Abstract
Background:
Lung functions are found to be impaired in coronary artery disease (CAD), congestive heart failure, left ventricular dysfunction, and after cardiac surgery. Diffusion capacity progressively worsens as the severity of CAD increases due to reduction in lung tissue participating in gas exchange.
Aims and Objectives:
Pranayama breathing exercises and yogic postures may play an impressive role in improving cardio-respiratory efficiency and facilitating gas diffusion at the alveolo-capillary membrane. This study was done to see the effect of yoga regimen on lung functions particularly diffusion capacity in CAD patients.
Materials and Methods:
A total of 80 stable CAD patients below 65 years of age of both sexes were selected and randomized into two groups of 40 each. Group I CAD patients were given yoga regimen for 3 months which consisted of yogic postures, pranayama breathing exercises, dietary modification, and holistic teaching along with their conventional medicine while Group II CAD patients were put only on conventional medicine. Lung functions including diffusion capacity were recorded thrice in both the groups: 0 day as baseline, 22nd day and on 90th day by using computerized MS medisoft Cardio-respiratory Instrument, HYP’AIR Compact model of cardio-respiratory testing machine was manufactured by P K Morgan, India. The recorded parameters were statistically analyzed by repeated measures ANOVA followed by Tukey's test in both the groups. Cardiovascular parameters were also compared before and after intervention in both the groups.
Results:
Statistically significant improvements were seen in slow vital capacity, forced vital capacity, peak expiratory flow rate, maximum voluntary ventilation, and diffusion factor/ transfer factor of lung for carbon monoxide after 3 months of yoga regimen in Group I. Forced expiratory volume in 1st sec (FEV1), and FEV1 % also showed a trend toward improvement although not statistically significant. HR, SBP and DBP also showed significant improvement in Group-I patients who followed yoga regimen.
Conclusions:
Yoga regimen was found to improve lung functions and diffusion capacity in CAD patients besides improving cardiovascular functions. Thus, it can be used as a complimentary or adjunct therapy along with the conventional medicine for their treatment and rehabilitation.
Keywords: Coronary artery disease, pulmonary function tests, pranayama, yoga regimen
INTRODUCTION
Coronary artery disease (CAD) is defined as impairment of heart function due to inadequate blood flow to the heart against its demand, caused by obstructive changes in the coronary circulation to the heart. Prevalence of CAD is greatly increasing in our country for the last several years and is expected to assume epidemic proportions soon. CAD causes more deaths and disabilities, and incurs greater economic costs than any other illness in the developed as well as developing countries. Projections based on the Global Burden of Disease Study estimate that by the year 2020, the burden of athero-thrombotic cardiovascular disease in India would surpass that in any other region in the world. [1] Studies in India have documented a five-fold higher prevalence of coronary heart disease in the urban as compared to the rural population. [2] Over the last three decades, progress in coronary artery bypass grafting and percutaneous interventions has improved the prognosis of CAD, but has not been able to address the basic etiopathology of CAD. [3,4] These are merely providing palliative relief at a high cost.
The lungs are linked in series with the cardiac pump, and they are not only influenced by mechanical alterations in pump function but also by neuro-humoral modulators and cytokines involved in the pathogenesis of various heart diseases. [5,6] It has also been proposed that increased levels of circulating cytokines such as tumor necrosis factor-α and interleukin-6 in CAD patients may induce changes in lung parenchyma. [7] High left atrial pressure may also induce chronic remodeling of the pulmonary vasculature and its wall thickening. There may also be an enhanced degree of airway reactivity. [8] Elevation of the capillary pressure causes alveolar-capillary membrane stress failure (i.e., increase in capillary permeability to water and ions, and disruption of local regulatory mechanisms for gas exchange), leading to a decrease in membrane conductance, an increase in capillary blood volume and subsequent impairment of diffusion capacity. [9,10] Diffusion factor of the lung for carbon monoxide (DLCO) may give an early indication of alveolar-capillary membrane dysfunction in CAD patients as data is lacking in stable patients of CAD.
