Abstract
Objective. To study the effects of a health check by a nurse alone or combined with an exercise intervention in middle-aged men at increased cardiovascular risk. Design. A randomized controlled trial. Setting and intervention. Primary care in Kirkkonummi municipality with 36 000 inhabitants. A health check by a nurse alone or combined with an exercise intervention to controls with no intervention was compared. Subjects. A total of 168 men aged 35 to 45 years with at least two cardiovascular risk factors and physical activity (PA) frequency < 3 times a week. Main outcome measures. Metabolic syndrome (MetS) as defined by International Diabetes Federation/American Heart Association and self-reported PA frequency. Results. Overall, focusing on health increased physical activity frequency in middle-aged men. After one year, 19% had increased PA to ≥ 3 times a week (95% CI 12–26). All study groups increased PA to ≥ 3 times: 26% of men in the exercise intervention group, 15% of men in the health check group, and 16% of controls. The differences between the groups were not statistically significant. The intervention did not have any meaningful impact on MetS or other cardiovascular outcomes at one-year follow up. Conclusions. Physical activity increased in all study groups of middle-aged men in this health-promotion trial. The interventions had no effect on metabolic syndrome or other cardiovascular outcomes in the participants. The trial increased awareness and collaboration in physical activity promotion among municipal health care and exercise services.
Key Words: Cardiovascular risk, exercise intervention, Finland, general practice, health check, metabolic syndrome
It is known that promotion of physical activity in primary care to sedentary adults leads to a small to medium improvement in self-reported physical activity at 12 months.
A 19% increase was observed at one year in overall self-reported physical activity in middle-aged men who participated in a health-promotion trial.
The change in physical activity did not have an effect on the health outcomes at one-year follow-up.
The trial had community effects: groups of men continued exercising together and the trial increased collaboration between health and exercise services in the municipality.
Introduction
Middle-aged men start to present symptoms of metabolic syndrome (MetS), which makes them a relevant target for health promotion. In Finland, the North Karelia project focused mostly on nutrition and serves as a model of an effective health-promotion intervention to reduce cardiovascular risk [1]. Nowadays, a sedentary lifestyle has become prevalent and it appears that increasing physical activity (PA) may be one of the most effective means to control cardiovascular risk.
The positive effects of PA are well studied: it promotes weight loss [2], especially when combined with dietary changes, it decreases the incidence of type 2 diabetes mellitus in high-risk groups [3], improves the MetS in general [4], and reduces HbA1c levels in patients with type 2 diabetes [5]. The challenge is that people do not adhere to PA recommendations. The main reasons for this in the middle-aged include economic factors, lack of time, and low motivation [6].
Although the effectiveness of such interventions on morbidity may now be questionable [7], there was a trend in Finland to conduct health checks for 40-year-old men to improve their lifestyle habits. Also in Kirkkonummi municipality, the health care policy-makers wanted to commence a programme of health checks. However, in addition to health checks we were able to start a randomized controlled trial studying the effectiveness of health checks alone or in combination with an exercise intervention.
Because an individual approach may not be sufficient for lifestyle changes, we added a group-based exercise intervention to the trial. This was especially important as Kirkkonummi is a commuter town in the Helsinki area where most inhabitants move to work in the capital region and as a result of this men end up lacking their natural groups of peers for exercise. Therefore, as one of the community targets with this trial we aimed to establish groups of men exercising together. We also wanted to create cooperation between the health centre and other municipal activities, such as adult education and exercise services in health promotion.
Although there is evidence for the effects of exercise plus diet in individuals already presenting with impaired glucose tolerance [3] and other clinical manifestations [4,5], there is still a need for studies on exercise alone in primary health care targeted at risk groups. Our aim was to target the risk group of middle-aged men with cardiovascular risk factors with two interventions: health checks and an exercise intervention, and to study the effects in a randomized controlled trial. In this paper, we present the findings of the trial with regard to its main outcomes: metabolic syndrome and physical activity.
