. doi: 10.1080/10903120190939751. [DOI] [PubMed] [Google Scholar]
- 4.Morrison LJ, Kierzek G, Diekema DS, Sayre MR, Silvers SM, Idris AH, Mancini ME. Part 3: ethics: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S665–S675. doi: 10.1161/CIRCULATIONAHA.110.970905. [DOI] [PubMed] [Google Scholar]
- 5.Verbeek PR, Vermeulen MJ, Ali FH, Messenger DW, Summers J, Morrison LJ. Derivation of a termination-of-resuscitation guideline for emergency medical technicians using automated external defibrillators. Acad Emerg Med. 2002;9:671–678. doi: 10.1111/j.1553-2712.2002.tb02144.x. [DOI] [PubMed] [Google Scholar]
- 6.Richman PB, Vadeboncoeur TF, Chikani V, Clark L, Bobrow BJ. Independent evaluation of an out-of-hospital termination of resuscitation (TOR) clinical decision rule. Acad Emerg Med. 2008;15:517–521. doi: 10.1111/j.1553-2712.2008.00110.x. [DOI] [PubMed] [Google Scholar]
- 7.Morrison LJ, Verbeek PR, Zhan C, Kiss A, Allan KS. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation. 2009;80:324–328. doi: 10.1016/j.resuscitation.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Ong ME, Jaffey J, Stiell I, Nesbitt L OPALS Study Group. Comparison of termination-of-resuscitation guidelines for basic life support: defibrillator providers in out-of-hospital cardiac arrest. Ann Emerg Med. 2006;47:337–343. doi: 10.1016/j.annemergmed.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 9.Sasson C, Hegg AJ, Macy M, Park A, Kellermann A, McNally B CARES Surveillance Group. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA. 2008;300:1432–1438. doi: 10.1001/jama.300.12.1432. [DOI] [PubMed] [Google Scholar]
- 10.Ruygrok ML, Byyny RL, Haukoos JS Colorado Cardiac Arrest & Resuscitation Collaborative Study Group; Denver Metro EMS Medical Directors. Validation of 3 termination of resuscitation criteria for good neurologic survival after out-of-hospital cardiac arrest. Ann Emerg Med. 2009;54:239–247. doi: 10.1016/j.annemergmed.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Skrifvars MB, Vayrynen T, Kuisma M, Castren M, Parr MJ, Silfverstople J, Svensson L, Jonsson L, Herlitz J. Comparison of Helsinki and European Resuscitation Council "do not attempt to resuscitate" guidelines, and a termination of resuscitation clinical prediction rule for out-of-hospital cardiac arrest patients found in asystole or pulseless electrical activity. Resuscitation. 2010;81:679–684. doi: 10.1016/j.resuscitation.2010.01.033. [DOI] [PubMed] [Google Scholar]
- 12.Morrison LJ, Visentin LM, Kiss A, Theriault R, Eby D, Vermeulen M, Sherbino J, Verbeek PR TOR Investigators. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2006;355:478–487. doi: 10.1056/NEJMoa052620. [DOI] [PubMed] [Google Scholar]
- 13.Shin SD, Ong ME, Tanaka H, Ma MH, Nishiuchi T, Alsakaf O, Karim SA, Khunkhlai N, Lin CH, Song KJ, et al. Comparison of emergency medical services systems across Pan-Asian countries: a Web-based survey. Prehosp Emerg Care. 2012;16:477–496. doi: 10.3109/10903127.2012.695433. [DOI] [PubMed] [Google Scholar]
- 14.Petrie DA, De Maio V, Stiell IG, Dreyer J, Martin M, O'Brien JA. Factors affecting survival after prehospital asystolic cardiac arrest in a Basic Life Support-Defibrillation system. CJEM. 2001;3:186–192. doi: 10.1017/s1481803500005522. [DOI] [PubMed] [Google Scholar]
- 15.Marsden AK, Ng GA, Dalziel K, Cobbe SM. When is it futile for ambulance personnel to initiate cardiopulmonary resuscitation? BMJ. 1995;311:49–51. doi: 10.1136/bmj.311.6996.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Ann Intern Med. 1990;112:949–954. doi: 10.7326/0003-4819-112-12-949. [DOI] [PubMed] [Google Scholar]
- 17.Mohr M, Bahr J, Schmid J, Panzer W, Kettler D. The decision to terminate resuscitative efforts: results of a questionnaire. Resuscitation. 1997;34:51–55. doi: 10.1016/s0300-9572(96)01048-9. [DOI] [PubMed] [Google Scholar]
- 18.Zive D, Koprowicz K, Schmidt T, Stiell I, Sears G, Van Ottingham L, Idris A, Stephens S, Daya M Resuscitation Outcomes Consortium Investigators. Variation in out-of-hospital cardiac arrest resuscitation and transport practices in the Resuscitation Outcomes Consortium: ROC Epistry-Cardiac Arrest. Resuscitation. 2011;82:277–284. doi: 10.1016/j.resuscitation.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ong ME, Tan EH, Ng FS, Yap S, Panchalingham A, Leong BS, Ong VY, Tiah L, Lim SH, Venkataraman A, et al. Comparison of termination-of-resuscitation guidelines for out-of-hospital cardiac arrest in Singapore EMS. Resuscitation. 2007;75:244–251. doi: 10.1016/j.resuscitation.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 20.Kajino K, Kitamura T, Iwami T, Daya M, Ong ME, Hiraide A, Shimazu T, Kishi M, Yamayoshi S. Current termination of resuscitation (TOR) guidelines predict neurologically favorable outcome in Japan. Resuscitation. 2013;84:54–59. doi: 10.1016/j.resuscitation.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 21.Shin SD, Kitamura T, Hwang SS, Kajino K, Song KJ, Ro YS, Nishiuchi T, Iwami T Seoul-Osaka Resuscitation Study (SORS) Group. Association between resuscitation time interval at the scene and neurological outcome after out-of-hospital cardiac arrest in two Asian cities. Resuscitation. 2014;85:203–210. doi: 10.1016/j.resuscitation.2013.10.021. [DOI] [PubMed] [Google Scholar]