Abstract
Basal Metabolic Rate (BMR) represents the largest component of total energy expenditure and is a major contributor to energy balance. Therefore, accurately estimating BMR is critical for developing rigorous obesity prevention and control strategies. Over the past several decades, numerous BMR formulas have been developed targeted to different population groups. A comprehensive literature search revealed 248 BMR estimation equations developed using diverse ranges of age, gender, race, fat free mass, fat mass, height, waist-to-hip ratio, body mass index, and weight. A subset of 47 studies included enough detail to allow for development of meta-regression equations. Utilizing these studies, meta-equations were developed targeted to twenty specific population groups. This review provides a comprehensive summary of available BMR equations and an estimate of their accuracy. An accompanying online BMR prediction tool (available at http://www.sdl.ise.vt.edu/tutorials.html) was developed to automatically estimate BMR based on the most appropriate equation after user-entry of individual age, race, gender, and weight.
Keywords: Basal Metabolic Rate, Resting Metabolic rate, Prediction, Meta-Analysis, Review, Meta-Regression
1. Introduction
Obesity is the result of a positive imbalance between energy intake and energy expenditure 1. The basal metabolic rate (BMR), defined as the energy required for performing vital body functions at rest, is the largest contributor to energy expenditure. Therefore estimating the total contribution of individual BMR to total daily energy expenditure is an important calculation for understanding, developing, and executing weight related interventions.1, 2 For example, BMR estimation is applied to determine target energy intake in weight loss programs, develop dynamic prediction models of weight gain and loss, identify patients with potential metabolic abnormalities, inform the design of public health programs promoting obesity prevention in diverse populations, and assess potential energy deficits in metabolically stressed patients, such as burn victims. Direct measurement of BMR through indirect calorimetry 3 is not feasible for frequent and timely individual use. As a result, the majority of BMR estimates obtained for weight loss interventions rely on BMR prediction equations. Over the past few decades, a large body of obesity related literature has been devoted to development of BMR equations targeted to specific population demographics.
BMR and the terms resting metabolic rate and resting energy expenditure are often used interchangeably4, however, some investigators differentiate between these terms based on the conditions under which they are measured 5. We limited our review of BMR studies to experiments that have measured the dependent variable, consistent with the definition of BMR 6,7 measured in the post-absorptive state, after at least 10 hours of fasting, determined through direct or indirect calorimetry6,7.. The extensive literature on BMR equations is based on the pioneering work of Harris and Benedict 8 and includes covariates such as age 2, 8–14, body composition (i.e. fat mass and fat free mass) 13, gender and race 15 on BMR. Most of the developed equations have focused on cross sectional data from targeted subpopulations (for example the young adults) and have used a specific equation structure. A review by Frankenfield et al. 16 compares commonly applied BMR prediction equations including Mifflin et al. , 17 Owen et al., 18, 19 Harris and Benedict 8 and WHO report20 to determine the most reliable prediction equation. However current reviews often fail to include different equation structures and populations with different age ranges and race. In fact, a single equation cannot adequately capture the variations across age, race, gender, and body composition.
The purpose of the current paper is to combine, analyze and categorize a comprehensive review of studies that estimate the relationship between BMR and known covariates. The results of the analysis were combined to determine the best fitting BMR prediction equations targeted to different population characteristics. A simple online tool1 that determines the best BMR estimate after user input of age, race, gender, weight, and height was developed to enhance clinical application of study results.
2. Methods
Overview
Models that predict BMR, include different determinants and metabolically active components at four different levels of molecular (Fat mass and fat free mass), cellular (extracellular fluid, and extracellular solids), tissue/organ and whole body (Body Mass). 21 In this Systematic Review, our purpose is to find all regression equations reported in the literature for predicting BMR based on molecular or whole body level factors. More detailed levels of cellular or tissue/organ components, while very important for advancement of our understanding of drivers of BMR, are not considered due to the complexity involved in quantifying those factors which reduces their value for widespread clinical application. In our review, the selected papers contain prediction models for healthy obese or non-obese individuals, differentiated based on their race, gender and age. Due to limited number of primary studies that account for dynamic changes in metabolic rate of a single individual over time (See 22, 23 for notable exceptions), our analysis focuses on equations using cross-sectional data. Then we apply a meta-regression analysis to generate a combined equation that is more robust in predicting BMR for each sub-population group. In our study we refer to meta-regression analysis as a method to develop a single regression equation that summarizes the findings of multiple regressions found in a number of studies.
Literature Search and Filtering
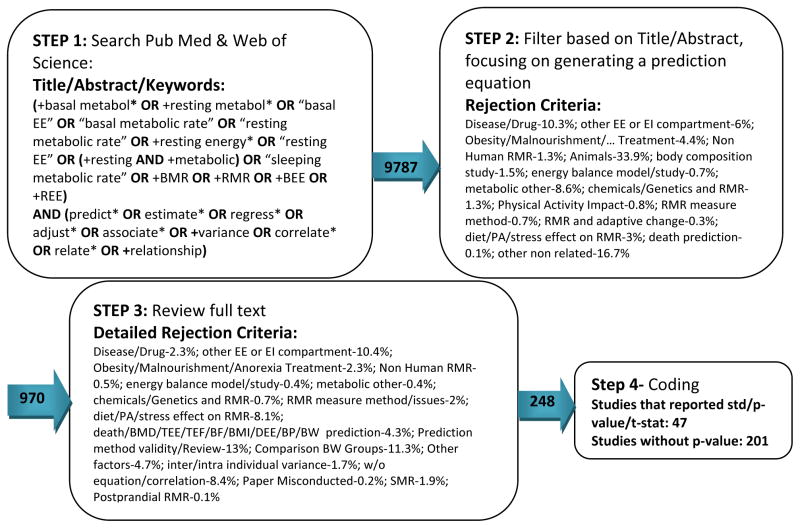
The comprehensive search of the literature was performed in four stages to identify all studies that predict a BMR equation based on an empirical dataset. The specific keywords, used to search PubMed and the Web of Science databases for studies published in any language between the earliest available date October 31, 1923 and March 3, 2011, are shown in Figure 1. Search terms are selected so that any publication, which finds a prediction model for BMR or its alternative terms (Resting Metabolic Rate (RMR), Resting Energy Expenditure (REE) or Basal Energy Expenditure (BEE)), is included. Retrieved articles were reviewed in two steps. First abstracts were reviewed and items obviously not fitting were excluded. Then the full text for the remaining articles were obtained and reviewed to select the articles that included a regression equation based on the criteria above. In a parallel process reference tracking helped identify additional studies not retrieved through automated search.
Figure 1.
Flowchart of literature search and selection process
Literature Coding
The regression equations reported in the remaining sample were extracted into a database. These studies fall into two categories, first, those studies that lack estimates of variance for reported regression coefficients. These are coded by including the data sample size and determinants used to estimate BMR for future research, but are not further analyzed in this paper because they lacked enough specificity to allow parametric meta-regression. The second group consisted of studies that include some measure of variance such as standard deviation, p-value, or t statistic. The details of the data set used in the study and the equations developed were extracted from this group (See online supporting information S1). Variance or standard deviation of reported regression parameters is needed for conducting meta-regression analysis. Therefore we follow a set of procedures to consistently extract/estimate this factor, which is described in online supporting information S2. The full set of references without estimates of variance is reported in online supporting information S4.