Material and methods
General design
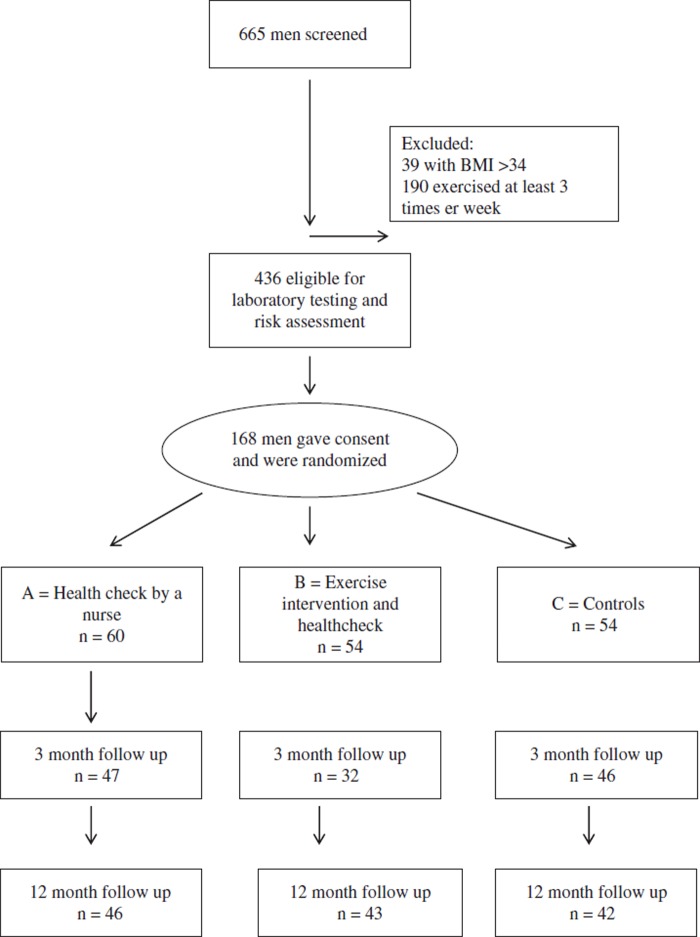
We planned a three-armed one-centre randomized controlled trial (see Figure 1). The methods have been described in detail earlier (8). Men were recruited by three methods: by invitation letters to 40-year-olds, by mass media and local campaigning, and by targeted recruiting in the health services. After screening and randomization, the first study arm received a 1½-hour health check intervention by a public health nurse. The second intervention arm received, in addition to the health check, a guided group exercise intervention of 12 weeks. The third group served as a control group, and men in this group had the opportunity to participate in the health checks and exercise interventions after one year.
Figure 1.
Participant flow diagram.
Participants
Inclusion criteria were predefined as follows: men aged 35 to 45 with at least two cardiovascular risk factors. These included BMI 27–34 kg/m2, waist circumference > 94 cm, fasting glucose > 6.1 mmol/l, total plasma cholesterol > 5.0 mmol/l, LDL-cholesterol > 3.0 mmol/l, triglycerides > 2.0 mmol/l, systolic blood pressure > 140 mmHg, diastolic blood pressure > 90 mmHg and currently either smoking or on cholesterol-lowering or blood pressure-lowering medication.
Exclusion criteria were as follows: BMI over 34 (or any other physical barrier preventing participation in the exercise intervention) or active exerciser (exercising for at least 30 minutes three times a week or more) or having an immediate health problem requiring treatment or a severe risk factor, for example, recently diagnosed or uncontrolled type I diabetes, or symptomatic coronary artery disease.
Randomization
Once the men had consented to participate in the study and the baseline measurements were carried out, they were randomly allocated to one of the three study groups. A randomization list based on random numbers was made and transferred to sequentially numbered, sealed envelopes. The study coordinator (SF) opened the envelopes in numbered order and informed participants of their study arm and procedures.
Study interventions
Health check intervention by a nurse
Public health nurses used standard practices in their health-promotion intervention. Prior to the onset of the trial, they attended a training session arranged by the Finnish Heart Association. In their interventions, the nurses used the type 2 diabetes disease risk assessment form (Finnish Diabetes Association) [9], and the cardiovascular risk assessment chart (the Finnish Heart Association). The intervention included assessments of individual risks, dietary habits, PA, and a motivational talk about these habits. The intervention lasted up to 90 minutes and did not include a follow-up.