There is a growing incidence of anxiety and stress related diseases like CAD for which conventional medicine offers only relief from symptom, not from the disease. The new millennium has heralded an unprecedented increase in such disorders and appropriate preventive and remedial measures are needed to be taken. Yogic exercises and pranayama may improve breathing patterns due to which respiratory bronchioles may be widened and perfusion of a large number of alveoli can be carried out efficiently. Yogic regimen may change the milieu at the bronchioles and the alveoli particularly at the alveolar-capillary membrane to facilitate diffusion and transport. Studies done by several researchers showed that yogic lifestyle intervention decreases the stenosis of coronary artery, decreases the anginal episodes, retards atherosclerosis, decreases sympathetic activity and improves exercise tolerance. [11,12,13,14,15,16] Adiponectin, interleukin-6, and various other cardiovascular disease risk makers are also found to be modified by a short-term yoga-based lifestyle intervention in obese people. [17] We have not come across any study showing the effect of a comprehensive yoga regimen on lung diffusion capacity in CAD patients to the best of our knowledge. Reports are available on improvement in lung functions and DLCO after yogic lifestyle intervention in asthma and chronic obstructive pulmonary disease (COPD) patients. [18,19]
As very few studies are available on the effect of yoga practices on lung functions and none on diffusion capacity in stable CAD patients, it is therefore, endeavored to study the effect of yogic regimen and lifestyle modification on lung diffusion capacity and other lung functions in patients with stable CAD.
MATERIALS AND METHODS
A total of 80 patients with stable CAD of age group 45-65 years (55.78 ± 8.95) were recruited from the Outpatient Department of Medicine, Guru Teg Bahadur Hospital, Delhi. All the patients were on regular conventional drug therapy. Most of them were on angiotensin-converting enzyme inhibitors of calcium channel blockers along with aspirin. The subjects were selected on the basis of certain inclusion and exclusion criteria.
Inclusion criteria
Angiographically proven CAD
Stable CAD for the last 2-6 years
Middle socioeconomic class.
Exclusion criteria
History of any previous illness such as stroke, unstable angina, myocardial infarction, tuberculosis, diabetes mellitus, and renal disease
Any disease known to affect lung function as well as the course of CAD such as asthma and COPD
Any history of smoking as it is a confounding factor.
Design
This was a prospective randomized parallel group controlled study on patients with CAD, conducted in the cardio-respiratory lab of the Department of Physiology, University College of Medical Sciences (UCMS), Delhi. The ethical clearance from the Ethical Committee of the institution was obtained before starting the study. All the subjects underwent complete physical and clinical assessment as given in the performa. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean blood pressure (MBP) were also recorded in both the groups. Informed and written consent from each subject was taken before recruiting him/her in the study.
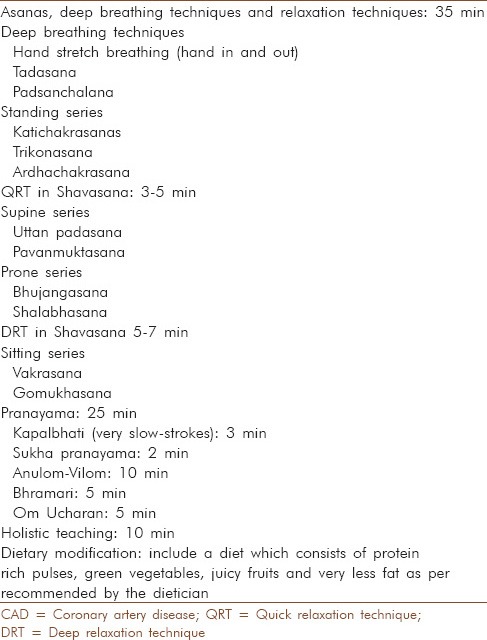
Due to the nonavailability (to the best of our knowledge) of any clearcut article on the effect of yogic intervention on DLCO, sample size of 80 was arbitrarily decided on the basis of observations mentioned by other researchers on other parameters of pulmonary function tests (PFTs) such as FEV1, forced vital capacity (FVC), and peak expiratory flow rate (PEFR). After the initial screening for selection criteria, the selected 80 CAD patients were randomized into two groups of 40 each according to a computer generated randomization list (www.randomization.com). After this all the patients in both the groups underwent a baseline recording of PFTs and single breath DLCO in the cardio-pulmonary lab of Department of Physiology, UCMS. PFTs were recorded thrice in all the subjects and the best of the three was considered for analysis. After the basal recording Group I CAD patients underwent yoga regimen which included yogic postures, pranayama, dietary modifications and holistic teaching [Table 1] along with the conventional medicine while Group II patients were put only on conventional treatment.
