Abstract
Introduction:
Yoga used as a major component of integrative treatment protocol in 14 Indian village camps improved quality-of-life in 425 lymphatic filariasis patients. They experienced better mobility and reduced disability. This paper documents the gait abnormalities observed in lower limb lymphedema patients and the locomotor changes following integrative treatment.
Materials and Methods:
Yoga postures were performed as explained by traditional yoga practice in two sessions: Before ayurvedic oil massage without compression bandages and after the massage with compression bandages. Each yoga posture lasted for 5 min and the whole session ended in 45 min. Throughout each session, we advised patients to do long, diaphragmatic breathing, concentrating on each breath. The flexion of joints was coordinated with exhalation and extension with inhalation. We educated the patients to do longer expiration than inspiration.
Results and Discussion:
A total of 98 patients (133 limbs) attending the 6th month follow-up were evaluated. The most common gait abnormality was antalgic gait. Structural and functional abnormalities were observed in hip, knee and ankle joints. We found that yoga as an adjunct to other components in integrative treatment improved the gait problems. Long standing lymphedema caused altered gait and joint deformities. This was mostly due to inactivity causing muscle weakness and edema within and around the muscles. Both large and small limbs have shown significant volume reduction (P < 0.01) during follow-up after 6 months.
Conclusion:
There can be a mixed etiology for gait related problems in lymphedema patients. Further studies are recommended to understand the causes of deformities in lymphedema patients and an exact role of yoga.
Keywords: Gait, integrative medicine, lower limb lymphedema, muscle weakness, range of motion, yoga
INTRODUCTION
Lymphatic filariasis (LF) has a negative impact on quality-of-life (QoL) due to its disability causing restriction in duration and capacity to work and changes of activity patterns. [1] Narahari et al. [2] developed a treatment protocol for lymphedema integrating ayurveda, biomedicine and yoga. In their protocol, breathing exercises in yoga helped to replace manual central lymph drainage, whereas the yoga postures (asanas) facilitated peripheral lymph drainage. The treatment protocol was found beneficial as it reduced disability in LF patients. Yoga used as a major component of modified integrative treatment protocol in 14 village camps improved QoL in 425 LF patients by reducing their disability. [3] Yoga was used in musculoskeletal disorders [4] to improve the postural control and mobility. [5] This paper discusses the benefits of yoga postures in improving locomotion among lymphedema patients as an adjunct to lymphatic clearance.
MATERIALS AND METHODS
We documented the locomotor changes in lower limb lymphedema of patients receiving integrative treatment in the out-patient department of the Institute of Applied Dermatology (IAD). Changes were studied in patients attending the 6th month follow-up during the period 2009-2012.
Patients with lower limb lymphedema (grade two late or three), of any age and gender, with one or both limbs affected, were selected. Those patients, who agreed to long-term treatment and had a family member for assistance, were enrolled. Patients signed written consent forms. Patients currently having or recently (within the month previous to patient selection) experienced an acute inflammatory episode (cellulitis/filarial fever) were treated with appropriate antibiotics initially to control cellulitis and then recruited for integrative treatment.