Exercise intervention
In addition to the health checks, the second intervention group was also invited to a group exercise intervention. The size of these groups varied from 10 to 20 people. The exercise intervention group met once a week and was guided by a physical education counsellor and consisted of various types of basic physical training. The exercise sessions lasted 60 minutes each. During the 12 weekly meetings several safe exercise activities of at least moderate intensity were introduced, such as Nordic walking, fitness circle, volleyball, swimming, circuit training, gym, boxing, zumba, etc.
In addition to the study interventions, all groups received, if necessary, standard treatment at Kirkkonummi Health Centre, a municipal public primary care unit. If a participant showed any need of medical treatment, or his medications required medical attention, he was referred to a primary care physician.
Outcome measures
The outcomes were measured after three and 12 months of the randomization. The blood tests were taken at months 0, 3, and 12. Other outcomes were measured by Internet surveys and, if the participant did not respond, by telephone surveys.
We had two primary outcome measures. First, MetS as defined by the International Diabetes Federation/American Heart Association [10], i.e. checking whether three or more of the following criteria were fulfilled: (i) systolic blood pressure ≥ 130 or diastolic blood pressure ≥ 85 or specific medication; (ii) triglycerides ≥ 1.7 mmol/L or specific medication; (iii) HDL cholesterol < 1.0 mmol/L or specific medication; (iv) fasting plasma glucose ≥ 5.6 mmol/L or specific medication; or (v) waist circumference > 94 cm. We chose metabolic syndrome as our main outcome measure as we expected that in this group of men with elevated cardiovascular risk it could be modified by our interventions.
The second primary outcome measure was self-reported PA assessed by asking how many times per week a participant performed any exercise that induced sweating and got the person at least slightly out of breath, i.e. was at least of moderate intensity, for at least 30 minutes.
Statistical analyses
The results are expressed as proportions or means and standard deviations (SD). Statistical comparisons between the groups with continuous variables in baseline characteristics were performed using analysis of variance or the Kruskall-Wallis test and with a chi-squared test or Fisher's exact test for dichotomous variables. The differences between groups in PA and MetS were tested by using bootstrap techniques. Bootstrapping is a re-sampling method, in which no assumptions on distribution are made [11]. The α-level was set at 0.05. All statistical analyses were performed using STATA (for Windows), version 10 (Stata Corp, College Station, TX, USA).
Results
