Abstract
Background:
Tobacco smoking is an integral part of prison life and an established part of the culture. Little attention has been paid to prevention of smoking in prison. Approximately 70–80% of prisoners have been identified as current smokers. Aim: To assess the effectiveness of smoking cessation intervention among male prisoners at Central Jail, Bangalore city.
Aim:
To assess the effectiveness of smoking cessation intervention among male prisoners at Central Jail, Bangalore city.
Materials and Methods:
A randomized controlled trial was planned among male prisoners in Central Jail, Bangalore city. There were 1600 convicted prisoners. A self-administered questionnaire was given to the prisoners to assess their smoking behavior by which prevalence of tobacco smoking was found. Exactly 1352 tobacco users were studied. Among them, there were 1252 smokers. Based on inclusion criteria and informed consent given by the prisoners, a sample of 600 was chosen for the study by systematic random sampling. Among the 600 prisoners, 300 were randomly selected for the study group and 300 for the control group.
Results:
Prevalence of tobacco smoking among the prisoners was 92.60%. In the present study, after smoking cessation intervention, 17% showed no change in smoking, 21.66% reduced smoking, 16% stopped smoking, and 45.33% relapsed (P < 0.0001) at the end of 6-month follow-up in the study group.
Conclusion:
Tobacco use was high among the prisoners. Tobacco reduction is possible in the prison even if the living conditions are not favorable. Relatively high rate of relapse in our study indicates that some policies should be adopted to improve smokers’ information on consequences of tobacco on health and motivational intervention should be added to prisoners.
Keywords: Male prisoners smoking, motivational interviewing, smoking cessation
INTRODUCTION
Tobacco is a highly addictive substance. It is estimated that 1.9 billion people currently smoke worldwide. Tobacco kills one in two users. It is responsible for the death of 1 in 10 adults, with 4.9 million deaths occurring worldwide each year.[1] Prisoners are a special population with high prevalence of smoking. Approximately 70–80% of prisoners have been identified as current smokers. Prisoners are also more likely to have comorbid conditions (psychiatric disorders) and substance dependence, and there is less likelihood of smoking cessation among prisoners in the absence of intensive interventions. Referring to Butler et al.[2] “Tobacco smoking is an integral part of prison life and an established part of the culture.” Little attention has been paid to smoking prevention in prison. Prevalence rates of smoking in prison are at least double or even triple compared to the general population.[3] The various treatment approaches for smoking cessation include cognitive–behavioral strategies (self-monitoring and coping skills), motivational strategies (techniques to clarify desire for change and reduce ambivalence toward change), and social influence strategies (addressing the social influences that serve to promote or maintain smoking). Motivational interviewing (MI) is a directive, patient-centered style of counseling, designed to help people to explore and resolve ambivalence about behavior change. The concept of MI evolved from experience in treating alcohol abuse, and was first described by Miller in 1983.[4] The aim of this study was to assess the effectiveness of smoking cessation intervention by MI in male prisoners at Central Jail, Parappana Agrahara, Bangalore.
MATERIALS AND METHODS
A randomized controlled study was conducted to assess the effectiveness of smoking cessation intervention among male prisoners at Central Jail in Bangalore city. The study was carried out on convicted male prisoners. Ethical clearance was obtained from the ethical committee of the Oxford Dental College, Hospital and Research Centre, Bangalore, India. The Inspector General Officer of the Central Jail was approached, and the details of the study were explained to him and his approval was obtained to proceed with the study. There were 4600 prisoners in the Central Jail, of which 1600 were convicted male prisoners, 2700 were undertrial prisoners, and 300 were female prisoners. A self-administered questionnaire was given to the prisoners to assess their smoking behavior by which the prevalence of tobacco smoking was found. Prevalence of tobacco use that included both chewable and smoking tobacco was 84.5% and prevalence of smoking among prisoners was 92.60%. Sample size was estimated at 95% Confidence Interval for 5% margin of error. The sample size required for the study was 300 per group. Inclusion criteria were current adult smokers who smoked any tobacco product either daily or occasionally at the time of the study, convicted male prisoners with at least 1 year left to serve, and prisoners giving informed consent to quit smoking.