Table 1.
Yoga regimen followed by the CAD patients
Blinding and masking
As this was an interventional study double blinding was not possible. Here, the statistician who did the randomization, data analyst, and the researcher who carried out the assessments were blinded to the intervention and treatment status of the patients.
Intervention for the yoga group
All the patients in Group I followed yoga regimen daily for 3 months (90 days). A yoga instructor taught them yogasanas and pranayamas daily for 60 min (6 days/week) in the Yoga Lab of the Physiology Department. This was followed by lectures and group discussions. These sessions were aimed at understanding the need for lifestyle change, weight management and stress and anxiety management their diet was also modified and protein rich pulses, green vegetables, juicy fruits, and very less fat were included as per recommended by the dietician. After this they were asked to practice the whole yoga regimen at home for the next 10 weeks. Compliance was checked telephonically once in 3 days and they were called to the lab weekly for the follow-up.
Intervention for the control group
Group II patients continued their conventional medical treatment after the baseline measurements of lung function tests and they were also put on yoga regimen once they have completed their 3 months follow-up as controls.
Test procedure
Recording of all the parameters of PFTs in both the groups were done thrice during the study period: First on 0 day as basal recording and then repeat recordings were taken on 22nd day and on 90th day after the intervention. Different parameters which were recorded were: Slow vital capacity (SVC), FVC, forced expiratory volume in 1st sec (FEV1), FEV1 /FVC ratio, PEFR, maximum voluntary ventilation (MVV), and single breath DLCO. These lung functions were assessed by using computerized MS medisoft Cardio-respiratory Instrument, HYP’AIR Compact model of cardio-respiratory testing machine was manufactured by P K Morgan, India. The data was analyzed and the results were shown on the computer screen. A total of three tests were performed for all the parameters of PFTs and the best of the three fulfilling the criteria of reproducibility and vitality was considered for analysis. Cardiovascular parameters such as HR, SBP, DBP, and MBP were recorded again in both the groups 90 days of intervention.
Statistical analysis
The data was analyzed intergroup as well as intragroup by using SPSS (Statistical Package for the Social Sciences)is a software used for statistical analysis and is developed by IBM. The baseline values of the two groups were checked for normal distribution by nonparametric Kolmogorov-Smirnov test. PFTs and DLCO within the groups repeated thrice were compared by using repeated measures ANOVA followed by Tukey's test. Significance was considered when P < 0.05. For comparison of PFTs and diffusion capacity between the two groups, unpaired Student's t-test was applied. Cardiovascular parameters - HR, SBP, DBP and MBP were compared after 90 days of intervention in both the groups by using paired student's t-test.
RESULTS
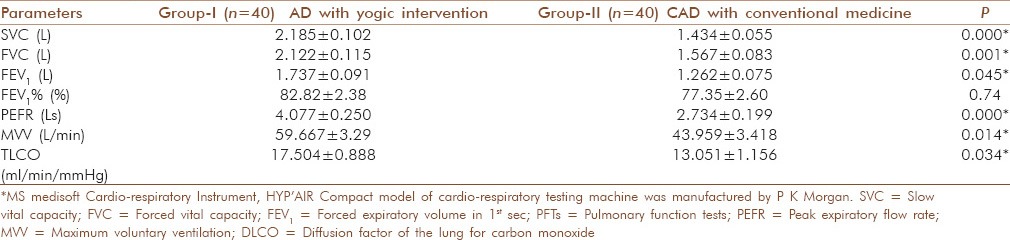
The mean ± standard deviation of SVC, FVC, FEV1, FEV1 %, PEFR, MVV, and DLCO in Group I CAD patients before yogic regimen and after 22nd and 90th day of yogic regimen are given in Table 1. These subjects showed a significant improvement in almost all the parameters of PFTs and in diffusion capacity (DLCO). The PFTs of CAD patients who were on conventional medicine only served as controls are shown in Table 2. These patients did not show significant improvement in lung functions on 22nd day and 90th day. Table 3 is depicting the intergroup comparison of these subjects and controls after 90 days of intervention where Group I CAD patients followed yogic regimen along with conventional medicine while Group II patients were only on conventional medicine. Patients on yogic regimen showed significant improvement in SVC, FVC, FEV1, PEFR, MVV, and DLCO.
