Abstract
Objective. Little is known about the prognosis of patients with chronic disease who contact the out-of-hours (OOH) service in primary care. The characteristics of contacts with the Danish out-of-hours service and daytime general practice, hospitalization, and death were studied during a 30-day follow-up period in patients with chronic heart diseases. Design. Cohort study. Setting and subjects. The study was based on data from 11 897 adults aged 18 + years from a Danish survey of OOH contacts, including information on consultation type. Reason for encounter (RFE) was categorized by OOH GPs at triage as either “exacerbation” or “new health problem”. Registry data were used to identify eligible patients, and the cohort was followed for 30 days after OOH contact through nationwide registries on healthcare use and mortality. Main outcome measures. The 30-day prognosis of chronic-disease patients after OOH contact. Results. Included patients with chronic disease had a higher risk of new OOH contact, daytime GP contact, and hospitalization than other patients during the 30-day follow-up period. OOH use was particularly high among patients with severe mental illness. A strong association was seen between chronic disease and risk of dying during follow-up. Conclusion. Patients with chronic disease used both daytime general practice and the out-of-hours service more often than others during the 30-day follow-up period; they were more often hospitalized and had higher risk of dying. The findings call for a proactive approach to future preventive day care and closer follow-up of this group, especially patients with psychiatric disease.
Key Words: Chronic disease, Denmark, general practice, OOH, out-of-hours service, primary healthcare, reasons for encounter
Limited knowledge exists on the prognosis of patients with chronic disease who attend out-of-hours (OOH) primary care.
Patients with at least one out of five selected chronic diseases had higher OOH and GP use and also increased risk of hospitalization than other patients during the 30-day follow-up period.
Patients with chronic disease in combination with OOH contact were at high risk of dying.
The findings mandate more proactive approaches to future preventive day care and follow-up of patients with chronic disease.
Introduction
An increasing number of people suffer from chronic diseases in the Western world due to lifestyle, rising life expectancy, and recent advances in medical science. In Western countries, patients diagnosed with chronic diseases consume 70–80% of all healthcare costs, and chronic diseases are estimated to account for more than 60% of all deaths [1,2]. Therefore, healthcare provision must be efficient and of high quality. A special aspect is the development of a more proactive approach to both daytime care and acute out-of-hours (OOH) care. Such a new direction will depend broadly on well-coordinated primary care [3,4]. Patients with chronic disease should, preferably, be seen by their own GP in the daytime to ensure coherent and comprehensive care. However, this group of patients also seem to have high needs for OOH care for handling both new health problems and exacerbations of existing chronic disease [5]. Nevertheless, little is known about the short-term prognosis for patients with chronic diseases who contact the OOH service. To better plan and optimize both daytime and OOH care for patients with chronic disease, more knowledge is needed regarding their short-term prognosis and their use of healthcare services after an OOH contact.
We aimed to analyse the 30-day prognosis after OOH contact for patients with one of five selected chronic diseases (i.e. heart disease, lung disease, diabetes, severe mental illness, or cancer) by studying the characteristics and the frequency of contacts with the OOH service, contacts with the daytime GP, hospitalization, and the risk of death.
Material and methods
Design and setting
The study was based on data from the Danish survey “Kontakt- og sygdomsmønster i lægevagten LV-KOS 2011” (LV-KOS), which has been described elsewhere in detail [6]. The LV-KOS survey was a comprehensive population-based cross-sectional study performed in the Central Denmark Region describing contacts with the OOH service during a 12-month period from 2010 to 2011. The GPs included patients through electronic pop-up questionnaires for three different types of contacts with the OOH service: telephone consultations, clinical consultations, or home visits. The pop-up questionnaires were integrated into the existing electronic OOH patient administration system. The OOH GPs were asked whether the reason for the encounter (RFE) in question regarded a “new event” or an “exacerbation” of an already diagnosed chronic disease. The frequency of the pop-up questionnaire was set to ensure both an acceptable GP workload and sufficient sample size for valid research results: one in every 10 telephone contacts, one in every three clinical consultations, and every home visit. We have previously shown that the participating GPs were representative of all GPs working in the OOH service during the study period. Likewise, the registered contacts (for all three types of contact) were highly representative of all contacts with the OOH in the region during the investigated period of time [6].