The steps of integrative treatment includes, skin wash, phanta soaking, bacterial entry point (BEP) care using modern dermatology drugs, Indian manual lymph drainage (IMLD), pre and post IMLD yoga postures, compression bandaging. [6] Detailed counseling sessions were given to patients and their family members during admission to treatment; discharge from treatment and during every follow-up, primarily to ascertain whether treatment instructions were being followed as advised. Counseling emphasized the care of BEP, self-care and the need for the life-long practice of treatment. The protocol was the same as described by Narahari et al. [6] All patients received the initial 2 weeks of supervised treatment as outpatients. In addition to treatment, patients were trained to continue all procedures as self-care and family member assisted program. A yoga information booklet in local languages was provided. Patients were followed-up 1 month, 3 months and 6th months, after the initial 2 weeks of supervised day care. [2]
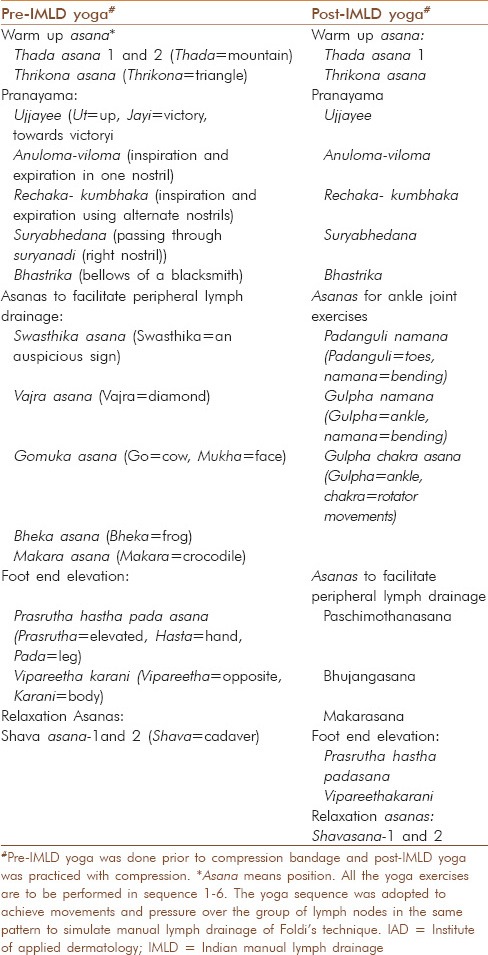
Yoga postures were performed as explained in the traditional yoga practice written by Swami Vivekananda. [7] A yoga therapist coached lymphedema patients on performing yoga. The postures incorporated in our yoga protocol are explained in Table 1.
Table 1.
The current yoga sequence for lower limb lymphedema patients at IAD
There are two positions for yoga postures; samasthithi, the starting position and sthithi, final position. Lymphedema patients moved from samasthithi to sthithi slowly with breathing coordination and vice versa. Patients remained in final position for 10-15 breaths depending on the yoga posture (e.g. 10 breathings for vajra asana). The initial position in standing yoga postures was, standing erect with feet parallel to each other and touching medially, placing the hands facing downwards with stretched fingers. In sitting postures, patient sat with both legs stretched forward and heels together, placing the palms on the floor by the side of the buttocks. The spine, neck and head were in the same line. The initial position for lying posture was supine, touching the chin to the chest. We educated patients to look straight ahead or to keep their eyes closed. The final position was dependent on the yoga posture. In Thada asana 1 final position was stretching of arms up and over the head and clasping the fingers while standing on toes.
We used 3 common positions of fingers and hands (Replica or symbol [Mudra] during the yoga postures; Chinmudra [symbol of good], Mrugi Mudra [symbol of animal] and Namaskara mudra [symbol of salutation]). Chinmudra was performed by keeping thumb and index finger flexed and joined together while other fingers were straight. Both the palms rested on the folded knee facing upwards in either Padma asana or Swastika asana. Mrugi Mudra was used to close nostrils for selective inhalation or exhalation during pranayama. Here, the right forefinger and middle finger are clenched, while the thumb and other two fingers are straight. Namaskara mudra was performed in Thada asana by keeping both the palms and fingers touching one another.
Each yoga asana (posture) took around 5 min to attain samasthithi to sthithi and vice versa. The entire session was completed in 45 min. Patients performed two such sessions per day. Pre-IMLD session was done in the morning and post IMLD - session during the evening. We advised the patients to do long, diaphragmatic breathing concentrating on breathing. The flexion of joints was coordinated with exhalation and extension with inhalation. We educated patients to do longer expiration than inspiration. All the patients were asked to continue the treatment procedures back home after discharge along with walking and climbing the stairs.
We avoided the yoga postures such as Bheka asana, Bhujanga asana, Vipareetha karani in patients with cardiac ailments and vajra asana in those with history of the femur or tibial fracture or those suffering from the knee joint arthritis.
Outcome measures
The gait pattern changes were observed before and after treatment. This was assessed through video recordings of patient's gait pattern. Muscle weakness was assessed clinically
The QoL of patients, assessed through LF specific QoL questionnaire (LFSQQ) [3] at admission and after completion of 6 months. All the questions were not answered by every patient. Questions that were not applicable were not answered, e.g. a house wife from urban locality didn’t attempt to answer questions on agrarian work. Therefore, percentage analysis was done based on the questions answered by each patient
Admission and follow-up volume measurement by water displacement method and girth measurements taken at eight points along the limb: Metatarsal; midfoot; ankle; end of calf; maximum calf bulk; patellar region; mid-thigh; and maximum bulk on standing.