Meta-Regression Analysis
Resulting equations are grouped based on sub-populations they were developed for (based on gender, age group, and race) and the structure of the regression equation (i.e. independent variables included and the transformations used). Within each group with homogenous population and equation structure, we combined all the extracted equations to form a single new equation that aggregates different previous findings. If a study estimates a single equation for two different groups (e.g. 18–50 and >50 years old groups), we used that equation separately in estimating the aggregate equations for each of the groups.
There are different approaches in the literature for synthesizing coefficients (slopes) of a set of similar regressions found in different studies into a single slope, 24 which in this paper we refer to as meta-regression2. The more statistically precise methods, such as the multivariate Generalized Linear Square approach, 24 require the covariance between different slopes. However the covariance matrices are rarely reported in studies. In fact none of the studies found in the literature search for this paper included the covariance matrix of slopes. Instead we used an alternative method that has been applied to different problems in the literature, 26–28 and only requires the regression coefficients and the standard error for each coefficient. In this method the meta-coefficient for each factor is calculated using a weighted average of the same coefficient across the different studies. The weights are reciprocal of the variance of those coefficients and also allow us to calculate the variance of the meta-coefficient (See online supporting information S2). The meta-regression analysis is conducted in Microsoft Excel (2010).
3. Results
The initial search identified 9787 studies, including 39 studies identified from cross-referencing, that cover a broad range of items. All of the titles and abstracts of these studies were reviewed in the first step to filter out the clearly un-related papers. The full set of exclusion criteria are shown in step 2 of Figure 1. Next, by reviewing the full text of 970 remaining studies, 712 studies were excluded due to different criteria reported in Figure 1, including (but not limited to) those that focus on inter/intra individual variance of BMR, studies just describing correlation values between BMR and different factors (but no regression equation), those focusing on sleeping metabolic rate or postprandial BMR (i.e. not after 10–12 hours fasting), those finding the relation between BMR and factors at a cellular level, such as blood adipocytokines, pulse pressure and protein turnover. After this screening process, 248 studies that generate a regression equation for predicting BMR based on a data set of healthy obese or non-obese individuals were reviewed and coded.
The final set of 248 papers is categorized into two groups. The first category, those lacking enough details to allow analytical meta-regression included 201 studies (See online supporting information S4 for the full list). The final category with enough details to enable meta-regression includes 47 studies. These papers report regression results for BMR as the independent variable and different sets of determinants. Both coefficients and their corresponding standard deviation (or a related concept such as p-value or t-statistic) are coded in a database.
The final set of studies is categorized into different groups based on the structure of the regression equation and the population subgroups distinguished by age, gender, and race. As a result seventeen categories of Regression Models and twenty subpopulation groups are identified. Note that age ranges for children, adult, and older adult vary slightly across different subpopulation groups due to variations in the definitions used for different studies (See online supporting information S3 for a summary table).
For each population group (based on age, gender, and race) and each regression structure meta regression formulas (See online supplement S2) are applied to estimate a single meta regression equation. These results are shown in Table 1. For each subpopulation, a list of resulting meta-regression equation results, the original references that were combined, and the range, mean, and standard deviation of R2 (a commonly reported measure of goodness of fit) for the original studies are reported.
Table 1.
Master table including meta-regression equations estimated for different equation structures and population groups. Meta-regression coefficients (standard error) are reported in each cell. Also reported are the number of studies, Range of R2, and average (Standard Error) of R2.
| Female | Male | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Structure | References | Range R2 | Average R2 (SD) |
β0 = Intercept |
β1 W | β2 H | β3 A | β4 FFM | β5 FM | β6 WHR | β7 BMI | Range R2 | Average R2 (SD) |
β0 = Intercept |
β1 W | β2 H | β3A | β4 FFM | β5FM | β6 WHR | β7 BMI | |
| White 5–18 | 1 | 35, 36, 37 | 0.48–0.859 | 0.65 (0.158) | 84.7(50.3) | 11.1(0.398) | 5.46 (0.753) | −24.8(3.03) | 0.6–0.859 | 0.695 (0.113) | 220(50.5) | 11.3(0.409) | 5.82 (0.77) | −25.5(3.15) | ||||||||
| 2 | 38 | 28.3(0.824) | 6.61(1.43) | 29.7 (0.682) | 4.37(2.99) | |||||||||||||||||
| 3 | 37 | 0.59 | 901(73.8) | 9.8 (0.72) | 0.59 | 933(73.8) | 12.2(0.72) | |||||||||||||||
