Abstract
Objective. To compare the likelihood of being a frequent attender (FA) to general practice among native Norwegians and immigrants, and to study socioeconomic and morbidity factors associated with being a FA for natives and immigrants. Design, setting and subjects. Linked register data for all inhabitants in Norway with at least one visit to the general practitioner (GP) in 2008 (2 967 933 persons). Immigrants were grouped according to their country of origin into low- (LIC), middle- (MIC), and high-income countries (HIC). FAs were defined as patients whose attendance rate ranked in the top 10% (cut-off point > 7 visits). Main outcome measures. FAs were compared with other GP users by means of multivariate binary logistic analyses adjusting for socioeconomic and morbidity factors. Results. Among GP users during the daytime, immigrants had a higher likelihood of being a FA compared with natives (OR (95% CI): 1.13 (1.09–1.17) and 1.15 (1.12–1.18) for HIC, 1.84 (1.78–1.89) and 1.66 (1.63–1.70) for MIC, and 1.77 (1.67–1.89) and 1.65 (1.57–1.74) for LIC for men and women respectively). Pregnancy, middle income earned in Norway, and having cardiologic and psychiatric problems were the main factors associated with being a FA. Among immigrants, labour immigrants and the elderly used GPs less often, while refugees were overrepresented among FAs. Psychiatric, gastroenterological, endocrine, and non-specific drug morbidity were relatively more prevalent among immigrant FA compared with natives. Conclusion. Although immigrants account for a small percentage of all FAs, GPs and policy-makers should be aware of differences in socioeconomic and morbidity profiles to provide equality of health care.
Key Words: Emigrants and immigrants, general practice, health care research, morbidity, Norway, primary health care, registries, socioeconomic factors
Immigrants are a heterogeneous growing group in Europe and they seem to use primary care differently than natives.
Immigrants more often become frequent attenders, especially those coming from middle- and low-income countries.
However, elderly immigrants are underrepresented among frequent attenders in general practice.
Gastrological, endocrine, and non-specific morbidity are relatively more prevalent among immigrant frequent attenders compared with natives.
Introduction
Frequent attenders (FAs) defined as the top 10% of general practice attenders, account for up to 50% of all contacts [1,2] in general practice, disproportionately consuming the general practitioner's (GP) and patient's time [2,3] and health resources [4] but not necessarily receiving optimal health care [5] and sometimes feeling themselves to be a burden to society [6]. Despite different definitions and high heterogeneity, FAs are characterized by increasing age, female gender, low social support, living alone, unemployment, and low income [1,7]. Moreover, high rates of physical and mental disease [1,7,8] multimorbidity [1], higher drug use, and polypharmacy [9] have been reported among FAs. Being a FA might be adequate if the patient needs frequent medical advice and control or to compensate for communication difficulties, but might be a sign of the patient not obtaining the expected help [5,6,29].
The share of migrants in Europe is growing, and migration itself is beginning to be recognized as an independent social determinant of health [10]. Norwegian GPs have approximately 10% of immigrants among their patients [11,12]. Knowledge of immigrants’ health service use is therefore needed to provide better care to this heterogenic group [13]. Although a higher share of native Norwegians use primary care services compared with immigrants, there is evidence that immigrants who use primary care have more GP contacts per patient [14,15]. However, little is known about predictors for becoming a FA among immigrants compared with natives. In this study we aimed to investigate the associations between being a FA and: (i) being an immigrant, (ii) demographic and morbidity variables for natives and immigrants separately, and (iii) reason for migration and length of stay in Norway for immigrants.
Material and methods
Design, setting, and data sources
Register data for 2008 from the National Population Register (NPR), the Norwegian Health Economics Administration Database (HELFO), and the Norwegian Prescription Database (NorPD) were linked using personal identification numbers assigned to all Norwegian citizens and immigrants staying in Norway for at least six months. Access to health care services is provided similarly to natives and immigrants with an identification number.
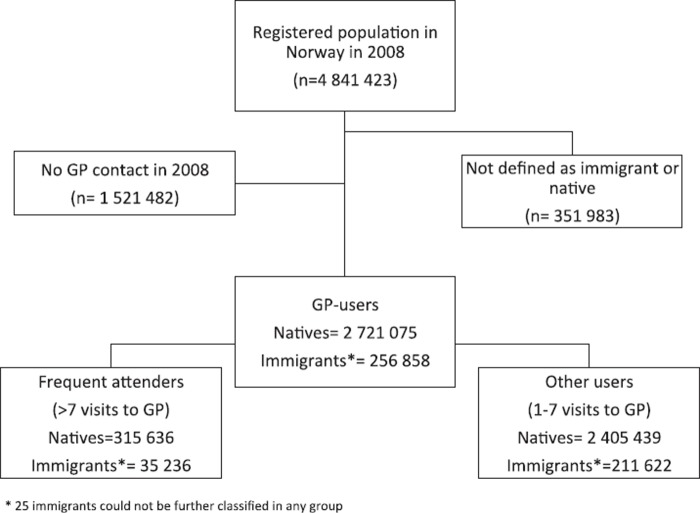
Among all registered inhabitants, those with at least one daytime visit to a GP in 2008 were included in this study and classified according to their native or immigrant background (Figure 1). Immigrants were defined as persons born abroad with both parents from abroad, and grouped according to the World Bank income categories of their country of origin into low- (LIC), middle- (MIC), and high-income countries (HIC) [16]. Natives were defined as persons born in Norway with both parents from Norway. Other combinations and 23 immigrants without country category were excluded.