Study population
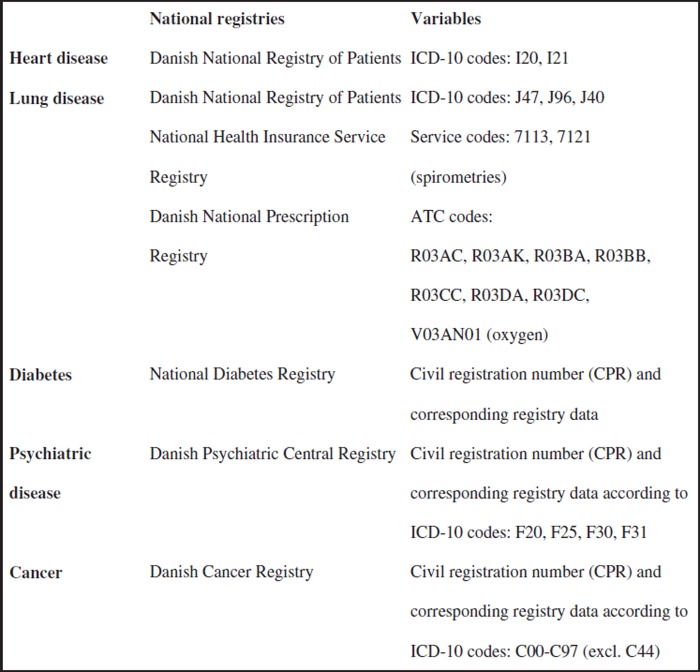
The study population comprised a cohort of 11 897 adult patients aged 18 years or older with a Danish civil registration (CPR) number, which is assigned to all Danish residents [7]. Patients who had died at the time of inclusion in the LV-KOS survey were excluded (n = 203). Included patients were categorized according to chronic disease defined as heart disease, lung disease, severe mental illness, diabetes, or cancer by using information from Danish nationwide registries (Figure 1) [5,8].
Figure 1.
Sources and codes for identification of patients with five chronic diseases.
Defining the populations with chronic disease
To identify patients with chronic disease, we linked the LV-KOS cohort [9] with information from Danish nationwide registries [8] by using the CPR number as key identifier for the period 1 January 2005 to the day before inclusion in the LV-KOS survey. We used information on recorded diagnoses (categorized according to the International Classification of Diseases (ICD-10) [10]), prescribed medicine (categorized according to the Anatomical Therapeutic Chemical (ATC) Classification System [11,12]), and data on health services provided by general practice [13] (see Figure 1). Classification of patients for the five chronic diseases was done in the following way. Heart disease: patients were categorized to heart disease if they were registered in the Danish National Hospital Register with a diagnosis of unstable angina (ICD-10 I20) or myocardial infarction (ICD-10 I21). Diabetes: the Danish National Diabetes Register contains all patients with a final diagnosis of diabetes (ICD-10 DE10-14, DH36.0, and DO24 (excluding DO24.4), and also lists patients who meet the criteria of an algorithm for identifying diabetes [14]. Therefore, patients were categorized as having diabetes if registered in the Danish National Diabetes Register. Psychiatric disease: patients were categorized as having severe psychiatric disease if registered with a diagnosis of schizophrenia (ICD-10 F20), schizoaffective disorders (ICD-10 F25), or bipolar affective disorder (ICD-10 F30 and F31) in the Danish Psychiatric Central Registry [15]. Cancer: patients with cancer were identified through their registration in the Danish Cancer Registry [16] (ICD-10 C00-C97), excluding non-melanoma skin cancers (C44). Lung disease: patients with lung disease were defined according to a validated electronic algorithm [17] comprising ICD-10 J40-J47 or J96, or redemption of at least two prescriptions for medications with ATC codes R03AC, R03AK, R03BA, R03BB, R03CC, R03DA, or R03DC (all including sub-codes) within the past 12 months, or oxygen treatment coded with ATC code V03AN01, or at least two spirometries based on the Danish health service codes 7113 or 7121 performed within the past 12 months. Data on redeemed prescriptions were collected from the Danish National Prescription Registry [11]. A group of patients was identified with two or more of the five selected chronic diseases and designated as “2 + diagnosed”. Patients with more than one of the five chronic diseases were included in the numerator for each specific disease.
Data on outcome
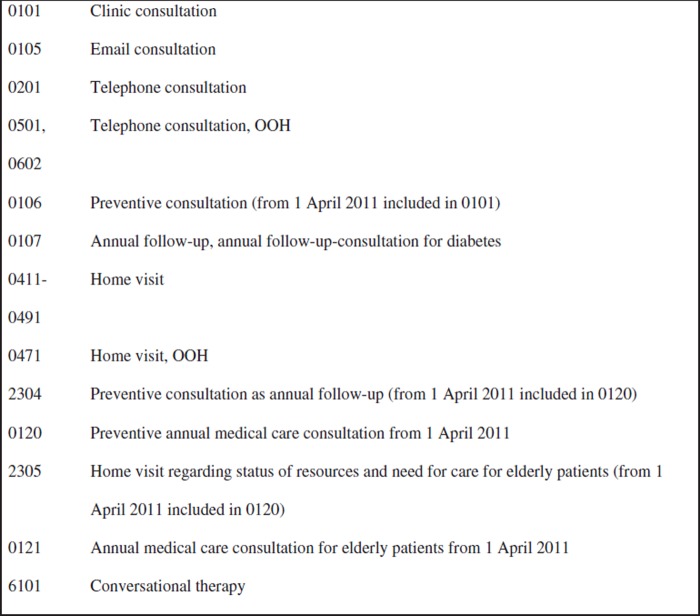
Information on the date of the index contact was obtained from the LV-KOS data. For patients with more than one contact, the first date of inclusion was used. Registry data were obtained for the time period from the index date and 30 days onwards. Data on face-to-face encounters at the OOH service or daytime general practice came from the Danish National Health Service Registry [13] and were based on the remuneration codes for services provided by general practice (Figure 2). Information on hospitalization was obtained from the Danish National Patient Registry [18] and the Danish Psychiatric Central Registry [15], while the date of death was obtained from the Danish Register of Causes of Death [19].