Table 2.
PFTs and DLCO in CAD patients before and after intervention in both the groups
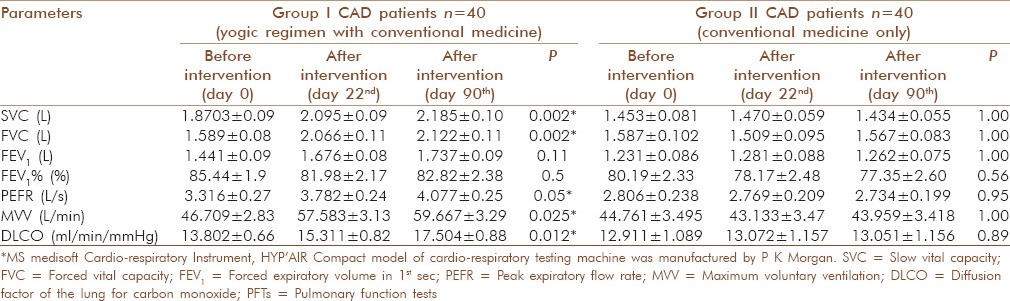
Table 3.
Intergroup comparison of PFTs and DLCO after 90 days of interventions
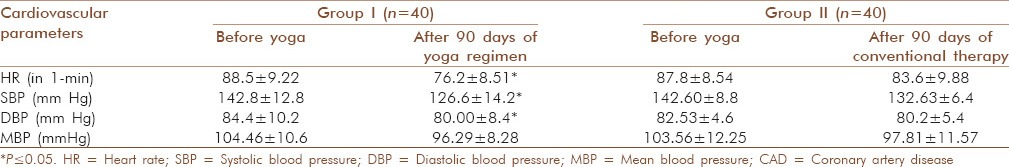
Group I patients who followed yoga regimen showed significant improvement in all the cardiovascular parameters (HR, SBP, and DBP) after 90 days while Group II patients who were on conventional treatment did not show much improvement [Table 4].
Table 4.
Cardiovascular parameters before and after intervention in both the groups of CAD patients
DISCUSSION
In this study, an improvement in almost all the parameters of PFTs - SVC, FVC, FEV1 %, PEFR, MVV, and DLCO was observed in CAD patients after following 3 months of yoga regimen. These improvements are statistically significant in CAD patients on yoga with conventional medicine as compared to patients on conventional medicine only.
This could be because of reduction of sympathetic reactivity attained with yogic training which may allow broncho-dilatation by correcting the abnormal breathing patterns and reducing the muscle tone of inspiratory and expiratory muscles. Due to improved breathing patterns, respiratory bronchioles may be widened and perfusion of a large number of alveoli can be carried out efficiently. [20] Yogic practice covers the entire field of our existence from physical, sensory, emotional, mental and spiritual to the highest self-realization. One of the hallmarks of yoga is balance - which is of both body and mind. Yoga improves the circulation and there is better perfusion of tissues. It increases the strength of respiratory muscles and reduces sympathetic reactivity thereby helps to reduce stress and anxiety which aggravate the severity of CAD.
The further advantage of yogic breathing lies in the fact that it is more a vertical breathing. By this vertical breathing all the alveoli of both the lungs open out evenly. Due to the even expansions of all the alveoli, a vast expense of alveolar membrane is available for exchange of gases. The larger the surface available for the process of diffusion, the better is the process. [21] Generally a small portion of lung capacity is been utilized. This inadequate supply of oxygen results in improper waste disposal from the body. The body functions are slowed down and the cells fail to regenerate themselves due to lack of sufficient energy. Pranayama, a well regulated breathing exercise increases the depth of breathing and expands lungs more than normal and recruits previously closed alveoli. Moreover, endurance power of the lung muscle also improves after adopting yoga. [22]
Ornish et al. showed short term and long term benefits of lifestyle changes (without using cholesterol lowering drugs) on coronary lesions and clinical manifestations of CAD. [14] Manchanda et al. showed similar benefits in Indian patient population in both these studies, number of subjects were small. [11] Recent study done in Global Hospital and Research Centre at Mt. Abu on 123 CAD patients and 360 coronary lesions showed a significant improvement not only in hormonal profile (which showed increased levels of endorphins, serotonin and decreased level of catecholamine), lipid profile, quality of life, but also showed a significant regression of atherosclerotic lesions angiographically in the yoga group. [23] We have also seen significant improvement in cardiovascular parameters such as HR, SBP, and DBP after 90 days yoga regimen in CAD patients.