Figure 1.
Flow-chart for the study population.
Variables
Information regarding gender, age, immigration category, country of origin, reason for migration (family reunification, labour, refugee, or other reasons), length of stay in Norway, place of residence (urban vs. rural or semi-rural [17]), marital status, education level (no education, low, middle or high), and income was obtained from NPR. Income information was defined as the sum of wage income and net business income during 2008 and categorized in accordance with the World Health Organization [18]: low income was defined as 60% below, and high income as 60% above the median income in the population studied. No income was reported for children and for nearly 80% of the older group.
The HELFO database contains administrative claims with International Classification of Primary Care (ICPC-2) based diagnoses for all patient contacts with a GP in Norway. Among inhabitants with at least one daytime visit to the GP in 2008 (66.9% of natives and 58.2% of immigrants), FAs were defined as patients whose attendance rate ranked in the top 10% disregarding age, gender, or other characteristics (cut-off point: > 7 visits). Other users were defined as the rest of the study population. A dichotomous pregnancy variable was created using ICPC-2 to identify women with at least one pregnancy-related diagnosis in 2008.
Data extracted from NorPD [19] comprised all drug prescriptions [20] dispensed during 2008. The Johns Hopkins University Adjusted Clinical Groups case-mix system (ACG® System) was used to organize each generic drug/route of administration combination into 19 Major Pharmacy Defined Morbidity Groups (Rx-MGs), including specific “other pharmacology groups”, according to primary anatomic-physiological system, morbidity differentiation, expected duration, and severity of the morbidity type targeted by the medication [21,22]. All 19 Rx-MGs groups were included as dichotomous variables. Additionally, the total number of unique drug/route of administration combinations for each patient was calculated.
Statistics
Descriptive analyses of the population divided into FAs and other users were followed by binary logistic regression analyses for the dependent variable FAs vs. other users. Analyses were conducted in three steps: first, including both natives and immigrants we studied the association between being immigrant and a FA; thereafter, for natives and each of the immigrant groups separately we studied the associations between demographic and morbidity variables and being a FA. Lastly, only immigrants with information on reason for migration (available since 1990 and not registered for Swedish and Danish immigrants), and length of stay in Norway were included to study the associations between these variables and being a FA.
Several logistic regression models with different adjusting variables were explored to find predictors for being a FA for immigrants and natives. Analyses were also conducted separately for both genders to be able to adjust for pregnancy. The models that best explained associations included adjustment for age categorized in four groups, gender, income level in Norway, and all Rx-MGs as 19 dichotomized variables, and are those shown in Tables I and III and Figure 1. The middle age category was chosen as reference based on exploration of the data, as FA increased with age, but the distribution of FAs in the older group was different for immigrants and natives. No income was selected as reference, as there was a clear pattern of decreasing use of GP with higher income level when studying all the population together. Education and income levels were associated and education was thus not included in the final analyses as there was a higher proportion of missing data. Pregnancy further improved the models (higher Nagelkerke R2), but it did not change the main results. For simplicity, pregnancy was only included in analyses presented by gender. All variables were included as covariates. Analyses were conducted in SPSS 20.0.
Table I.
Characteristics of the study population: Frequent attenders (FA) vs. other users for native Norwegians and high-, middle-, and low-income country immigrants.
