Abstract
A real-time PCR assay was developed to diagnose and identify the causative agents of suspected mycobacterial lymphadenitis. Primers and probes for the real-time PCR were designed on the basis of the internal transcribed spacer sequence, enabling the recognition of the genus Mycobacterium and the species Mycobacterium avium and M. tuberculosis. The detection limit for the assay was established at 1,100 CFU/ml of pus, and the specificity tests showed no false-positive reaction with other mycobacterial species and other pathogens causing lymphadenitis. From 67 children with suspected mycobacterial lymphadenitis based on a positive mycobacterial skin test, 102 samples (58 fine-needle aspirates [FNA] and 44 tissue specimens) were obtained. The real-time PCR assay detected a mycobacterial infection in 48 patients (71.6%), whereas auramine staining and culturing were positive for 31 (46.3%) and 28 (41.8%) of the patients. The addition of the real-time PCR assay to conventional diagnostic tests resulted in the recognition of 13 more patients with mycobacterial disease. These results indicate that the real-time PCR is more sensitive than conventional staining and culturing techniques (P = 0.006). The M. avium-specific real-time PCR was positive for 38 patients, and the M. tuberculosis-specific real-time PCR was positive for 1 patient. Analysis of 27 patients from whom FNA and tissue biopsy specimens were collected revealed significantly more positive real-time PCR results for FNA than for tissue biopsy specimens (P = 0.003). Samples from an age-matched control group of 50 patients with PCR-proven cat scratch disease were all found to be negative by the real-time PCR. We conclude that this real-time PCR assay with a sensitivity of 72% for patients with lymphadenitis and a specificity of 100% for the detection of atypical mycobacteria can provide excellent support for clinical decision making in children with lymphadenitis.
Nontuberculous mycobacterial (NTM) lymphadenitis appears to be an emerging disease in children (6, 13). The portals of entry are the pharyngeal mucosa, tonsils, conjunctiva, gingiva, salivary glands, and skin (7, 14). Cervicofacial lymphadenitis, the most frequent head and neck manifestation of NTM infection, often presents as chronic, unilateral lymphadenopathy with characteristic violaceous overlying skin changes. It may be difficult to differentiate NTM lymphadenitis from lymphadenitis caused by other microorganisms, such as staphylococci, streptococci, and Bartonella species. The Mycobacterium avium complex accounts for 80% of NTM lymphadenitis cases, followed by M. scrofulaceum in the United States and M. malmoense in Europe (1, 8). The exact incidence of NTM lymphadenitis in children in The Netherlands is unknown but is estimated to be 0.4 patients per 100,000 inhabitants annually.
Currently, the most commonly used treatment for NTM lymphadenitis is excision of the infected lymph node. Surgery is preferred because of a higher risk of sinus tract formation or recurrence of infection when other conservative therapies are used (1, 14, 20, 21). A number of recent case reports, however, suggested that effective treatment of NTM lymphadenitis is possible with specific antimycobacterial agents (2, 17, 29). Since culture results for mycobacteria can take as long as 12 weeks, a rapid diagnostic technique is required to institute appropriate antimycobacterial therapy.
Several molecular assays have been developed for the detection or identification of mycobacteria, but most of them are for M. tuberculosis only (5, 11, 19, 27, 31). The existing molecular methods for the identification of atypical mycobacteria are mainly applied on cultured mycobacteria and lack specificity or sensitivity when used directly on clinical materials (15, 18, 24). A real-time PCR technique for the detection of mycobacteria is able to detect a specific sequence during amplification and needs no hybridization or further processing time for analysis. It is easy to use and able to attain high sensitivity mainly because of the use of short amplicons.
In this study, a real-time PCR assay for the genus Mycobacterium and the mycobacterial species M. avium and M. tuberculosis was developed for direct use on fine-needle aspirates (FNA) and biopsy specimens from patients with suspected mycobacterial lymphadenitis. The target chosen for PCR was the internal transcribed spacer (ITS) sequence between the 16S and the 23S rRNA genes. The ITS contains sufficient sequence variations to differentiate mycobacterial species (23, 24) but is still conserved enough to allow the development of a genus Mycobacterium-specific PCR for the detection of all species possibly involved in lymphadenitis.