| 5 | 39, 40, 41, 37 | 0.57–0.7 | 0.625 (0.058) | 218(25.9) | 23.9(1.4) | 0.47–0.7 | 0.583 (0.0943) | 219(26.2) | 25.4(1.44) | |||||||||||||
| 8 | 37 | 0.31 | 1600(139) | 15.8(9.6) | 0.31 | 848(139) | 94.9(9.6) | |||||||||||||||
| 9 | 37 | 0.59 | 870(44.5) | −6.69(3.29) | 23.7(0.837) | 0.59 | 870(44.5) | −6.69(3.29) | 23.7 (0.837) | |||||||||||||
| 10 | 37 | 0.59 | 909(46) | 12(0.418) | −13.6(3.41) | 0.59 | 1150(46) | 12(0.418) | −13.6(3.41) | |||||||||||||
| 11 | 14, 36, 37, 42 | 0.47–0.79 | 0.642 (0.12) | 513(33.2) | −7.77(1.48) | 15.4(1.3) | 12.1 (0.819) | 0.59–0.79 | 0.678 (0.074) | 680(33.3) | −7.61(1.49) | 16.9(1.36) | 12.8 (0.868) | |||||||||
| 15 | 37 | 0.41 | −708(327) | 15.8 (2.04) | 0.41 | −1320(327) | 21 (2.04) | |||||||||||||||
| 16 | 37 | 0.47 | 890(109) | 25.6 (2.93) | 0.47 | 639(109) | 41.8 (2.93) | |||||||||||||||
| 17 | 37 | 0.58 | 956(72.2) | 17.4 (1.41) | 0.58 | 954(72.2) | 23.9(1.41) | |||||||||||||||
| Black 5–17 | 5 | 39, 40, 41 | 0.5–0.7 | 0.57 (0.113) | 53.5(27.5) | 29.5(2.81) | 0.51–0.7 | 0.587 (0.1) | 55(27.5) | 30 (2.77) | ||||||||||||
| 11 | 14 | 0.79 | −235(53.8) | −15 (7.31) | 19.8(6.4) | 7.6(5.03) | 0.79 | −111(53.8) | −15(7.31) | 19.8 (6.4) | 7.6(5.03) | |||||||||||
| Hispanic 4–6 | 5 | 43 | 0.384–0.792 | 0.588 (0.288) | 28.6(26.6) | 13(1.63) | 0.384 – 0.792 | 0.588 (0.288) | 28.6(26.6) | 13 (1.63) | ||||||||||||
| White 18–57 | 1 | 44, 45, 46, 37 | 0.449–0.75 | 0.619 (0.129) | 301(65.1) | 10.2 (0.152) | 3.09 (0.385) | −3.09 (0.168) | 0.6–0.75 | 0.671 (0.0619) | 522(65.8) | 10.4 (0.156) | 3.19 (0.388) | −3.1(0.169) | ||||||||
| 2 | 38 | 28.3(0.824) | 6.61(1.43) | 29.7 (0.682) | 4.37(2.99) | |||||||||||||||||
| 3 | 47, 48$, 37, 49$ | 0.449–0.9 | 0.645 (0.188) | 632(33.3) | 10.9 (0.324) | 0.59 – 0.9 | 0.745 (0.219) | 778(39.1) | 11.7 (0.339) | |||||||||||||
| 4 | 50$, 51, 52, 53, 47 | 0.526–0.91 | 0.804 (0.15) | 360(29.5) | 21(0.494) | 4.68 (0.455) | 0.612 – 0.91 | 0.809 (0.135) | 361(30.8) | 21.1 (0.498) | 4.77(0.483) | |||||||||||
| 5 | 48$, 54, 55 , 56, 53, 57, 58, 37, 59 | 0.53–0.922 | 0.675 (0.115) | 473(15.5) | 20.1 (0.43) | 0.53 – 0.922 | 0.674 (0.121) | 503(15.6) | 18.3 (0.436) | |||||||||||||
| 6* | 12 | 0.806 | 4.65 (0.229) | −0.00125 (0.000405) | 0.624** (0.202) | 0.0907*** (0.0294) | 0.806 | 4.71(0.229) | −0.00125 (0.000405) | 0.624** (0.202) | 0.0907*** (0.0294) | |||||||||||
| 8 | 37 | 0.33 | 2020(33) | −5.02 (0.668) | 0.33 | 2640(33) | −8.37 (0.668) | |||||||||||||||
| 9 | 37, 45 | 0.588–0.59 | 0.589 (0.00141) | 838(22.8) | −2.41 (0.176) | 19.7 (0.287) | 0.588 – 0.59 | 0.589 (0.00141) | 830(22.8) | −2.41 (0.176) | 19.7 (0.287) | |||||||||||
| 10 | 37, 60 | 0.42–0.6 | 0.51 (0.127) | 781(22) | 11 (0.178) | −3.45 (0.232) | 0.6 – 0.69 | 0.645 (0.0636) | 1050(22.2) | 11(0.178) | −3.53 (0.236) | |||||||||||
| 11 | 61, 44, 53 , 42, 62$, 63, 64, 65, 66, 37 , 67, 68, 46 | 0.425–0.88 | 0.66 (0.136) | 682(25) | −3.08 (0.194) | 12.9 (0.47) | 5.9(0.313) | 0.45 – 0.88 | 0.711 (0.208) | 898(27.1) | −3.32 (0.207) | 14.3 (0.507) | 6.46(0.374) | |||||||||
| 12 | 45 | 0.657 | 1380(59.6) | −6.18 (0.744) | 11.5 (0.462) | 0.657 | 1930(59.6) | −6.18 (0.744) | 11.5(0.462) | |||||||||||||
| 13 | 45 | 0.647 | 886(72.2) | −6.08 (0.742) | 26.8 (1.07) | 0.647 | 1440(72.2) | −6.08 (0.742) | 26.8 (1.07) | |||||||||||||
| 14 | 69 | 0.736 | 560(131) | 5.39 (2.15) | 14.1 (3.73) | 0.736 | 560(131) | 5.39(2.15) | 14.1 (3.73) | |||||||||||||
| 15 | 37 | 0.38 | −417(203) | 13.9 (1.18) | 0.38 | −1390(203) | 21.3 (1.18) | |||||||||||||||
| 16 | 37 | 0.47 | 794(53.2) | 23.4 (1.28) | 0.47 | 985(53.2) | 30.4 (1.28) | |||||||||||||||
| 17 | 37 | 0.57 | 631(43.4) | 21.7 (0.882) | 0.57 | 856(43.4) | 30.4(0.882) | |||||||||||||||
| White >50 | 1 | 44, 45, 46, 37 | 0.449–0.75 | 0.619 (0.129) | 301(65.1) | 10.2 (0.152) | 3.09(0.385) | −3.09(0.168) | 0.6 – 0.75 | 0.671 (0.0619) | 522(65.8) | 10.4(0.156) | 3.19 (0.388) | −3.1 (0.169) | ||||||||
| 3 | 47, 37 | 0.59–0.9 | 0.745 (0.219) | 568(39.1) | 11.1 (0.339) | 0.59 – 0.9 | 0.745 (0.219) | 743(39.1) | 11.7(0.339) | |||||||||||||
| 4 | 70$, 51, 52, 53, 47 | 0.526–0.89 | 0.751 (0.149) | 290(32.4) | 19.9 (0.541) | 4.71 (0.466) | 0.612 – 0.89 | 0.789 (0.121) | 291(34.3) | 20 (0.547) | 4.64(0.497) | |||||||||||
| 5 | 37, 59, 57, 53 | 0.59–0.74 | 0.669 (0.0642) | 429(17.9) | 20.9 (0.53) | 0.59 – 0.74 | 0.669 (0.0642) | 464(17.9) | 18.6 (0.53) | |||||||||||||
| 6* | 12 | 0.806 | 4.65 (0.229) | −0.00125 (0.000405) | 0.624** (0.202) | 0.0907*** (0.0294) | 0.806 | 4.71(0.229) | −0.00125 (0.000405) | 0.624** (0.202) | 0.0907*** (0.0294) | |||||||||||
| 7 | 71, 72 | 479(80.6) | −1.99 (0.928) | 16.1 (0.606) | 6.09 (0.434) | 118 (34) | 893(80.6) | −7.06 (0.928) | 16.1 (0.606) | 6.09(0.434) | 118 (34) | |||||||||||
| 8 | 37, 71, 72 | 0.33 | 1950(30.5) | −4.72 (0.572) | 0.33–0.33 | 0.33 | 2570(30.5) | −8.29 (0.572) | ||||||||||||||
| 9 | 37, 45, 59 | 0.588–0.77 | 0.649 (0.105) | 838(22.8) | −2.43 (0.175) | 19.8 (0.283) | 0.588 – 0.77 | 0.649 (0.105) | 829(22.8) | −2.43 (0.175) | 19.8 (0.283) | |||||||||||
| 10 | 37, 60, 59 | 0.42–0.74 | 0.587 (0.16) | 784(21.9) | 10.9 (0.173) | −3.47 (0.231) | 0.6 – 0.74 | 0.677 (0.0709) | 1050(22.1) | 10.9(0.173) | −3.55 (0.235) | |||||||||||
| 11 | 61, 44, 53, 42, 62$, 63, 64, 65, 66, 37, 67, 68, 46 | 0.425–0.88 | 0.66 (0.136) | 682(25) | −3.08 (0.194) | 12.9 (0.47) | 5.9 (0.313) | 0.45 – 0.88 | 0.711 (0.208) | 898(27.1) | −3.32 (0.207) | 14.3 (0.507) | 6.46(0.374) | |||||||||
| 12 | 45 | 0.657 | 1380(59.6) | −6.18 (0.744) | 11.5 (0.462) | 0.657 | 1930(59.6) | −6.18 (0.744) | 11.5(0.462) | |||||||||||||