Very few reports are available which document an improvement in lung functions and prevention of complications after following yoga based lifestyle modification. Our previous pilot study on CAD patients reported an improvement in PEFR, ratio of FEV1 :FVC (FEV1 %), MVV, and forced mid-expiratory flow (25-75) after following 2 weeks of pranayama breathing exercises. [24] The limitation of this study were that the sample size was small, patients performed only pranayama and DLCO could not be recorded. In the present study, the subject size was bigger and they followed a proper yoga based lifestyle which included yogic postures, pranayama, diet management along with holistic teaching for a longer duration, that is, 3 months. Yogic exercises and pranayama may improve lung functions and prevent serious cardio-respiratory complications by emphasizing optimal physical and mental conditioning. Yogic lifestyle modification therapy can be used as an adjunct to pharmacological treatment in CAD patients to achieve optimal results.
Strength of the study
Strength of our study is that it is first randomized control trial depicting the improvement in PFTs especially in diffusion capacity after following a longer duration of yoga regimen (3 months) under the guidance of a yoga instructor. Cardiovascular parameters - HR, SBP, DBP and MBP were compared after 90 days of intervention in both the groups by using paired student's T-test.
Limitations of the study
We have recruited CAD patients irrespective of their gender so the differences on the basis of gender have not been seen in this study. Cardiovascular parameters such as HR, SBP, DBP, and MBP were recorded before and after intervention but the correlation between respiratory and cardiovascular parameters were not done in this study.
CONCLUSIONS
In spite of tremendous advancement in medical technology conventional medicine has proved ineffective in tackling many disorders which have psychosomatic origin. Complementary therapy like yogic exercises and pranayama breathing can be encouraged in CAD patients for their treatment and rehabilitation.
ACKNOWLEDGMENTS
The study was sponsored by grants-in-aid from Central Council for Research in Yoga and Naturopathy (CCRYN), Department of Ayush, Ministry of Health and Family Welfare, New Delhi. We express our sincere gratitude and thanks to all our patients for keeping faith in us and following the yogic regimen as instructed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Chadha SL. Urban-rural differences in prevalence of coronary heart disease and its risk factors. Curr Sci. 1998;74:1069–73. [PMC free article] [PubMed] [Google Scholar]
- 3.Bravata DM, Gienger AL, McDonald KM, Sundaram V, Perez MV, Varghese R, et al. Systematic review: The comparative effectiveness of percutaneous coronary interventions and coronary artery bypass graft surgery. Ann Intern Med. 2007;147:703–16. doi: 10.7326/0003-4819-147-10-200711200-00185. [DOI] [PubMed] [Google Scholar]
- 4.Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–16. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 5.Remetz MS, Cleman MW, Cabin HS. Pulmonary and pleural complications of cardiac disease. Clin Chest Med. 1989;10:545–92. [PubMed] [Google Scholar]
- 6.Hosenpud JD, Stibolt TA, Atwal K, Shelley D. Abnormal pulmonary function specifically related to congestive heart failure: Comparison of patients before and after cardiac transplantation. Am J Med. 1990;88:493–6. doi: 10.1016/0002-9343(90)90428-g. [DOI] [PubMed] [Google Scholar]
- 7.Saadeddin SM, Habbab MA, Ferns GA. Markers of inflammation and coronary artery disease. Med Sci Monit. 2002;8:RA5–12. [PubMed] [Google Scholar]