(Part of this study was presented at the 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, Ill. [L. Bruijnesteijn V. C., J. A. Lindeboom, J. M. Prins, E. C. J. Claas, E. J. Kuijper, Abstr. 43rd ICAAC, abstr. D-1880, p. 192, 2003].)
MATERIALS AND METHODS
Bacterial strains.
The mycobacterial strains used for sensitivity and specificity testing and for optimization of PCR are listed in Table 1. The strains were either ATCC strains or clinical isolates, identified by 16S RNA sequencing and obtained from the Medical Microbiological Laboratory (Leiden University Medical Center, Leiden, The Netherlands), the Regional Public Health Laboratory (Leeuwarden, The Netherlands; supplied by G. Noordhoek), and the National Institute of Public Health and the Environment (Bilthoven, The Netherlands). All mycobacterial strains were cultured in liquid Dubos medium. Additionally, 36 strains belonging to 28 different species were also used in specificity tests. Some of these species are established pathogens causing lymphadenitis, and others are normal inhabitants of the oropharynx. The species belonged to the genera Streptococcus, Staphylococcus, Bordetella, Haemophilus, Neisseria, Chlamydia, Bartonella, Campylobacter, Legionella, and Corynebacterium and to the family Enterobacteriaceae.
TABLE 1.
Reference strains and clinical isolates used in this study and results of real-time PCR
| Straina | Real-time PCR resultsb for:
|
||
|---|---|---|---|
| Genus Mycobacterium | M. avium | M. tuberculosis | |
| M. intracellulare LUMC 5 | + | − | − |
| M. intracellulare LUMC 7 | + | − | − |
| M. intracellulare ATCC 13950 | + | − | − |
| M. avium LUMC 14 | + | + | − |
| M. avium subsp. silvaticum LUMC 18 | + | + | − |
| M. avium subsp. avium RIVM D71076 | + | + | − |
| M. avium subsp. avium RIVM 160/74 | + | + | − |
| M. avium subsp. avium RIVM R13 | + | + | − |
| M. avium subsp. paratuberculosis ATCC 19698 | + | + | − |
| M. avium subsp. paratuberculosis ATCC 43544 | + | + | − |
| M. scrofulaceum RIVM 2002-530 | + | − | − |
| M. scrofulaceum RIVM 2002-1933 | + | − | − |
| M. tuberculosis ATCC 35822 | + | − | + |
| M. bovis LUMC 1 | + | − | + |
| M. kansasii ATCC 12478 | + | − | − |
| M. kansasii LUMC 30 | + | − | − |
| M. kansasii LUMC 31 | + | − | − |
| M. kansasii LUMC 32 | + | − | − |
| M. xenopi LUMC 59 | + | − | − |
| M. xenopi LUMC 60 | + | − | − |
| M. malmoense M 2148 | + | − | − |
| M. malmoense M 2240 | + | − | − |
| M. malmoense M 1172 | + | − | − |
| M. haemophilum LUMC 201 | + | − | − |
| M. fortuitum LUMC 101 | + | − | − |
| M. gordonae ATCC 14470 | + | − | − |
| M. marinum LUMC 48 | + | − | − |
LUMC, Leiden University Medical Center; ATCC, American Type Culture Collection; RIVM, National Institute of Public Health and the Environment; M, Regional Public Health Laboratory. Identification of clinical strains was performed at RIVM.
+, positive; −, negative.
RIVM strains.
Patients and samples.
Samples from affected lymph nodes were obtained from patients included in the CHIMED study. The CHIMED study is a multicenter trial in The Netherlands for studying the optimal treatment of children with NTM cervicofacial lymphadenitis. Surgical excision is compared to an antimicrobial treatment consisting of clarithromycin and rifabutin. To be eligible, patients must have a positive skin test for atypical mycobacteria (29, 30). Differential skin testing with sensitins for M. avium, M. scrofulaceum, and M. kansasii and purified protein derivative (Statens Seruminstitut, Copenhagen, Denmark) consists of two simultaneous injections each on the middle part of the ventral surface and on the dorsal surface of the right forearm.