| 13 | 45 | 0.647 | 886(72.2) | −6.08 (0.742) | 26.8 (1.07) | 0.647 | 1440(72.2) | −6.08 (0.742) | 26.8 (1.07) | |||||||||||||
| 15 | 37 | 0.38 | −417(203) | 13.9 (1.18) | 0.38 | −1390(203) | 21.3 (1.18) | |||||||||||||||
| 16 | 37 | 0.47 | 794(53.2) | 23.4 (1.28) | 0.47 | 985(53.2) | 30.4 (1.28) | |||||||||||||||
| 17 | 37 | 0.57 | 631(43.4) | 21.7 (0.882) | 0.57 | 856(43.4) | 30.4(0.882) | |||||||||||||||
| Asian 18–30 | 1 | 63 | 0.834 | −101(337) | 11.5 (1.1) | 5.59 (2.01) | −3.3 (0.598) | **** | 0.834 | 883(471) | 11.5(1.1) | 5.59 (2.01) | −3.3 (0.598) | |||||||||
| 3 | 73 | 593(133) | 10.9 (2.72) | |||||||||||||||||||
| 10 | 74& | **** | 0.41 | 860(152) | 11.6(1.3) | −3.37 (1.03) | ||||||||||||||||
| Black 18–50 | 1 | 46 | 0.675 | 883(471) | 8.7 (1.4) | −0.342 (2.94) | −3.9 (0.8) | 0.675 | 1100(471) | 8.7 (1.4) | −0.342 (2.94) | −3.9 (0.8) | ||||||||||
| 3 | 49, 75& | 0.548 | 302(148) | 13.2 (3.55) | 0.548 | 500(96.5) | 15.6 (1.6) | |||||||||||||||
| 4 | 76 | 0.75–0.84 | 0.783 (0.0441) | 397(79.5) | 20.6 (2.72) | 1.9 (0.575) | 0.75 – 0.84 | 0.783 (0.0441) | 421(82.8) | 20.6 (2.72) | 1.9(0.575) | |||||||||||
| 5 | 59, 76 ,75& | 0.66–0.83 | 0.748(0.0695) | 400(42) | 16.6 (0.949) | 0.66 – 0.83 | 0.73 (0.0718) | 392(39.1) | 17.4 (0.861) | |||||||||||||
| 11 | 64, 46 | 0.68–0.71 | 0.695 (0.015) | 678(92.8) | −3.28 (0.485) | 13.6 (1.16) | 5.95 (1.03) | 0.68 – 0.71 | 0.695 (0.015) | 787(92.8) | −3.28 (0.485) | 13.6 (1.16) | 5.95(1.03) | |||||||||
| Black >50 | 1 | 46 | 0.675 | 883(471) | 8.7 (1.4) | −0.342 (2.94) | −3.9 (0.8) | 0.675 | 1100(471) | 8.7 (1.4) | −0.342 (2.94) | −3.9 (0.8) | ||||||||||
| 3 | 49& | 0.63 | 302(148) | 13.2 (3.55) | ||||||||||||||||||
| 4 | 76 | 0.75–0.84 | 0.783 (0.0441) | 397(79.5) | 20.6 (2.72) | 1.9 (0.575) | 0.75 – 0.84 | 0.783 (0.0441) | 421(82.8) | 20.6 (2.72) | 1.9(0.575) | |||||||||||
| 5 | 59, 76 | 0.66–0.83 | 0.748 (0.0695) | 400(42) | 16.6 (0.949) | 0.66 – 0.83 | 0.748 (0.0695) | 400(42) | 16.6 (0.949) | |||||||||||||
| 9 | 59 | 0.69 | 1260(262) | −11.2 (3.4) | 15.9 (5.52) | 0.69 | 1260(262) | −11.2 (3.4) | 15.9 (5.52) | |||||||||||||
| 10 | 59 | 0.67 | 1420(281) | 7.6 (0.7) | −11.4 (3.5) | 0.67 | 1590(281) | 7.6 (0.7) | −11.4 (3.5) | |||||||||||||
| 11 | 64, 46 | 0.68–0.71 | 0.695 (0.015) | 678(92.8) | −3.28 (0.485) | 13.6 (1.16) | 5.95 (1.03) | 0.68 – 0.71 | 0.695 (0.015) | 787(92.8) | −3.28 (0.485) | 13.6 (1.16) | 5.95(1.03) | |||||||||
| >50 Hispanic | 3 | 77 | 0.75 | 394(105) | 13.6 (1.62) | 0.75 | 502(105) | 13.6 (1.62) | ||||||||||||||
| 18–50 Native American | 11 | 65 | 0.88 | 705(60.3) | −2.2 (0.8) | 15 (1.1) | 4.4 (0.7) | 0.88 | 829(60.3) | −2.2 (0.8) | 15 (1.1) | 4.4(0.7) | ||||||||||
Structure 6 estimates logeBMR.
Coefficient for logeFFM
Coefficient for logeFM
The age group is 18–50.
This reference only applies to the female equation.
This reference only applies to the male equation.
Abbreviations- W: Weight (kg); H: Height (cm); A: Age (years); FFM: Fat-Free Mass (kg); FM: Fat Mass (kg); WHR: Waist-to-Hip-Ratio; BMI: Body Mass Index (kg/m2). F: Female; M: Male; T: White; B: African American; P: Hispanic; S: Asian; I: Pima Native American; Equation Structures- 1: β0 + β1W + β2H + β3A; 2: β4FFM + β5FM; 3: β0 + β1W; 4: β0 + β4FFM + β5FM; 5: β0 + β4FFM; 6: β0 + β3A + β4logeFFM + β5logeFM; 7: β0 + β3A + β4FFM +β5FM + β6WHR; 8: β0 + β3A; 9: β0 + β3A + β4FFM; 10: β0 + β1W + β3A; 11: β0 + β3A + β4FFM + β5FM; 12: β0 + β3A + β5FM; 13: β0 + β3A + β7BMI; 14: β0 + β1W + β4FFM; 15: β0 + β2H; 16: β0 + β7BMI; 17: β0 + β5FM;
Using the Resulting Equations
For a concrete example, consider calculating the expected BMR for a 35-year-old white female who weighs 75 kg (165 lb) and is 165 cm (5’ 5”) tall. With this information we can look up the designated rows in Table 1 (identified as “White 18–57”; the left hand columns for female) and identify equation structures 1, 3, 10, and 15 for which meta regression equations are available. Based on R2 values, structures 1 and 3 are deemed more accurate. Equation structure 1 can be read as: BMR=301+10.2W+3.09H-3.09A, calculating this with W=75kg, H=165cm, and A=35, we obtain a BMR of 1467.7 kcal/Day. This value is close to the predictions obtained from Harris and Benedict 8 (H&B) equation3 (1513.8), World Health Organization (WHO) report 20 equation4 (1558.7) and Institute of Medicine (IOM) report 29 equation5 (1475.9). While offering results consistent with more commonly used equations for typical cases, Table 1 can provide empirically estimated equations for older ages (Note that the Harris Benedict sample was under 45, and WHO equations do not include age) and when additional data items are available (e.g. fat free mass (FFM) and waist to hip ratio (WHR); neither included in WHO, IOM, or H&B equations). Table 1 can also provide estimated variations across different ethnicities (not included in WHO, IOM, or H&B equations). Such flexibility can be beneficial in making the best use of available data for research and clinical applications. We also have developed an online tool, which predicts BMR for subjects in different demographic groups depending on what information (e.g. age, weight, and height) is available about them. In addition to the meta-regression results developed in this paper, the tool includes the relevant predictions from IOM and WHO reports for each subject, allowing the user to make comparisons and reach an informed consensus. Details are reported in online supplement S5.
