Abstract
Objective. To assess the effectiveness of a two-year school-based intervention, consisting of integrated and replicable physical activity and nutritional education on weight, fat percentage, cardiovascular risk factors, and blood pressure. Design and setting. Six elementary schools in Reykjavik were randomly assigned to be either intervention (n = 3) or control (n = 3) schools. Seven-year-old children in the second grade in these schools were invited to participate (n = 321); 268 (83%) underwent some or all of the measurements. These 286 children were followed up for two years. Intervention. Children in intervention schools participated in an integrated and replicable physical activity programme, increasing to approximately 60 minutes of physical activity during school in the second year of intervention. Furthermore, they received special information about nutrition, and parents, teachers, and school food service staff were all involved in the intervention. Subjects. 321seven-year-old schoolchildren. Main outcome measures. Blood pressure, obesity, percentage of body fat, lipid profile, fasting insulin. Results. Children in the intervention group had a 2.3 mmHg increase in systolic blood pressure (SBP) and a 2.9 mmHg increase in diastolic blood pressure (DBP) over the two-year intervention period, while children in the control group increased SBP by 6.7 mmHg and DPB by 8.4 mmHg. These changes were not statistically significant. Furthermore there were no significant changes in percentage body fat, lipid profile, or fasting insulin between the intervention and control schools. Conclusion. A two-year school-based intervention with increased physical activity and healthy diet did not have a significant effect on common cardiovascular risk factors.
Key Words: Blood pressure, children, general practice, Iceland, intervention, nutrition, physical activity, school
A school-based intervention, focusing on increasing physical activity and promoting a healthy diet, was conducted to have a positive impact on cardiovascular risk factors among seven- to nine-year-old children. The intervention resulted in:
No significant reduction of age-related increase in blood pressure.
No significant effect on fat percentage or other cardiovascular risk factors.
No significant effect on systolic blood pressure among overweight children.
Introduction
The prevalence of overweight and obesity has increased in recent decades and remains high among children and adolescents [1]. Studies have shown that obesity in childhood is an important predictor of adult obesity [2], and if overweight begins early in childhood, obesity in adulthood is likely to be more severe [3]. Obesity is an important cardiovascular risk factor [4], but it may also lead to lower self- esteem and other psychological problems [5]. Physical inactivity and unhealthy diet are common, modifiable risk factors for obesity that underlie other major chronic diseases, including heart disease, stroke, and diabetes [6]. Prevention is better than cure and primary care providers are among those who definitely play an essential role in the campaign against these lifestyle-related chronic diseases. It is therefore important to study how we can get people and particularly children to stay healthy without developing these chronic diseases.
Sedentary behaviour is associated with higher blood pressure (BP) in young children [6], and a higher level of physical activity is associated with lower BP [7]. Furthermore, more physically active nine-year-old children have been shown to lower systolic blood pressure over a year-year interval [8], and measures aimed at preventing a decline in physical activity during adolescence may prevent higher BP in youth [9]. However, in a meta-analysis of intervention studies of 36 weeks and less, the BP effect of exercise was insignificant (1–3 mmHg) [10], but the length of intervention may be of importance as Hansen et al. showed an effect of 4–6 mmHg after eight months’ training but not after three months’ training on both systolic and diastolic blood pressure [11]. High intake of fruits and vegetables may be important as well and has been shown to lower BP in children and lower early gains in SBP and DBP, compared with children with low intake [12] .
The treatment of obesity and efforts to increase physical activity is a difficult, but challenging, task and the need to prevent obesity in early life is of paramount importance. However, school-based physical activity and dietary intervention studies have shown contradictory results when it comes to successfully improving risk-factor profiles of many of the aforementioned chronic diseases [13,14].
We conducted a school-based intervention study emphasizing increased physical activity and healthier nutrition. In previously published papers we have described the effect that the intervention had on fitness and nutrition and the status of an array of common cardiovascular disease (CVD) risk factors among these seven-year-old schoolchildren [15–17]. The main aim of this paper is to report the effect of the two-year school-based intervention on these same CVD risk factors.