| Natives Norway | HIC1 immigrants | MIC2 immigrants | LIC3 immigrants | |||||
| FA | Other | FA | Other | FA | Other | FA | Other | |
| Number of patients | 315 636 | 2 405 439 | 11 812 | 88 769 | 19 602 | 98 314 | 3823 | 24 371 |
| Women, % | 63.0 | 53.8 | 66.4 | 55.0 | 63.3 | 55.2 | 65.9 | 49.2 |
| Age, in years, mean (SD) | 54.5 (20.9) | 41.7 (23.4) | 50.7 (18.2) | 42.9 (18.4) | 41.8 (12.8) | 37.4 (14.8) | 36.1 (12.1) | 29.9 (14.3) |
| Married, % | 44.7 | 38.4 | 52.0 | 49.2 | 70.3 | 60.6 | 55.2 | 40.3 |
| Urban, % | 65.3 | 64.1 | 78.4 | 76.1 | 88.3 | 84.7 | 83.0 | 79.3 |
| Income level in Norway: | ||||||||
| Number with valid information | 313 619 | 2 394 603 | 11 764 | 88 430 | 19 525 | 98 018 | 3820 | 24 344 |
| No income, % | 43.6 | 37.7 | 31.4 | 25.3 | 31.7 | 31.6 | 40.2 | 43.5 |
| Low income, % | 13.2 | 14.2 | 12.1 | 12.6 | 15.1 | 17.5 | 18.1 | 21.6 |
| Middle income, % | 38.8 | 37.7 | 51.1 | 50.2 | 49.8 | 44.5 | 39.8 | 32.4 |
| High income, % | 4.4 | 10.4 | 5.5 | 11.9 | 3.4 | 6.3 | 1.8 | 2.5 |
| Education level: | ||||||||
| Number with valid information | 306 272 | 1 992 612 | 8545 | 51 784 | 14 710 | 65 902 | 2593 | 14 660 |
| No education, % | 0.1 | 0.1 | 0.6 | 0.6 | 4.1 | 2.9 | 8.7 | 5.8 |
| Low education, % | 36.3 | 29.6 | 27.1 | 23.2 | 44.9 | 42.2 | 51.4 | 54.7 |
| Middle education, % | 44.8 | 44.8 | 38.5 | 34.0 | 30.3 | 29.9 | 23.3 | 22.5 |
| High education, % | 18.8 | 25.5 | 33.8 | 42.3 | 20.7 | 24.9 | 16.7 | 17.0 |
| Immigrants, reason for migration: | ||||||||
| Number with valid information | n.a. | n.a. | 5880 | 57 117 | 12 972 | 72 051 | 3427 | 22 354 |
| Family reunification, % | n.a. | n.a. | 31.3 | 31.5 | 50.5 | 53.6 | 33.1 | 34.9 |
| Labour immigrant, % | n.a. | n.a. | 21.4 | 27.6 | 1.9 | 3.4 | 0.3 | 0.6 |
| Refugees, % | n.a. | n.a. | 9.3 | 6.2 | 43.8 | 36.7 | 63.6 | 61.0 |
| Other reasons, % | n.a. | n.a. | 38.0 | 34.7 | 3.8 | 6.2 | 3.0 | 3.5 |
| Length of stay: | ||||||||
| Years in Norway, mean | n.a. | n.a. | 22.1 | 16.0 | 15.1 | 13.0 | 8.2 | 7.1 |
| Use of services: | ||||||||
| Number of GP visits, mean (SD) | 11.8 (5.5) | 2.7 (1.7) | 11.5 (4.3) | 2.7 (1.7) | 11.7 (4.4) | 2.9 (1.8) | 11.5 (3.9) | 2.7 (1.8) |
| Percentage of all visits to the GP in Norway | 33.2 | 57.7 | 1.2 | 2.1 | 2.0 | 2.5 | 0.4 | 0.6 |
| Pregnancy: | ||||||||
| Percentage of women with a pregnancy diagnosis | 13.7 | 4.7 | 22.7 | 9.4 | 28.7 | 11.9 | 49.1 | 15.9 |
| Pharmacological treatment: | ||||||||
| Number of active ingredients, mean (SD) | 8.5 (11.8) | 3.4 (2.7) | 7.1 (11.5) | 2.8 (2.7) | 6.5 (11.7) | 2.7 (2.9) | 5.3 (11.5) | 2.0 (2.7) |
Notes: 1. HIC = high income country. 2. MIC = middle-income country 3. LIC: low-income country.
This study is part of the project “Immigrants’ health in Norway”, which was approved by the Regional Committee for Medical and Health Research Ethics. As a nationwide register study, consent was not considered necessary. The Norwegian Social Science Data Service prepared the final pseudonymized data file.
Results
The study population included 2 967 933 persons with at least one GP daytime visit in 2008 in Norway (see Figure 1). Table I gives the characteristics of the population by immigrant background for both FAs and other users. For variables with missing information, the numbers of persons entered in the analyses are included in the table. For all groups, FAs were more often women, older, married, pregnant, and lived in urban places. Other users more often had high education and high income in Norway. A higher percentage of refugees and lower percentages of both family reunification and labour immigrants were observed among FAs compared with other users. The mean number of pharmacological drugs purchased was higher for FAs compared with other users.