Impact of Body Composition
Overall, consistent with previous findings, Fat-Free Mass is the best independent predictor of BMR 13 as evidenced by good predictive power of equation structure 5 (β0 + β4FFM) in many population groups. Weight is almost as good a predictor as Fat-Free Mass, based on comparing the effect sizes for different independent variables. FM has a moderately positive coefficient and provides a slight improvement in predictive power. Comparing structures 4 (β0 + β4FFM+ β5FM) and 5 (β0 + β4FFM), it appears that impact of FM and FFM are independent, i.e. inclusion of FM does not change the FFM coefficient. Moreover, logarithmic functions may describe the FFM and FM effect as well as, if not better than, linear effects (comparing structures 6 and 11). In fact with logarithmic functional forms for FFM/FM the intercept shrinks considerably, suggesting that with the logarithmic nonlinearity FM and FFM can explain the majority of variation in BMR.
Impact of Age
The direct impact of age is most pronounced for the children but is also significant in adults, and is consistently negative. The age impact is slightly stronger in male than female. Age also has a more subtle interaction with other factors. Comparing equation structures 4 (β0 + β4FFM+ β5FM) and 11 (β0+ β3A + β4FFM + β5FM), we note that by including Age, the coefficient for FFM shrinks (from ~20 to ~13 kcal/kg/day for adults) while the constant term becomes larger, i.e. age and a constant term can replace a significant portion of FFM contribution to BMR. This may suggest a reduction in tissue-specific organ metabolic rates as people age. 30 The underlying mechanisms to explain the compensating effects of FFM and Age may require cellular level measures in BMR estimation31 yet inclusion of Waist to Hip Ratio (WHR) among the independent variables restores some of the direct effect of FFM (structure 7: β0 + β3A + β4FFM +β5FM + β6WHR), suggesting that WHR is informative in understanding the interaction of Age and FFM. Other predictors including height and BMI are statistically significant when included, but their significance may be attributed to lack of controls for fat-free mass or weight in those equations.
Best Fitting Equations for Subpopulations
We elaborate on the best fitting equation structures for each major subpopulation separately. For Female-White-5–18 group, equation structures 1 (β0 + β1W + β2H + β3A), 2 (β4FFM + β5FM), 5 (β0 + β4FFM) and 11 (β0+ β3A + β4FFM + β5FM), are the results of combining 3 or more studies. Structures 1 and 11 have the highest average R2, but structure 5 is also very close (average R2=0.625). Nevertheless including Age, Height, and FM can all lead to more precise BMR predictions. The same conclusions hold for ‘Male-White-5–18 and, should the required information be available, we suggest applying either structure 1 or 11 for predicting BMR in this sub-population as well. Only two equation structures have been estimated for African-American youth (4.7–17 years old). While more studies have used structure 5, structure 11 offers a better fit and thus can be recommended. A single equation structure is available for Hispanic children (4–6 years).
For adult white groups (male and female, 18–50 and 50+ groups) structures 1, 2, 3 (β0 + β1W), 4 (β0 + β4FFM + β5FM), 5, 9 (β0 + β3A + β4FFM), 10 (β0 + β1W + β3A) and 11 are estimated based on multiple studies.
Structures 4, 5 and 11 have higher average R2 with 4 and 11 providing a good balance in terms of precision and empirical support (more than 5 studies and R2 between 0.7 and 0.8). For the adult African American groups, equations 4, 5, and 11 are well supported and offer good fits with R2 values typically between 0.6 and 0.8. For other population groups (Asians, Native Americans and adult Hispanics) a single regression exists for each equation structure and therefore available choices are limited.
4. Conclusions
This study provides a comprehensive review of the BMR prediction equation literature to develop meta-predictive equations using seventeen different structures and for twenty different subpopulations. Providing robust equations for predicting expected BMR, the results can inform obesity interventions in diverse populations. For example the equations can inform setting energy intake goals in weight loss programs, help build dynamic models of weight gain and loss, speed up the calibration of personalized obesity interventions, enable the identification of patients with potential metabolic abnormalities, estimate energy deficits for metabolically stressed individuals, and inform the design of public health programs promoting obesity prevention in diverse populations. The equations provide enough flexibility for accommodating a host of different independent variables, depending on the availability of data for the application at hand. The accompanying BMR prediction tool simplifies the application of results by practitioners.
From the 248 studies with predictive equations that we retrieved, only 19% included enough detail regarding their estimated equations to allow for reliable comparison and meta-regression. Mathematical models 32 increasingly rely on regression equations such as those summarized here. Weight change experiments and commercial weight loss centers often depend upon BMR regression equations to design their interventions. Explicit quantification of variance is a critical factor for pooling data and models, improving these models, and appropriately informing health care providers on the accuracy and limitations of developed models.
In practice, application of a best fitting equation is also limited by data availability. While FFM, FM, and waist and hip circumference are significant predictors of BMR, these variables may not be available to researchers or individuals. We take a step towards addressing this challenge by providing meta-regression equations with different independent factors, including those that only rely on a subset of easily measured covariates (weight, age, height, gender, and race).
Several areas for future research can improve these results. Individual life histories can provide additional predictive variables not included in our meta-regression equations due to the limited number of longitudinal primary studies. For example rapid weight loss can lead to sustained BMR reduction even if FFM is sustained, effectively changing the coefficient for FFM 22. Such information may be especially relevant for designing individualized interventions. Methodologically, the meta-regression formulations we used, while commonly applied in the literature 26–28, assume independence among estimated coefficients, which could not be verified in the absence of the correlation matrix for coefficients. This may have led to under-estimation of variance in meta-coefficients. Moreover, researchers will be interested in the net value of adding each independent variable in balancing equation complexity against the predictive power of a model. If different models (with different combinations of independent variables) are estimated on the same data, measures such as Bayesian 33 and Akaike 34 Information Criteria can be used to tradeoff model parsimony against predictive power. Such comparisons are not feasible in the current study because each equation is estimated on a different dataset, nevertheless estimated parameter variances provide related information on marginal value of different BMR predictors. Improved meta-regression techniques could be developed to correct for these potential shortcomings. Individual-level data can also be used to empirically compare the precision of different equation structures we have identified.
Supplementary Material
Acknowledgments
We thank the editor and three anonymous reviewers for their constructive feedback. Participants in the National Collaborative on Childhood Obesity Research (NCCOR) Envision’s Comparative Modeling Network (CompMod) program provided helpful comments. Financial Support Provided through Envision’s CompMod program and NIH Office of Behavioral and Social Sciences Research (OBSSR) contract: HHSN276201000004C and grant R21HL113680.
Footnotes
We thank one of the reviewers for recommending the development of this tool, which is available at http://www.sdl.ise.vt.edu/tutorials.html and also as part of the online supplement on Journal’s website.
Some refer to meta-regression as running a regression on a common summary statistic drawn from the primary studies as the dependent variable 25. Our use of the term differs from this definition.