Material and methods
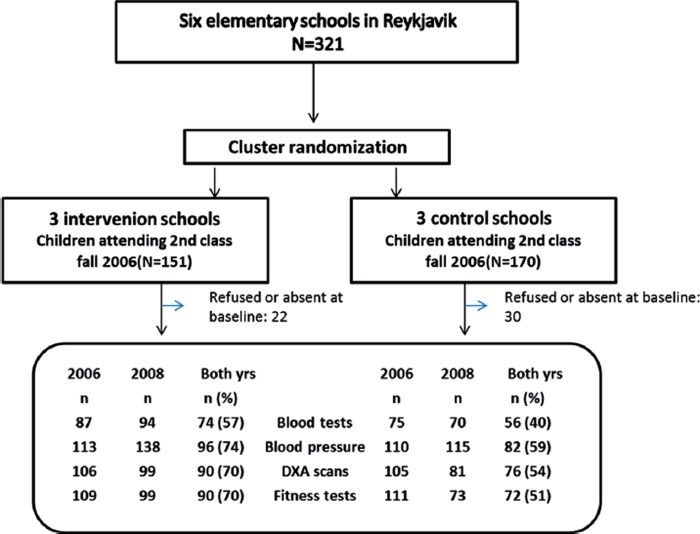
This study was a cluster-randomized controlled trial carried out to assess the effect of a two-year school-based intervention. From a pool of all elementary schools in Reykjavik, the capital of Iceland, which had more than 30 students in second grade, a total of six elementary schools were randomly selected. These six schools were paired with regard to number of students and social background, such that each pair comprised the two schools that Reykjavik Board of Education thought were most alike. One of the paired schools was randomly selected to participate in the intervention and the other school was used as a control. All children attending second grade in these schools were invited. Of the 321 children invited, 268 (83%) gave informed consent to participate in the study but 53 (17%) refused to participate. All measurements were conducted between September and December 2006 and repeated two years later, i.e. between September and December 2008. A flow chart showing participation in the primary outcome measurements is shown in Figure 1.
Figure 1.
Flow chart showing number (%) of participations in the primary outcome measurements in 2006 and 2008.
The study was approved by the National Bioethics Committee as well as the Icelandic Data Protection Commission (Study number: VSN b200605002&03).
Measurements
When weight was measured children had their underwear on but no other clothes. A calibrated scale was used (Seca 708, Seca Ltd., Birmingham, UK). Weight was measured to the nearest 0.1 kg. Height was measured to the nearest mm with a transportable stadiometer or a calibrated stadiometer found at school. Percentage of body fat mass was measured with dual energy X-ray absorptiometry (DXA). The scans were run using the paediatric programme of Hologic QDR 4500. Fasting blood samples were obtained using standard procedures after overnight fasting. BP was measured three times in the left arm of seated participants at five-minute intervals, and the average of all measurements was used for analysis. A Trimline Hader Aneroid Sphygmomanometer was used with three different cup sizes approximately midway between olecranon and acromion. The same medical doctor, aided by two trained assistants, performed all the measurements. In all, 178 (67%) children had BP measurements both in 2006 and 2008. In the intervention schools 113 (88%) children had BP measurements in 2006, and 96 (85%) children were measured again in 2008. In the control schools, 110 (80%) children were measured in 2006, and 82 (75%) children were measured again in 2008. Subcutaneous skinfold measurements were taken three times at five sites, using a Harpenden skinfold calliper (Baty Internationnal, Burgess Hill, UK). Measurements of skinfold thickness were performed by lifting a skinfold and subcutaneous fat away from the underlying muscle and this thickness was measured with the skinfold calliper. The mean values from each site were then summed and used for analysis.
Food records were recorded continuously over three days, two weekdays and one weekend at the same time in 2006 and 2008[16].
Intervention
Teachers’ involvement. The teachers received training at bimonthly workshop meetings and through informal on-site meetings, both to provide teachers with expert information on physical activity and nutrition and to give them opportunities for dialogue with their colleagues regarding the evolvement of the intervention. Teachers’ physical activity log books were the basis for estimating the time children spent doing physical activity under a teacher's supervision at school.
