Abstract
Attentional deficits are common and significant sequelae of pediatric traumatic brain injury (TBI). However, little is known about how the underlying neural processes that support different components of attention are affected. The present study examined brain activation patterns using fMRI in a group of young children who sustained a TBI in early childhood (n = 5; mean age = 9.4), and a group of age-matched control children with orthopedic injuries (OI) (n = 8) during a continuous performance task (CPT). Four children in the TBI group had moderate injuries, and one had a severe injury. Performance on the CPT task did not differ between groups. Both TBI and OI children activated similar networks of brain regions relevant to sustained attention processing, but the TBI group demonstrated several areas of significantly greater activation relative to controls, including frontal and parietal regions. These findings of over-activation of the relevant attention network in the TBI group contrast with those obtained in imaging studies of Attention-Deficit/Hyperactivity Disorder where under-activation of the attention network has been documented. This study provides evidence that young children’s brains function differently following a traumatic brain injury, and that these differences persist for years after the injury.
Keywords: Childhood brain disorder, Continuous performance test, Brain imaging, Children, Head injury, Neuropsychology
INTRODUCTION
Pediatric traumatic brain injury (TBI) results in substantial neurobehavioral morbidity for survivors, including persistent impairments in emotional, social, behavioral, and neuropsychological functioning that persist well beyond the acute phase of injury (e.g., Anderson et al., 2001, 2006; Taylor et al., 2002; Yeates et al., 2005). A clear relationship has been observed for physical and cognitive outcomes in TBI, with the severity of TBI contributing to greater impairment (Anderson et al., 2001, 2006; Catroppa &Anderson, 2005). The neuropathophysiology of TBI is complex, and often involves both focal and diffuse lesions, primary and secondary injuries to the brain, and acute as well as late effects (Polvishock & Katz, 2005). Focal lesions are most likely to occur in the frontal and temporal cortices because of their location near the anterior and middle fossa of the skull (Yeates, 2000). Shear-strain injuries in TBI occur at the boundaries between white and grey matter, most commonly near the basal ganglia, periventricular regions, superior cerebellar peduncles, fornices, corpus callosum, and brain stem (Yeates, 2000).
Although the neuroanatomical correlates of attention and TBI have not yet been established, it seems that there is some overlap in brain regions that are particularly vulnerable to injury in TBI and the structures believed to support attention (e.g., Mirsky et al., 1991; Rothbart & Posner, 2001). For example, Posner has delineated a three-component attention model in which different neural substrates support unique attentional processing networks (Rothbart & Posner, 2001). In this model, the executive attention network involves inhibitory control processes and suppression of prepotent responses and is subserved by the anterior cingulate, prefrontal cortex, and basal ganglia. The alerting network maintains arousal and involves the right frontal cortex, right parietal cortex, thalamus, and brain stem. Finally, the sensory-orienting network, responsible for covert orienting to sensory signals, is supported by the parietal lobes, temporoparietal junction, frontal eye fields, superior colliculus, and thalamus (Rothbart & Posner, 2001; for review see Max et al., 2005a).
Attention deficits are common and significant sequelae of pediatric TBI (Max et al., 2005b, 2005c). In general, children with severe TBI display poorer performance on a variety of measures of attention than less-severely injured or healthy control children across behavioral paradigms (e.g., Anderson et al., 1998, 2005; Catroppa & Anderson, 2005; Ewing-Cobbs et al., 1998; Yeates et al., 2005). Attention deficits adversely affect neurobehavioral outcomes and functional skills (Ganesalingam et al., 2006, 2007). More specifically, sustained attention, conceptualized as the capacity to maintain arousal and alertness towards a task over time (Mirsky et al., 1991), is believed to be integral in the regulation of cognitive resources needed for academic achievement, adaptive functioning, and social functioning (Dennis et al., 1995). Sustained attention is often measured using continuous performance tests (e.g., CPT; Rosvold et al., 1956), which assess the ability to maintain attention for critical but temporally infrequent events, presented in the absence of simultaneous distractors. Deficits in sustained attention, as measured by lower levels of performance or slower processing speed, have been reported in school-age children or adolescents with TBI compared to controls (e.g., Catroppa & Anderson, 1999; Dennis et al., 1995; Robin et al., 1999; Wassenberg et al., 2004) and also in children with severe TBI compared to children with mild to moderate TBI (e.g., Catroppa &Anderson, 2003). Finally, research also suggests that a TBI in a young child results in potentially more severe sequelae than for older children (Anderson et al., 2000). Children injured in early, compared to late, childhood perform worse on sustained attention tasks regardless of injury severity (Ewing-Cobbs et al., 1998), and preschool-aged children who sustain severe TBI are at risk for significant and long-term impairments in information processing speed and accuracy (Anderson et al., 2005).
With respect to functional neuroimaging (fMRI), several studies of TBI in adults have demonstrated alterations in brain activation patterns during performance of working memory tasks compared to controls. McAllister and colleagues (1999, 2001) documented differences in brain activation patterns between adults with mild TBI and controls during a working memory (N-back) task. Although task performance did not differ between groups across all conditions, adults with mild TBI demonstrated over-activation in the neural circuit mediating working memory shortly after the injury compared to healthy controls when the task was moderately difficult (McAllister et al., 1999, 2001). Similarly, three studies examining working memory in moderate to severely injured adults using versions of N-back tasks observed a more distributed representation of working memory in TBI patients compared to non-injured controls (Christodoulou et al., 2001; Perlstein et al., 2004; Scheibel et al., 2003). Newsome and colleagues (2007a) compared severely injured TBI patients to orthopedically-injured (OI) controls on an N-back task, and observed that TBI patients activated the same areas as OI patients, but tended to recruit these areas bilaterally or in the contralateral hemisphere. Scheibel and colleagues (2007) compared adults with moderate to severe TBI to OI controls on a stimulus-response compatibility task and observed that TBI patients had greater brain activation in several task-related brain regions during stimulus-response incompatibility compared to OI patients.
These imaging studies with adults suggest that the neural circuitry supporting working memory is altered after a brain injury, but it is unclear if this holds true for pediatric TBI and for additional cognitive domains. Two recent fMRI studies have investigated the neural correlates of cognitive processes in children with TBI. Karunanayaka and colleagues (2007) examined language processing using a verb generation task, and found that children with moderate to severe TBI had significantly greater activation in language-related brain areas compared to OI controls. Newsome and colleagues (2007b) used an N-back task to examine working memory, and observed greater brain activation in frontal and extrafrontal brain regions in children with moderate to severe TBI compared to noninjured children. Given these converging findings in both adult and pediatric TBI, one might anticipate similar results on a sustained attention task following pediatric TBI, with children with TBI evidencing over-activation in the attentional neural circuitry relative to OI controls.
The present study sought to examine brain activation using fMRI in a group of children with moderate to severe TBI and a comparison group of children with OI during a CPT. In this version, children were instructed to detect and respond to immediate repetition of any stimuli presented in a continuous stream. This form of CPT, termed Identical Pairs (CPT-IP), is an established measure of sustained attention (Borgaro et al., 2003; Cornblatt et al., 1988) that has been successfully adapted for fMRI and previously used with adolescents with bipolar disorder and Attention-Deficit/Hyperactivity Disorder (ADHD) (Adler et al., 2005; Strakowski et al., 2004). In contrast to the N-back tasks described earlier, the CPT-IP utilized here has a low memory load and slow presentation rate, which place higher demands on vigilance and sustained attention rather than working memory (Borgaro et al., 2003).