From September 2001 until November 2003, 67 patients with affected lymph nodes in the neck were included in the study. FNA were taken from affected lymph nodes and transported in saline to the microbiological laboratory at Leiden University Medical Center. The lymph nodes removed from surgically treated patients were also investigated. Clinical samples arrived at the laboratory within 6 h. All samples were kept at 4°C until processing. An age-matched control group consisted of 50 patients with affected lymph nodes. Cat scratch disease was diagnosed by Bartonella henselae-specific PCR of samples from these affected lymph nodes at the Department of Medical Microbiology, St. Elisabeth Hospital, Tilburg, The Netherlands (3).
Conventional mycobacterial diagnostic tests.
Patient samples were tested for contamination with rapidly growing bacteria by culturing on standard brain heart infusion agar. When contamination was found, the aspirates or biopsy specimens were decontaminated with an NaCl-NaOH decontamination protocol (12). Auramine staining was performed on directly obtained materials or on decontaminated materials for the detection of acid-fast rods. When auramine-positive rods were detected, Ziehl-Neelsen staining was performed to confirm the presence of acid-fast rods. Culturing was done at 35°C by using Bactec bottles with liquid mycobacteria growth indicator tube (MGIT) (Becton Dickinson Microbiology Systems) medium and on solid Löwenstein-Jensen medium. Positive culture results for acid-fast bacteria were further investigated by using the Inno-Lipa assay (InnoGenetics, Gent, Belgium), a reverse hybridization assay in which the mycobacterial species is identified. When no growth was detected after 12 weeks of incubation, the culture results were listed as negative. Samples were also investigated for the presence of other bacterial pathogens by conventional bacterial culturing and by PCR for B. henselae (3).
Nucleic acid isolation for real-time PCR.
Aliquots of the clinical samples used for PCR were first decontaminated with the NaCl-NaOH method. DNA from cultured strains was extracted without decontamination. Each patient sample was divided into three aliquots. One aliquot was spiked with 2.5 × 104 CFU of M. bovis and used as a control for DNA extraction and PCR inhibition. The other two aliquots were tested as duplicates of the patient sample. Extraction of DNA for the real-time PCR was performed as described by Boom et al. (4). Briefly, 90 μl of decontaminated material or bacterial culture was extracted, and the DNA was eluted in 100 μl of Tris-EDTA (0.1 M; pH 8.0). The extracted DNA was stored at −20°C until used in the PCR.
Primers and probes.
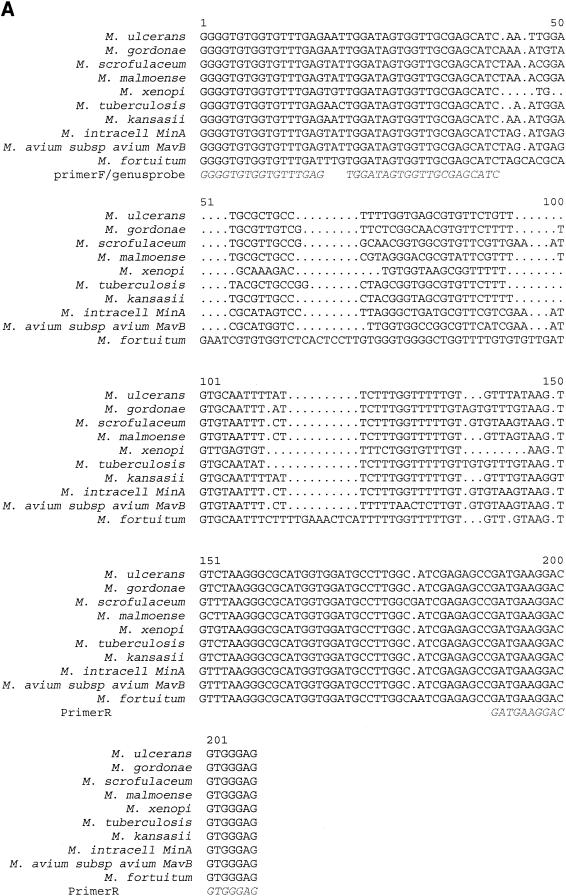
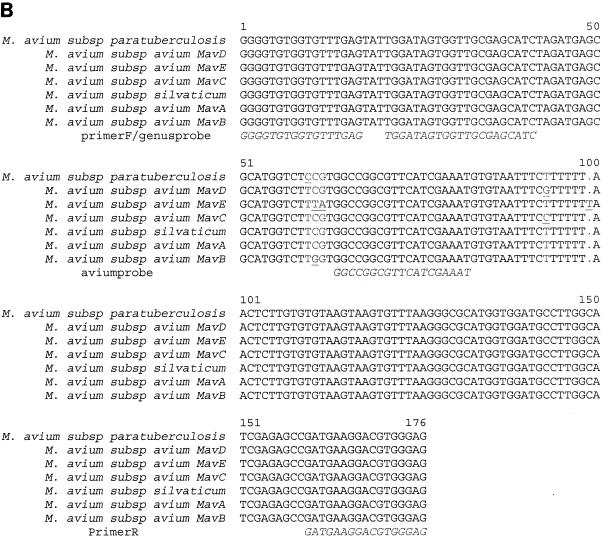