Figure 2.
Remuneration codes for services provided by general practice (used in this study).
Statistical analyses
The study population was divided into two groups according to the GPs’ assessment of the RFE as either “exacerbation of chronic disease” or “new health problem”. Descriptive analyses were performed for each of the five chronic diseases (irrespective of individuals with multiple diagnoses) by gender and for different age groups. Outcome measures for repeated contacts with the OOH service, contacts with the daytime GP, hospital admission, and death were calculated for each patient.
Due to the sampling method (i.e. one in 10 telephone contacts, one in three clinical consultations, and every home visit), weighted analyses using sampling weights defined as the reciprocal of the sampling fraction were performed [20].
For chronic patients with and without exacerbation, we calculated rates and rate ratios between the two groups for repeated OOH contacts, daytime contacts with general practice, hospital admissions, and deaths during the follow-up period. Patients who died during the follow-up period were excluded at the time of death. Incidence rate ratios (IRR) with corresponding 95% confidence intervals (95% CI) were assessed using a Poisson regression model with robust error variance to account for clustering at GP level.
The association between RFE and prognostic outcome after index contact was assessed using logistic regression models with robust error variance measured as odds ratios (OR) with corresponding 95% CI and adjustments for gender and age. The reference group consisted of patients without any of the five selected chronic diseases. Data were analysed using STATA /MP 12.1 (StataCorp LP, College Station, TX, USA).
Results
Outcomes were measured as contact with the OOH service, contact with the daytime GP, risk of hospital admission, and risk of death.
Repeated contact with the OOH service
Approximately 25% of the patients with severe psychiatric disease, patients with exacerbation of heart disease, and patients with 2 + diagnosis made new contacts with the OOH service during the 30 days of follow-up. In other chronic disease groups, the figures were approximately 20% or less, while this was 13% for other patients (Table I). Patients with a history of cancer and no exacerbation had the lowest number of repeated contacts with the OOH service compared with all other groups, including the remaining population (Table I). Patients with exacerbation had a significantly higher risk of repeated contacts with the OOH service during the follow-up period than patients contacting for a new health problem, and the risk was increased nearly threefold in patients with heart disease (IRR = 2.90 (95% CI 2.02;4.17)) (Table II). In comparison with patients without any of the five chronic diseases, the adjusted OR for repeated contact with the OOH during the follow-up was generally higher for patients who presented a new health problem at the index contact, in particular for patients with severe psychiatric disease (OR = 2.45 (95% CI 1.28;5.08) (Table III).
Table I.
Proportions of patients who either had a new contact with the OOH, a contact with the daytime GP, a hospital admission, or died during a 30-day follow-up after OOH contact: Distribution shows the five chronic diseases, the 2 + diagnosed, and other patients.1,2
| Heart disease n = 493 (100%) |
Lung disease n = 1654 (100%) |
Diabetes n = 1525 (100%) |
Psychiatric disease n = 355 (100%) |
Cancer n = 1490 (100%) |
2 + diagnosed n = 1126 (100%) |
Other patients n = 7696 (100%) |
Total population n = 11 897 (100%) |
|||||||||
| Exacerbation | ||||||||||||||||
| Proportion, n (%): | ||||||||||||||||
| OOH | 27 | (19.1) | 96 | (19.1) | 63 | (15.2) | 31 | (24.6) | 64 | (20.5) | 75 | (24.1) | 132 | (13.2) | 335 | (15.7) |
| Daytime GP | 109 | (74.9) | 414 | (70.6) | 277 | (71.2) | 76 | (59.1) | 235 | (68.8) | 262 | (69.5) | 639 | (64.9) | 1438 | (67.1) |
| Hospital admission | 43 | (34.5) | 139 | (25.4) | 93 | (24.0) | 45 | (30.0) | 72 | (27.2) | 90 | (3.8) | 243 | (21.7) | 520 | (23.1) |
| Death | 15 | (8.7) | 37 | (10.0) | 2 | (0.5) | 47 | (16.4) | 36 | (14.1) | 24 | (1.5) | 108 | (1.5) | 108 | (4.6) |
| New health problem | ||||||||||||||||
| Proportion, n (%): | ||||||||||||||||
| OOH | 41 | (15.6) | 137 | (14.2) | 139 | (12.0 | 43 | (24.7) | 111 | (8.7) | 85 | (21.6) | 676 | (12.8) | 1043 | (10.8) |
| Daytime GP | 248 | (67.8) | 749 | (67.3) | 851 | (72.9) | 148 | (62.9) | 813 | (69.4) | 561 | (73.5) | 3,938 | (56.2) | 6094 | (59.5) |
| Hospital admission | 87 | (32.0) | 260 | (24.1) | 305 | (27.8) | 61 | (25.7) | 72 | (26.4) | 192 | (1.6) | 1,446 | (18.5) | 2229 | (20.4) |
| Death | 29 | (9.9) | 50 | (3.49) | 62 | (4.3) | 2 | (0.2) | 85 | (6.9) | 61 | (7.3) | 81 | (0.5) | 234 | (1.4) |
Notes: 1Contact distribution-related weighted estimates (95% confidence interval). 2Patients with more than one of the five chronic diseases were included in the numerator for each specific disease; hence the sum of all diseases sum to more than the total population.