To our knowledge, no studies have yet examined the neural correlates of sustained attention in children with TBI. In this study, we sought to characterize the neural activation pattern engaged by sustained attention in young children with TBI compared to a control group of children with OI. The study is novel in its use of fMRI to examine the long-term consequences of early pediatric TBI on attention processing. In-scanner task performance data was collected in order to relate attentional functioning to brain activation patterns, and out of scanner neuropsychological testing performance and parent rating measures were collected to characterize the samples and validate the in-scanner task. We hypothesized that children with TBI and OI would activate similar brain regions during the task as identified in the previous studies of similar CPT tasks, but that the children with TBI would demonstrate an over-activation of brain regions supporting sustained attention compared to controls.
METHODS
This project was part of a larger ongoing study of child and family recovery from TBI and OI in young children entitled Child and Family Sequence of Preschool Brain Injury, (directed by S.L. Wade). The parent project employed a concurrent cohort/prospective research design involving repeated assessments of young children with TBI and young children with OI and their families, recruited from three tertiary care children’s hospitals in Ohio. Inclusion of a comparison group of children with OI allowed examination of the consequences of TBI relative to the functioning of a group of children likely to be similar in pre-injury behavior and family characteristics. Eligibility requirements for both groups included: injury requiring overnight hospitalization, age at injury between 36 to 84 months, and English as the primary spoken language in the home. Eligibility for the TBI group also included diagnosis of TBI and evidence of altered neurological status on the Glasgow Coma Scale (GCS) and/or abnormalities on imaging [MRI or computed tomography (CT) scan]. Children who sustained non-blunt head trauma (e.g., projectile wounds, strokes, drowning) were excluded. Inclusion in the OI group required a documented bone fracture (other than the skull) and the absence of any evidence of loss of consciousness or other findings suggestive of brain injury. Exclusion criteria for both groups included: previous history of TBI; pre-existing neurological disorder or medical problem affecting the central nervous system; diagnosis of mental retardation or developmental disability; documentation of child abuse as the cause of injury; and prior psychiatric disorder requiring hospitalization. The parent project and the imaging study reported here were approved by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center (CCHMC).
Participants
We contacted all children in the parent study at the CCHMC site who had sustained a TBI and who were at least six years of age and at least 12-months post injury regarding participation in the neuroimaging study. Potentially eligible children with OI were matched on time since injury, age, gender, ethnicity, and handedness with the TBI group. Fourteen children with TBI and 17 children with OI were identified from the parent project based on these criteria, and 23 (74%) consented to participate in the imaging study. This subset was representative of the larger parent sample on all demographic, injury-related, and neuropsychological variables.
Thirteen children successfully completed the CPT-IP protocol and were retained for analysis. Those excluded either had unusable data (due to excessive motion, defined as exceeding 0.75 voxel size for more than 25% of the functional data) or were unable to complete the imaging protocol because of time constraints or discomfort. Children who successfully completed the scanning procedures did not differ statistically, as verified by ANOVA, from those who failed to complete the scan or from the larger group of eligible children on any demographic, injury-related, or neuropsychological variables.
Table 1 provides the demographic information of participants included in the current report. The groups did not differ significantly in age, time since injury, sex, handedness, or maternal education level. Scans of the TBI participants taken at the time of injury were used to determine TBI severity. Consistent with previous studies (Fletcher et al., 1990), moderate severity was defined as a lowest GCS of 9–12, or a score of 13–15 accompanied by a skull fracture, mass lesion, or other indication of specific brain injury on CT or MRI; and severe TBI was defined as a lowest GCS score of 3–8. Using these criteria, one child had a severe TBI and four had moderate TBI.
Table 1.
Demographic and injury-related characteristics of participants
| ID | Age (yrs) |
Sex | Maternal education |
Injury mechanism |
Time since injury (yrs) |
GCS | Imaging at injury |
TBI severity |
|---|---|---|---|---|---|---|---|---|
| TBI_1 | 9.04 | F | 2 | Fall | 3.33 | 15 | Abnormal | Moderate |
| TBI_2 | 6.72 | M | 1 | Ped versus MVC | 3.08 | 9 | Abnormal | Moderate |
| TBI_3 | 6.93 | M | 4 | Fall | 2.50 | 14 | Abnormal | Moderate |
| TBI_4 | 8.33 | F | 5 | Fall | 1.75 | 9 | Abnormal | Moderate |
| TBI_5 | 6.90 | F | 2 | Fall | 1.25 | 3 | Abnormal | Severe |
| OI_1 | 7.34 | M | 2 | Fall | n/a | n/a | n/a | n/a |
| OI_2 | 8.70 | M | 2 | Fall | n/a | n/a | n/a | n/a |
| OI_3 | 6.47 | M | 4 | Fall | n/a | n/a | n/a | n/a |
| OI_4 | 9.10 | F | 2 | Sledding | n/a | n/a | n/a | n/a |
| OI_5 | 7.70 | M | 2 | Fall | n/a | n/a | n/a | n/a |
| OI_6 | 8.19 | F | 5 | Fall | n/a | n/a | n/a | n/a |
| OI_7 | 6.46 | M | 2 | Ped versus MVC | n/a | n/a | n/a | n/a |
| OI_8 | 7.32 | F | 3 | Furniture fell on leg | n/a | n/a | n/a | n/a |
Note. TBI = traumatic brain injury; OI = orthopedic injury; Ped versus MVC = pedestrian and motor vehicle collision. Maternal education level: 1 = 2 yrs high school; 2 = high school degree; 3 = 2 years college; 4 = 4 years college; 5 = graduate degree.
As part of the present study, current structural MRI scans were evaluated quantitatively by a pediatric neuroradiologist for focal abnormalities. All children with TBI had imaging findings that were consistent with the severity of injury. Positive imaging findings in three OI children likely represent incidental findings that are inconsistent with TBI sequelae and unlikely to affect the attentional networks examined in this study. Consequently, these participants were retained in the study.
Neuropsychological battery
To better characterize the sample, the following scores were drawn from the 12-month post-injury assessment of the parent project. The General Conceptual Ability (GCA) score on the Differential Ability Scales (DAS) provided an assessment of overall cognitive ability (Elliott, 1990). The Attention Focusing subscale of the Children’s Behavior Questionnaire (CBQ; Rothbart et al., 2001) and the attention deficit/hyperactivity problems subscale (ADHD subscale) of the Child Behavioral Check List (CBCL; Achenbach, 1991) are reported to describe the participants’ attentional functioning based on parent report. On the day of functional neuroimaging, two subtests of the Test of Every-day Attention for Children (TEA-Ch, Manly et al., 1999) battery were administered. The Sky Search subtest, which requires the child to find all of the matching pairs of ships in a visual array and circle them as quickly as they can, provided a test of selective attention. The Score! Subtest, which requires the child to listen to a series of tones presented at irregular intervals over approximately 12 minutes and count them silently, provided a measure of sustained attention. The TEA-Ch has established reliability and validity in assessing aspects of attention and executive functions, and has been used with pediatric TBI (Anderson et al., 1998; Manly et al., 2001).