Data analysis
The data were analyzed through SPSS 16 (SPSS Inc., Chicago, IL, USA). It classified the limbs as small or large, based on two-step cluster analysis. This is an automatic analysis when the data available are sufficiently large. The two-step cluster analysis procedure is an exploratory tool designed to reveal natural groupings (or clusters) within a dataset that would otherwise not be apparent. Displacement of 8.7 L of water was the dividing point between large and small limbs; a limb which displaced more than 8.7 L was considered a large limb. There were two kinds of assumptions while analyzing the results. The limb data were used for assessing volume changes and patient data for QoL changes. A paired t-test was used for comparison of limb volume changes and for assessing the significance of changes in QoL. Pearson correlation was used to identify association between age and LFSQQ domain changes. Disease duration is a categorical variable; hence we used Spearman's rank correlation coefficient instead of Karl-Pearson correlation coefficient to find out the association with LFSQQ domain changes. Cohen's d was used to identify the standardized difference between LFSQQ domain changes before and after 6 months and in unilateral and bilaterally affected patients. Cohen's d is the difference between two means divided by a standard deviation for the data. Outcome data were stored in Microsoft Access database. Ethical clearance was obtained from Institutional Ethics Committee of IAD.
RESULTS
Totally 98 patients (133 limbs) who attended 6th month follow up at IAD were evaluated. Results following two-step cluster analysis performed by SPSS version 16 (SPSS Inc., Chicago, IL, USA) revealed 93 (69.9%) limbs as small and 40 (30.1%) limbs as large. Table 2 shows the percentage volume reduction during follow ups. In small limbs, reduction was from 5.5 to 4.4 L; whereas large limbs had 12.6 L at baseline and reduced to 6.8 L in 6 months duration. Both limbs had shown significant volume difference (P < 0.01) during the follow-up [Figure 1].
Table 2.
Reduction in volume in large and small limbs at different follow-ups
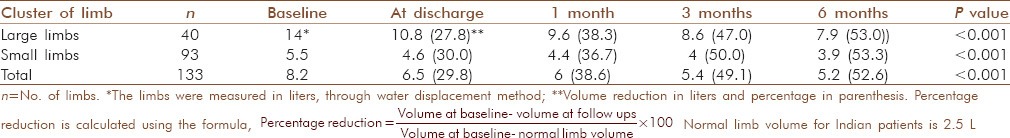
Figure 1.

The volume reduction observed after 14 days of integrative treatment. The outer rotation of hip observed at baseline was corrected after treatment
Mobility changes using LFSQQ
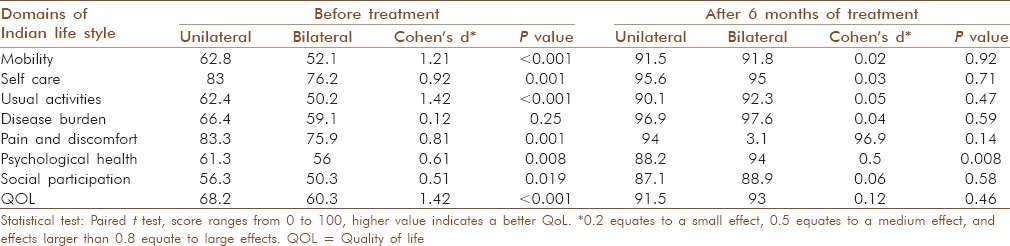
Table 3 shows differences in mean scores for LFSQQ domains at admission and at the 6th month follow-up. All the domains showed significant changes after 6 months of treatment. There was a weak correlation between age of the patients and disease duration with changes in LFSQQ domains [Table 3]. The changes in LFSQQ domains with unilateral and bilateral limbs were calculated. At baseline, patients with bilateral limbs showed poorer LFSQQ domain values in all domains except disease burden. After 6 months of treatment, there were no differences in LFSQQ domains except in psychological health [Table 4].
Table 3.