Table II.
Risk for patients with an OOH index contact due to an exacerbation for new contact with OOH, contact with daytime GP, hospital admission, or death during 30-day follow-up, distributed over the five chronic diseases, for other patients, and for the total population (shown as incidence risk rate [IRR]).
| Heart disease n = 493 (100%) |
Lung disease n = 1654 (100%) |
Diabetes n = 1525 (100%) |
Psychiatric disease n = 355 (100%) |
Cancer n = 1490 (100%) |
2 + diagnosed n = 1126 (100%) |
Other patients n = 7696 (100%) |
Total population n = 11 897 (100%) |
|||||||||
| IRRs of outcome for patients with exacerbation:1 | ||||||||||||||||
| IRR (95%CI) | ||||||||||||||||
| OOH | 2.90 | (2.02;4.17) | 1.72 | (1.38;2.15) | 2.23 | (1.74;2.87) | 2.00 | (1.32;3.03) | 2.40 | (1.90;3.04) | 2.11 | (1.68;2.71) | 2.25 | (1.91;2.64) | 2.50 | (2.24;2.79 |
| Daytime GP | 1.43 | (1.22;1.66) | 1.28 | (1.12;1.40) | 1.39 | (1.26;1.54) | 1.29 | (1.02;1.64) | 1.43 | (1.28;1.60) | 1.31 | (1.18;1.46) | 1.56 | (1.45;1.67) | 1.57 | (1.50;1.65) |
| Hospital admission | 1.11 | (0.90;1.36) | 0.99 | (0.93;1.06) | 1.00 | (0.92;1.09) | 0.98 | (0.94;1.01) | 1.04 | (0.94;1.17) | 0.95 | (0.85;1.06) | 0.99 | (0.97;1.00) | 1.01 | (0.99;1.04) |
| Death | 0.99 | (0.94;1.04) | 1.29 | (1.19;1.40) | 1.21 | (1.00;1.31) | 1.01 | (0.99;1.05) | 1.43 | (1.29;1.59) | 1.26 | (1.15;1.36) | 0.92 | (0.85;0.98) | 1.07 | (0.86;1.34) |
Note: 1 Patients who presented as “new health problem” as reference.
Table III.