Exclusion criteria were inmates with acute mental illness (current suicidal ideation/actively psychotic) or mental retardation such that they could not provide informed consent and medically compromised inmates (like those with respiratory disorders). Fagerstrom questionnaire was used to determine the level of nicotine addiction. The degree of nicotine dependency was assessed by Fagerstrom test. Smokerlyzer, the Micro CO monitor, was used to measure alveolar carbon monoxide in ppm concentrations and the percentage carboxyhemoglobin (COHB). Before commencing the study, a pilot study was performed. Informed consent was obtained. To the 1600 convicted prisoners, a self-administered questionnaire was given to assess their smoking behavior by which the prevalence of tobacco was found. There were 1352 tobacco users in the present study. Among these, there were 1252 smokers. Based on inclusion criteria, a sample of 600 was chosen for the study by systematic random sampling. Among 600 prisoners, 300 were selected for each group (study and control) by simple random sampling. Motivational intervention was given for the study group. The topics for the intervention included: introduction to tobacco, prevalence of tobacco use, effects of tobacco use on general health and dental health, psychosocial factors influencing tobacco use, healthy diet and behavioral intervention for prevention of tobacco use. Follow-up was done for both study and control groups at the end of the 6th month using the same proforma, and Fagerstrom test was done by using Fagerstrom questionnaire and carbon monoxide grade was estimated by using smokerlyzer.
All the data were entered into a database on Microsoft Excel. Microsoft Word and Excel have been used to generate tables and graphs. Statistical analysis was done using SPSS software version 16. Descriptive statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean (SD) (Min.–Max.) and the results on categorical measurements are presented as number (%). Significance was assessed at 5% level of significance. Chi-square/Fisher's exact test were used to find the significance of study parameters on a categorical scale between two or more groups.
RESULTS
The total study population was 600: 300 in the study group and 300 in the control group. Response rate was 90%. Also, 5% prisoners in the study group and 3% prisoners in the control group were aged between 18 and 20 years, 44% prisoners in the study group and 48.66% prisoners in the control group were between 21 and 30 years, 32.33% prisoners in the study group and 29.33% prisoners in the control group were between 31 and 40 years, 11.66% prisoners in the study group and 11.66% prisoners in the control group were between 41 and 50 years, and 7% prisoners in the study group and 7.33% prisoners in the control group were 51–60 years of age. Among the tobacco users, 1252 (92.60%) were smokers [Table 1]. Age of onset of tobacco usage showed that it was 15–20 years in 45.33% in the study group and 39.66% in the control group, 21–30 years in 47.66% in the study group and 53% in the control group, and more than 30 years in 7.0% in the study group and 7.33% in the control group. 48.33% prisoners in the study group and 52% prisoners in the control group started using tobacco due to stress. About 90.66% in the study group gave prison stress as the reason that increased the need for tobacco use. Prisoners who were willing to quit tobacco use formed 88.66% in the study group and 78% prisoners in the control group [Table 2], and 11.33% prisoners in the study group and 22% prisoners in the control group were not willing to quit tobacco. Also, 64.28% prisoners in the study group and 70.51% prisoners in the control group wanted to quit tobacco due to health reasons.
Table 1.
Prevalence and characteristics of tobacco users in the study population
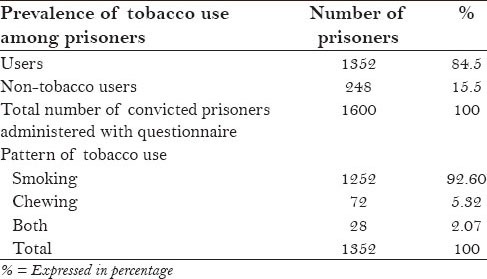
Table 2.