Changes in LFSQQ domains before and after 6 months of treatment and correlation with age and disease duration in 98 lymphedema patients
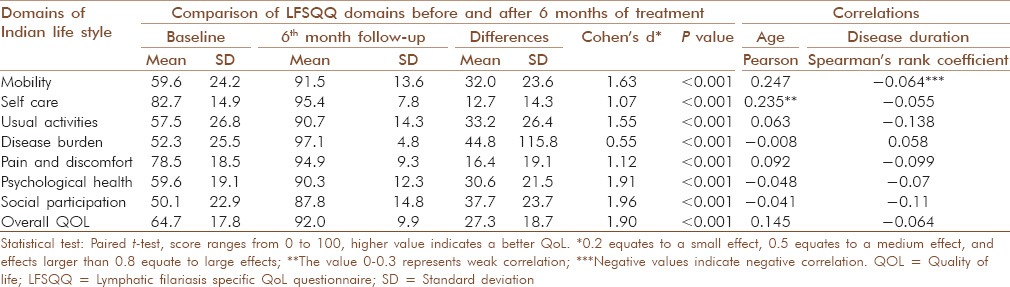
Table 4.
Comparison of LFSQQ domains before and after 6 months of treatment in patients with unilateral and bilateral limbs
Gait abnormalities observed in lymphedema patients
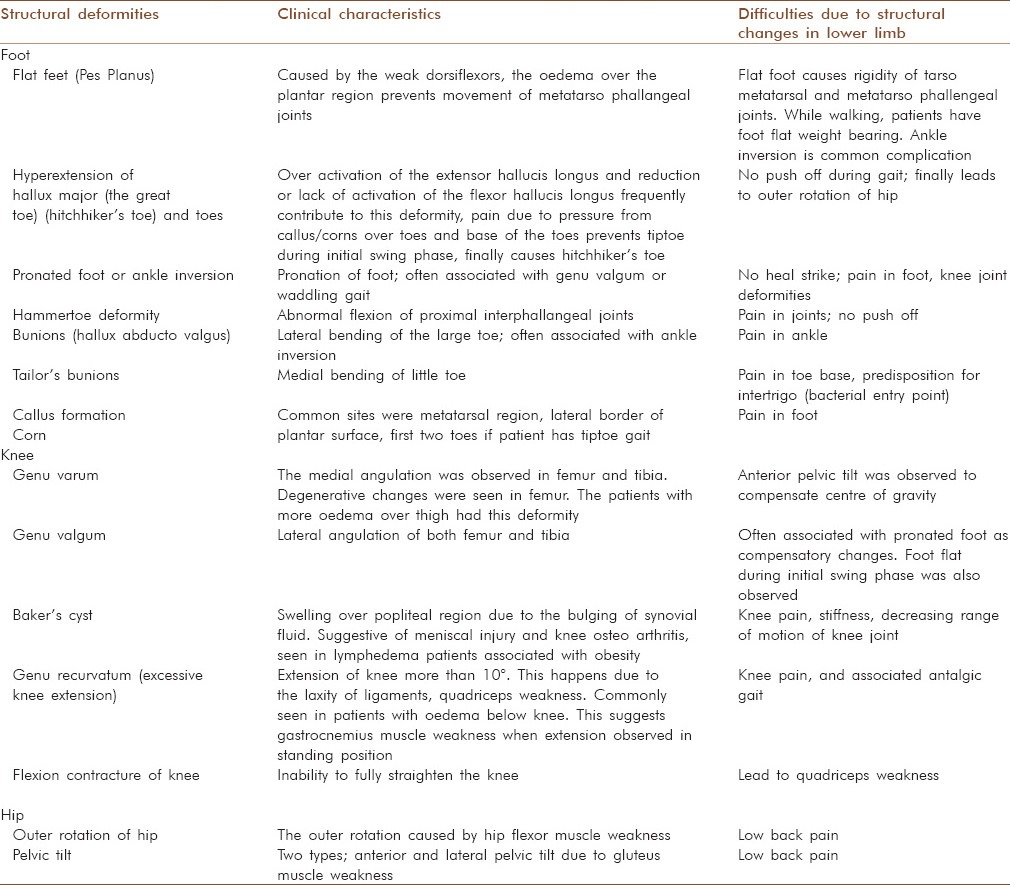
The common gait abnormality was antalgic gait. The unequal size of the limb in unilaterally affected patients or difference in grading and severity in bilaterally affected patients resulted in antalgic gait. Patients usually had shortened swing phase of the uninvolved/less involved side, which resulted in degenerative changes in knee. Patients with degenerative changes in knee had impaired joint movements. Stiff-knee gait was common in patients with excessive knee contracture. The patients with edematous swelling in the thigh region showed a specific pattern which mimics scissors gait. Such patients had excessive adduction of the leg in swing, plantar flexion of the ankle and outer rotation of the hip. This method was to compensate for the center of gravity while walking. However, there was no neurological involvement, the patients did not have muscle spasticity and arm swing was not altered. Some patients showed lurch gait, suggesting weak gluteus maximus. The affected side begins to contract at the moment of heel-strike, slowing forward motion of the trunk by arresting flexion of hip and initiating extension; the trunk lurches backward at heel-strike on weakened side to interrupt the forward motion of the trunk. The LF patients also showed Trendelenberg gait pattern (unilateral trunk bending) due to weak gluteus medius. This gait allows the opposite side of pelvis to tilt downward during stance on the weak side. Both compensated and uncompensated gluteus medius weakness were observed in our patients. Lymphedema patients who were obese with more edema over thigh had waddling gait, sometimes coexisting with flat foot, genu valgum. This pattern suggests weak adductors of lower limb. Increased edema also had a major role. The functional limb length inequality was observed in seven patients with edema over plantar surface of foot, flexion contracture of the knee. The common structural and functional abnormalities due to the improper gait are explained in Table 5. These abnormalities occur in hip, knee and foot. These abnormalities further impaired the gait pattern.