Odds ratios (OR) for OOH users within each of the five disease groups for getting in contact with the healthcare system or dying during the 30-day follow-up (patients without chronic disease served as reference group).1,2
| Odds ratio (95% CI) | |||||||||||||||||||||||||||||||
| OOH | Daytime GP | Hospital admission | Death | ||||||||||||||||||||||||||||
| Crude | Adjusted3 | Crude | Adjusted3 | Crude | Adjusted3 | Crude | Adjusted3 | ||||||||||||||||||||||||
| Heart disease | |||||||||||||||||||||||||||||||
| Reference | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||||||||||
| Exacerbation | 0.17 | (0.04;0.69) | 0.32 | (0.08;1.30) | 0.90 | (0.53;1.51) | 0.67 | (0.39;1.18) | 2.27 | (1.25;4.11) | 1.64 | (0.90;3.01) | 14.98 | (5.62;39.95) | 4.71 | (1.80;12.30) | |||||||||||||||
| New health problem | 1.16 | (0.45;2.96) | 2.30 | (0.90;5.93) | 1.03 | (0.73;1.44) | 0.82 | (0.57;1.18) | 2.03 | (1.35;3.04) | 1.41 | (0.92;2.14) | 17.17 | (8.37;35.25) | 3.00 | (1.39;6.51) | |||||||||||||||
| Lung disease: | |||||||||||||||||||||||||||||||
| Reference | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||||||||||
| Exacerbation | 0.46 | (0.25;0.83) | 0.75 | (0.40;1.38) | 0.98 | (0.75;1.29) | 0.76 | (0.57;1.02) | 1.46 | (1.07;2.01) | 1.13 | (0.82;1.59) | 14.93 | (7.76;28.72) | 5.42 | (2.82;10.40) | |||||||||||||||
| New health problem | 0.94 | (0.56;1.59) | 1.27 | (0.90;1.80) | 1.08 | (0.9;1.30 | 0.93 | (0.78;1.14) | 1.36 | (1.09;1.70) | 1.18 | (0.94;1.48) | 5.57 | (3.06;5.80) | 2.03 | (1.43;2.88) | |||||||||||||||
| Diabetes: | |||||||||||||||||||||||||||||||
| Reference | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||||||||||
| Exacerbation | 0.63 | (0.19;2.09) | 1.27 | (0.37;4.36) | 0.95 | (0.69;1.31) | 0.77 | (0.55;1.09) | 1.36 | (0.90;2.03) | 1.01 | (0.67;1.52) | 17.49 | (8.76;34.93) | 5.83 | (2.74;12.39) | |||||||||||||||
| New health problem | 0.95 | (0.55;1.65) | 1.63 | (0.90;2.95) | 1.47 | (1.21;1.76) | 1.25 | (1.03;1.52) | 1.66 | (1.34;2.05) | 1.32 | (1.05;1.65) | 6.96 | (4.09;11.85) | 2.82 | (1.53;5.14) | |||||||||||||||
| Psychiatric disease: | |||||||||||||||||||||||||||||||
| Reference | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||||||||||
| Exacerbation | 0.25 | (0.09;0.70) | 0.34 | (0.12;0.96) | 0.34 | (0.19;0.61) | 0.31 | (0.17;0.57) | 1.84 | (1.03;3.29) | 1.64 | (0.91;2.94) | 0.77 | (0. 18;3.28) | 1.62 | (0.33;7.87) | |||||||||||||||
| New health problem | 2.23 | (1.08;4.63) | 2.45 | (1.18;5.08) | 0.76 | (0.53;1.08) | 0.78 | (0.51;1.05) | 1.49 | (0.98;2.26) | 1.46 | (0.95;2.25) | 0.33 | (0.0.8;1.40) | 0.81 | (0.16;4.01) | |||||||||||||||
| Cancer: | |||||||||||||||||||||||||||||||
| Reference | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||||||||||
| Exacerbation | 0.63 | (0.21;1.85) | 1.03 | (0.35;3.08) | 0.86 | (0.61;1.22) | 0.67 | (0.47;0.96) | 1.60 | (1.02;2.49) | 1.24 | (0.99;1.93) | 30.76 | (16.43;57.61) | 12.65 | (6.19;25.87) | |||||||||||||||
| New health problem | 0.58 | (0.31;1.11) | 0.90 | (0.48;1.70) | 1.35 | (1.12;1.62) | 1.06 | (0.87;1.28) | 1.54 | (1.23;1.93) | 1.23 | (0.98;1.56) | 11.67 | (7.10;19.17) | 4.06 | (2.40;6.90) | |||||||||||||||
| 2 + diagnosed: | |||||||||||||||||||||||||||||||
| Reference | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||||||||||
| Exacerbation | 0.34 | (0.15;0.79) | 0.67 | (0.29;1.58) | 0.65 | (0.46;0.92) | 0.47 | (0.33;0.69) | 2.39 | (1.59;3.59) | 1.71 | (1.12;2.61) | 25.68 | (12.97;50.86) | 8.97 | (4.55;17.68) | |||||||||||||||
| New health problem | 0.53 | (0.22;1.27) | 0.91 | (0.39;2.12) | 1.26 | (1.00;1.59) | 0.99 | (0.77;1.26) | 1.00 | (0.90;1.10) | 1.00 | (0.92;1.11) | 12.33 | (7.06;21.53) | 3.96 | (2.18;7.19) | |||||||||||||||
Notes: 1Patients without any of the five chronic diseases served as reference group. 2Contact distribution-related weighted estimates (95% confidence interval). 3Adjusted for gender and age.
Contact to the daytime GP
Fewer patients with severe psychiatric disease had a daytime GP contact during the follow-up period compared with all other groups (see Table I). Patients with exacerbation of chronic disease had a higher risk of having daytime GP contact during the follow-up period than patients with a new health problem (seeTable II). Except for patients with diabetes who presented a new health problem, patients with chronic disease had significantly lower adjusted OR for a daytime GP contact compared with patients without one of the chronic diseases; the lowest ORs were observed in patients with exacerbation of severe psychiatric disease (OR = 0.31 (95% CI 0.17;0.57) (see Table III).