Physical activity (PA). The PA intervention has been described in detail elsewhere [18]. In brief, the PA intervention was progressive in nature, starting with approximately 30 minutes a day at the start of the study and increasing to approximately 60 minutes a day in the latter intervention year, where teachers who implemented the intervention used various strategies to better integrate PA into the daily routine at school. Accelerometers were used to assess both the volume and intensity of PA. Cardiorespiratory fitness (watts/kg) was measured with a Monark ergometer. This maximal ergometer test was run as follows: every three minutes the weight on the wheel was increased, and participants kept a steady pace on the bike until exhausted, or until he or she could no longer keep a steady pace. The protocol was the same as in the European Youth Heart Study [19].
Nutrition. The main focus of the dietary intervention was on increasing fruit and vegetable intake, with both educational material and homework assignments [16]. Food-based dietary guidelines on fish, fish liver oil and milk intake were also in focus, and parents, teachers, and school food service staff were involved in the intervention. Dietary intake was assessed with three-day weighed dietary records in autumn 2006 and autumn 2008.
Statistical analyses
Randomization was performed at the school level, while the outcome data were collected by repeated measurements on individuals. SPSS version 19 was used for analysis except for factor analyses where an R statistical pack was used.
Results were expressed as mean and standard deviation, with a 95% confidence interval. Statistical significance was deemed to be at p ≤ 0.05. When comparing the control and intervention groups for increase in blood pressure, we calculated the difference between the measurements made in 2006 and 2008 and used factor analysis to assess whether there was a significant difference between groups. A paired-samples t-test was used to assess whether a variable had changed significantly within a group over these two years.
Results
Blood tests
Baseline characteristics of both the control and intervention group are given in Table I. At baseline the mean age of the study participants was 7.3 years. The sum of five skinfolds was 32.7 ± 11.3 mm (SD), and the fat percentages was 24.4% ± 6.3% (SD) at baseline, and in both groups these parameters increased over the next two years without significant differences between groups. Lipid profile, fasting insulin, HbA1c, and fasting glucose levels did not change differently between the groups (Table II).
Table I.
Descriptive statistics of the study population at start of the study.
| All | Intervention | Control | p | 95% CI | ||||
| n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | |||
| Age (years) | 267 | 7.3 ± 0.3 | 128 | 7.4 ± 0.3 | 139 | 7.3 ± 0.3 | 0.01 | 0.02, 0.14 |
| Height (cm) | 265 | 127.0 ± 5.2 | 128 | 127.1 ± 5.3 | 138 | 127.0 ± 5.3 | 0.88 | –1.38, 1.18 |
| Weight (kg) | 267 | 26.3 ± 4.4 | 128 | 25.8 ± 4.0 | 139 | 26.8 ± 4.6 | 0.07 | –0.08, 2.01 |