Distribution of the study population according to tobacco usage before and after intervention in the study group prisoners
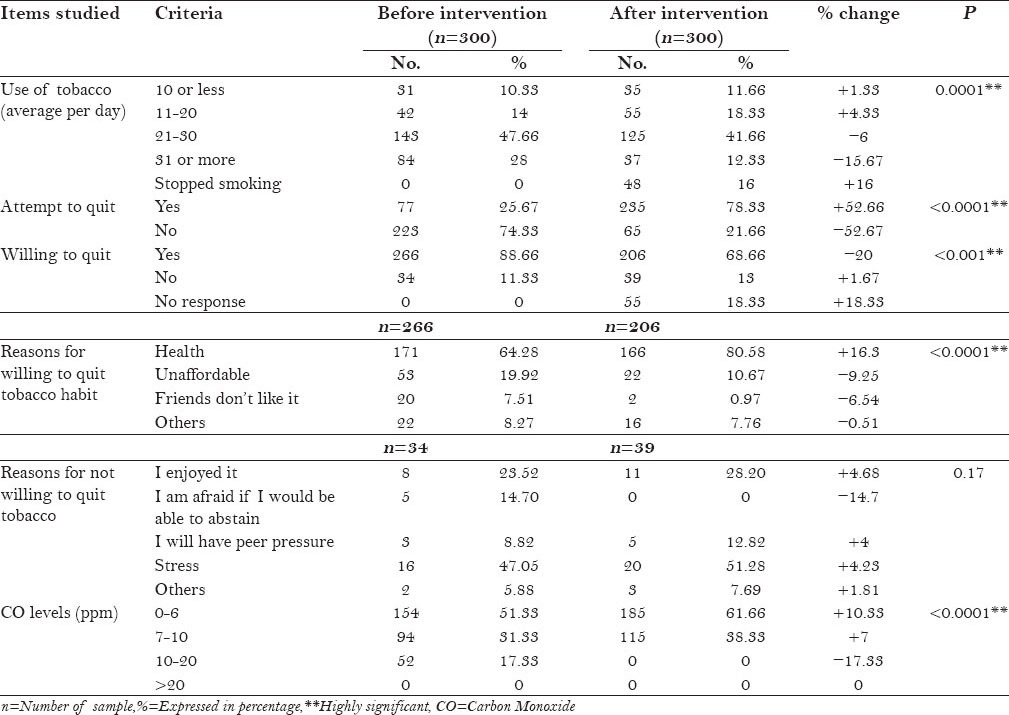
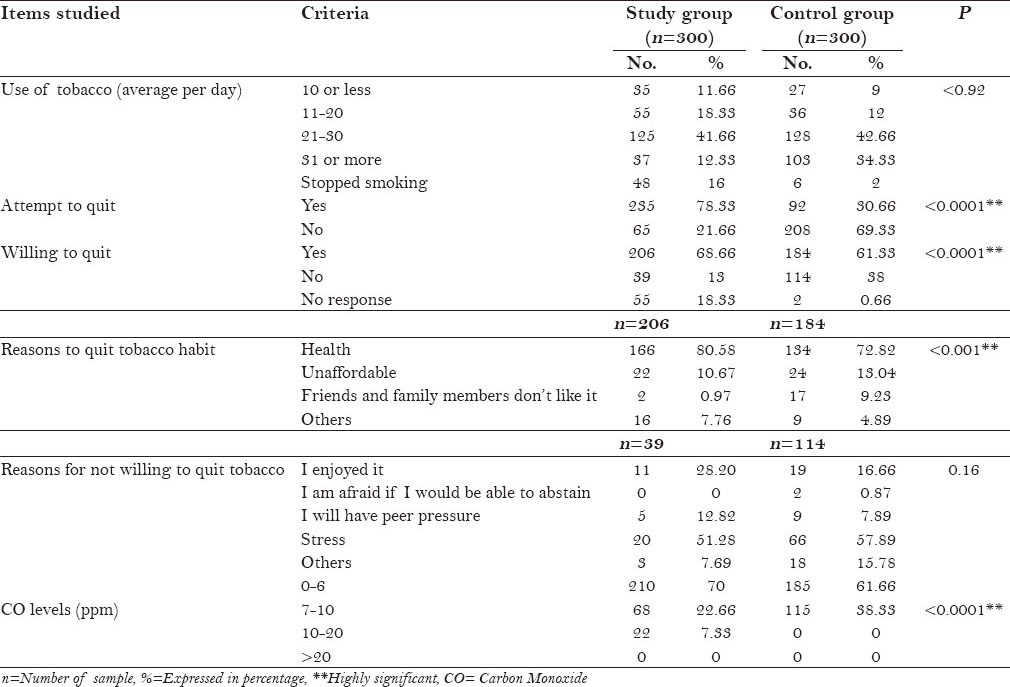
The intervention of tobacco cessation showed a positive percentage change of +16% in the study group, who stopped using tobacco completely after intervention [Table 3]. Regarding the effect on physical and psychosocial problems faced by the prisoners, a positive percentage change of +5.81% was noticed in prisoners having lack of sense of well-being. The other factors like headache (−2.93%) and irritability (−2.42%) showed a negative percentage change after intervention. The main reasons given by the prisoners who did not want to quit tobacco usage before intervention in the study group were: for enjoyment by 23.52% prisoners, 14.70% were afraid of being unable to abstain, peer pressure by 8.82% prisoners, and other reasons like stress by 47.05% prisoners. After intervention, the reasons given were: for enjoyment by 28.20% prisoners, peer pressure by 12.82% prisoners, and other reasons like stress by 51.28% prisoners. Majority (44.66%) of the prisoners had CO level between 0 and 6 ppm, 40% prisoners had a level between 7 and 10 ppm, and 15.33% prisoners had a level between 10 and 20 ppm before intervention. The percentage increased to 70% prisoners with CO level of 0–6 ppm, and a decrease of −17.34% was observed in prisoners with CO level 7–10 ppm and −8% in those with CO level 10–20 ppm after intervention. The CO levels were significant after intervention, with P < 0.001.