Three age cohorts were invited to the study, the 1969 born (n = 313 and 122 responded), the 1970 born (n = 330 and 110 responded), and the 1971 born (n = 303 and 88 responded). Overall, 320 of 946 invited men (34%) responded and participated in the screening. An additional 345 men became interested in the trial via the mass media, campaigning, or targeted invitations. Between 2009 and 2011, a total of 665 men aged between 35 and 45 years responded to the screening questionnaire of the trial. The participant flow diagram is presented in Figure 1. After laboratory testing and risk assessment, altogether 168 men consented and were randomized into the trial. The baseline characteristics of the men are presented in Table I.
Table I.
Baseline participant characteristics: mean (and standard deviation).
| All (n = 168) | Health check (n = 60) | Exercise intervention (n = 54) | Controls (n = 54) | P1 | |
| Mean age, years (SD) | 40.3 (2.9) | 40.2 (2.5) | 40.4 (2.8) | 40.3 (3.5) | 0.95 (NS) |
| Weight, kg (SD) | 88.4 (11.9) | 89.3 (12.9) | 89.6 (11.1) | 86.2 (11.4) | 0.26 (NS) |
| Height, cm (SD) | 180.8 (6.4) | 181.3 (6.6) | 180.5 (6.3) | 180.7 (6.2) | 0.79 (NS) |
| Waist circumference, cm (SD) | 99 (13.4) | 99 (11.6) | 101 (18.0) | 98 (10.2) | 0.55 (NS) |
| Systolic blood pressure, mmHg (SD) | 134 (12.9) | 132 (14.3) | 135 (10.2) | 136 (13.9) | 0.28 (NS) |
| Diastolic blood pressure, mmHg (SD) | 84 (9.0) | 82 (9.5) | 86 (7.6) | 84 (9.7) | 0.09 (NS) |
| RR medication (%) | 8 | 3 | 11 | 9 | 0.27 (NS) |
| Glucose, mmol/l (SD) | 5.7 (0.7) | 5.8 (0.9) | 5.7 (0.6) | 5.6 (0.4) | 0.67 (NS) |
| Cholesterol, mmol/l (SD) | 5.4 (0.8) | 5.5 (0.8) | 5.3 (0.8) | 5.2 (0.8) | 0.05 (NS) |
| LDL, mmol/l (SD) | 3.6 (0.7) | 3.7 (0.7) | 3.5 (0.7) | 3.5 (0.7) | 0.10 (NS) |
| HDL, mmol/l (SD) | 1.4 (0.4) | 1.3 (0.4) | 1.4 (0.4) | 1.4 (0.3) | 0.90 (NS) |
| Triglycerides, mmol/l (SD) | 1.4 (0.7) | 1.6 (0.9) | 1.4 (0.7) | 1.2 (0.5) | 0.01 (*) |
| Metabolic syndrome, n (%) | 45 (7) | 59 (13) | 42 (13) | 35 (13) | 0.03 (*) |
| Frequency of physical activity (at least moderate intensity, ≥ 30 minutes), n (%)2 | |||||
| Sometimes or never | 58 (35) | 21 (35) | 21 (31) | 16 (40) | 0.07 (NS) |
| 1–2 times/week | 110 (65) | 39 (65) | 33 (69) | 38 (60) |
Notes: 1Statistical comparisons between the groups were performed using analysis of variance or Kruskall–Wallis test for continuous variables and chi-squared test or Fisher's exact test for categorical variables. 2The men who exercised ≥ 3 times/week were excluded from the trial and therefore no one exercised this much at baseline.
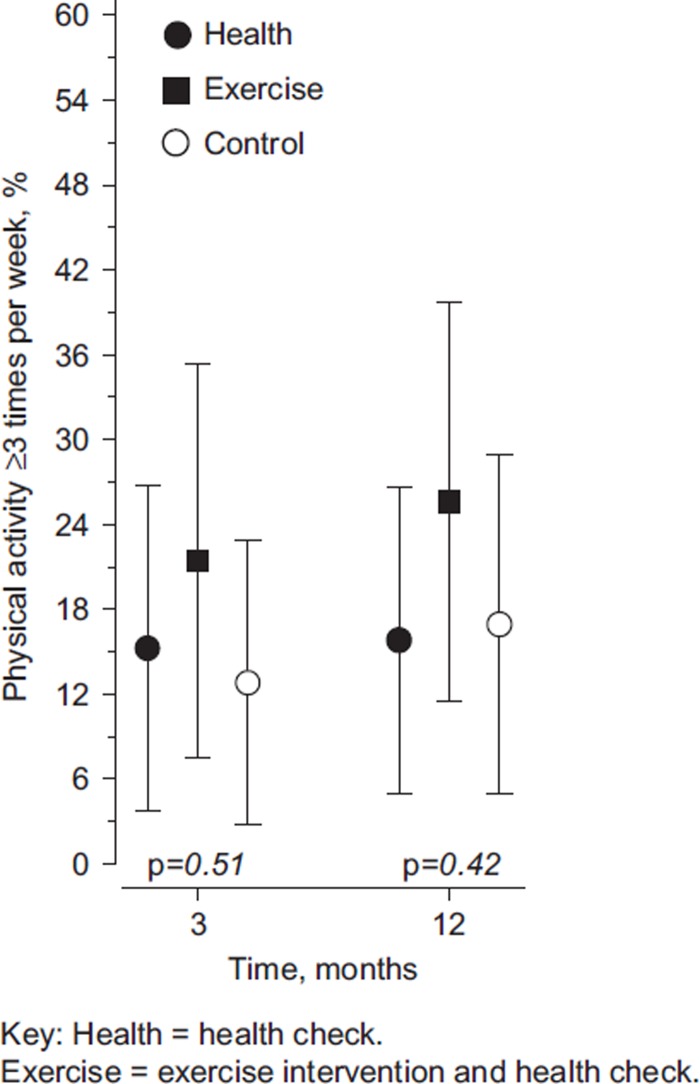
Physical activity
Overall, the men in the trial increased their PA frequency. Since men who exercised at least three times per week were excluded from the trial, none of the participants exercised three times per week at baseline. All study groups increased their PA (Figure 2), and of all participants, 19% (95% CI 12–26) continued exercising at least three times a week at 12 months. In the exercise intervention group, 26% (95% CI 11–40) of men pursued exercising at least three times a week, in the health check group 16% (95% CI 5–27) and in the control group 17% (95% CI 5–29); however the differences between the groups were not statistically significant (Figure 2).