Table 5.
Structural changes in lymphedematous legs due to improper gait patterns
The patients with uncompensated pelvic tilt, impaired shoulder and anterio-superior ileac spine alignment showed improvement after 14 days of treatment in Trendelenberg gait pattern. The initial reduction of limb volume corrected the postural dysfunction during the initial 2 weeks in patients with waddling and lurch gait patterns. Patients reported a reduction in knee pain in 2 weeks. They also reported reduced frequency of analgesics consumption. The patients were able to climb stairs without difficulty after 6 months of treatment [Figure 2]. There were no changes in structural abnormalities of toe, but we observed increased range of motion in tarso-metatarsal and metatarso-phallengeal joints.
Figure 2.

Changes in Trendelenberg gait pattern (Unilateral trunk bending). Upper raw before treatment. Lower raw shows changes after 5 months of treatment
DISCUSSION
Both large and small limbs have shown significant volume reduction (P < 0.01) during the follow-up after 6 months [Table 2]. Irrespective of the age of the patient and the duration of the disease overall QoL, assessed through LFSQQ, showed significant changes (P < 0.01) with a mean difference of 27.3 after 6 months of the treatment [Table 3]. The result shows that patients’ mobility had the highest impact on QoL at baseline and this was reversed (P < 0.01). The changes in LFSQQ domains with unilateral and bilateral limbs were assessed [Table 4]. Although unilaterally affected patients had better mean scores at baseline, after 6 months of treatment, there were no differences in LFSQQ domains except the psychological health. The impact of the disease is the same in both groups but bilaterally affected patients had more difficulty to do physical activities than unilateral limbs. The age and disease duration did not have any impact on the QoL of the patients [Table 3].
The treatment was designed as an integrative module by combining the skin care therapies of Ayurveda, coordinated and slow movements of yoga and dermatology drugs to treat BEP. The pathophysiological basis was according to the principles of lymphology. The consensus statement of the International Society of Lymphology stresses the importance of skin care. [8] Skin care procedures such as washing and the application of emollients restore the barrier function and skin health. IMLD is a skin care procedure administered in Ayurveda, but modified and adopted as described by Narahari et al. [6] The benefits of skin care are mentioned in Ayurveda and in biomedicine. Ayurveda describes that lymphatic channels (srotas) are activated and metabolic activity in the skin are improved with certain procedures. IMLD uses oil, facilitates lymph drainage by correcting the pathophysiology of lymphedema. Compression bandaging was done to achieve the reduction in capillary filtration, increased lymphatic absorption and stimulation of lymphatic transport, improvement in venous pump and breakdown of fibro sclerotic tissue. [9]
Multimodality interventions, just as much as single interventions, have to be supported by the evidence of efficacy. Randomized control trials (RCT) were designed and continued to be used for single intervention drug studies. RCT has limitations when generalizing the outcome to patients belonging to different ethnic backgrounds, severity of the disease and when associated with co-morbidities while comparing with other levels of evidence. [10] RCTs may be inappropriate, where the effects of treatment are large and dramatic. [11] Observational studies tend to provide larger treatment effects than RCTs. Our integrative treatment model did not achieve the level of evidence of a well-conducted RCT design but as before-and-after interventional study, [12] using objective outcome measures in line with Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (The Cochrane Collaboration, 2011) recommendations. [13] Therefore for this pilot study we have chosen an observational study design albeit, RCT will define the exact role of Yoga.