Hospital admission
The risk of being hospitalized during the follow-up period did not seem to increase for 2 + diagnosed patients who had been registered with an exacerbation compared with those without exacerbation (IRR = 0.95 (95% CI 0.85; 1.06)), while the risk increased for patients with heart disease (IRR = 1.11 (95% C: 0.90;1.36)) (see Table II). Patients with chronic disease consistently had a higher OR of being hospitalized during the follow-up period compared with patients without any of the five investigated chronic diseases, although some of the results did not reach statistical significance (see Table III).
Death
More patients with exacerbation of cancer died during the follow-up period compared with all other patient groups, while only a few patients with severe psychiatric disease died (see Table I). The risk of death during the follow-up period was higher for patients with exacerbation of lung disease (IRR = 1.29 (95% CI 1.19;1.40), diabetes (IRR = 1.21 (95% CI 1.00;1.31)), or cancer (IRR = 1.43 (95% C: 1.29; 1.59)) (see Table II). For patients with exacerbation of heart disease, the OR of death was nearly fivefold higher (OR = 4.71 (95% CI 1.80;12.30) than for patients without these chronic diseases. Patients with heart disease who presented a new health problem had the highest proportion of deaths of all groups (see Table III). The OR for death was more than 12 times higher for patients with exacerbation of cancer (OR = 12.65 (95% CI 6.19;25.87) and nearly nine times higher for 2 + diagnosed patients (OR = 8.97 (95% CI 4.55;17.68)) (see Table III). The risk of death was especially high among patients aged 61 years or more (Table IV).
Table IV.
Distribution of patients who died during the 30-day follow-up period after OOH contact with respect to age, exacerbation, or new health problem, and gender.1
| Heart disease (n = 357) |
Lung disease (n = 1395) |
Diabetes (n = 1331) |
Psychiatric disease (n = 320) |
Cancer (n = 1223) |
2 + diagosed (n = 2392) |
|||||||
| All deaths | 44 | (9.6) | 87 | (4.7) | 93 | (5.5) | 4 | (0.3) | 132 | (8.7) | 97 | (9.0) |
| Age groups: | ||||||||||||
| < 60 years | 0 | (0) | 6 | (7.8) | 4 | (5.9) | 1 | (25.0) | 11 | (16.0) | 12 | (13.8) |
| 61–75 years | 10 | (10.2) | 24 | (19.3) | 25 | (15.5) | 3 | (75.0) | 49 | (28.3) | 38 | (21.0) |
| 75 + years | 34 | (89.8) | 57 | (72.9) | 64 | (78.5) | 0 | (0) | 72 | (55.7) | 90 | (65.2) |
| Exacerbation | 15 | (24.5) | 37 | (43.8) | 31 | (38.8) | 2 | (50.0) | 47 | (35.8) | 48 | (36.2) |
| New health problem | 29 | (75.5) | 50 | (56.2) | 62 | (61.2) | 2 | (50.0) | 85 | (64.2) | 92 | (63.8) |
| Gender: | ||||||||||||
| Men | 23 | (69.4) | 41 | (42.2) | 43 | (40.2) | 3 | (75.0) | 62 | (44.3) | 68 | (46.7) |
| Women | 21 | (30.6) | 46 | (57.8) | 50 | (59.8) | 1 | (25.0) | 70 | (55.7) | 72 | (53.3) |
Note: 1In numbers with corresponding contact distribution-related weighted percentage.
Discussion
Main findings
Patients with exacerbation of chronic disease had a high risk of repeated OOH use, hospitalization, and death during the 30-day follow-up period. Nevertheless, these patients were less likely to have an encounter with their daytime GP during the follow-up period than patients without chronic disease, except for patients with diabetes who more often sought daytime GP care in this period. Patients with severe psychiatric disease illness had a higher OOH use than all other patients, and a large proportion of all patients with heart disease were hospitalized during the follow-up period.
A strong association was seen between chronic disease and risk of death during the follow-up period; approximately 10% of the patients with heart disease who presented a new health problem and 10% of the patients with exacerbation of diabetes died during this period. The risk of death was especially high for patients with cancer exacerbation, which could be a consequence of worsening disease.
Strengths and weaknesses of the study
Major strengths of this study included the considerable sample size and the high validity and completeness of Danish registry data [14;21]. The study was based on comprehensive and unique data on contacts with the OOH service in a large and randomly sampled population to ensure high statistical precision. Despite the considerable population size, our cohort of adults was divided into smaller groups according to chronic disease and exacerbation. This may have affected the statistical precision in some of the estimates, although we obtained reasonable confidence intervals.
We studied five common and well-defined chronic diseases for which registrations generally have high validity and demands for healthcare frequently vary. We included only data from patients who fulfilled the inclusion criteria for our study for the five years prior to the index date. Patients diagnosed more than five years ago were assigned to the group of “other patients”. Therefore, our results may not be fully generalizable to patients diagnosed more than five years prior to the index date or to patients diagnosed with other chronic diseases.