Primers were selected based on alignments of the ITS region with sequences from the National Center for Biotechnology Information (NCBI) database (http://www.ncbi.nlm.nih.gov) and the Ridom GmbH database (http://www.ridom.com) and sequences derived from clinical isolates. Sequence alignments were made to investigate the interspecies variations and the intraspecies variations. The alignments included all three subspecies of M. avium and five sequevars of M. avium (A, B, C, D, and E). From these alignments, conserved regions were used to select primers specific for the genus Mycobacterium. The forward primer was selected from the ITS region; the reverse primer was selected from the 23S rRNA gene (Fig. 1). Another small conserved sequence in the ITS region was used for the Taqman probe specific for the genus Mycobacterium. The larger part of the ITS region contains a high degree of variation; probes specific for M. avium (molecular beacon) and M. tuberculosis (Taqman probe) were designed from this part (Fig. 1B). The choice of a molecular beacon or a Taqman probe was based on the overall stability of the secondary structures in the probe sequence.
FIG. 1.
(A) Alignment of ITS fragments used in the real-time PCR assay of various mycobacterial species. M. intracell, M. intracellulare. (B) Alignment of ITS fragments used in the real-time PCR assay of M. avium strains.
The PCR primer and probe sequences were selected by using the Primer3 program (http://www-genome.wi.mit.edu/cgi-bin/primer/primer3_www.cgi) (25) and were checked with Oligo-Analyzer 3.0 (http://biotools.idtdna.com/analyzer), an online service of IDT Biotools (Coralville, Iowa), to ensure minimal self-complementarity and to prevent the presence of secondary structures.
The molecular beacon for M. avium was designed by using the Mfold program (http://biotools.idtdna.com/mfold) (IDT Biotools). Additional criteria for a good probe included a melting temperature at least 7°C above the melting temperatures of the primers and a relatively short amplicon, with a maximum of 200 nucleotides. The stem sequence of the molecular beacon was selected to have a melting temperature compatible with that of the beacon. The beacon formed a stable structure at the proposed annealing temperature of 55°C, with no secondary structures (26). An NCBI BLAST search was performed to check the specificity of the DNA sequences of the primers and probes. Primers were synthesized at Eurogentec (Seraing, Belgium), and probes were synthesized at Biolegio (Malden, The Netherlands). Selected primers and probes are shown in Table 2.
TABLE 2.
Sequences of oligonucleotides used in this study
| Primer or probe | Sequence (5′-3′) |
|---|---|
| Forward primer | GGGGTGTGGTGTTTGAG |
| Reverse primer | CTCCCACGTCCTTCATC |
| Mycobacterium-specific Taqman probe | Fam-TGGATAGTGGTTGCGAGCATC-Tamra |
| M. avium-specific molecular beacon | Fam-CCCACCGGCCGGCGTTCATCGAAATGGTGGG-DabCyl |
| M. tuberculosis-specific Taqman probe | Hex-GCTAGCCGGCAGCGTATCCAT-BHQ1 |
Sensitivity testing.
Quantified dilutions of M. avium and M. bovis were prepared by measuring optical density (spectrophotometry) and CFU. Aliquots of 20 μl, containing serial dilutions of 110 to 107 CFU/ml, were added to water and pooled pus samples. The influence of decontamination on the sensitivity of the assay was investigated by comparing decontamination before spiking with decontamination after spiking.
Real-time PCR.