| WB%fat | 211 | 24.4 ± 6.2 | 106 | 23.9 ± 1.9 | 105 | 24.8 ± 1.9 | 0.28 | –0.75, 2.6 |
| Sum of five skinfolds (mm) | 226 | 32.7 ± 11.3 | 110 | 31.6 ± 11.0 | 113 | 32.7 ± 11.3 | 0.5 | –0.74, 2.6 |
| Total cholesterol (mmol/L) | 162 | 4.4 ± 0.7 | 87 | 4.4 ± 0.6 | 75 | 4.3 ± 0.6 | 0.12 | –0.16, 0.10 |
| HDL-cholesterol (mmol/L) | 164 | 1.55 ± 0.3 | 89 | 1.6 ± 0.3 | 75 | 1.5 ± 0.3 | 0.12 | –0.07, 0.04 |
| LDL-cholesterol (mmol/L) | 162 | 2.5 ± 0.6 | 87 | 2.6 ± 0.6 | 75 | 2.5 ± 0.5 | 0.15 | –0.3, 0.05 |
| Triglycerides (mmol/L) | 162 | 0.64 ± 0.22 | 87 | 0.59 ± 0.2 | 75 | 0.69 ± 0.2 | 0.01 | 0.02, 0.16 |
| Fasting glucose (mmol/L) | 150 | 4.6 ± 0.3 | 82 | 4.6 ± 0.3 | 68 | 4.6 ± 0.3 | 0.35 | –0.05, 0.15 |
| HbA1C (%) | 164 | 5.42 ± 0.3 | 86 | 5.3 ± 0.3 | 75 | 5.5 ± 0.2 | 0.86 | –0.12, 0.10 |
| Insulin (mU/L) | 160 | 3.99 ± 2.27 | 87 | 3.83 ± 2.32 | 75 | 4.16 ± 2.23 | 0.2 | –0.38, 1.03 |
| SBP (mmHg) | 222 | 94 ± 6 | 125 | 95 ± 7 | 97 | 93 ± 6 | 0.07 | –4.0, 0.65 |
| DBP (mmHg) | 222 | 56 ± 5 | 125 | 57 ± 5 | 97 | 55 ± 4 | 0.01 | –2.7, 0.38 |
| Fitness | 220 | 2.42 ± 0.54 | 109 | 2.48 ± 0.57 | 111 | 2.36 ± .49 | 0.1 | –.26, 0.02 |
Notes: Wb%fat = whole body percentage fat; SBP = systolic blood pressure; DBP = diastolic blood pressure; HDL = high density lipoprotein; LDL = low density lipoprotein.
Table II.
Comparison of various cardiovascular risk factors between intervention group and control group after intervention.
| Variable | Intervention | Control | ||||
| Change from | Change from | |||||
| Mean ± SD | 2006 | 95% CI | Mean ± SD | 2006 | 95% CI | |
| Weight kg | 32.5 ± 5.5 | + 6.6 | 6.1, 7.0 | 33.7 ± 7.1 | + 6.9 | 6.4, 7.5 |
| Height cm | 136.8 ± 5.3 | + 9.6 | 9.1, 10.0 | 138.5 ± 6.1 | + 11.5 | 11.2, 11.8 |
| BMI kg/m2 | 17.3 ± 2.1 | + 1.3 | 1.1, 1.5 | 17.7 ± 2.8 | + 0.95 | 0.7, 1.2 |
| Wb%fat | 25.5 ± 7.6 | + 1.67 | 1.1, 2.2 | 26.4 ± 5.2 | + 1.53 | 0.85, 2.2 |
| Total cholesterol (mmol/L) | 4.53 ± 0.69 | + 0.06 | –0.06, 0.17 | 4.29 ± 0.59 | –0.01 | –0.12, 0.13 |
| HDL cholesterol (mmol/L) | 1.58 ± 0.30 | –0.01 | –0.05, 0.05 | 1.52 ± 0.25 | + 0.02 | –0.05, 0.08 |
| LDL-cholesterol (mmol/L) | 2.65 ± 0.60 | + 0.05 | –0.04, 0.15 | 2.50 ± 0.51 | 0.00 | –0.09, 0.09 |
| Triglycerides (mmol/L) | 0.63 ± 0.39 | 0.02 | –0.09, 0.12 | 0.60 ± 0.31 | –0.07 | –0.16, 0.03 |
| Fasting glucose (mmol/L) | 4.30 ± 0.39 | –0.3 | –0.38, –0.19 | 4.31 ± 0.30 | –0.39 | –0.47, –0.28 |
| HbA1C (%) | 5.38 ± 0.73 | + 0.07 | –0.14, 0.25 | 5.70 ± 0,24 | + 0.19 | 0.14, 0.25 |
| S-Insulin (mU/L) | 5.49 ± 2.60 | + 1.5 | 0.98, 2.5 | 6.48 ± 3.56 | + 2.1 | 1.2, 3.1 |
| SBP (mmHg) | 98.1 ± 5.6 | + 2.3 | 1.1, 3.6 | 99.3 ± 6.1 | + 6.7 | 5.2, 8.3 |
| DBP (mmHg) | 59.8 ± 5.7 | + 2.9 | 1.9, 3.9 | 63.3 ± 6.6 | + 8.4 | 6.7, 9.9 |
| Sum of five skinfolds (mm) | 38.4 ± 16.0 | + 7.3 | 5.8, 8.9 | 40.0 ± 17.0 | + 6.9 | 5.3, 8.5 |
| Fitness (watts/kg) | 2.81 ± 0.50 | 0.26 | 0.16, 0.35 | 2.47 ± 0.48 | + 0.1 | 0.00, 0.20 |
Notes: Wb%fat = whole body percentage fat; SBP = systolic blood pressure; DBP = diastolic blood pressure; HDL = high density lipoprotein; LDL = low density lipoprotein.