FAs comprised 11.6% of the native Norwegians, and 11.7% of HIC, 16.6% of MIC, and 13.6% of LIC immigrants. Binary logistic regression adjusted analyses for FA vs. other users confirmed the higher odds of all immigrants compared with natives to be FA: 1.13 (1.09–1.17) for HIC, 1.84 (1.78–1.89) for MIC, and 1.77 (1.67–1.89) for LIC men and 1.15 (1.12–1.18) for HIC, 1.66 (1.63–1.70) for MIC, and 1.65 (1.57–1.74) for LIC women.
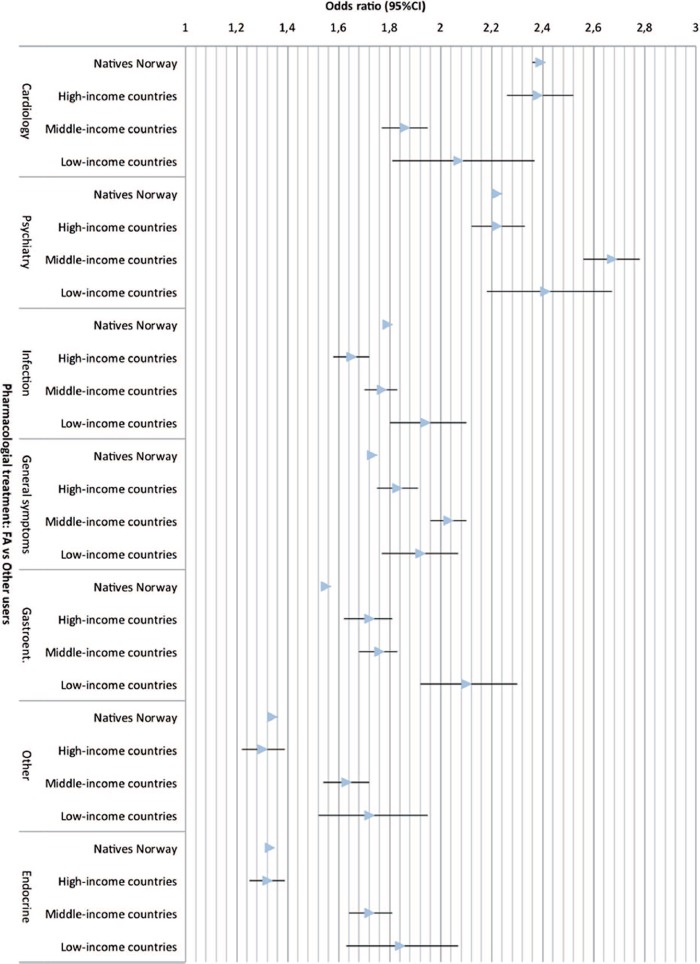
Concerning our second research question, the associations between age, gender, pregnancy, and income level and being FAs vs. other users are presented in Table II for natives and immigrants, as both crude and adjusted odds ratios (OR). For all groups, children (0–14 years old) had the lowest odds of being FAs. Being older than 65 years was also associated with lower probability of being a FA, particularly for MIC and LIC immigrants. Among women, pregnancy was the main explaining factor for all FA groups. Compared with having no income, middle income in Norway was associated with higher odds of being a FA after adjustment, while high income was a protective factor, but only for natives, HIC immigrants, and MIC men. Low income in Norway constituted a risk factor for being a FA for HIC and MIC immigrants, but was protective for Norwegians. The adjusted associations between being FA and selected Rx-MGs are depicted in Figure 2. Cardiovascular, psychiatric, infectious, and general symptoms’ pharmacological morbidity was most strongly associated with FA. There were minor differences across native and immigrant groups in the association between most Rx-MG and being a FA, except for psychiatry, gastroenterological, endocrine, and “other and non-specific” Rx-MG, which were relatively more prevalent among some immigrant FAs, and cardiology, which was less prevalent among MIC FAs.
Table II.
Association between socioeconomic characteristic and being a frequent attender for native Norwegians and high-, middle-, and low-income country immigrants: Crude and adjusted odds ratios and 95% confidence intervals.