Table 3.
Distribution of study population according to tobacco usage after 6 months in the study group and control group
DISCUSSION
Tobacco use is a major risk factor for cancer of the oral cavity, periodontal disease, and tooth loss. Based on 12 studies that have estimated oral cancer risk in smokers compared with non-tobacco users, the pooled risk estimate is 3.43 times higher in smokers.[5] The community of prisoners differs from other social groups in terms of psychosocial factors, their level of education, alcohol and substance abuse, attitude toward health, and lifestyle. All these factors account for the higher prevalence of tobacco usage among prisoners, in comparison with the general population.[6] A smoke-free environment may increase the willingness of smokers to consider quitting smoking and also reduces the risk of fires. However, the principal benefit of smokeless environment in prison is the reduction in second-hand smoke.[7] This study is the first of its kind in which MI method was used for smoking cessation. MI is a particular way of helping clients recognize and do something about their current or potential problems. The strategies of MI are more persuasive than coercive, more supportive than argumentative, and the overall goal is to increase the client's intrinsic motivation so that change arises from within rather than being imposed from others.[8] Psychological studies indicate that smokers who successfully quit smoking were more frequently controlled by their intrinsic rather than extrinsic motives (e.g. the will to receive a reward).[9] Smoking cessation strategies, using pharmacotherapies (e.g. buprion or nortriptyline), nicotine replacement therapies, and counseling intervention based on cognitive intervention are readily accessible in the community. However, these are rarely available to prisoners.[10] Nicotine replacement gum was not allowed in prison because it could be used to block locks or form the key impressions. Using nicotine transdermal patch was not economically feasible. In the present study, prevalence of smoking was 92.60% among the convicted prisoners. According to a study conducted by the National Institute of Mental Health and Neuro Sciences (NIMHANS), 67.3% of the prison population (undertrial prisoners and convicted prisoners) reported ever using tobacco in some form in their lives. This was more than double the prevalence of tobacco use in Karnataka (29.6%, figure for 2001).[11] A recent study conducted by Narkauskaite et al. in Lithuanian prisons revealed a smoking prevalence of 85.3% among the prisoners. It was estimated that around 64–88% of the prisoners smoke (Tielking, Becker, and Stöver 2003; Department of Health and Prison Service 2007; Narkauskaite et al. 2007). Prevalence rates of smoking in prison are at least double or even triple compared to the general population. Prisons are unique settings with high rates of both smoking prevalence and individuals who have smoking-related health problems. These individuals also are unlikely to access community-based smoking cessation treatment; therefore; prison can serve as a unique point of contact for conducting smoking cessation intervention for these individuals.[12] In the present study, 90.66% subjects in the case group and 84.66% in the control group consider “prison stress” as the factor that increases the need for tobacco usage. Similar findings (77%) were reported by Sieminska et al. in 2006. According to the study conducted by NIMHANS, undertrial prisoners are significantly more likely to have smoked or chewed tobacco, compared to convicted prisoners.[11] The reason could be the stress of judgment in undertrial prisoners. In the present study, negative percentage of change (−15.67) was obtained in the study group prisoners who were using 31 cigarettes smoked per day. The physical and psychological problems faced while attempting to quit were reduced in the case group and increased in the control group after intervention. This might be because the case group subjects knew how to tackle with these problems. In the present study, only 19% in the study group stopped smoking during the third month and 16% at the end of the sixth month and only 0.66% stopped smoking in the control group. In a similar study conducted by Harcouet et al., prisoners were given motivational counseling to reduce tobacco use, along with nicotine transdermal patch.[13] In a study done by Cropsy et al. cognitive–behavioral intervention along with pharmacological intervention was given to female prisoners. This study was conducted in southeastern United States and showed a prevalence of 14% at the end of 6-month follow-up.[3] At the end of the sixth month follow-up, 21.66% had reduced the use of tobacco and 45.33% ended up in relapse in the study group. A review by Hughes and Carpenter indicated that smokers who significantly reduce their smoking can maintain these reductions for long periods. Another review found that a reduction in tobacco intake did not undermine cessation.[10] The high rate of relapses during smoking cessation, mainly within 6 months, is common both in correctional and general populations. The study conducted by Sieminska et al. showed 67% relapse in prisoners who attempted to quit. Boredom and stress were mentioned as the main factors for relapse in quitting attempts. Prison inmates are able to quit or reduce tobacco consumption while in prison, but any smoking cessation intervention in this setting needs to address prison-specific issues such as boredom, stress, court appearance, and isolation from family and friends. It appears that quitting while incarcerated has no adverse effects on either the physical or mental health of an individual inmate. Age and a history of illicit drug use seemed to influence the success of inmates participating in our smoking cessation treatment.[10] Limitations of the study were as follows. First, we enrolled only adult male prisoners and we do not know how these results would apply to female prisoners or to juvenile offenders. As prison is a unique environment of long-term confinement, there is high possibility of relapse. Pharmacological intervention along with MI will be more effective than pharmacological intervention only.[3] Dissemination of information among prisoners of study and control groups was unavoidable.