The yoga postures were part of IAD's integrative treatment protocol for lymphedema patients and were employed to achieve lymph drainage. Lymph drainage is normally achieved by, in addition to contraction of lymphatic vessel wall, contraction of skeletal muscles, active and passive body movements, pulsation of arteries adjacent to lymphatics and compression of tissues as in compression therapy. Although there are frequent anatomical variants the commonest are the largest lymph trunk, the thoracic duct which drains the lymph from the lower half of the body, the deep layers of the back and three body quadrants. The right lymphatic duct drains lymph from the right upper quadrant of the body, whereas the thoracic duct drains lymph from the other parts and finally joins with the left subclavian vein. The initial three postures (Thada asana 1, Thada asana 2 and Thrikona asana) allow dermal stretch of the whole body and movements of all joints, thus activating joint pumps and muscle pumps. Later the central lymphatic clearance was achieved by breathing exercises. During inhalation, lymph from thoracic duct and right lymphatic duct is drawn in to the great veins. The flow of lymph is similar to the process of blood flow into the thoracic cage while in artificial respiration when using a “tank respirator.” [14] During the tan respirator experiments, expiration is caused when positive pressure develops around the body, negative pressure causes inspiration. Positive pressure inside the lungs impedes the flow of blood into the chest and heart from peripheral veins. Deep, slow, methodical breathing, as in Ujjayi and rechaka kumbhaka induces intra-thoracic pressure changes also leading to parasympathetic nerve stimulation linked to the vagus which lies mostly on the left of the body. Alternate nostril breathing of Anuloma viloma facilitates the activity of the contra lateral cerebral hemisphere. [15] Breathing (inhalation or exhalation) through the right nostril in suryabhedana stimulates the sympathetic nervous system. [16,17] Controlled diaphragmatic breathing as in Bhastrika, creates pressure differences in both abdomen and thoracic region and allow lymph to drain towards the thorax. The stroke of continued exhalation in Bhasthrika has maximum lymphatic clearance and at the same time forceful movements over the abdomen lead to peripheral drainage.
The rate of lymphatic clearance can be increased by a small amount of ankle movement. [18] Padanguli namana, Gulpha namana and Gulpha chakrasana facilitate maximum ankle movement, thus help to lymph drainage from extremities. Swasthika asana and vajra asana give pressure over inguinal and popliteal nodes, since it allows flexion of the hip and knee joint. There are pressure differences in every yoga posture. In Bheka asana or Bhujanga asana, extension of the spinal column and shoulder joints plays an important role allowing maximum stretch of the anterior part of the body. This exercise stretches the dermis and that has maximum network of lymphatics, allowing flow of lymph and venous blood. Shava asana 1 and 2 were end postures for relaxation. The flexion of joints was coordinated with exhalation and extension with inhalation. During extension of joints with inhalation, lymph from thoracic duct and right lymphatic duct is drawn in to the great veins; whereas flexion with exhalation allows lymph drainage toward chest. We educated patients to do longer expiration than inspiration to maximize lymph flow.
The sequence of yoga asanas were designed to achieve the lymphatic drainage [Table 1]. Manual lymph drainage (MLD) begins from neck and shoulder region, axillary region. The drainage is then directed from the abdomen through the back to the axilla. Then the drainage extends to the inguinal region, lumbar and gluteal region and the lower limb. Yoga sequence is designed in such a way that the pressure of movement of the joints and muscles are exerted on groups of lymph nodes in the sequence required for Foldi's MLD. [19]
The physical disability due to lymphedema (i.e. increased limb volume) has a major role in determining the QoL changes. This was further impaired by deformities executed by improper gait pattern. Normal gait requires adequate strength, ROM of joints and balance. Lymphedema patients show a very characteristic gait deviation that is associated with either compensation or a consequence of a specific impairment. An altered gait pattern reflects lower extremity defects or injury of joint muscles and loss of toe muscle and abnormal balance function. The body adapts certain biomechanical compensations (often subconsciously), which leads to more muscle tension and body rigidity. This rigidity reduces the movement of the abdomen and thoracic region, thus inhibiting respiratory movements. This has an influence on the venous and lymph drainage. Exercises to correct posture have a positive impact on minimizing body rigidity and muscle tone. [20] Earlier studies showed that locomotor disability and functional impairment [21] are common in LF patients. These patients had difficulty to perform yoga initially, but they improved after continuous yoga practice.