BMR=655+9.5634W+1.8496H-4.6756A
BMR=(3619+36.4W+1.046H)/4.184 (note that equation is modified to provide BMR in Kcal/day rather than J/Day)
BMR=247+8.6W+4.105H-2.67A
Conflict of interest
The authors declare no conflict of interest.
Additional Supplementary Information may be found in the online version of this article at the International Journal of Obesity’s website. The file includes the following:
S1. Coding Details
S2. Procedures to calculate meta coefficients and calculate variance of reported regression parameters based on p-value or t-statistic.
S3- Study categories, equation structures, and the related references.
S4. The first category of studies, identified from the Systematic Review, include 201 studies. These studies predict a BMR equation based on an empirical dataset, but lack enough detail to allow analytical meta-regression.
S5. The equations used in the online BMR prediction tool.
References
- 1.Abdel-Hamid TK. Modeling the dynamics of human energy regulation and its implications for obesity treatment. System Dynamics Review. 2002;18(4):431–471. [Google Scholar]
- 2.Poehlman ET. Energy expenditure and requirements in aging humans. J Nutr. 1992;122(11):2057–65. doi: 10.1093/jn/122.11.2057. [DOI] [PubMed] [Google Scholar]
- 3.Ferrannini E. The theoretical bases of indirect calorimetry: A review. Metabolism. 1988;37(3):287–301. doi: 10.1016/0026-0495(88)90110-2. [DOI] [PubMed] [Google Scholar]
- 4.Bogardus C, Lillioja S, Ravussin E, Abbott W, Zawadzki JK, Young A, et al. Familial dependence of the resting metabolic rate. N Engl J Med. 1986;315(2):96–100. doi: 10.1056/NEJM198607103150205. [DOI] [PubMed] [Google Scholar]
- 5.Heymsfield SB, Thomas D, Bosy-Westphal A, Shen W, Peterson CM, Muller MJ. Evolving concepts on adjusting human resting energy expenditure measurements for body size. Obes Rev. 2012 doi: 10.1111/j.1467-789X.2012.01019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sherman HC. Chemistry of food and nutrition. Macmillan Co; New York: 1946. [Google Scholar]
- 7.Torun B, Davies P, Livingstone M, Paolisso M, Sackett R, Spurr G. Energy requirements and dietary energy recommendations for children and adolescents 1 to 18 years old. Eur J Clin Nutr. 1996;50(Suppl 1):S37–80. discussion S80–1. [PubMed] [Google Scholar]
- 8.Harris J, Benedict F. A biometric Study of basal metabolism in man. Carnegie Institution; Washington, DC: 1919. [Google Scholar]
- 9.Cunningham JJ. A reanalysis of the factors influencing basal metabolic rate in normal adults. Am J Clin Nutr. 1980;33(11):2372–4. doi: 10.1093/ajcn/33.11.2372. [DOI] [PubMed] [Google Scholar]
- 10.Maffeis C, Schutz Y, Micciolo R, Zoccante L, Pinelli L. Resting metabolic rate in six- to ten-year-old obese and nonobese children. The Journal Of Pediatrics. 1993;122(4):556–562. doi: 10.1016/s0022-3476(05)83535-8. [DOI] [PubMed] [Google Scholar]
- 11.Vaughan L, Zurlo F, Ravussin E. Aging and energy expenditure. Am J Clin Nutr. 1991;53(4):821–825. doi: 10.1093/ajcn/53.4.821. [DOI] [PubMed] [Google Scholar]
- 12.Speakman JR, Westerterp KR. Associations between energy demands, physical activity, and body composition in adult humans between 18 and 96 y of age. Am J Clin Nutr. 2010;92(4):826–34. doi: 10.3945/ajcn.2009.28540. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham J. Body composition as a determinant of energy expenditure: a synthetic review and a proposed general prediction equation. Am J Clin Nutr. 1991;54(6):963–969. doi: 10.1093/ajcn/54.6.963. [DOI] [PubMed] [Google Scholar]
- 14.Tershakovec AM, Kuppler KM, Zemel B, Stallings VA. Age, sex, ethnicity, body composition, and resting energy expenditure of obese African American and white children and adolescents. Am J Clin Nutr. 2002;75(5):867–71. doi: 10.1093/ajcn/75.5.867. [DOI] [PubMed] [Google Scholar]
- 15.Bhopal RS, Rafnsson SB. Could mitochondrial efficiency explain the susceptibility to adiposity, metabolic syndrome, diabetes and cardiovascular diseases in South Asian populations? Int J Epidemiol. 2009;38(4):1072–81. doi: 10.1093/ije/dyp202. [DOI] [PubMed] [Google Scholar]
- 16.Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc. 2005;105(5):775–89. doi: 10.1016/j.jada.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51(2):241–7. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 18.Owen OE, Holup JL, D'Alessio DA, Craig ES, Polansky M, Smalley KJ, et al. A reappraisal of the caloric requirements of men. Am J Clin Nutr. 1987;46(6):875–85. doi: 10.1093/ajcn/46.6.875. [DOI] [PubMed] [Google Scholar]
- 19.Owen OE, Kavle E, Owen RS, Polansky M, Caprio S, Mozzoli MA, et al. A reappraisal of caloric requirements in healthy women. Am J Clin Nutr. 1986;44(1):1–19. doi: 10.1093/ajcn/44.1.1. [DOI] [PubMed] [Google Scholar]
- 20.WHO. Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert Consultation. World Health Organ Tech Rep Ser. 1985;724:1–206. [PubMed] [Google Scholar]
- 21.Wang Z, Heshka S, Gallagher D, Boozer CN, Kotler DP, Heymsfield SB. Resting energy expenditure-fat-free mass relationship: new insights provided by body composition modeling. Am J Physiol Endocrinol Metab. 2000;279(3):E539–45. doi: 10.1152/ajpendo.2000.279.3.E539. [DOI] [PubMed] [Google Scholar]
- 22.Johannsen DL, Knuth ND, Huizenga R, Rood JC, Ravussin E, Hall KD. Metabolic Slowing with Massive Weight Loss despite Preservation of Fat-Free Mass. J Clin Endocrinol Metab. 2012 doi: 10.1210/jc.2012-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall KD. Modeling Metabolic Adaptations and Energy Regulation in Humans. Annu Rev Nutr. 2012 doi: 10.1146/annurev-nutr-071811-150705. [DOI] [PubMed] [Google Scholar]
- 24.Becker BJ, Wu MJ. The synthesis of regression slopes in meta-analysis. Stat Sci. 2007;22(3):414–429. [Google Scholar]
- 25.Nelson J, Kennedy P. The Use (and Abuse) of Meta-Analysis in Environmental and Natural Resource Economics: An Assessment. Environmental and Resource Economics. 2009;42(3):345–377. [Google Scholar]
- 26.Bini LM, Coelho AS, Diniz-Filho JA. Is the relationship between population density and body size consistent across independent studies? A meta-analytical approach. Braz J Biol. 2001;61(1):1–6. doi: 10.1590/s0034-71082001000100002. [DOI] [PubMed] [Google Scholar]