Teachers’ activity log books on the time spent doing PA showed a gradual increase from approximately 35 minutes per day in the autumn of 2006 to 65 minutes per day in the spring of 2008, but these values then dropped to approximately 40 minutes per day in the fall of 2008. Accelerometer results showed that children in the intervention schools spent an estimated additional time of approximately four minutes of moderate-to-vigorous physical activity, compared with controls during school hours in the autumn of 2007 (i.e. after one year of intervention) (p < 0.01). At that time teachers’ activity log books showed approximately 50 minutes of daily PA during school hours, but at the end of the two-year study period when activity log books showed approximately 40 minutes of PA daily, accelerometer results did not show a significant difference between intervention and control schools (p = 0.1). Moreover, children with higher BMI were less active than children with lower BMI (p = 0.01).
Fitness
There was a non-significant increase in cardiorespiratory fitness in the intervention group (p = 0.18). This improvement was on average 0.286 watts/kg or 0.37 z-score units.
Nutrition
Total fruit and vegetable intake increased significantly by 47% in the intervention schools and decreased by 27% in the control schools. Fibre intake increased significantly in the intervention schools (17%, p < 0.01) but not in the control schools (7%, p = 0.09).
Blood pressure
Both systolic blood pressure (SBP) and diastolic blood pressure (DBP) increased from 2006 to 2008 in both groups. The rise in SBP was 2.4 mmHg higher in the control group compared with the intervention group and in DBP 4.7 mmHg. However, these differences in blood pressure changes were not statistically significant, either for SBP (p = 0.15, Table III) or DBP (p = 0.13, Table IV). Compared with normal-weight children, overweight children on average had 3.6 and 5.2 mmHg higher SBP in 2006 and 2008 (p < 0.05 for both years) and 2.1 and 3.9 mmHg higher DBP (p = 0.08 and < 0.05).
Table III.
Regression cluster analysis with SBP at the end of intervention as the dependent factor.
| SBP: mm/hg (SE) | p | |
| Group (0,1) | –2.5 (1.4) | 0.15 |
| Gender (0,1) | –0.4 (0.1) | 0.66 |
| SBP pre | 0.4 (0.8) | < 0.01 |
Notes: Group: 1 = Intervention group, 0 = Control group. Gender: Female = 1, Male = 0, SBP pre: systolic blood pressure at study start.
Table IV.
Regression cluster analysis with DBP at the end of intervention as the dependent factor.
| DBP: mm/hg (SE) | p | |
| Group (0,1) | –4.7 (2.5) | 0.13 |
| Gender (0,1) | 2.0 (0.8) | 0.01 |
| DBP pre | 0.5 (0.1) | < 0.01 |
Notes: Group: 1 = Intervention group, 0 = Control group. Gender: Female = 1, Male = 0, DBP pre: Diastolic blood pressure at study start.
Discussion
The main finding of the study was that a two-year school-based intervention did not prevent an increase in blood pressure among seven- to nine-year-old children. However, there was a noticeable trend in the direction of a lower increase in age-related increase in blood pressure among children in the intervention group. Furthermore, no improvements were observed with regard to other common CVD risk factors, such as blood lipids.
In line with many other studies [20], our study showed a positive association between BP and BMI. No significant change in body fat percentage was observed between the groups. The difference that was noted in BP between groups applied for both genders and for normal-weight and overweight children with regard to DBP, but not SBP. In obese adolescents exercise plus diet intervention seems to have more effect on BP than exercise alone [21], and exercise without weight change has been shown to lower BP in hypertensive adolescents [22,23]. Among overweight children as a group, in our study there was no statistical difference in the rate of increase in SBP, indicating that overweight children possibly did not participate as much in the intervention, or that they might have more resistant BP than other children, thus needing more intense and longer intervention to achieve significant changes.