The cohort was followed for up to 30 days without loss to follow-up. Consequently, selection bias is an unlikely explanation for our findings. The identification of adults with chronic disease was based on a correlation of CPR numbers and data from Danish health registries. We regard this procedure as the most valid method due to the high positive predictive value found for the specific diseases (as presented elsewhere) [17,22–24].
The GP-assessed information for each contact allowed us to distinguish between contact due to an exacerbation of a chronic disease and contact due to a new health problem. This information was obtained specifically for the LV-KOS survey. To our knowledge, no previous research or existing data sources contain as detailed data on OOH contacts. However, the LV-KOS data did not reveal any exhaustive information as to whether the recorded exacerbations were due to the already identified chronic disease (selected by us) or due to a competing chronic disease (unknown to us).
Findings in relation to other studies
To our knowledge, no previous studies have explored the short-time prognosis for patients with chronic disease in the OOH primary care setting as presented in the present study. In a recent Irish study among 150 elderly multi-morbid patients [25], it was found that patients with unplanned contacts with general practice in the daytime or out of hours more often had severe physical complains than patients with planned contacts with the healthcare system. In relation to our study results, these findings underline the relevance of further research in out-of-hours chronic care and identification of factors that may lead to acute medical needs.
In our study, patients with heart disease were often hospitalized and had a high 30-day mortality rate compared with all other patient groups. A former study on treatment of acute myocardial infarction (AMI) showed a higher AMI frequency among patients with a significantly shorter history of heart symptoms prior to the AMI event [26]. This might explain our results on the high proportion of patients with heart disease with repeated OOH contact and the high proportion of patients with heart disease who were hospitalized or died during the follow-up period. This calls for further studies of these two groups and their motivations for contacting the OOH service.
In a study of the use of primary care among patients with mental illness, Johansen et al. found that this group of patients had a low use of both OOH services and daytime general practice in relation to their psychiatric disease, but more often contacted psychiatric specialists [27]. They showed that increased OOH use among these patients was mostly caused by a worsening of the psychiatric disease. Our findings correspond highly with these results as we found that these patients were mostly managed by the OOH service or referred to hospital care rather than treated by the daytime GP during follow-up. This finding indicates prevention potential if GPs take a more proactive role. The high risk of hospitalization during follow-up could indicate a worsening of the psychiatric disease and the significantly higher 30-day mortality for patients with an exacerbation of severe psychiatric illness calls for further research into this particular group.
Our results show that patients with cancer use their daytime GP much more than the OOH services, which may indicate that reasonably good overall disease control is provided in the daytime. Worth et al. [28] also found a low OOH use among cancer patients, which was explained by well-functioning daytime care and a reluctance to contact OOH. Our findings showed that cancer patients with exacerbation had markedly higher OOH use than cancer patients without exacerbation. This corresponds with the findings by Worth et al., who found that the overall RFE at the OOH service was cancer-related pain. The high OR for hospital admissions among cancer patients during follow-up may call for optimization of basic palliative care for these patients.
In conclusion, the short-term prognosis for patients with chronic disease who had contacted the OOH service indicated increased need for OOH attention. Patients with one of the five investigated chronic diseases had significantly higher 30-day mortality rates than other patients.
Further research is needed to identify future OOH initiatives that may ensure better care. Our findings also call for more research in the general developments that could help establish a more proactive preventive approach to daytime care, and patients with psychiatric disease seem to require special attention.
Acknowledgements
The authors would like to thank the OOH GPs from the Central Denmark Region for their participation.
Source of funding
The project was funded by the Danish National Research Foundation for Primary Care and the Health Foundation. Mogens Vestergaard is supported by an unrestricted grant from the Lundbeck Foundation.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the contents and writing of the paper.
Ethical approval
The project was approved by the Danish Data Protection Agency (J.no. 2011-41-6365). No ethical concerns with the study were identified. According to Danish national regulations, the study did not require approval from the Committee on Health Research Ethics of the Central Denmark Region as data included only non-identifiable personal information and no biomedical intervention was performed.