Patients with lymphedema are generally inactive due to the discomfort caused by edema, fear of increase in edema when they perform exercises or walk and occasionally due to pain. This inactivity or less joint movements cause minimized muscle action which results in flaccid muscles. Most of the altered gait patterns in lymphedema patients were due to the muscle weakness. The most affected muscles were gluteus, quadriceps femoris, gastrocnemius, soleus and flexor digitorium longus. The structural abnormalities due to the improper gait further hampered the patients’ mobility. The yoga postures in our treatment protocol improved the gait by enabling proper movements. The Thada asana, Thrikona asana, Gomukha asana, Bheka asana, Paschimothana asana and Bhujanga asana provides movements of the spinal column, shoulder, elbow, wrist, hip, knee, ankle, tarso metatarsal and metatarso phallengeal joint. Muscles over the lymph node groups in the region are put into action possible supporting nodal drainage and also strengthens knee. The body posture gets corrected due to the stretching (anterior stretch in Paschimothana asana, posterior in Thada asana 2, Bheka asana, Bhujanga asana, lateral in thrikona asana and upward stretch in Thada asana 1, Gomukha asana). Body balancing on tiptoe during Thada asana 1, corrects the gait pattern and improves flat foot, hyperextension of hallux major (great toe) (Hitchhiker’ Toe) and toes, hammer toe deformity and bunions. The breathing exercises (pranayama) have no direct influence on joint movements. However it increases oxygen consumption of the body. Padanguli namana, Gulpha namana, Gulpha chakrasana has maximum movement of ankle, tarsometatarsal and metatarsophallengeal joints. The major muscles involved are peroneus muscles (longus, brevis, tertius), tibialis anterior, tibialis posterior Gastrocnemius, Soleus and those muscles of the foot which activate smaller joints of the foot, especially flexor digitorium longus (Padanguli namana) and Gastrocnemius, Soleus (Gulpha namana and Gulpha chakrasana). Swasthika asana, vajra asana has maximum movement of hip, knee and ankle joint. These asanas will strengthen weak hip abductors in patients with Trendenlenberg gait, Waddling gait [Figure 2]. Increased abdominal pressure in Bhujanga asana and Bheka asana activates rectus muscles. Gomukha asana and Bheka asana provide hip and knee strengthening and it corrects the outer rotation of hip, anterior and lateral pelvic tilt. Prasrutha hastha padasana, Vipareetha karani provides knee strengthening, improves weak gluteus muscles.
The patients with associated diseases and elderly patients had difficulty in performing the yoga exercises. Patients with bilaterally affected limbs and scrotal lymphedema had difficulty in attaining the final position of yoga, compared to those with unilateral limb lymphedema. This study is an observational study and it has limitations for generalizability. Other limitations of the study were the need for a long duration and intensive engagement with each of the patients and their family members to follow the entire protocol. In the case of elderly patients, those who have no family support and those who are employed had difficulty in continuing the treatment procedure as it is a lifelong treatment.