Some prior studies indicate that a combination of increased PA and healthy nutrition and lifestyle has a positive effect on BP in children after one to three years of intervention [24,25]. This is somewhat in line with the result of this study. There is some indication that the amount of PA may be important [7], but change in BP in childhood may also be related to change in physical fitness; children increasing in fitness seem to have lower year-related increases in BP [26]. Baseline fitness and improved fitness may both be associated with lower BP in adolescents [26], and young adults are less likely to develop hypertension later in life if they are fit [27]. Other studies have not been as promising [28]. Finally, since BP in childhood predicts hypertension and metabolic syndrome later in life [29,30], early intervention is of importance.
In our study children in the intervention group consumed more fruits and vegetables at the end of the study [16], and the intervention group increased their fitness by an average of 0.37 z-score units [17]. This could be one of the reasons why a positive trend was seen on age-related increase in BP in the intervention group compared with the control group.
Effects of school-based PA on BMI have not been promising, and meta-analysis has shown that increased PA in schools is unlikely to affect childhood obesity [28]. On the other hand, a study done by Kriemler et al. has concluded that multi- component physical activity intervention reduced adiposity in children [13]. The outcome was measured in the spring after nine months of intervention, but school-based changes have been shown to be lost during summer vacation [31], and in a three-year follow-up the effect on obesity had disappeared [32]. In this study the PA was highest early in 2008, but the measurements of the effects of intervention were performed almost five months later, after summer vacation, which perhaps led to attenuation of favourable changes in the participants’ risk-factor profile.
Studies have shown associations between objectively measured PA and clustered metabolic risk factors in children [33]. Change in fitness has been shown to be reflected in changes in total cholesterol, high-density lipoprotein, and systolic BP [34]. Our study did not show significant change in metabolic risk factors or BP between the intervention and control groups.
In Iceland GPs provide health services for elementary schools. As many of the chronic diseases such as obesity and type II diabetes are strongly associated with lifestyle more effort has been put into getting people to adopt to healthy lifestyle with regard to both food and exercise. It is thus important to start early and introduce these healthy habits to young children. GPs and other primary care providers play an extremely important role in implementing this.
The strength of this study was the length of the intervention period (two years); however, two years is a short time for inducing sustained lifestyle changes. Another strength of this study is objective measurements with DXA scans of body composition. One weakness of this study was that PA decreased at the end of the study period, after summer vacation, possibly because of high teacher turnover at the end of the study. At the end of the study, six of eight teachers were either on maternity leave or had started teaching a different class. The new teachers only received minimal training at one meeting in the autumn of 2008. Furthermore, the extra PE lesson per week, which was introduced to the intervention schools only in the autumn of 2007, was no longer available as of autumn 2008. When the study ended, Iceland was in a state of financial crisis affecting all families, and it is possible that this may have had negative effects on the response to the intervention at the end of the study. Approximately 20% of the participants in BP measurements from 2006 to 2008 dropped out as some students did not participate in all parts of the study, and others had moved away from the area. Another limitation is that the researchers did know which group was the intervention group, and a possible effect on the results because of this cannot be precluded. It is also possible that due to small sample size we have failed to detect a significant effect that could be present.
Our study shows that it is possible to increase PA and promote healthy eating when teachers integrate them into the daily routine at school. However, this increase in PA can easily be lost again, and the goal of 60 minutes of PA/day was not achieved at the end of the study.
We conclude that having teachers integrate PA and nutrition into the daily routine at school can have a positive effect on children's PA and possibly BP but not significant effects on BMI or other cardiovascular risk factors.
Acknowledgements
The study was supported by the Icelandic Centre for Research, the City of Reykjavík, the Ministry of Education, Science and Culture, Brim Seafood, and the Primary Health Care Research Fund.