References
- 1.Awlan L, Armstrong T, Cowan M. Noncommunicable diseases. Country Profiles 2011. France: World Health Organization; 2011. [Google Scholar]
- 2.Jørgensen SJ, editor. Copenhagen: Sundhedsstyrelsen; 2005. Kronisk sygdom. Patient, sundhedsvæsen og samfund [Patient, healthcare system and society] [Google Scholar]
- 3.Starfield B. The future of primary care: Refocusing the system. N Engl J Med. 2008;13:2087–91. doi: 10.1056/NEJMp0805763. [DOI] [PubMed] [Google Scholar]
- 4.Wagner EH. Academia, chronic care, and the future of primary care. J Gen Intern Med. 2010;25((Suppl 4)):636–8. doi: 10.1007/s11606-010-1442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flarup L, Moth G, Christensen MB, Vestergaard M, Olesen F, Vedsted P. Chronic-disease patients and their use of out-of-hours primary healthcare: A cross-sectional study. BMC Fam Pract. 2014;15:114–35. doi: 10.1186/1471-2296-15-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flarup L, Moth G, Christensen MB, Vestergaard M, Olesen F, Vedsted P. A feasible method to study the Danish out-of-hours primary care service. Dan Med J. 2014;61:1–5. [PubMed] [Google Scholar]
- 7.Pedersen CB, Gøtzsche H, Møller JØ, Mortensen PB. The Danish Civil Registration System. Dan Med Bull. 2006; 53:441–9. [PubMed] [Google Scholar]
- 8.Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation, and archiving. Scand J Public Health. 2011;39((7 Suppl)):12–16. doi: 10.1177/1403494811399956. [DOI] [PubMed] [Google Scholar]
- 9.Mortensen PB, Gøtzsche H, Bøcker Pedersen C, Østrup Møller J. The Danish Civil Registration System: A cohort of eight million persons. Dan Med Bull. 2006;53:441–9. [PubMed] [Google Scholar]
- 10.WHO. International statistical classification of diseases and related health problems. Tenth revison. Geneva: World Health Organization; 1992. [Google Scholar]
- 11.Kildemoes HW, Sorensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39:38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- 12.WHO. Introduction to drug utilization research. Geneva: World Health Organization; 2003. [Google Scholar]
- 13.Olivarius NdF, Hollnagel H, Krasnik A, Pedersen PA, Thorsen H. The Danish National Health Service Register. A tool for primary health care research. Dan Med Bull. 1997; 44:449–54. [PubMed] [Google Scholar]
- 14.Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K. The Danish National Diabetes Register: Trends in incidence, prevalence and mortality. Diabetologia. 2008;51:2187–96. doi: 10.1007/s00125-008-1156-z. [DOI] [PubMed] [Google Scholar]
- 15.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011; 39((7 Suppl)):54–7. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- 16.Storm HH, Michelsen EV, Clemmensen IH, Pihl J. The Danish Cancer Registry: History, content, quality and use. Dan Med Bull. 1997;44:535–9. [PubMed] [Google Scholar]
- 17.Smidth M, Sokolowski I, Kaersvang L, Vedsted P. Developing an algorithm to identify people with chronic obstructive pulmonary disease (COPD) using administrative data. BMC Med Inform Decis Mak. 2012;12:38–45. doi: 10.1186/1472-6947-12-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39((7 Suppl)):30–3. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 19.Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39((7 Suppl)):26–9. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- 20.Korn EL. Sample weights and imputation: Analysis of health surveys. Hoboken: Wiley; 1999. [Google Scholar]
- 21.Thygesen LC, Ersboll AK. Danish population-based registers for public health and health-related welfare research: Introduction to the supplement. Scand J Public Health. 2011;39((7 Suppl)):8–10. doi: 10.1177/1403494811409654. [DOI] [PubMed] [Google Scholar]
- 22.Kristensen JK, Sandbæk A, Lassen JF, Bro F, Lauritzen T. Use and validation of public data files for identification of the diabetic population in a Danish county. Dan Med Bull. 2001;48:33–7. [PubMed] [Google Scholar]
- 23.Kumler T, Gislason GH, Kirk V, Bay M, Nielsen OW, Kober L. Accuracy of a heart failure diagnosis in administrative registers. Eur J Heart Fail. 2008;10:658–60. doi: 10.1016/j.ejheart.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sorensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83–9. doi: 10.1186/1471-2288-11-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Surate Solaligue DE, Hederman L, Martin CM. What weekday? How acute? An analysis of reported planned and unplanned GP visits by older multi-morbid patients in the Patient Journey Record System database. J Eval Clin Pract. 2014;20:522–6. doi: 10.1111/jep.12171. [DOI] [PubMed] [Google Scholar]
- 26.Noman A, Ahmed JM, Spyridopoulos I, Bagnall A, Egred M. Mortality outcome of out-of-hours primary percutaneous coronary intervention in the current era. Eur Heart J. 2012; 33:3046–53. doi: 10.1093/eurheartj/ehs261. [DOI] [PubMed] [Google Scholar]
- 27.Johansen IH, Morken T, Hunskaar S. Contacts related to mental illness and substance abuse in primary health care: A cross-sectional study comparing patients’ use of daytime versus out-of-hours primary care in Norway. Scand J Prim Health Care. 2010;28:160–5. doi: 10.3109/02813432.2010.493310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Worth A, Boyd K, Kendall M, Heaney D, Macleod U, Cormie P, et al. Out-of-hours palliative care: A qualitative study of cancer patients, carers and professionals. Br J Gen Pract. 2006;56:6–13. [PMC free article] [PubMed] [Google Scholar]