| Native Norwegians0 | HIC1 Immigrants | MIC2 Immigrants | LIC3 Immigrants | |||||||||||||||||||||||||||||
| Women | Men | Women | Men | Women | Men | Women | Men | |||||||||||||||||||||||||
| Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | |||||||||||||||||
| Age: | ||||||||||||||||||||||||||||||||
| 0–14 years | 0.12 (0.11–0.12) | 0.51 (80.49–0.53) | 0.17 (0.16–0.18) | 0.49 (0.47–0.51) | 0.11 (0.08–0.15) | 0.56 (0.42–0.75) | 0.12 (0.09–0.16) | 0.49 (0.33–0.63) | 0.07 (0.06–0.10) | 0.49 (0.37–0.64) | 0.10 (0.08–0.13) | 0.50 (0.39–0.65) | 0.08 (0.06–0.11) | 0.40 (0.28–0.57) | 0.10 (0.08–0.14) | 0.55 (0.38–0.78) | ||||||||||||||||
| 15–44 years | 0.88 (0.87–0.89) | 1.26 (1.24–1.28) | 0.48 (0.48–0.49) | 0.95 (0.93–0.97) | 0.81 (0.77–0.86) | 0.98 (0.91–1.06) | 0.44 (0.41–0.48) | 0.87 (0.80–0.96) | 0.72 (0.89–0.75) | 0.96 (0.90–1.02) | 0.53 (0.50–0.60) | 0.97 (0.91–1.03) | 0.79 (0.70–0.90) | 0.83 (0.70–0.98) | 0.44 (0.38–0.50) | 0.89 (0.76–1.05) | ||||||||||||||||
| 45–64 years (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||||||
| 65 years and older | 1.48 (1.46–1.49) | 0.93 (0.92–0.95) | 1.99 (1.96–2,01) | 1.05 (1.02– 1.07) | 1.36 (1.27–1.46) | 0.87 (0.79–0.95) | 1.71 (1.57–1.86) | 0.89 (0.79–1.00) | 0.63 (0.56–0.70) | 0.43 (0.37–0.48) | 0.84 (0.75–0.94) | 0.62 (0.54–0.70) | 0.72 (0.50–1.01) | 0.41 (0.27–0.63) | 0.89 (0.61–1.31) | 0.58 (0.37–0.91) | ||||||||||||||||
| Income in Norway: | ||||||||||||||||||||||||||||||||
| No income (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||||||
| Low income | 0.80 (0.79–0.81) | 0.95 (0.93–0.97) | 0.80 (0.80–0.82) | 0.87 (0.85–0.89) | 0.73 (0.68–0.79) | 1.06 (0.96–1.16) | 0.85 (0.76–0.95) | 1.18 (1.03–1.34) | 0.90 (0.85–0.96) | 1.20 (1.12–1.29) | 0.78 (0.72–0.85) | 1.18 (1.07–1.31) | 1.02 (0.91–1.14) | 1.04 (0.90–1.19) | 0.87 (0.73–1.05) | 0.95 (0.78–1.18) | ||||||||||||||||
| Middle income | 0.97 (0.96–0.98) | 1.26 (1.24–1.28) | 0.74 (0.73–0.75) | 1.10 (1.08–1.13) | 0.95 (0.90–1.01) | 1.55 (1.43–1.67) | 0.67 (0.62–0.72) | 1.42 (1.26–1.59) | 1.29 (1.23–1.34) | 1.80 (1.70–1.90) | 0.95 (0.89– 1.00) | 1.69 (1.57–1.83) | 1.50 (1.36–1.66) | 1.56 (1.38–1.75) | 1.70 (1.49–1.94) | 1.86 (1.56–2.21) | ||||||||||||||||
| High income | 0.50 (0.49–0.52) | 0.71 (0.70–0.74) | 0.35 (0.34–0.36) | 0.51 (0.49–0.52) | 0.52 (0.46–0.59) | 0.84 (0.73–0.97) | 0.33 (0.29–0.34) | 0.57 (0.49–0.66) | 0.78 (0.68–0.89) | 1.06 (0.91–1.24) | 0.48 (0.43–0.54) | 0.75 (0.66–0.84) | 0.84 (0.52– 1.36) | 0.86 (0.50–1.48) | 1.24 (0.91–1.69) | 1.02 (0.72–1.44) | ||||||||||||||||
| Pregnancy: | ||||||||||||||||||||||||||||||||
| Non-pregnant (ref.) | 1 | 1 | n.a. | n.a. | 1 | 1 | n.a. | n.a. | 1 | 1 | n.a. | n.a. | 1 | 1 | n.a. | n.a. | ||||||||||||||||
| Pregnant | 3.21 (3.17–3.26) | 6.48 (6.36–6.60) | n.a. | n.a. | 2.84 (2.67–3.02) | 7.26 (6.70–7.87) | n.a. | n.a. | 2.97 (2.84–3.11) | 6.69 (6.30–7.10) | n.a. | n.a. | 5.13 (4.67–5.62) | 8.28 (7.35–9.33) | n.a. | n.a. | ||||||||||||||||
Notes: *Logistic regression. Results adjusted for all other applicable variables in the table (age, pregnancy for women, income levels) and for pharmacological treatment (all 19 major Rx-MGs). 0. Native Norwegians. Nagelkerke R2 for adjusted model: 0.254 for women, 0.255 for men. 1. HIC = high-income country. Nagelkerke R2 for adjusted model: 0.251 for women, 0.237 for men. 2. MIC = middle-income country. Nagelkerke R2 for adjusted model: 0.301 for women, 0.245 for men. 3. LIC = low-income country. Nagelkerke R2 for adjusted model: 0.351 for women, 0.258 for men. n.a. = not applicable.