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics. 2001;108:712–18. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 4.Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–74. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz MB, Puhl RR. Childhood obesity: A societal problem to solve. Obes Rev. 2003;4:57–71. doi: 10.1046/j.1467-789x.2003.00093.x. [DOI] [PubMed] [Google Scholar]
- 6.Martinez-Gomez D, Tucker J, Heelan KA, Welk GJ, Eisenmann JC. Associations between sedentary behavior and blood pressure in young children. Arch Pediatr Adolesc Med. 2009;163:724–30. doi: 10.1001/archpediatrics.2009.90. [DOI] [PubMed] [Google Scholar]
- 7.Leary SD, Ness AR, Smith GD, Mattocks C, Deere K, Blair SN, Riddoch C. Physical activity and blood pressure in childhood: Findings from a population-based study. Hypertension. 2008;51:92–8. doi: 10.1161/HYPERTENSIONAHA.107.099051. [DOI] [PubMed] [Google Scholar]
- 8.Gidding SS, Barton BA, Dorgan JA, Kimm SYS, Kwiterovich PO, Lasser NL, Robson AM, Stevens VJ, Van Horn L, Simons-Morton DG. Higher self-reported physical activity is associated with lower systolic blood pressure: The Dietary Intervention Study in Childhood (DISC) Pediatrics. 2006;118:2388–93. doi: 10.1542/peds.2006-1785. [DOI] [PubMed] [Google Scholar]
- 9.Maximova K, O’Loughlin J, Paradis G, Hanley JA, Lynch J. Declines in physical activity and higher systolic blood pressure in adolescence. Am J Epidemiol. 2009;170:1084–94. doi: 10.1093/aje/kwp255. [DOI] [PubMed] [Google Scholar]
- 10.Kelley GA, Kelley KS. Exercise and resting blood pressure in children and adolescents: A meta-analysis. Pediatr Exercise Sci. 2003;15:83–97. doi: 10.1111/j.1520-037x.2003.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansen HS, Froberg K, Hyldebrandt N, Nielsen JR. A controlled-study of 8 months of physical-training and reduction of blood-pressure in children: The Odense schoolchild. BMJ. 1991;303:682–5. doi: 10.1136/bmj.303.6804.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore LL, Singer MR, Bradlee ML, Diousse L, Proctor MH, Cupples LA, Ellison RC. Intake of fruits, vegetables, and dairy products in early childhood and subsequent blood pressure change. Epidemiology. 2005;16:4–11. doi: 10.1097/01.ede.0000147106.32027.3e. [DOI] [PubMed] [Google Scholar]
- 13.Kriemler S, Zahner L, Schindler C, Meyer U, Hartmann T, Hebestreit H, Brunner-La Rocca HP, van Mechelen W, Puder JJ. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785. doi: 10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Sluijs EMF, McMinn AM, Griffin S. Effectiveness of interventions to promote physical activity in children and adolescents: Systematic review of controlled trials. BMJ. 2007;335:703–7. doi: 10.1136/bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hrafnkelsson H, Magnusson KT, Sigurdsson EL, Johannsson E. Association of BMI and fasting insulin with cardiovascular disease risk factors in seven-year-old Icelandic children. Scand J Prim Health Care. 2009;27:186–91. doi: 10.1080/02813430903155028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kristjansdottir AG, Johannsson E, Thorsdottir I. Effects of a school-based intervention on adherence of 7–9-year-olds to food-based dietary guidelines and intake of nutrients. Public Health Nutrition. 2010;13:1151–61. doi: 10.1017/S1368980010000716. [DOI] [PubMed] [Google Scholar]
- 17.Magnusson KT, Hrafnkelsson H, Sigurgeirsson I, Johannsson E, Sveinsson T. Limited effects of a 2-year school-based physical activity intervention on body composition and cardiorespiratory fitness in 7-year-old children. Health Educ Res. 2012;27:484–94. doi: 10.1093/her/cys049. [DOI] [PubMed] [Google Scholar]