- 8.Braith RW, Welsch MA, Feigenbaum MS, Kluess HA, Pepine CJ. Neuroendocrine activation in heart failure is modified by endurance exercise training. J Am Coll Cardiol. 1999;34:1170–5. doi: 10.1016/s0735-1097(99)00339-3. [DOI] [PubMed] [Google Scholar]
- 9.Agostoni P, Bussotti M, Cattadori G, Margutti E, Contini M, Muratori M, et al. Gas diffusion and alveolar-capillary unit in chronic heart failure. Eur Heart J. 2006;27:2538–43. doi: 10.1093/eurheartj/ehl302. [DOI] [PubMed] [Google Scholar]
- 10.Guazzi M. Alveolar-capillary membrane dysfunction in chronic heart failure: Pathophysiology and therapeutic implications. Clin Sci (Lond) 2000;98:633–41. [PubMed] [Google Scholar]
- 11.Manchanda SC, Narang R, Reddy KS, Sachdeva U, Prabhakaran D, Dharmanand S, et al. Retardation of coronary atherosclerosis with yoga lifestyle intervention. J Assoc Physicians India. 2000;48:687–94. [PubMed] [Google Scholar]
- 12.Joshi LN, Joshi VD, Gokhale LV. Effect of short term ‘Pranayam’ practice on breathing rate and ventilatory functions of lung. Indian J Physiol Pharmacol. 1992;36:105–8. [PubMed] [Google Scholar]
- 13.Patel C, Marmot MG, Terry DJ, Carruthers M, Hunt B, Patel M. Trial of relaxation in reducing coronary risk: Four year follow up. Br Med J (Clin Res Ed) 1985;290:1103–6. doi: 10.1136/bmj.290.6475.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280:2001–7. doi: 10.1001/jama.280.23.2001. [DOI] [PubMed] [Google Scholar]
- 15.Yogendra J, Yogendra HJ, Ambardekar S, Lele RD, Shetty S, Dave M, et al. Beneficial effects of yoga lifestyle on reversibility of ischaemic heart disease: Caring heart project of International Board of Yoga. J Assoc Physicians India. 2004;52:283–9. [PubMed] [Google Scholar]
- 16.Smith C, Fowler S. Efficacy of breathing and coughing exercises in the prevention of pulmonary complications after coronary artery surgery. Chest. 1995;107:587–8. doi: 10.1378/chest.107.2.587. [DOI] [PubMed] [Google Scholar]
- 17.Sarvottam K, Magan D, Yadav RK, Mehta N, Mahapatra SC. Adiponectin, interleukin-6, and cardiovascular disease risk factors are modified by a short-term yoga-based lifestyle intervention in overweight and obese men. J Altern Complement Med. 2013;19:397–402. doi: 10.1089/acm.2012.0086. [DOI] [PubMed] [Google Scholar]
- 18.Khanam AA, Sachdeva U, Guleria R, Deepak KK. Study of pulmonary and autonomic functions of asthma patients after yoga training. Indian J Physiol Pharmacol. 1996;40:318–24. [PubMed] [Google Scholar]
- 19.Singh S, Soni R, Singh KP, Tandon OP. Effect of yoga practices on pulmonary function tests including transfer factor of lung for carbon monoxide (TLCO) in asthma patients. Indian J Physiol Pharmacol. 2012;56:63–8. [PubMed] [Google Scholar]
- 20.Soni R, Munish K, Singh K, Singh S. Study of the effect of yoga training on diffusion capacity in chronic obstructive pulmonary disease patients: A controlled trial. Int J Yoga. 2012;5:123–7. doi: 10.4103/0973-6131.98230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rai L. A Physiological Approach to Yoga. Gurgaon, India: Anubhav Rai Publishers; 1996. Discovering Human Potential Energy: Health, Stress, Illness, Lifestyle and Disease Reversal. [Google Scholar]
- 22.Chanavirut R, Khaidjapho K, Jarce P, Pongnaratorn P. Yoga exercise increases chest wall expansion and lung volumes in young healthy Thais. Thai J Physiol Sci. 2006;19:1–7. [Google Scholar]
- 23.Gupta SK, Sawhney RC, Rai L, Chavan VD, Dani S, Arora RC, et al. Regression of coronary atherosclerosis through healthy lifestyle in coronary artery disease patients - Mount Abu Open Heart Trial. Indian Heart J. 2011;63:461–9. [PubMed] [Google Scholar]
- 24.Yadav A, Singh S, Singh KP. Role of Pranayama breathing exercises in rehabilitation of CAD patients - A pilot study. Indian J Tradit Knowledge. 2009;8:455–8. [Google Scholar]