Figure 2.
Major pharmacy defined morbidity groups for frequent attenders vs. other users: Adjusted results for native Norwegians and high-, middle-, and low-income country immigrants. Notes: Logistic regression. Variables in the model: gender, age-categorized income level in Norway and all 19 Major Pharmacy Defined Morbidity Groups.
To study the impact of reason for migration and length of stay on being a FA, binary logistic regression analyses including only immigrants were conducted (Table III). Compared with family reunification immigrants, labour immigrants from MIC and LIC had lower likelihood of being a FA, while refugees were at risk for being a FA (non-significant for LIC). Longer stay in Norway slightly increased the chance of being a FA for HIC immigrants.
Table III.
Association between reason for migration and length of stay and being a frequent attender for high-, middle-, and low-income country immigrants: Crude and adjusted odds ratios and 95% confidence intervals.
| HIC1 Immigrants | MIC2 Immigrants | LIC3 Immigrants | ||||
| Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | |
| Reason for migration: | ||||||
| Number included in analyses | 62 997 | 62 878 | 85 023 | 84 830 | 25 781 | 25 755 |
| Family reunification (ref.) | 1 | 1 | 1 | 1 | 1 | 1 |
| Labour | 0.78 (0.73–0.84) | 1.04 (0.95–1.13) | 0.58 (0.50–0.66) | 0.74 (0.64–0.86) | 0.50 (0.26–0.98) | 0.42 (0.20–0.86) |
| Refugees | 1.52 (1.37–1.68) | 1.63 (1.46–1.83) | 1.26 (1.22–1.31) | 1.17 (1.12–1.23) | 1.10 (1.02–1.19) | 1.07 (0.98–1.16) |
| Other | 1.11 (1.04–1.18) | 0.94 (0.87–1.01) | 0.65 (0.59–0.72) | 0.81 (0.73–0.90) | 0.92 (0.74–1.14) | 1.02 (0.81–1.29) |
| Length of stay in Norway: | ||||||
| Number included in analyses | 100 581 | 62 878 | 117 916 | 84 830 | 28 194 | 25 755 |
| 0–2 years (ref.) | 1 | 1 | 1 | 1 | 1 | 1 |
| 3 years or longer | 2.28 (2.16–2.42) | 1.10 (1.02–1.18) | 2.20 (2.07–2.33) | 1.05 (0.98–1.13) | 1.44 (1.32–1.57) | 0.92 (0.83–1.02) |
Notes: *Logistic regression. Results adjusted for gender, age-categorized income in Norway, pharmacological treatment (all 19 major Rx-MGs), and other variables in the table (reason for migration and length of stay in Norway). 1. HIC = high-income country. Nagelkerke R2 for adjusted model: 0.198. 2. MIC = middle-income country. Nagelkerke R2 for adjusted model: 0.230. 3. LIC = low-income country. Nagelkerke R2 for adjusted model: 0.254.
Discussion
Principal findings
Our study states the higher odds of immigrants compared with native Norwegians of becoming a FA once they have been in contact with general practice in the daytime. Although there were differences between immigrants, common to most of them was that the elderly, labour immigrants, and those earning a high income used general practice less often, while pregnant women, refugees, and those earning a middle income were overrepresented among FAs, after adjusting for pharmacologic-based morbidity and other socioeconomic factors. Some immigrant FAs had relatively lower prevalence of cardiologic problems, which were the most prevalent pharmacological risk factors for Norwegians, while psychiatry, gastroenterological, endocrine, and “other and non-specific” pharmacy groups were more prevalent among immigrant compared with native FAs.
Strengths and weaknesses
The main strengths of our study are the nationwide coverage, with inclusion of all registered immigrants and no selection bias, the inclusion of information on both morbidity burden and socioeconomic factors, and the possibility to differentiate immigrants according to their origin. Our definition of frequent attendance as the top 10% of attenders at general practice is discriminative from normal attenders in terms of patient characteristics compared with broader definitions [2]. However, we explored several limits (including more than eight visits), but more than seven was the number that came nearer to 10% of the whole population. Results in this paper would nevertheless have not changed using narrower definitions. Our study has some weaknesses too. We have no data for undocumented immigrants. The NorPD contains information on prescription drugs purchased, not on actual drug use. However, the use of purchased medication as a proxy for consumption is recognized in epidemiology [23]. Also, although the ACG System and Rx-MCG are validated as morbidity burden adjusting risk measurements [24–26], they are not culturally validated. Our results cannot reflect prevalence of illnesses, as they do not address non-pharmacological treatment or those not seeking help.