Stimuli and behavioral tasks used for fMRI
Each participant underwent up to three functional scans during a single scanning session. The results of the additional scans/tasks are presented elsewhere (Karunanayaka et al., 2007).
The CPT paradigm employed here was modeled upon one used previously (Adler et al., 2005). Data from the CPT paradigm consisted of 10 (5 CPT and 5 control) alternating 33s blocks. Each block began with a 3s instruction followed by a 30s task period. During the task period, single digits (“0”, “9”, “3”, etc.) appeared one at a time centrally on the screen at the rate of one per second and participants were asked to press a button if and only if a number was repeated on two consecutive trials. The probability of a target appearing (i.e., repetition) was set to be one out of six, leading to an average of five targets per block. During the control period, the single digit “1” is shown at the rate of one per second, and participants were asked to press the button five times in a self-paced manner.
fMRI Data acquisition and analyses
Scans were performed on a 3T Siemens Trio MRI scanner. A T2*-weighted, spin-echo EPI sequence was used for fMRI scans (TR/TE = 3000/38 ms, FOV = 25.6 × 25.6 cm, matrix = 64 × 64, slice thickness = 4 mm). Thirty-six slices were acquired at 121 time points during the alternating 33-s task periods (i.e., control-experimental-control-experimental-control …) for a total imaging time of 363 s. The first 11 time points from the first control period were discarded to allow for T1 relaxation effects. A T1-weighted, 3D MP-RAGE whole brain scan was performed for anatomical co-registration (TR/TE = 2000/2.93 ms, FOV = 21.9 × 21.9 cm, matrix = 256 × 205, scan time = 230 s) prior to the functional scans.
fMRI image post-processing was done using in-house software written in IDL (Research Systems Inc., Boulder, Colorado, USA). The EPI images were corrected for geometrical distortion and Nyquist ghost artifacts using the multi-echo reference method (Schmithorst et al., 2001). The reconstructed EPI data were corrected for drift using quadratic baseline correction on a pixel-by-pixel basis (Hu et al., 1995; Le & Hu, 1996), co-registered to further reduce the effects of motion artifacts (Thevenaz & Unser, 1998), and transformed into Talairach coordinates (Talairach & Tournoux, 1988) using a linear affine transformation shown previously to be valid for individuals 5 to 18 years of age (Muzik & Chugani, 2000; Wilke et al., 2002).
For each participant, Pearson’s correlation coefficient between MR data and a boxcar reference waveform (33s-on-33s-off for 5 cycles, with a 6s delay to allow for the canonical hemodynamic response to peak) were computed pixel by pixel and then transformed into z-score maps using Fisher’s z-transformation. Group analyses were performed on these z-maps from individual subjects in the context of the random-effects General Linear Model (GLM). A post-processing filter (6 mm FWHM) was then applied before significant regions of activation on a voxel-by-voxel basis were identified (Worsley & Friston, 1995), generating a statistical parameter map. A clustering method was used for the adjustment of multiple comparisons (Xiong et al., 1995). In addition, Monte-Carlo simulation was used to determine the p-value corresponding to a certain combination of cluster size and z-threshold. For each cluster, the Talairach coordinates of the pixel that showed the maximum value within the cluster (i.e., the maxima) is reported.
RESULTS
Behavioral CPT Performance
Performance data from five TBI and six OI controls was recorded during the fMRI scans. Data from two participants in the OI group were lost because of computer malfunction. Mean hit rates (0.75 vs. 0.72), false alarm rates (0.003 vs. 0.003), and the corresponding A′ (0.94 vs. 0.93), a non-parametric measure of discrimination akin to d′, did not differ significantly between the TBI and OI groups, respectively.
Group comparisons of neuropsychological measures and their relationship with CPT A′
No significant group differences were found on any of the neuropsychological measures (see Table 2). Using a cutoff of two standard deviations above the mean on the CBCL ADHD subscale, no participant exceeded the symptom threshold for ADHD.
Table 2.
Group differences on in-scanner task and neuropsychological measures
| Mean (SD) | ANOVA | ||||
|---|---|---|---|---|---|
| TBI group | OI group | Mean square | F | p | |
| CPT task | |||||
| Hit rate | .753 (.286) | .716 (.236) | .004 | .057 | .817 |
| False alarm rate | .003 (.007) | .003 (.006) | .000 | .017 | .900 |
| Discriminability (A') | .937 (.072) | .927 (.058) | .000 | .051 | .827 |
| DAS: GCAa | 99.80 (19.75) | 102.88 (16.04) | 29.094 | .095 | .763 |
| TEA-Ch:Sky Search subtestb | 8.60 (5.55) | 7.88 (1.46) | 1.617 | .129 | .726 |
| TEA-Ch: Score! Subtestb | 12.80 (3.27) | 9.63 (3.96) | 31.017 | 2.235 | .163 |
| CBCL: ADHD subscalec | 57.20 (9.01) | 55.00 (6.63) | 14.117 | .240 | .635 |
| CBQ: Attention Focusingd | 4.41 (1.12) | 4.71 (.86) | .263 | .283 | .605 |
Note. DAS GCA = Differential Ability Scales General Conceptual Ability score; TEA-Ch = Test of Everyday Attention for Children; CBCL = Child Behavioral Checklist; CBQ = Child Behavior Questionnaire.
Standard Score,
Scaled Score,
T-score,
CBQ subscale score (mean of item scores).
Table 3 displays the first order Pearson correlation coefficients between A′ and other neuropsychological measures of attention after controlling for group status (TBI vs. OI), uncorrected for multiple comparisons. CBQ Attentional Focus and DAS GCA scores were each significantly correlated with A′ (r >.71). The TEA-ch subtests were not significantly correlated with A′, although the trend was in the expected direction.
Table 3.
First order linear inter-correlation between A' and neuropsychological measures, controlling for group status
| Sky search (TEA-Ch) |
Score! (TEA-Ch) |
CBQ attentional focusing |
DAS GCA |
||
|---|---|---|---|---|---|
| A' (CPT) | r | .484 | .557 | .716 | .732 |
| p | .157 | .094 | .020 | .016 | |
| Sky Search | r | — | .632 | .583 | .535 |
| (TEA-Ch) | p | — | .050 | .077 | .111 |
| Score! (TEA-Ch) | r | — | — | .464 | .278 |
| p | — | — | .177 | .437 | |
| CBQ Attentional | r | — | — | — | .509 |
| Focusing | p | — | — | — | .133 |
Note. DAS GCA = Differential Ability Scales General Conceptual Ability score; TEA-Ch = Test of Everyday Attention for Children; CBCL = Child Behavioral Checklist; CBQ = Child Behavior Questionnaire.