The real-time PCR was performed with a 50-μl reaction mixture consisting of 25 μl of 2× IQ Supermix (Bio-Rad, Veenendaal, The Netherlands), 3.0 mM MgCl2, 20 pmol of each primer, 10 pmol of probe, and 10 μl of template. The PCR thermal profile consisted of an initial incubation for 3 min at 95°C, followed by 50 cycles of 30 s at 95°C, 40 s at 55°C, and 30 s at 72°C (the annealing temperature for the M. tuberculosis-specific PCR was 52°C instead of 55°C). Amplification, detection, and data analysis were performed with an iCycler IQ real-time detection system (Bio-Rad). The same reaction mixture and the same PCR profile were used for all three probes.
Each DNA extract was tested undiluted and diluted 10-fold by the real-time PCR for detection of the genus Mycobacterium and the species M. avium. For the M. avium-specific PCR, M. avium DNA was used as a positive control instead of M. bovis DNA.
Statistical analysis.
All statistical calculations were performed with SPSS 10.0.7. The Wilcoxon signed rank test was used for a comparison of FNA and tissue biopsy specimens from patients from whom both materials were collected. For other calculations, a chi-square test was used.
RESULTS
Test characteristics in vitro.
Quantified dilutions of M. avium and M. bovis were tested in water and pooled pus samples. All three real-time PCRs reached a sensitivity of 2.7 CFU when spiked in water and a sensitivity of 27 CFU when spiked in pus, establishing a detection limit for the assay of 1,100 CFU/ml of pus. The sensitivity of the assay was not influenced by the decontamination protocol.
The specificity was assessed with DNA from 11 mycobacterial species (Table 1) and 36 other human pathogens. Several pathogens that may cause lymphadenitis, such as Staphylococcus aureus, Streptococcus pyogenes, Nocardia spp., and Bartonella spp., were also included in this specificity testing. No nonspecific results were obtained in the genus Mycobacterium-specific PCR. The M. tuberculosis-specific PCR detected only M. tuberculosis and M. bovis. The M. avium-specific PCR recognized seven isolates belonging to all three subspecies of M. avium and was negative for M. scrofulaceum, M. intracellulare, and other species tested (Table 1).
Patient samples.
From 67 patients included in the CHIMED study, 102 samples were obtained (58 FNA and 44 tissue specimens) (Table 3). Auramine staining was positive for 31 patients (46.3%). Mycobacteria could be cultured from 28 patients (41.8%) and included M. avium (n = 22), M. malmoense (n = 2), M. kansasii (n = 1), M. tuberculosis (n = 1), and Mycobacterium spp. (n = 2). The real-time PCR assay detected a mycobacterial infection in 48 patients (71.6%). The M. avium-specific real-time PCR was positive for 38 patients, and the M. tuberculosis-specific real-time PCR was positive for 1 patient (Table 3). The remaining nine PCR-positive patients were found to be positive only by the genus-specific real-time PCR. The real-time PCR assay was more sensitive for the detection of atypical mycobacteria in patients with lymphadenitis than were staining and culturing (P value determined by the chi-square test, 0.006). When all tests were combined, the diagnosis of mycobacterial infection could be verified for 55 (82.1%) of 67 patients. The mycobacterial species was not identified for 12 of these 55 patients, because the samples were found to be positive only by the genus Mycobacterium-specific PCR (n = 8) or only by auramine staining (n = 2) or because the cultured species could not be identified by the reverse line blot assay (n = 2). Samples from the age-matched control group of 50 patients were all found to be negative by the real-time PCR.
TABLE 3.
Results of real-time PCR, auramine staining, and mycobacterial culturing of FNA and tissue samples from 67 patients with suspected NTM lymphadenitis
| Positive diagnostic test | Total no. (%) of:
|
|
|---|---|---|
| Patients (n = 67) | Samples (n = 102) | |
| Auramine staining | 31 (46.3) | 38 (37.3) |
| Mycobacterial culturing | 28 (41.8) | 35 (34.3) |
| Real-time PCR | 48 (71.6) | 68 (66.7) |
| Genus specific | 45 (67.2) | 59 (57.8) |
| M. tuberculosis specific | 1 (1.5) | 1 (1.0) |
| M. avium specific | 38 (56.7) | 53 (52.0) |
| Any test | 55 (82.1) | 76 (74.5) |
The results indicated higher recovery from FNA than from tissue specimens from lymph nodes obtained during surgical excision or biopsy (Table 4). For 27 patients from whom FNA and tissue biopsy specimens were collected, specific real-time PCRs for the genus Mycobacterium and the species M. avium both yielded significantly more positive results for FNA than for tissue biopsy specimens (P values determined by the Wilcoxon test, 0.001 and 0.0011, respectively). Tissue biopsy specimens never were found to be positive by the real-time PCR when FNA were found to be negative. Although acid-fast staining and culture results were also more frequently positive for FNA than for surgically removed tissue (no statistical significance), tissue biopsy specimens yielded three more positive results when only conventional diagnostic tests were applied for patients from whom both materials were obtained (Table 4).