- 27.Manning AK, LaValley M, Liu C-T, Rice K, An P, Liu Y, et al. Meta-analysis of gene-environment interaction: joint estimation of SNP and SNP × environment regression coefficients. Genetic Epidemiology. 2011;35(1):11–18. doi: 10.1002/gepi.20546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ros GH, Temminghoff EJM, Hoffland E. Nitrogen mineralization: a review and meta-analysis of the predictive value of soil tests. European Journal of Soil Science. 2011;62(1):162–173. [Google Scholar]
- 29.IOM. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) INSTITUTE OF MEDICINE OF THE NATIONAL ACADEMIES; Washington, D.C: 2005. [Google Scholar]
- 30.St-Onge MP, Gallagher D. Body composition changes with aging: the cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition. 2010;26(2):152–5. doi: 10.1016/j.nut.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Z, Heshka S, Heymsfield SB, Shen W, Gallagher D. A cellular-level approach to predicting resting energy expenditure across the adult years. Am J Clin Nutr. 2005;81(4):799–806. doi: 10.1093/ajcn/81.4.799. [DOI] [PubMed] [Google Scholar]
- 32.Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, Gortmaker SL, et al. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011;378(9793):826–37. doi: 10.1016/S0140-6736(11)60812-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwartz GE. Estimating the dimension of a model. Annals of Statistics. 1978;6(2):461–464. [Google Scholar]
- 34.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- 35.Molnar D, Jeges S, Erhardt E, Schutz Y. Measured and predicted resting metabolic rate in obese and nonobese adolescents. J Pediatr. 1995;127(4):571–7. doi: 10.1016/s0022-3476(95)70114-1. [DOI] [PubMed] [Google Scholar]
- 36.Lazzer S, Agosti F, De Col A, Sartorio A. Development and cross-validation of prediction equations for estimating resting energy expenditure in severely obese Caucasian children and adolescents. Br J Nutr. 2006;96(5):973–9. doi: 10.1017/bjn20061941. [DOI] [PubMed] [Google Scholar]
- 37.Lazzer S, Bedogni G, Lafortuna CL, Marazzi N, Busti C, Galli R, et al. Relationship between basal metabolic rate, gender, age, and body composition in 8,780 white obese subjects. Obesity (Silver Spring) 2010;18(1):71–8. doi: 10.1038/oby.2009.162. [DOI] [PubMed] [Google Scholar]
- 38.Garby L, Garrow JS, Jorgensen B, Lammert O, Madsen K, Sorensen P, et al. Relation between energy expenditure and body composition in man: specific energy expenditure in vivo of fat and fat-free tissue. Eur J Clin Nutr. 1988;42(4):301–5. [PubMed] [Google Scholar]
- 39.Sun M, Gower BA, Nagy TR, Trowbridge CA, Dezenberg C, Goran MI. Total, resting, and activity-related energy expenditures are similar in Caucasian and African-American children. Am J Physiol. 1998;274(2 Pt 1):E232–7. doi: 10.1152/ajpendo.1998.274.2.E232. [DOI] [PubMed] [Google Scholar]
- 40.Kaplan AS, Zemel BS, Stallings VA. Differences in resting energy expenditure in prepubertal black children and white children. J Pediatr. 1996;129(5):643–7. doi: 10.1016/s0022-3476(96)70143-9. [DOI] [PubMed] [Google Scholar]
- 41.DeLany JP, Bray GA, Harsha DW, Volaufova J. Energy expenditure in preadolescent African American and white boys and girls: the Baton Rouge Children's Study. Am J Clin Nutr. 2002;75(4):705–13. doi: 10.1093/ajcn/75.4.705. [DOI] [PubMed] [Google Scholar]
- 42.Bosy-Westphal A, Wolf A, Buhrens F, Hitze B, Czech N, Monig H, et al. Familial influences and obesity-associated metabolic risk factors contribute to the variation in resting energy expenditure: the Kiel Obesity Prevention Study. Am J Clin Nutr. 2008;87(6):1695–701. doi: 10.1093/ajcn/87.6.1695. [DOI] [PubMed] [Google Scholar]
- 43.Wren RE, Blume H, Mazariegos M, Solomons N, Alvarez JO, Goran MI. Body composition, resting metabolic rate, and energy requirements of short- and normal-stature, low-income Guatemalan children. Am J Clin Nutr. 1997;66(2):406–12. doi: 10.1093/ajcn/66.2.406. [DOI] [PubMed] [Google Scholar]
- 44.Bernstein RS, Thornton JC, Yang MU, Wang J, Redmond AM, Pierson RN, Jr, et al. Prediction of the resting metabolic rate in obese patients. Am J Clin Nutr. 1983;37(4):595–602. doi: 10.1093/ajcn/37.4.595. [DOI] [PubMed] [Google Scholar]
- 45.Huang KC, Kormas N, Steinbeck K, Loughnan G, Caterson ID. Resting metabolic rate in severely obese diabetic and nondiabetic subjects. Obes Res. 2004;12(5):840–5. doi: 10.1038/oby.2004.101. [DOI] [PubMed] [Google Scholar]
- 46.Javed F, He Q, Davidson LE, Thornton JC, Albu J, Boxt L, et al. Brain and high metabolic rate organ mass: contributions to resting energy expenditure beyond fat-free mass. Am J Clin Nutr. 2010;91(4):907–12. doi: 10.3945/ajcn.2009.28512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Piers LS, Soares MJ, McCormack LM, O'Dea K. Is there evidence for an age-related reduction in metabolic rate? J Appl Physiol. 1998;85(6):2196–204. doi: 10.1152/jappl.1998.85.6.2196. [DOI] [PubMed] [Google Scholar]
- 48.Welle S, Forbes GB, Statt M, Barnard RR, Amatruda JM. Energy-Expenditure under Free-Living Conditions in Normal-Weight and Overweight Women. Am J Clin Nutr. 1992;55(1):14–21. doi: 10.1093/ajcn/55.1.14. [DOI] [PubMed] [Google Scholar]
- 49.Foster GD, Wadden TA, Vogt RA. Resting energy expenditure in obese African American and Caucasian women. Obes Res. 1997;5(1):1–8. doi: 10.1002/j.1550-8528.1997.tb00276.x. [DOI] [PubMed] [Google Scholar]
- 50.Bronstein MN, Mak RP, King JC. Unexpected relationship between fat mass and basal metabolic rate in pregnant women. Br J Nutr. 1996;75(5):659–68. doi: 10.1079/bjn19960171. [DOI] [PubMed] [Google Scholar]
- 51.Soares MJ, Piers LS, O'Dea K, Collier GR. Plasma leptin concentrations, basal metabolic rates and respiratory quotients in young and older adults. Int J Obes Relat Metab Disord. 2000;24(12):1592–9. doi: 10.1038/sj.ijo.0801450. [DOI] [PubMed] [Google Scholar]
- 52.Nelson KM, Weinsier RL, Long CL, Schutz Y. Prediction of resting energy expenditure from fat-free mass and fat mass. Am J Clin Nutr. 1992;56(5):848–56. doi: 10.1093/ajcn/56.5.848. [DOI] [PubMed] [Google Scholar]