fMRI Analysis: overall effects and group comparison
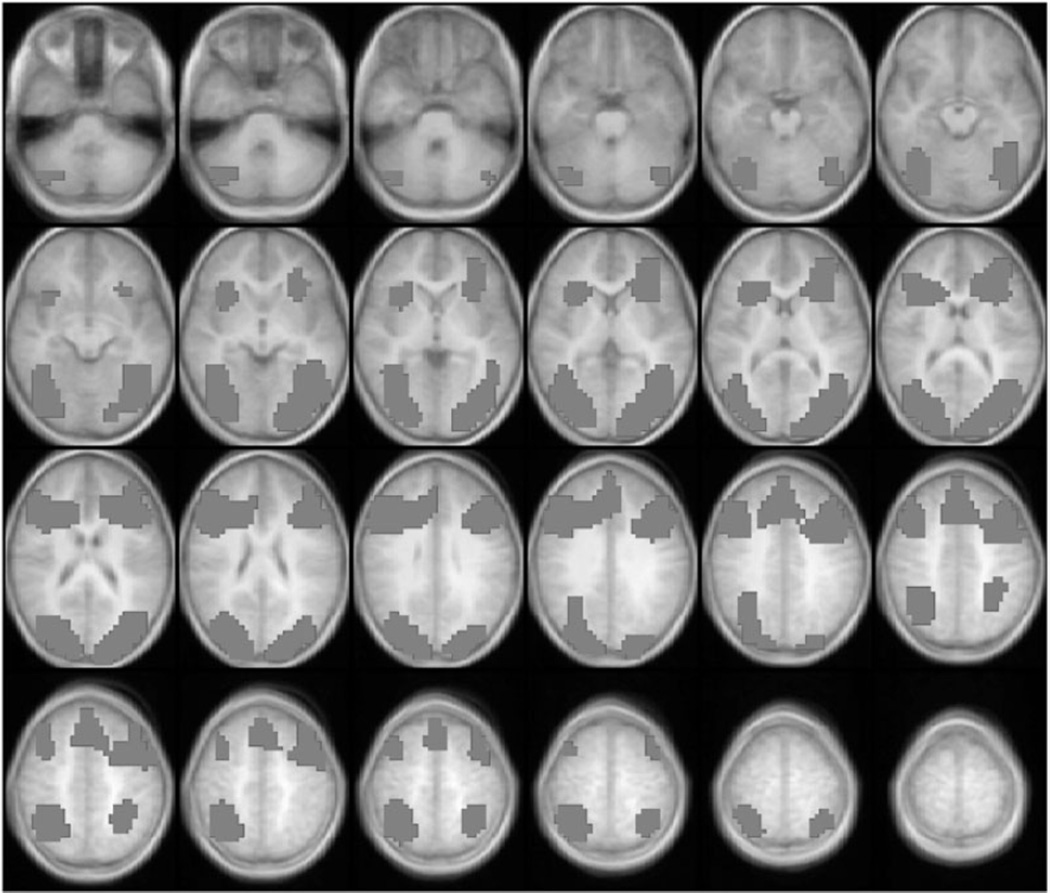
Figure 1 presents the statistical parametric map (composite Z-score map) of brain regions that were significantly activated during the CPT task compared to the control task in the entire sample. Significant activation was defined by a nominal z = 6.0, cluster = 20, corrected p ≤ .05 for multiple comparisons. A predominantly bilateral pattern of activation was seen in dorsolateral as well as ventrolateral prefrontal cortices, anterior cingulate, posterior parietal cortex, lingual and fusiform gyrus, and other occipital areas.
Fig. 1.
Brain activation map for the entire group of participants. Only positive activation foci (CPT > Control) are shown here. Images are horizontal slices 4 mm apart and start at z = −29 mm from the top left to z = +63 mm on the bottom right. Images are in radiological convention: left side of the images corresponds to the right hemisphere. Image parameters are as follows: nominal z = 6.0, cluster = 20, corrected p < .05 for multiple comparisons.
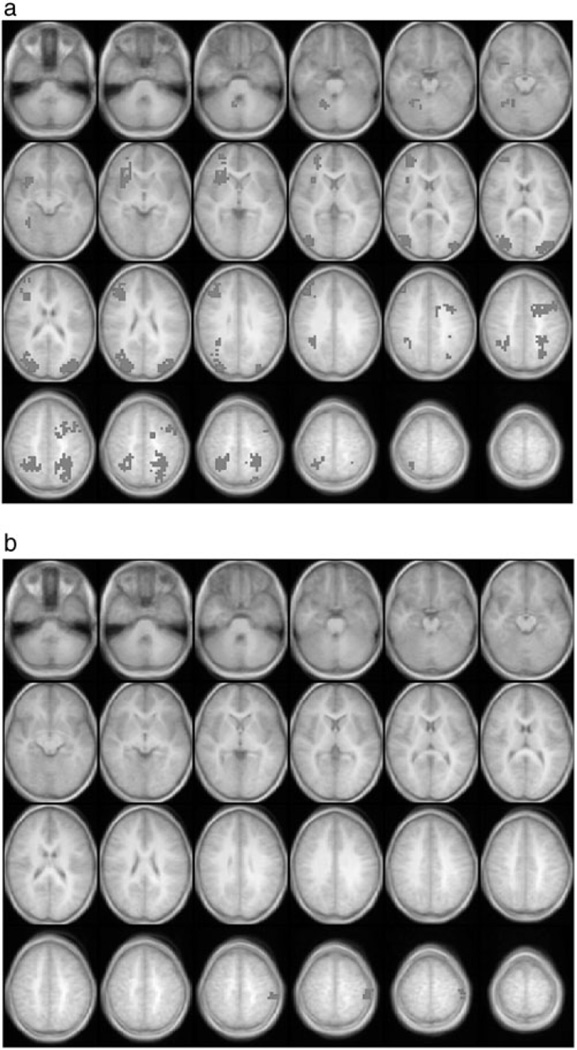
With respect to group-related differences (Table 4, Fig. 2a and 2b), participants in the TBI group had higher levels of activation in a variety of areas including right cerebellum, right lingual gyrus (BA 19), right insula, right inferior (BA 45, 47) and middle (BA 10) frontal gyrus, bilateral medial occipital gyrus (BA 19), bilateral superior frontal gyrus (BA 9, 46) with a strong right-sided asymmetry, mid-line cingulate gyrus, and wide extent of the precuneus bilaterally (BA 7). Participants in the OI group demonstrated greater activation in the primary somatosensory and motor cortex (BA 2/3 and BA 40). Re-examination of group differences in CPT-related brain activation using the nonparametric Spearman’s rho rank-order correlation yielded substantially similar findings to those found in the parametric analysis reported here.
Table 4.