Figure 2.
Percentage of men who performed physical activity at least three times a week at three and 12 months in study groups.
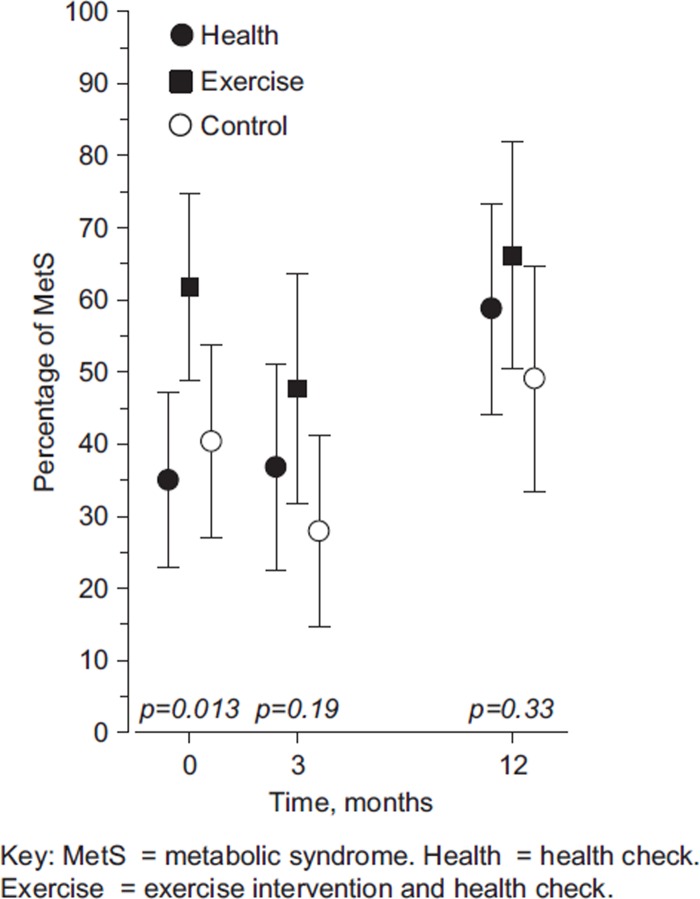
Metabolic syndrome
At baseline, 45% of men fulfilled the criteria for MetS. Although there was a trend towards a decreased proportion of men with MetS at three months, after 12 months the prevalence of MetS had returned to the original level or above (Figure 3). There were no differences between the intervention groups and the control group in the prevalence of MetS.
Figure 3.
Percentage of men with 95% confidence intervals with metabolic syndrome at three and 12 months in study groups.
Other outcomes
The cardiovascular outcomes are presented in Table II. The interventions had no statistically significant effects on these outcomes at three months or at 12 months.
Table II.
Cardiovascular outcomes three months and 12 months after the intervention: Mean (and standard deviation).1.
| All | Health check | Exercise intervention | Controls | |
| Weight, kg 3 m 12 m |
87.3 (11.8) 88.3 (11.8) |
90.0 (12.8) 89.6 (11.3) |
87.9 (12.1) 89.9 (10.9) |
84.7 (10.3) 85.5 (13.0) |
| Systolic blood pressure, mmHg (SD) 3 m 12 m |
135 (13.0) 136 (11.9) |
131 (8.0) 135 (11.8) |
138 (14.1) 139 (11.7) |
136 (14.8) 134 (12.2) |
| Diastolic blood pressure, mmHg (SD) 3 m 12 m |
83 (8.7) 85 (9.4) |
81 (8.3) 83 (10.2) |
86 (8.6) 87 (8.2) |
80 (9.1) 83 (9.7) |
| Glucose, mmol/l (SD) 3 m 12 m |
5.6 (0.6) 5.7 (0.6) |
5.5 (0.5) 5.6 (0.6) |
5.6 (0.8) 5.7 (0.6) |
5.6 (0.5) 5.7 (0.6) |
| Cholesterol, mmol/l (SD) 3 m 12 m |
5.2 (0.8) 5.4 (0.9) |
5.4 (0.8) 5.5 (0.8) |
5.1 (0.9) 5.3 (0.9) |
5.1 (0.8) 5.2 (0.8) |
| LDL, mmol/l (SD) 3 m 12 m |
3.5 (0.7) 3.5 (0.7) |
3.6 (0.7) 3.7 (0.7) |
3.4 (0.8) 3.5 (0.8) |
3.4 (0.7) 3.4 (0.7) |
| HDL, mmol/l (SD) 3 m 12 m |
1.4 (0.3) 1.4 (0.4) |
1.3 (0.3) 1.4 (0.3) |
1.4 (0.3) 1.4 (0.4) |
1.4 (0.3) 1.5 (0.4) |
| Triglycerides, mmol/l (SD) 3 m 12 m |
1.3 (0.6) 1.4 (0.7) |
1.4 (0.7) 1.5 (0.8) |
1.2 (0.5) 1.4 (0.7) |
1.1 (0.4) 1.2 (0.5) |
Note: 1Differences are statistically non-significant.