- 53.Ravussin E, Rising R. Daily Energy Expenditure in Humans: Measurements in a Respiratory Chamber and by Doubly Labeled Water. In: Kinney JMe., editor. Energy metabolism: tissue determinants and cellular corollaries. New York, NY: Raven; 1992. pp. 81–96. [Google Scholar]
- 54.Jensen MD, Braun JS, Vetter RJ, Marsh HM. Measurement of body potassium with a whole-body counter: relationship between lean body mass and resting energy expenditure. Mayo Clin Proc. 1988;63(9):864–8. doi: 10.1016/s0025-6196(12)62688-3. [DOI] [PubMed] [Google Scholar]
- 55.Heshka S, Yang MU, Wang J, Burt P, Pi-Sunyer FX. Weight loss and change in resting metabolic rate. Am J Clin Nutr. 1990;52(6):981–6. doi: 10.1093/ajcn/52.6.981. [DOI] [PubMed] [Google Scholar]
- 56.Weigle DS, Sande KJ, Iverius PH, Monsen ER, Brunzell JD. Weight loss leads to a marked decrease in nonresting energy expenditure in ambulatory human subjects. Metabolism. 1988;37(10):930–6. doi: 10.1016/0026-0495(88)90149-7. [DOI] [PubMed] [Google Scholar]
- 57.Pannemans DL, Westerterp KR. Energy expenditure, physical activity and basal metabolic rate of elderly subjects. Br J Nutr. 1995;73(4):571–81. doi: 10.1079/bjn19950059. [DOI] [PubMed] [Google Scholar]
- 58.Tataranni PA, Ravussin E. Variability in metabolic rate: biological sites of regulation. Int J Obes Relat Metab Disord. 1995;19(Suppl 4):S102–6. [PubMed] [Google Scholar]
- 59.Blanc S, Schoeller DA, Bauer D, Danielson ME, Tylavsky F, Simonsick EM, et al. Energy requirements in the eighth decade of life. Am J Clin Nutr. 2004;79(2):303–10. doi: 10.1093/ajcn/79.2.303. [DOI] [PubMed] [Google Scholar]
- 60.De Lorenzo A, Andreoli A, Bertoli S, Testolin G, Oriani G, Deurenberg P. Resting metabolic rate in Italians: relation with body composition and anthropometric parameters. Acta Diabetol. 2000;37(2):77–81. doi: 10.1007/s005920070023. [DOI] [PubMed] [Google Scholar]
- 61.Ferraro R, Lillioja S, Fontvieille AM, Rising R, Bogardus C, Ravussin E. Lower Sedentary Metabolic-Rate in Women Compared with Men. J Clin Invest. 1992;90(3):780–784. doi: 10.1172/JCI115951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hunter GR, Weinsier RL, Gower BA, Wetzstein C. Age-related decrease in resting energy expenditure in sedentary white women: effects of regional differences in lean and fat mass. Am J Clin Nutr. 2001;73(2):333–7. doi: 10.1093/ajcn/73.2.333. [DOI] [PubMed] [Google Scholar]
- 63.Ganpule AA, Tanaka S, Ishikawa-Takata K, Tabata I. Interindividual variability in sleeping metabolic rate in Japanese subjects. Eur J Clin Nutr. 2007;61(11):1256–61. doi: 10.1038/sj.ejcn.1602645. [DOI] [PubMed] [Google Scholar]
- 64.Gallagher D, Albu J, He Q, Heshka S, Boxt L, Krasnow N, et al. Small organs with a high metabolic rate explain lower resting energy expenditure in African American than in white adults. Am J Clin Nutr. 2006;83(5):1062–7. doi: 10.1093/ajcn/83.5.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fontvieille AM, Ferraro RT, Rising R, Larson DE, Ravussin E. Energy-Cost of Arousal - Effect of Sex, Race and Obesity. International Journal of Obesity. 1993;17(12):705–709. [PubMed] [Google Scholar]
- 66.Kunz I, Schorr U, Klaus S, Sharma AM. Resting metabolic rate and substrate use in obesity hypertension. Hypertension. 2000;36(1):26–32. doi: 10.1161/01.hyp.36.1.26. [DOI] [PubMed] [Google Scholar]
- 67.Nielsen S, Hensrud DD, Romanski S, Levine JA, Burguera B, Jensen MD. Body composition and resting energy expenditure in humans: role of fat, fat-free mass and extracellular fluid. Int J Obes Relat Metab Disord. 2000;24(9):1153–7. doi: 10.1038/sj.ijo.0801317. [DOI] [PubMed] [Google Scholar]
- 68.Wyatt HR, Grunwald GK, Seagle HM, Klem ML, McGuire MT, Wing RR, et al. Resting energy expenditure in reduced-obese subjects in the National Weight Control Registry. Am J Clin Nutr. 1999;69(6):1189–93. doi: 10.1093/ajcn/69.6.1189. [DOI] [PubMed] [Google Scholar]
- 69.Horie LM, Gonzalez MC, Torrinhas RS, Cecconello I, Waitzberg DL. New Specific Equation to Estimate Resting Energy Expenditure in Severely Obese Patients. Obesity (Silver Spring) 2011 doi: 10.1038/oby.2010.326. [DOI] [PubMed] [Google Scholar]
- 70.Weinsier RL, Nelson KM, Hensrud DD, Darnell BE, Hunter GR, Schutz Y. Metabolic Predictors of Obesity - Contribution of Resting Energy-Expenditure, Thermal Effect of Food, and Fuel Utilization to 4-Year Weight-Gain of Post-Obese and Never-Obese Women. J Clin Invest. 1995;95(3):980–985. doi: 10.1172/JCI117807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Luhrmann PM, Bender R, Edelmann-Schafer B, Neuhauser-Berthold M. Longitudinal changes in energy expenditure in an elderly German population: a 12-year follow-up. Eur J Clin Nutr. 2009;63(8):986–92. doi: 10.1038/ejcn.2009.1. [DOI] [PubMed] [Google Scholar]
- 72.Luhrmann PM, Edelmann-Schafer B, Neuhauser-Berthold M. Changes in resting metabolic rate in an elderly German population: cross-sectional and longitudinal data. J Nutr Health Aging. 2010;14(3):232–6. doi: 10.1007/s12603-010-0055-4. [DOI] [PubMed] [Google Scholar]
- 73.Piers LS, Shetty PS. Basal metabolic rates of Indian women. Eur J Clin Nutr. 1993;47(8):586–91. [PubMed] [Google Scholar]
- 74.Soares MJ, Francis DG, Shetty PS. Predictive equations for basal metabolic rates of Indian males. Eur J Clin Nutr. 1993;47(6):389–94. [PubMed] [Google Scholar]
- 75.Dellabianca P, Jequier E, Schutz Y. Lack of Metabolic and Behavioral Adaptations in Rural Gambian Men with Low Body-Mass Index. Am J Clin Nutr. 1994;60(1):37–42. doi: 10.1093/ajcn/60.1.37. [DOI] [PubMed] [Google Scholar]
- 76.Luke A, Rotimi CN, Adeyemo AA, Durazo-Arvizu RA, Prewitt TE, Moragne-Kayser L, et al. Comparability of resting energy expenditure in Nigerians and U.S. blacks. Obes Res. 2000;8(5):351–9. doi: 10.1038/oby.2000.42. [DOI] [PubMed] [Google Scholar]
- 77.Aleman-Mateo H, Salazar G, Hernandez-Triana M, Valencia ME. Total energy expenditure, resting metabolic rate and physical activity level in free-living rural elderly men and women from Cuba, Chile and Mexico. Eur J Clin Nutr. 2006;60(11):1258–65. doi: 10.1038/sj.ejcn.1602446. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.