Regions of interest showing significantly greater activation by group during the CPT task compared to control condition
| Region of interest | Brodmann’s areas |
Talairach coordinates |
||
|---|---|---|---|---|
| x | y | z | ||
| Children with TBI | ||||
| Middle frontal gyrus | ||||
| R | 9 | 42 | 31 | 31 |
| L | 9 | −46 | 27 | 27 |
| Middle frontal gyrus | ||||
| R | 46 | 38 | 27 | 19 |
| L | 46 | −38 | 27 | 23 |
| Middle and superior frontal gyrus (R) | 10 | 30 | 51 | 11 |
| Precentral gyrus (L) | 6/9 | −38 | 7 | 39 |
| Cingulate gyrus | ||||
| R | 23/24 | 2 | −29 | 27 |
| L | 23/24 | −2 | −9 | 27 |
| Cingulate gyrus (L) | 31 | −22 | −66 | 39 |
| Superior parietal lobe (R) | 7 | 30 | −49 | 59 |
| R | 7 | −22 | −49 | 43 |
| L | 7 | 26 | −49 | 43 |
| Middle occipital gyrus | ||||
| R | 19 | 34 | −81 | 15 |
| L | 19 | −34 | −81 | 15 |
| Fusiform gyrus | 37 | 26 | −49 | −9 |
| Cerebellum (R) | — | 18 | −49 | −17 |
| Orthopedic controls | ||||
| Postcentral gyrus | 2/3 | −46 | −25 | 55 |
| Inferior parietal lobe | 40 | −46 | −33 | 55 |
Fig. 2.
a (top) & b (bottom). Group differences in CPT-related brain activation. The TBI group had significantly higher levels of activation in a variety of brain regions relative to the OI group (top). In contrast, the OI group had higher levels of activation only in a confined region of left primary somatosensory/motor cortices (bottom). Image conventions and parameters are as in Figure 1.
fMRI Analysis: relationship with task performance
Eleven TBI and OI participants with performance data were included. This analysis identified brain regions across participants (n = 11) with activation levels positively correlated with A′, after controlling for group. Significant correlations were defined as an r-value of ≤.05, with a nominal z = 6.0, and a cluster size of 20 to control for multiple comparisons. As shown in Figure 3 and Table 5, activation in anterior cingulate was positively related to A′, as were activation in visual association areas (e.g., BA 19) and precuneus (BA 7) in the parietal region. Given the small sample size, the restricted range of A′ across all 11 children, and the fact that several in the TBI group performed very similarly on A′, we were unable to examine whether the relationship between task performance and brain activation differed depending on group status.
Fig. 3.
Statistical parametric map showing brain regions in which activation level was positively correlated with task performance (A′) after controlling for group status as a covariate. The 11 participants with A′ data were included in this analysis. Image conventions and parameters are as in Figure 1.
Table 5.
Regions of interest showing significant correlation between task performance and activation across groups
| Region of interest | Brodmann’s areas |
Talairach coordinates |
||
|---|---|---|---|---|
| x | y | z | ||
| Medial frontal gyrus | ||||
| R | 9 | 2 | 47 | 23 |
| L | 9 | −2 | 27 | 23 |
| Medial frontal gyrus | ||||
| R | 11 | 2 | 47 | −17 |
| L | 11 | −2 | 43 | −13 |
| Middle and superior frontal gyrus | ||||
| R | 10 | 2 | 51 | −9 |
| L | 10 | −2 | 51 | −9 |
| Inferior frontal gyrus (R) | 45 | 50 | 27 | 3 |
| Inferior frontal gyrus (R) | 47 | 50 | 27 | −1 |
| Precentral gyrus | 4 | −54 | −9 | 27 |
| Precentral gyrus | 6 | −54 | −5 | 31 |
| Anterior cingulate | ||||
| R | 32 | 2 | 43 | −5 |
| L | 32 | −2 | 43 | −5 |
| Superior temporal gyrus (R) | 38 | 42 | 15 | −25 |
| Superior temporal gyrus (L) | 39 | −46 | −57 | 27 |
| Superior temporal gyrus (L) | 22 | −46 | −53 | 19 |
| Superior parietal lobe | ||||
| R | 7 | 34 | −49 | 55 |
| L | 7 | −18 | −49 | 59 |
| Inferior parietal lobe (L) | 40 | −46 | −57 | 43 |
| Precuneus | ||||
| R | 7 | 18 | −81 | 43 |
| L | 7 | −10 | −81 | 43 |
| Cuneus | ||||
| R | 19 | 18 | −85 | 31 |
| L | 19 | −14 | −89 | 31 |
| Occipital gyrus | ||||
| R | 19 | 22 | −85 | 23 |
| L | 19 | −26 | −85 | 23 |
| Lingual gyrus (R) | 19 | 26 | −53 | 3 |
| Cerebellum (R) | — | 14 | −33 | −17 |
DISCUSSION
The findings from this study provide preliminary evidence that neural activation in children is altered following TBI during a task requiring sustained attention. Specifically, we found over-activation of parietal and frontal regions in children with TBI relative to OI controls. These findings are consistent with our hypotheses that children with TBI would activate similar networks of brain regions during the CPT as children with orthopedic injuries, but would demonstrate an over-activation of brain regions purported to support sustained attention. The findings are also consistent with the existing literature on CPT tasks and neural activation changes in adults after TBI. Taken together, the results suggest that neural activation may remain altered following TBI in young children who show good behavioral recovery.
This study demonstrates the feasibility and utility of assessing attention with fMRI in young children following TBI. The children with TBI successfully completed the scanning protocol and were equivalent to control children on CPT task performance. In-scanner performance was commensurate with performance on global neuropsychological measures, standardized attention measures, and parent rating scales of attention for both groups of children. This suggests that the CPT task used in-scanner is a valid measure of sustained attention for children with TBI. In addition, results such as ours highlight that when comparison groups demonstrate equivalent behavioral performance, the underlying neural mechanisms may still differ. By equating behavioral performance across groups, one can control for variability in performance that would otherwise confound the interpretation of any differences in brain activation patterns that are observed. Consequently, differences in brain activation patterns during the CPT-IP task can be interpreted to represent differences in neural mechanisms or characteristics (i.e. capacity or resource allocation) rather than performance parameters (i.e. accuracy or effort). Future fMRI studies may parametrically vary task difficulty to gain further insights into the response characteristics of the attentional networks in children with TBI.
The overall pattern of brain activation across groups was consistent with a previous study of sustained attention using the same CPT-IP task. Comparing Figure 1 of the present study to findings of Adler and colleagues (2005) in adolescents with bipolar disorder reveals activation in the same brain regions during the CPT task compared to the control task, including the bilateral dorsolateral and ventrolateral prefrontal cortex, anterior cingulate, posterior parietal cortex, lingual and fusiform gyrus, and other occipital areas.
We also found a pattern of over-activation of the relevant attention network in the parietal and frontal regions in children with TBI relative to controls. These findings are in direct contrast to those from fMRI investigations of the neural substrates of observed attention deficits in ADHD. This literature suggests that adolescents and adults with ADHD show reduced or under-activation of relevant neural circuits (Epstein, in press; Rubia et al., 2005; Smith et al., 2006; Tamm et al., 2006). Our findings of over-activation in regions related to sustained attention align more closely with fMRI studies of adult TBI using working memory tasks (McAllister et al., 2001; Scheibel et al., 2007), and recent fMRI studies of children with TBI (Karunanayaka et al., 2007; Newsome et al., 2007b), suggesting that observed attentional deficits in pediatric TBI and ADHD may not share a common underlying neuropathology. Nevertheless, some children with TBI develop significant inattention problems post-injury, often termed secondary ADHD (SADHD) (Max et al., 2005b, 2005c). Inattention appears to be a non-specific cognitive symptom that can result from a number of neuropathologies, and future studies examining the neural correlates in children with ADHD would be help clarify this issue.