- 18.Magnusson KT, Sigurgeirsson I, Sveinsson T, Johannsson E. Assessment of a two-year school-based physical activity intervention among 7–9-year-old children. Int J Behav Nutrition Physical Activity. 2011;8:138. doi: 10.1186/1479-5868-8-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wedderkopp N, Froberg K, Hansen HS, Andersen LB. Secular trends in physical fitness and obesity in Danish 9-year-old girls and boys: Odense School Child Study and Danish substudy of the European Youth Heart Study. Scand J Med Sci Sports. 2004;14:150–5. doi: 10.1111/j.1600-0838.2004.00365.x. [DOI] [PubMed] [Google Scholar]
- 20.Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. The relationship of body mass index and blood pressure in primary care pediatric patients. J Pediatr. 2006;148:195–200. doi: 10.1016/j.jpeds.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 21.Becque MD, Katch VL, Rocchini AP, Marks CR, Moorehead C. Coronary risk incidence of obese adolescents: Reducion by exercise plus diet intervention. Pediatrics. 1988;81:605–12. [PubMed] [Google Scholar]
- 22.Hagberg JM, Goldring D, Ehsani AA, Heath GW, Hernandez A, Schechtman K, Holloszy JO. Effect of exercise training on the blood-pressure and hemodynamic features of hypertensive adolescents. Am J Cardiol. 1983;52:763–8. doi: 10.1016/0002-9149(83)90412-5. [DOI] [PubMed] [Google Scholar]
- 23.Gutin B, Basch C, Shea S, Contento I, Delozier M, Rips J, Irigoyen M, Zybert P. Blood-pressure, fitness, and fatness in 5-year-old and 6-year-old children. JAMA. 1990;264:1123–7. [PubMed] [Google Scholar]
- 24.Alexandrov AA, Maslennikova GY, Kulikov SM, Propirnij GA, Perova NV. Primary prevention of cardiovascular- disease: 3-year intervention results in boys of 12 years of age. Prev Med. 1992;21:53–62. doi: 10.1016/0091-7435(92)90005-3. [DOI] [PubMed] [Google Scholar]
- 25.Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Healthier options for public schoolchildren program improves weight and blood pressure in 6- to 13-year-olds. J Am Diet Assoc. 2010;110:261–7. doi: 10.1016/j.jada.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 26.Shea S, Basch CE, Gutin B, Stein AD, Contento IR, Irigoyen M, Zybert P. The rate of increase in blood-pressure in children 5 years of age is related to changes in aerobic fitness and body-mass index. Pediatrics. 1994;94:465–70. [PubMed] [Google Scholar]
- 27.Carnethon MR, Evans NS, Church TS, Lewis CE, Schreiner PJ, Jacobs DR, Sternfeld B, Sidney S. Joint associations of physical activity and aerobic fitness on the development of incident hypertension coronary artery risk development in young adults. Hypertension. 2010;56:49–55. doi: 10.1161/HYPERTENSIONAHA.109.147603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: A meta-analysis. Can Med Assoc J. 2009;180:719–26. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–46. doi: 10.1542/peds.2006-2543. [DOI] [PubMed] [Google Scholar]
- 30.Chen XL, Wang YF. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation. 2008;117:3171–80. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carrel AL, Clark RR, Peterson S, Eickhoff J, Allen DB. School-based fitness changes are lost during the summer vacation. Arch Pediatr Adolesc Med. 2007;161:561–4. doi: 10.1001/archpedi.161.6.561. [DOI] [PubMed] [Google Scholar]
- 32.Meyer U, Schindler C, Zahner L, Ernst D, Hebestreit H, van Mechelen W, Rocca H, Probst-Hensch N, Puder JJ, Kriemler S. Long-term effect of a school-based physical activity program (KISS) on fitness and adiposity in children: A cluster-randomized controlled trial. Plos One. 2014;9:10. doi: 10.1371/journal.pone.0087929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steele RM, Brage S, Corder K, Wareham NJ, Ekelund U. Physical activity, cardiorespiratory fitness, and the metabolic syndrome in youth. J Appl Physiol. 2008;105:342–51. doi: 10.1152/japplphysiol.00072.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jago R, Froberg K, Cooper AR, Eiberg S, Andersen LB. Three-year changes in fitness and adiposity are independently associated with cardiovascular risk factors among young Danish children. J of Physical Activity & Health. 2010;7:37–44. doi: 10.1123/jpah.7.1.37. [DOI] [PubMed] [Google Scholar]