Findings in relation to other studies
To our knowledge, immigrant background among FAs has not been studied before. As previously described in the general population [1,7], increasing age was associated with being a FA for most groups before adjustment. However, taking into account morbidity burden and other explanatory variables, our study revealed that some of the eldest immigrant groups had nearly half the likelihood of being FA compared with middle-aged patients.
According to previous studies [1,7], females were overrepresented among FAs. However, this association was much weaker when adjusting for pregnancy (results not shown). Although some FA studies exclude pregnant women [1], we aimed to explore demographic differences between groups, and thus chose to keep pregnant women and present results by gender for some analyses, showing that pregnancy is crucial but does not alone explain differences between native and immigrant FAs.
While other studies have related unemployment and low-income status to being a FA [1,7], our adjusted results indicated that high income was mainly protective, but middle income in Norway represented a risk factor for being a FA. The fact that some low and no income groups and elderly immigrants, especially females, had lower odds of being a FA could be a sign of the “inverse care law” [27], representing underuse among vulnerable groups, and should be targeted in primary care policies.
The most relevant pharmacy groups in our study are already described among FAs in the previous literature: antibiotics, analgesics, psychotropic, cardiovascular, and gastrointestinal drugs [5,8,9]. Also, high prevalence of medically unexplained symptoms [28] and high use of antidiabetics have been previously described among non-Western immigrants who often visit their GP. Relative differences in pharmacological morbidity between immigrant and native FAs versus other users should be further investigated.
Meaning of the study
Among general practice users, immigrants have a higher likelihood of being a FA compared with natives. A patient can become a FA because of his/her own perception of health care need and satisfaction with care given [30], because of the GP's own capability of dealing with some types of patients [31], or because of system factors [8,14]. GPs should consider that consultations with immigrants and natives might be different in some of these three regards. Further research should explore the adequacy of the attendance of FAs according to the patient's immigrant background.
Acknowledgments
The corresponding author had a travel stipend grant from Meltzer Research Fund.
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
References
- 1.Vedsted P, Christensen MB. Frequent attenders in general practice care: A literature review with special reference to methodological considerations. Public Health. 2005;119:118–37. doi: 10.1016/j.puhe.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Smits FT, Brouwer HJ, ter Riet G, van Weert HC. Epidemiology of frequent attenders: A 3-year historic cohort study comparing attendance, morbidity and prescriptions of one-year and persistent frequent attenders. BMC Public Health. 2009;9:36. doi: 10.1186/1471-2458-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hauswaldt J, Hummers-Pradier E, Junius-Walker U. Health service use among patients with chronic or multiple illnesses, and frequent attenders: Secondary analysis of routine primary care data from 1996 to 2006. Deutsches Arzteblatt Int. 2012;109:814–20. doi: 10.3238/arztebl.2012.0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smits FT, Brouwer HJ, Zwinderman AH, Mohrs J, Smeets HM, Bosmans JE, et al. Morbidity and doctor characteristics only partly explain the substantial healthcare expenditures of frequent attenders: A record linkage study between patient data and reimbursements data. BMC Fam Pract. 2013;14:138. doi: 10.1186/1471-2296-14-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spence D. Frequent attenders are getting poor care. BMJ. 2014;348:g208. doi: 10.1136/bmj.g208. [DOI] [PubMed] [Google Scholar]
- 6.Wiklund-Gustin L. Struggling on my own: A cognitive perspective on frequent attenders’ conception of life and their interaction with the healthcare system. Psychiatry J. 2013; 2013:580175. doi: 10.1155/2013/580175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gill D, Sharpe M. Frequent consulters in general practice: A systematic review of studies of prevalence, associations and outcome. J Psychosom Res. 1999;47:115–30. doi: 10.1016/s0022-3999(98)00118-4. [DOI] [PubMed] [Google Scholar]