Discussion
Our pragmatic trial of an exercise intervention and health checks in a municipal health centre was able to change the exercise habits of middle-aged men in all study groups. We recruited men with at least two cardiovascular risk factors and low levels of PA. After one year, 19% of these sedentary men had increased their PA frequency to at least three times a week. There were no differences between the study groups in PA.
Our results are similar to previous studies on health promotion in primary care. A systematic review published in 2012 [12] observed small effects with physical activity promotion for patients recruited in primary care. It provided an estimation of a number needed to treat (NNT) of 12, which means that 12 patients need to be targeted with physical activity promotion for one to become active. This can be compared with smoking cessation advice, where NNTs of 50 to 120 have been reported [13].
Although men increased the frequency of exercise, we found no effects on health outcomes, metabolic syndrome, or individual cardiovascular outcomes. For substantial health benefits, adults should do at least 150 minutes a week of moderate intensity, or 75 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of these [14,15]. Our outcome measure, self-reported physical activity, is somewhat crude and does not take into account the intensity of the exercise or the potential exercise during working hours. However, in a pragmatic primary health care trial it was the most feasible method.
The changes in exercise habits did not have effects on the prevalence of metabolic syndrome in the participants. Either the change in activity was not large enough, the follow-up was not long enough to observe the effects, or other lifestyle changes such as dieting would have been required. It also appears that metabolic syndrome is difficult to alter and may not be an optimal outcome measure. The choice of the outcome measures must be considered as a limitation of this trial.
Randomized controlled trials are not commonly conducted in primary care in Finland. This effort taught us several lessons. Using mass media and local campaigning was effective for recruitment but it also contaminated the trial as the project was very visible in the local newspaper and events, which led to the control men also receiving some of the intervention.
The weakness of our study is that it lacks power. It was designed for 300 men, and we were able to recruit and randomize only 168 men. Although the trial received much attention in the community and men eagerly took part in the screening survey, it was difficult to motivate them to attend for laboratory testing and to participate in the follow-up. Middle-aged men live busy lives with work and families and it is challenging for them to commit themselves to a weekly intervention. According to the group counsellors, the participation rates in the exercise groups varied between 50% and 80%.
Participants in the control group were invited to complete an online questionnaire with health- and lifestyle-related questions at baseline and at three and 12 months. Furthermore, they were promised health counselling and group exercise training after the 12-month study period. The questionnaires, keeping in contact with the study coordinator, and future health counselling and exercise training may have motivated them to increase their PA.
Our results are consistent with previous primary care studies reporting increases in PA levels also among the control group. In a Dutch study, a tailored PA intervention increased PA levels but not more than in the control group [16]. It appeared that the physical activity measurements independently affected participants’ behaviour [17].
The community targets in our study were successful. Some men in the exercise intervention groups continued exercising together after the trial, which was one of our community aims. In addition, the trial also increased collaboration between the health and exercise services in the municipality. An exercise counsellor started consultations at the health centre, and physicians learnt to better refer their patients to the municipal exercise services. Since family medicine is not only for individuals but also for communities, it is important to put the focus on community consequences of trials [18].
In conclusion, our trial led to small changes in the physical activity of middle-aged men but we observed no changes in cardiovascular health. We were, however, able to increase awareness and collaboration in the municipality on physical activity health promotion.