Our findings are broadly consistent with other fMRI studies that observed altered, more extensive, neural activation patterns in patients with TBI (Christodoulou et al., 2001; McAllister et al., 1999, 2001; Newsome et al., 2007a, 2007b; Perlstein et al., 2004; Scheibel et al., 2003, 2007). For example, other studies also reported over-activation in regions mediating working memory (McAllister et al., 2001) or response inhibition (Scheibel et al., 2007) in adult patients with TBI. As in the McAllister study, we also detected no significant differences between groups in activation in the anterior cingulate, a region long believed to play a role in sustained attention, perhaps because performance in both studies was closely matched between groups (but see Newsome et al., 2007b). Regions in which higher levels of activation were related to working memory load for the adults with TBI compared to controls, specifically bilateral parietal and inferior and superior frontal areas (McAllister et al., 2001), also displayed higher levels of activation in children with TBI relative to their controls in the present study. However, children with TBI showed more activation in the ventrolateral prefrontal cortex predominantly on the right side compared to controls, a result not observed by McAllister and colleagues (2001). Finally, in this study, only two brain regions, confined to primary somatosensory and motor cortex (BA 2/3 and BA 40) were noted to have higher levels of CPT-related activation in children with OI relative to children with TBI.
Our findings are also consistent with a study investigating the neural substrates of language following pediatric TBI in an overlapping cohort of children with TBI and OI (Karunanayaka et al., 2007). A Verb Generation (VG) task, in which participants covertly generated as many verbs as possible, was used to assess language processing. Although both groups demonstrated similar networks of neural activation during the VG task, the TBI group had significantly greater activation in language-related areas than controls, specifically in the right superior temporal gyrus and the right middle temporal gyrus (Karunanayaka et al., 2007). This finding provided evidence that children with TBI may require additional neural resources to achieve comparable performance to children without neurological insults.
McAllister and colleagues (2001) suggested two possible neural mechanisms to explain the observed neural over-activation following TBI: differences in capacity or allocation of neural resources. Specifically, there may be a decrease in attentional capacity in children with TBI, rendering the CPT task more challenging, and hence more effortful, for these individuals to perform at behavioral levels comparable to controls. Activation in the bilateral posterior parietal regions as well as the right prefrontal regions may be specifically augmented in children with TBI as a compensatory mechanism. Alternatively, subtle deficits in frontal executive functions may have rendered the children with TBI less able to efficiently match available processing resources (which may be unimpaired) to the task demands. Consequently, they may over-commit processing resources to the CPT task without enhancing performance. The neural mechanisms proposed by McAllister and colleagues (2001) may differ only in very subtle ways, and future studies employing multiple conditions that vary in task difficulty are needed to distinguish them.
Although small sample size and restricted range of behavioral performance prohibited an analysis of whether the relationship between task performance and brain activation in specific regions changed depending on group status or injury severity, when compared across all participants, activation in the anterior cingulate, visual association areas (e.g., BA 19), and precuneus (BA 7) in the parietal region was positively related to task performance after controlling for group status. In contrast, Karunanayaka and colleagues (2007) found that increased activation in children with TBI relative to controls was associated with poorer behavioral performance. Similarly, in Scheibel and colleagues (2007), activation in the anterior cingulate and medial prefrontal cortex in the TBI group was unrelated to performance accuracy on the stimulus-response compatibility task. The authors suggest that this finding may represent an inefficient utilization of neural resources (Scheibel et al., 2007). Adler and colleagues (2005) reported that in adolescents with bipolar disorders but without comorbid ADHD, anterior cingulate activation correlated negatively with performance on a similar CPT task, and no correlation with performance was observed in anterior cingulate activation for adolescents with bipolar disorders with comorbid ADHD.
There is an inconsistency in these patterns of correlations across studies (and hence task paradigms), in that a higher level of brain activation is not always associated with higher skill level or proficiency. In the present study, although participants across groups showed a positive relationship between brain activation and performance, participants in the TBI group did not perform significantly better than participants in the OI group even though they showed more activation in a subset of brain regions (Fig. 2). Future studies with larger samples are needed to examine group differences in the relationship between activation level and behavioral performance in greater detail.
The present results must be considered preliminary in light of several methodological limitations. The sample was small and included mostly children with moderate TBI, thus findings may not generalize to the larger TBI population. In contrast to the literature, our sample did not demonstrate behavioral deficits in attention. However, the lack of behavioral differences in the groups allowed us to examine subtle effects of TBI on neural processing. Larger studies are needed to allow for better statistical control of demographic and injury-related confounding variables that were unable to be addressed here. Additional studies with other groups of children are also needed to determine the representativeness of our findings. It is possible that the finding of over-activation observed in this study and the Karunanayaka et al. (2007) study represents sample-specific characteristics.
Additionally, studies examining other aspects of attention processing will be valuable as children with TBI may demonstrate greater impairment on selective attention and/or divided attention tasks, and the neural networks supporting these processes may be differentially affected. Finally, future studies are needed to clarify both the short and long-term effects of TBI neural processing on other cognitive tasks besides attention, because of the possibility that TBI results in a generalized pattern of over-activation in the brain, rather than over-activation specific to attention processing. We found group differences in activation in some regions outside of the attentional network but were unable to determine if these areas are recruited as compensatory mechanisms for the attentional task or as part of a generalized pattern of over-activation.
The finding that neural activation is altered following pediatric TBI during tasks requiring sustained attention has promising clinical implications. Persistent changes in neural mechanisms years following early childhood TBI suggest that attention should continue to be assessed in the chronic phase of TBI. Moreover, insights from imaging studies such as ours will inform our understanding of attention deficits following pediatric TBI, thus facilitating the development of more effective and appropriate cognitive rehabilitation interventions.
ACKNOWLEDGMENTS
The authors thank Vincent Schmithorst, Ph.D. for programming consultation, and Caleb Adler, M.D. for use of the CPT-IP paradigm. This work was supported in part by (1) NIH grant RO1-HD044279 from the National Council on Medical Rehabilitation Research in the National Institute of Child Health and Human Development; (2) UPHS GCRC Grant #M01 RR 08084 from the National Center for Research Resources, NIH; (3) NIH grant RO1-HD044279 from the U.S. National Institute of Child Health and Human Development; and (4) NIH grant RO1-HD38578 from the US National Institute of Child Health and Human Development. Funding for the fMRI scans was provided by the Association of Volunteers of the Convalescent Hospital for Children, Cincinnati Children’s Hospital Medical Center. The first author was supported by a University Dean’s Distinguished Dissertation Award sponsored by the University of Cincinnati.