- 8.Morriss R, Kai J, Atha C, Avery A, Bayes S, Franklin M, et al. Persistent frequent attenders in primary care: Costs, reasons for attendance, organisation of care and potential for cognitive behavioural therapeutic intervention. BMC Fam Pract. 2012;13:39. doi: 10.1186/1471-2296-13-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vedsted P, Sorensen HT, Mortensen JT. Drug prescription for adult frequent attenders in Danish general practice: A population-based study. Pharmacoepidemiol Drug Saf. 2004;13:717–24. doi: 10.1002/pds.939. [DOI] [PubMed] [Google Scholar]
- 10.Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381:1235–45. doi: 10.1016/S0140-6736(12)62086-8. [DOI] [PubMed] [Google Scholar]
- 11.Statistics Norway S. Immigrants and their descendants, 1 January 2013. Available at http://www.ssb.no/innvbef (accessed February 2014)
- 12.Diaz E, Raza A, Hjorleifsson S, Sandvik H. Immigrant and native regular general practitioners in Norway: A comparative registry-based observational study. Eur J Gen Pract. 2013:1–7. doi: 10.3109/13814788.2013.823600. Early online. [DOI] [PubMed] [Google Scholar]
- 13.Rehabilitering Mo., editor. Oslo: Helsedirektoratet; 2012. Nasjonal Strategi om Innvandreres helse 2013–2017 [Norwegian National Strategy Document on Immigrant Health] [Google Scholar]
- 14.Nørredam M, Nielsen SS, Krasnik A. Migrants’ utilization of somatic healthcare services in Europe: A systematic review. Eur J Public Health. 2010;20:555–63. doi: 10.1093/eurpub/ckp195. [DOI] [PubMed] [Google Scholar]
- 15.Diaz E, Calderón-Larrañaga A, Prado-Torres A, Poblador-Plou B, Gimeno-Feliu L-A. How do immigrants use primary healthcare services? A register-based study in Norway. Eur J Public Health. 2014 doi: 10.1093/eurpub/cku123. In press. [DOI] [PubMed] [Google Scholar]
- 16.World Bank. New country classifications, 2013. Available at http://data.worldbank.org/news/new-country-classifications (accessed February 2014)
- 17.Statistics Norway S. Classification of centrality, 2013. Available at http://www.ssb.no/metadata/conceptvariable/vardok/927/en (accessed February 2014)
- 18.European Commission. Research findings – social situation monitor – risk of poverty on basis of different thresholds. Available at http://ec.europa.eu/social/main.jsp?catId = 1050&intPageId = 1894&langId = en (accessed February 2014)
- 19.Furu K. Establishment of the nationwide Norwegian Prescription Database (NorPD) – new opportunities for research in pharmacoepidemiology in Norway. Norw J Epidemiol. 2008;18:129–36. [Google Scholar]
- 20.Collaborating Centre for Drug Statistics Methodology. Available at http://www.whocc.no/atc_ddd_index/ (accessed February 2014)
- 21.Weiner JP. Technical Reference Guide Version 10.0. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; 2011. The Johns Hopkins ACG System. [Google Scholar]
- 22.Kuo RN, Lai MS. Comparison of Rx-defined morbidity groups and diagnosis- based risk adjusters for predicting healthcare costs in Taiwan. BMC Health Serv Res. 2010;10:126. doi: 10.1186/1472-6963-10-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication in primary care. BMJ. 1993;307:846–8. doi: 10.1136/bmj.307.6908.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orueta JF, Nuno-Solinis R, Mateos M, Vergara I, Grandes G, Esnaola S. Predictive risk modelling in the Spanish population: A cross-sectional study. BMC Health Serv Res. 2013;13:269. doi: 10.1186/1472-6963-13-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sibley LM, Moineddin R, Agha MM, Glazier RH. Risk adjustment using administrative data-based and survey- derived methods for explaining physician utilization. Med Care. 2010;48:175–82. doi: 10.1097/MLR.0b013e3181c16102. [DOI] [PubMed] [Google Scholar]
- 26.Huntley AL, Johnson R, Purdy S, Valderas JM, Salisbury C. Measures of multimorbidity and morbidity burden for use in primary care and community settings: A systematic review and guide. Ann Fam Med. 2012;10:134–41. doi: 10.1370/afm.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hart JT. The inverse care law. Lancet. 1971;1:405–12. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 28.Verhaak PF, Meijer SA, Visser AP, Wolters G. Persistent presentation of medically unexplained symptoms in general practice. Fam Pract. 2006;23:414–20. doi: 10.1093/fampra/cml016. [DOI] [PubMed] [Google Scholar]
- 29.Lyratzopoulus G, Neal RD, Barbiere JM, Rubin GP, Abel GA. Variation in the number of general practitioner consultations before hospital referral for cancer: Findings from a the 2010 National Cancer Patient Experience Survey in England. Lancet Oncology. 2012;13:353–65. doi: 10.1016/S1470-2045(12)70041-4. [DOI] [PubMed] [Google Scholar]
- 30.Lien E, Nafstad P, Rosvold EO. Non-western immigrants’ satisfaction with the general practitioners’ services in Oslo, Norway. Int Journal Equity Health. 2008;7:7. doi: 10.1186/1475-9276-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varvin S, Aasland OG. Legers forhold til flyktningpasienten [Doctors’ relationships to refugee patients] Tidsskrift for den Norske Legeforening. 2009;129:1488–90. doi: 10.4045/tidsskr.08.0212. [DOI] [PubMed] [Google Scholar]