Acknowledgements
The authors would like to thank Ms Maria Teräväinen for help with the study material, and the public health nurses that performed the health checks as well as the employees at the municipal adult education and exercise services for excellent collaboration.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Ethics approval
The trial was approved by the municipal authorities and by the Coordinating Ethics Committee at Helsinki University Hospital on 8 June, 2009 (ref: 4/13/03/00/09). The study was registered at Controlled Trials (http://www.controlled-trials.com). Trial number: ISRCTN80672011.
References
- 1.Pietinen P, Lahti-Koski M, Vartiainen E, Puska P. Nutrition and cardiovascular disease in Finland since the early 1970s: A success story. J Nutr. 2001;13:150–4. [PubMed] [Google Scholar]
- 2.Shaw KA, Gennat HC, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006:CD003817. doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orozco LJ, Buchleitner AM, Gimenez-Perez G, Roquéi Figuls M, Richter B, Mauricio D. Exercise or exercise and diet for preventing type 2 diabetes mellitus. Cochrane Database Syst Rev. 2008:CD003054. doi: 10.1002/14651858.CD003054.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Johnson JL, Slentz CA, Houmard JA. Exercise training amount and intensity effects on metabolic syndrome (from Studies of a Targeted Risk Reduction Intervention through Defined Exercise) Am J Cardiol. 2007;13:1759–66. doi: 10.1016/j.amjcard.2007.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Umpierre D, Ribeiro PA, Kramer CK, Leitão CB, Zucatti AT, Azevedo MJ, Gross JL, Ribeiro JP, Schaan BD. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: A systematic review and meta-analysis. JAMA. 2011;13:1790–9. doi: 10.1001/jama.2011.576. [DOI] [PubMed] [Google Scholar]
- 6.Leijon ME, Faskunger J, Bendtsen P, Festin K, Nilsen P. Who is not adhering to physical activity referrals, and why? Scand J Prim Health Care. 2011;29:234–40. doi: 10.3109/02813432.2011.628238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev. 2012;10:CD009009. doi: 10.1002/14651858.CD009009.pub2. [DOI] [PubMed] [Google Scholar]
- 8.From S, Liira H, Leppävuori J, Remes-Lyly T, Tikkanen H, Pitkälä K. Effectiveness of exercise intervention and health promotion on cardiovascular risk factors in middle-aged men. A protocol of a randomized controlled trial. BMC Public Health. 2013;13:125. doi: 10.1186/1471-2458-13-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finnish Diabetes Association. DEHKO – Development Programme for the Prevention and Care of Diabetes in Finland 2000–2010. Programme for the Prevention of Type 2 Diabetes in Finland 2003–2010. ISBN 952-5301-36-2. 2003. Availabale at: http://www.diabetes.fi/files/1108/Programme_for_the_Prevention_of_Type_2_Diabetes_in_Finland_2003-2010.pdf.
- 10.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;13:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 11.Efron B, Tibshirani RJ. An introduction to the bootsrap. New York: Chapman & Hall; 1993. [Google Scholar]
- 12.Orrow G, Kinmonth AL, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: Systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344:e1389. doi: 10.1136/bmj.e1389. doi: 10.1136/bmj.e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2008;((2)):CD000165. doi: 10.1002/14651858.CD000165.pub3. [DOI] [PubMed] [Google Scholar]
- 14.USDHHS. Washington, DC: USDHHS; 2008. 2008 physical activity guidelines for Americans. Available at: http://www.health.gov/paguidelines/pdf/paguide.pdf. [Google Scholar]
- 15.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP American College of Sports Medicine. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 16.Van Sluijs EM, van Poppel MN, Twisk JW, Chin A, Paw MJ, Calfas KJ, van Mechelen W. Effect of a tailored physical activity intervention delivered in general practice settings: Results of a randomized controlled trial. Am J Public Health. 2005;95:1825–31. doi: 10.2105/AJPH.2004.044537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Sluijs EM, van Poppel MN, Twisk JW, van Mechelen W. Physical activity measurements affected participants’ behavior in a randomized controlled trial. J Clin Epidemiol. 2006;59:404–11. doi: 10.1016/j.jclinepi.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Van Weel C, Roberts RG, De Maeseneer J. Practice and research: Seeking common ground to benefit people. Fam Pract. 2012;29((Suppl 1)):i10–12. doi: 10.1093/fampra/cmr055. doi: 10.1093/fampra/cmr055. [DOI] [PubMed] [Google Scholar]