REFERENCES
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Adler CM, Delbello MP, Mills NP, Schmithorst V, Holland S, Strakowski SM. Comorbid ADHD is associated with altered patterns of neuronal activation in adolescents with bipolar disorder performing a simple attention task. Bipolar Disorders. 2005;7:577–588. doi: 10.1111/j.1399-5618.2005.00257.x. [DOI] [PubMed] [Google Scholar]
- Anderson VA, Catroppa C, Dudgeon P, Morse SA, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20:42–57. doi: 10.1037/0894-4105.20.1.42. [DOI] [PubMed] [Google Scholar]
- Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Recovery of intellectual ability following traumatic brain injury in childhood: Impact of injury severity and age at injury. Pediatric Neurosurgery. 2000;32:282–290. doi: 10.1159/000028956. [DOI] [PubMed] [Google Scholar]
- 5.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Outcome from mild head injury in young children: A prospective study. Journal of Clinical and Experimental Neuropsychology. 2001;23:705–717. doi: 10.1076/jcen.23.6.705.1015. [DOI] [PubMed] [Google Scholar]
- Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Attentional and processing skills following traumatic brain injury in early childhood. Brain Injury. 2005;19:699–710. doi: 10.1080/02699050400025281. [DOI] [PubMed] [Google Scholar]
- Anderson V, Fenwick T, Manly T, Robertson I. Attentional skills following traumatic brain injury in childhood: A componential analysis. Brain Injury. 1998;12:937–949. doi: 10.1080/026990598121990. [DOI] [PubMed] [Google Scholar]
- Borgaro S, Pogge DL, DeLuca VA, Bilinger L, Stokes J, Harvey PD. Convergence of different versions of the continuous performance test: Clinical and scientific implications. Journal of Clinical and Experimental Neuropsychology. 2003;25:283–292. doi: 10.1076/jcen.25.2.283.13646. [DOI] [PubMed] [Google Scholar]
- Catroppa C, Anderson V. Attentional skills in the acute phase following pediatric traumatic brain injury. Child Neuropsychology. 1999;5:251–264. doi: 10.1076/0929-7049(199912)05:04;1-R;FT251. [DOI] [PubMed] [Google Scholar]
- Catroppa C, Anderson V. Children’s attentional skills 2 years post-traumatic brain injury. Developmental Neuropsychology. 2003;23:359–373. doi: 10.1207/S15326942DN2303_3. [DOI] [PubMed] [Google Scholar]
- Catroppa C, Anderson V. A prospective study of the recovery of attention from acute to 2 years following pediatric traumatic brain injury. Journal of the International Neuropsychological Society. 2005;11:84–98. doi: 10.1017/S1355617705050101. [DOI] [PubMed] [Google Scholar]
- Christodoulou C, Deluca J, Ricker JH, Madigan NK, Bly BM, Lange G, Kalnin AJ, Liu W-C, Steffner J, Diamond BJ, Ni AC. Functional magnetic resonance imaging of working memory impairment after traumatic brain injury. Journal of Neurology, Neurosurgery and Psychiatry. 2001;71:161–168. doi: 10.1136/jnnp.71.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornblatt BA, Risch NJ, Faris G, Friedman D, Erlenmeyer-Kimling L. The Continuous Performance Test, Identical Pairs version (CPT-IP): I, New findings about sustained attention in normal families. Psychiatry Research. 1988;29:65–68. doi: 10.1016/0165-1781(88)90076-5. [DOI] [PubMed] [Google Scholar]
- Dennis M, Wilkinson M, Koski L, Humphreys RP. Attention deficits in the long term after childhood head injury. In: Broman SH, Michel ME, editors. Traumatic head injury in children. New York: Oxford University Press; 1995. pp. 165–187. [Google Scholar]
- Elliott CD. Differential ability scales: Introductory and technical handbook. San Antonio, TX: The Psychological Corporation; 1990. [Google Scholar]
- Epstein JN. A pathophysiology of attention deficit hyperactivity disorder: Clues from neuroimaging. In: Rumsey J, Ernst M, editors. Neuroimaging in Developmental Clinical Neuroscience. (in press). [Google Scholar]
- Ewing-Cobbs L, Prasad M, Fletcher JM, Levin HS, Miner ME, Eisenberg HM. Attention after pediatric traumatic brain injury: A multidimensional assessment. Child Neuropsychology. 1998;4:35– 48. [Google Scholar]
- Fletcher JM, Ewing-Cobbs L, Miner M, Levin HS, Eisenberg HM. Behavioral changes after closed head injury in children. Journal of Consulting and Clinical Psychology. 1990;58:93–98. doi: 10.1037//0022-006x.58.1.93. [DOI] [PubMed] [Google Scholar]
- Ganesalingam K, Sanson A, Anderson V, Yeates KO. Self-regulation and social and behavioral functioning following childhood traumatic brain injury. Journal of the International Neuropsychological Society. 2006;12:609–621. doi: 10.1017/S1355617706060796. [DOI] [PubMed] [Google Scholar]
- Ganesalingam K, Sanson A, Anderson V, Yeates KO. Self-regulation as a mediator of the effects of childhood traumatic brain injury on social and behavioral functioning. Journal of the International Neuropsychological Society. 2007;13:298–311. doi: 10.1017/S1355617707070324. [DOI] [PubMed] [Google Scholar]
- Hu X, Le TH, Parrish T, Erhard P. Retrospective estimation and correction of physiological fluctuation in functional MRI. MRM. 1995;34:201–212. doi: 10.1002/mrm.1910340211. [DOI] [PubMed] [Google Scholar]
- Karunanayaka P, Holland S, Yuan W, Altaye M, Jones BV, Michaud L, Walz NC, Wade SL. Neural substrate differences in language networks and associated language-related behavioral impairments in children with TBI: A preliminary fMRI investigation. Neuro Rehabilitation. 2007;22:355–369. [PMC free article] [PubMed] [Google Scholar]
- Le TH, Hu X. Retrospective estimation and correction of physiological artifacts in fMRI by direct extraction of physiological activity from MR data. MRM. 1996;35:290–298. doi: 10.1002/mrm.1910350305. [DOI] [PubMed] [Google Scholar]
- Manly T, Anderson V, Nimmo-Smith I, Turner A, Watson P, Robertson I. The differential assessment of children’s attention: The Test of Everyday Attention for Children (TEA-Ch), normative sample and ADHD performance. Journal of Child Psychology & Psychiatry. 2001;42:1065–1081. doi: 10.1111/1469-7610.00806. [DOI] [PubMed] [Google Scholar]
- Manly T, Robertson IH, Anderson C, Nimmo-Smith I. TEACH: The Test of Everyday Attention for Children. Bury St. Edmunds, UK: Thames Valley Test Co.; 1999. [Google Scholar]
- Max JE, Manes FF, Robertson BAM, Mathews K, Fox PT, Lancaster J. Prefrontal and executive attention network lesions and the development of Attention-Deficit/Hyperactivity symptomatology. Journal of the American Academy of Child and Adolescent Psychiatry. 2005a;44:443–450. doi: 10.1097/01.chi.0000156661.38576.0f. [DOI] [PubMed] [Google Scholar]
- Max JE, Schachar RJ, Levin HS, Ewing-Cobbs L, Chapman SB, Dennis M, Saunders A, Landis J. Predictors of attention-deficit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. Journal of the American Academy of Child & Adolescent Psychiatry. 2005b;44:1032–1040. doi: 10.1097/01.chi.0000173293.05817.b1. [DOI] [PubMed] [Google Scholar]