CONCLUSION
Findings of the present study suggest that the intervention has suggestive significance on tobacco usage. The reason of their attempt was apprehension toward health. Tobacco use was high among the prisoners. Prison represents an important but a neglected venue to address smoking cessation. Tobacco reduction is possible in prison even if the living conditions are not favorable. This study indicates that smoking cessation interventions among male prison populations are feasible, acceptable, and effective, compared with similar interventions delivered in the general population.
Recommendations
Relatively high rate of relapse in our study indicates that some policies should be adopted to improve smokers’ information on consequences of tobacco for health and motivational intervention should be added to prisoners.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hartwig C, Stöver H, Weilandt C. Report on tobacco smoking in prison. Directorate – General for Health and Consumers. Drug Policy and Harm Reduction. 2008:1–36. [Google Scholar]
- 2.Butler T, Richmond R, Belcher J, Wilhelm K, Wodak A. Should smoking be banned in prisons? Tob Control. 2007;16:291–3. doi: 10.1136/tc.2007.021600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cropsey K, Eldridge G, Weaver M, Villalobos G, Stitzer M, Best A. Smoking cessation intervention for female prisoners: Addressing an urgent public health need. Am J Public Health. 2008;98:1894–901. doi: 10.2105/AJPH.2007.128207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubak S. Motivational interviewing: A systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–12. [PMC free article] [PubMed] [Google Scholar]
- 5.Ramseier CA, Warnakulasuriya S, Needleman IG, Gallagher JE, Lahtinen A, Ainamo A, et al. Consensus report: 2nd European workshop on tobacco use prevention and cessation for oral health professionals. Int Dent J. 2010;60:3–6. [PubMed] [Google Scholar]
- 6.Cropsey KL, Kristeller JL. The effects of a prison smoking ban on smoking behavior and withdrawal symptoms. Addict Behav. 2005;30:589–94. doi: 10.1016/j.addbeh.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Action on smoking and health fact sheets. Smoke free Prisons. [Last accessed on 2010 Jan 25]. Available from: http://www.ash.org.uk .
- 8.Rosenthal AC. Atlanta, Georgia: 2006. National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, U.S. department of health and human services, Centers for disease control and prevention; pp. 1–127. [Google Scholar]
- 9.Curry SJ, Wagner EH, Grothaus LC. Evaluation of intrinsic and extrinsic motivation interventions with a self-help smoking cessation program. J Consult Clin Psychol. 1991;59:318–24. doi: 10.1037//0022-006x.59.2.318. [DOI] [PubMed] [Google Scholar]
- 10.Soria R, Legido A, Escolano C, López Yeste A, Montoya J. A randomised controlled trial of motivational interviewing for smoking cessation. Br J Gen Pract. 2006;56:768–74. [PMC free article] [PubMed] [Google Scholar]
- 11.Math SB. National Institute of Mental Health and Neuro Sciences, Mental health and substance use problems in prisons: The Bangalore prison mental health study; local lessons for national Action. Executive summary. 2011:1–20. [Google Scholar]
- 12.Cropsey KL, Kristeller JL. Motivational factors related to quitting smoking among prisoners during a smoking ban. Addict Behav. 2003;28:1081–93. doi: 10.1016/s0306-4603(02)00230-7. [DOI] [PubMed] [Google Scholar]
- 13.Harcouët L, Balanger S, Meunier N, Mourgues A, Grabar S, Haouili B, et al. Tobacco reduction in a prison of France. Rev Med Interne. 2008;29:357–63. doi: 10.1016/j.revmed.2007.10.008. [DOI] [PubMed] [Google Scholar]