CONCLUSION
Long standing lymphedema caused altered gait and joint deformities in small and large volume limbs. This was mostly due to the inactivity causing muscle weakness and edema with in and around the muscles. Yoga postures improve movements and helped the patients to negotiate with these deformities. There is a possibility that the lymphedema is not the sole cause of gait problems. In this pilot observational study, Yoga as an adjunct to other components in integrative treatment improved the gait problems. There can be a mixed etiology for gait related problems in lymphedema patients. Further studies are recommended to understand the causes of deformities in lymphedema patients and an exact role of yoga.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ramaiah KD, Radhamani MP, John KR, Evans DB, Guyatt H, Joseph A, et al. The impact of lymphatic filariasis on labour inputs in southern India: Results of a multi-site study. Ann Trop Med Parasitol. 2000;94:353–64. doi: 10.1080/00034983.2000.11813550. [DOI] [PubMed] [Google Scholar]
- 2.Narahari SR, Ryan TJ, Mahadevan PE, Bose KS, Prasanna KS. Integrated management of filarial lymphedema for rural communities. Lymphology. 2007;40:3–13. [PubMed] [Google Scholar]
- 3.Aggithaya MG, Narahari SR, Vayalil S, Shefuvan M, Jacob NK, Sushma KV. Self care integrative treatment demonstrated in a rural community setting improves health related quality of life of lymphatic filariasis patients in endemic villages. Acta Trop. 2013;126:198–204. doi: 10.1016/j.actatropica.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 4.Büssing A, Michalsen A, Khalsa SB, Telles S, Sherman KJ. Effects of yoga on mental and physical health: A short summary of reviews. Evid Based Complement Alternat Med. 2012;2012:165410. doi: 10.1155/2012/165410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zettergren KK, Lubeski JM, Viverito JM. Effects of a yoga program on postural control, mobility, and gait speed in community-living older adults: A pilot study. J Geriatr Phys Ther. 2011;34:88–94. doi: 10.1519/JPT.0b013e31820aab53. [DOI] [PubMed] [Google Scholar]
- 6.Narahari SR, Ryan TJ, Bose KS, Prasanna KS, Aggithaya GM. Integrating modern dermatology and Ayurveda in the treatment of vitiligo and lymphedema in India. Int J Dermatol. 2011;50:310–34. doi: 10.1111/j.1365-4632.2010.04744.x. [DOI] [PubMed] [Google Scholar]
- 7.Swami V. Complete Illustrated Book of Yoga. New York, NY: Crown Publishers; 1988. [Google Scholar]
- 8.International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema.2009 Concensus Document of the International Society of Lymphology. Lymphology. 2009;42:51–60. [PubMed] [Google Scholar]
- 9.Moffatt C. Compression Therapy in Practice. Trowbridge: Wounds UK; 2007. [Google Scholar]
- 10.Rawlins MD. De Testimonio on the Evidence for Decisions about the Use of Therapeutic Interventions. London: Royal College of Physicians; 2008. [DOI] [PubMed] [Google Scholar]
- 11.Nahin RL, Straus SE. Research into complementary and alternative medicine: Problems and potential. BMJ. 2001;322:161–4. doi: 10.1136/bmj.322.7279.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Narahari SR, Bose KS, Aggithaya MG, Swamy GK, Ryan TJ, Unnikrishnan B, et al. Community level morbidity control of lymphoedema using self care and integrative treatment in two lymphatic filariasis endemic districts of South India: A non randomized interventional study. Trans R Soc Trop Med Hyg. 2013;107:566–77. doi: 10.1093/trstmh/trt054. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] The Cochrane Collaboration. 2011 [Google Scholar]
- 14.Hall JE. Guyton and Hall Textbook of Medical Physiology. Philadelphia: Elsevier Saunders; 2011. [Google Scholar]
- 15.Telles S, Joshi M, Somvanshi P. Yoga breathing through a particular nostril is associated with contralateral event-related potential changes. Int J Yoga. 2012;5:102–7. doi: 10.4103/0973-6131.98220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaqas B, Ryan TJ. Lymphoedema: Pathophysiology and management in resource-poor settings-relevance for lymphatic filariasis control programmes. Filaria J. 2003;2:4. doi: 10.1186/1475-2883-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 18.Mortimer PS, Simmonds R, Rezvani M, Robbins M, Hopewell JW, Ryan TJ. The measurement of skin lymph flow by isotope clearance - Reliability, reproducibility, injection dynamics, and the effect of massage. J Invest Dermatol. 1990;95:677–82. doi: 10.1111/1523-1747.ep12514347. [DOI] [PubMed] [Google Scholar]
- 19.Foldi M, Foldi E, Kubic S. Textbook of Lymphology. Munich: Elsevier; 2007. [Google Scholar]
- 20.Schrale G, Ryan TJ. Managing oedema and fibrosis with coordinated movement. J Lymphoedema. 2011;6:82–6. [Google Scholar]
- 21.Ramaiah KD, Kumar KN, Ramu K, Pani SP, Das PK. Functional impairment caused by lymphatic filariasis in rural areas of south India. Trop Med Int Health. 1997;2:832–8. doi: 10.1046/j.1365-3156.1997.d01-406.x. [DOI] [PubMed] [Google Scholar]