- Max JE, Schachar RJ, Levin HS, Ewing-Cobbs L, Chapman SB, Dennis M, Saunders M, Landis J. Predictors of secondary attention-deficit/hyperactivity disorder in children and adolescents 6 to 24 months after traumatic brain injury. Journal of the American Academy of Child & Adolescent Psychiatry. 2005c;44:1041–1049. doi: 10.1097/01.chi.0000173292.05817.f8. [DOI] [PubMed] [Google Scholar]
- McAllister TW, Saykin AJ, Flashman LA, Sparling MB, Johnson SC, Guerin SJ, Mamourian AC, Weaver JB, Yanofsky N. Brain activation during working memory 1 month after mild traumatic brain injury: A functional MRI study. Neurology. 1999;53:1300–1308. doi: 10.1212/wnl.53.6.1300. [DOI] [PubMed] [Google Scholar]
- McAllister TW, Sparling MB, Flashman LA, Guerin SJ, Mamourian AC, Saykin AJ. Differential working memory load effects after mild traumatic brain injury. Neuroimage. 2001;14:1004–1012. doi: 10.1006/nimg.2001.0899. [DOI] [PubMed] [Google Scholar]
- Mirsky AF, Anthony BJ, Duncan CC, Ahern MB, Kellam SG. Analysis of the elements of attention: A neuropsychological approach. Neuropsychology Review. 1991;2:109–145. doi: 10.1007/BF01109051. [DOI] [PubMed] [Google Scholar]
- Muzik O, Chugani DC. Statistical parametric mapping: Assessment of application in children. NeuroImage. 2000;12:538–549. doi: 10.1006/nimg.2000.0651. [DOI] [PubMed] [Google Scholar]
- Newsome MR, Scheibel RS, Hunter JV, Wang ZJ, Chu Z, Li X, Levin HS. Brain activation during working memory after traumatic brain injury in children. Neurocase. 2007b;13:16–24. doi: 10.1080/13554790601186629. [DOI] [PubMed] [Google Scholar]
- Newsome MR, Scheibel RS, Steinberg JL, Troyanskaya M, Sharma RG, Rauch RA, Li X, Levin HS. Working memory brain activation following severe traumatic brain injury. Cortex. 2007a;43:95–111. doi: 10.1016/s0010-9452(08)70448-9. [DOI] [PubMed] [Google Scholar]
- Perlstein WM, Cole MA, Demery JA, Seignourel PJ, Dixit NK, Larson MJ, Briggs RW. Parametric manipulation of working memory load in traumatic brain injury: Behavioral and neural correlates. Journal of the International Neuropsychological Society. 2004;10:724–741. doi: 10.1017/S1355617704105110. [DOI] [PubMed] [Google Scholar]
- Polvishock JT, Katz DI. Update of neuropathology and neurological recovery after traumatic brain injury. Journal of Head Trauma Rehabilitation. 2005;20:76–94. doi: 10.1097/00001199-200501000-00008. [DOI] [PubMed] [Google Scholar]
- Robin DA, Max JE, Stierwalt JAG, Guenzer LC, Lindgren SD. Sustained attention in children and adolescents with traumatic brain injury. Aphasiology. 1999;13:701–708. [Google Scholar]
- Rosvold HE, Mirsky AF, Sarason I, Bransome E, Beck L. A continuous performance test of brain damage. Journal of Consulting Psychology. 1956;20:343–350. doi: 10.1037/h0043220. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The Children’s Behavior Questionnaire. Child Development. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Posner MI. Mechanism and variation in the development of attentional networks. In: Nelson CA, Luciana M, editors. Handbook of Developmental Cognitive Neuroscience. Cambridge, MA: The MIT Press; 2001. pp. 353–363. [Google Scholar]
- Rubia K, Smith AB, Brammer MJ, Toone B, Taylor E. Abnormal brain activation during inhibition and error detection in medication-naive adolescents with ADHD. American Journal of Psychiatry. 2005;162:1067–1075. doi: 10.1176/appi.ajp.162.6.1067. [DOI] [PubMed] [Google Scholar]
- Scheibel RS, Newsome MR, Steinberg JL, Pearson DA, Rauch RA, Mao H, Troyanskaya M, Sharma RG, Levin HS. Altered brain activation during cognitive control in patients with moderate to severe traumatic brain injury. Neurorehabilitation and Neural Repair. 2007;21:36–45. doi: 10.1177/1545968306294730. [DOI] [PubMed] [Google Scholar]
- Scheibel RS, Pearson DA, Faria LP, Kotrla KJ, Aylward E, Bachevalier J, Levin HS. An fMRI study of executive functioning after severe diffuse TBI. Brain Injury. 2003;17:919–930. doi: 10.1080/0269905031000110472. [DOI] [PubMed] [Google Scholar]
- Schmithorst VJ, Dardzinski BJ, Holland SK. Simultaneous correction of ghost and geometric distortion artifacts in EPI using a multiecho reference scan. IEEE Transactions on Medical Imaging. 2001;20:535–539. doi: 10.1109/42.929619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AB, Taylor E, Brammer M, Toone B, Rubia K. Task-specific hypoactivation in prefrontal and temporoparietal brain regions during motor inhibition and task switching in medication-naive children and adolescents with attention deficit hyperactivity disorder. American Journal of Psychiatry. 2006;163:1044–1051. doi: 10.1176/ajp.2006.163.6.1044. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, Adler CM, Holland SK, Mills N, Del-Bello MP. A preliminary fMRI study of sustained attention in authymic, unmedicated bipolar disorder. Neuropsychopharmacology. 2004;29:1734–1740. doi: 10.1038/sj.npp.1300492. [DOI] [PubMed] [Google Scholar]
- Talairach J, Tournoux P. Coplanar stereotactic atlas of the human brain. New York: Thieme; 1988. [Google Scholar]
- Tamm L, Menon V, Reiss AL. Parietal attentional system aberrations during target detection in adolescents with attention deficit hyperactivity disorder: Event-related fMRI evidence. American Journal of Psychiatry. 2006;163:1033–1043. doi: 10.1176/ajp.2006.163.6.1033. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Thevenaz P, Unser M. A pyramid approach to subpixel registration based on intensity. IEEE Transactions on Image Processing. 1998;7:27–41. doi: 10.1109/83.650848. [DOI] [PubMed] [Google Scholar]
- Wassenberg R, Max JE, Lindgren SD, Schatz A. Sustained attention in children and adolescents after traumatic brain injury: Relation to severity of injury, adaptive functioning, ADHD and social background. Brain Injury. 2004;18:751–764. doi: 10.1080/02699050410001671775. [DOI] [PubMed] [Google Scholar]
- Wilke M, Schmithorst VJ, Holland SK. Assessment of spatial normalization of whole-brain magnetic resonance images in children. Human Brain Mapping. 2002;17:48–60. doi: 10.1002/hbm.10053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worsley KJ, Friston KJ. Analysis of fMRI time-series revisited–Again. NeuroImage. 1995;2:173–181. doi: 10.1006/nimg.1995.1023. [DOI] [PubMed] [Google Scholar]
- Xiong J, Gao JH, Lancaster JL, Fox PT. Clustered pixels analysis for functional MRI activation studies of the human brain. Human Brain Mapping. 1995;3:287–301. [Google Scholar]
- Yeates KO. Closed-head injury. In: Yeates KO, Ris MD, Taylor HG, editors. Pediatric neuropsychology: Research, theory, and practice. New York: Guilford Press; 2000. [Google Scholar]
- Yeates KO, Armstrong K, Janusz J, Taylor HG, Wade S, Stancin T, Drotar D. Long-term attention problems in children with traumatic brain injury. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:574–584. doi: 10.1097/01.chi.0000159947.50523.64. [DOI] [PubMed] [Google Scholar]