TABLE 4.
Results of diagnostic tests of materials from 27 patients from whom both FNA and tissue biopsy specimens were collected
| Diagnostic test | No. (%) of patients with the following test results for FNA and excisional biopsy specimens:
|
|||
|---|---|---|---|---|
| FNA +, biopsy + | FNA +, biopsy − | FNA −, biopsy + | FNA −, biopsy − | |
| Auramine staining | 8 (29.6) | 6 (22.2) | 3 (11.1) | 10 (37.0) |
| Mycobacterial culturing | 6 (22.2) | 5 (18.5) | 2 (7.4) | 14 (51.9) |
| Real-time PCR assaya | 16 (59.3) | 9 (33.3) | 0 | 2 (7.4) |
| M. avium specific | 12 (44.4) | 9 (33.3) | 1 (3.7) | 5 (18.5) |
| Genus specific | 10 (37.0) | 13 (48.1) | 1 (3.7) | 3 (11.1) |
| Any positive diagnostic test | 16 (59.3) | 9 (33.3) | 0 | 2 (7.4) |
Significantly better performance with FNA than with tissue samples, as determined by the Wilcoxon test. P values for real-time PCR assay, M. avium-specific real-time PCR assay, genus-specific real-time PCR assay, and any positive diagnostic test were 0.003, 0.011, 0.001, and 0.005, respectively.
Compared to a positive mycobacterial skin test as an indication of the presence of a mycobacterial infection, the sensitivity, specificity, positive predictive value, and negative predictive value of the real-time PCR assay for patients with lymphadenitis were 71.6, 100, 100, and 72.5%, respectively. The application of the real-time PCR assay to all collected samples revealed 66.7% sensitivity, 100% specificity, 100% positive predictive value, and 59.5% negative predictive value. In total, the PCR assay detected a mycobacterial infection in 13 more patients than when only conventional diagnostic tests were performed.
DISCUSSION
In the past few years, real-time PCR assays have been implemented in clinical microbiological laboratories. A few assays for the detection of mycobacteria have been described (15, 19). However, assays for mycobacterial species other than M. tuberculosis have not been successfully applied to clinical patient material and are mainly restricted to the identification of cultured isolates. In this study, we developed a real-time PCR to identify the causative agents of mycobacterial lymphadenitis. Primers for the real-time PCR were designed to amplify an amplicon in the ITS between the 16S and the 23S rRNA genes of mycobacteria, enabling the annealing of a genus-, M. avium-, or M. tuberculosis-specific probe. The detection limit of the assay was established at 1,100 CFU/ml of pus, and the assay was shown to be specific. For patients with suspected NTM lymphadenitis, the real-time PCR was significantly more sensitive than conventional staining and culturing. All samples were also tested for the presence of inhibition of the assay by spiking portions of the samples and by diluting the samples 10 times. We did not encounter any inhibition, but the risk of inhibition will remain, considering the nature of the clinical materials (26).
Among 67 patients with suspected NTM lymphadenitis, successful identification of the pathogen was achieved for 55 of the patients by acid-fast staining, culturing, or real-time PCR. For 48 patients, it was possible to identify the pathogen within 2 days by the real-time PCR, whereas culturing of the remaining mycobacteria took 4 to 8 weeks. M. avium was identified in 39 patients, i.e., 71% of all confirmed mycobacterial infections in this study. This result corresponds to those of earlier studies where the M. avium complex was found to be the most common species in atypical mycobacterial lymphadenitis (8, 14, 22).
Our results also indicate that FNA have a higher recovery rate than tissue samples for diagnostic testing by the real-time PCR. The high recovery rate for FNA in the PCR diminishes the need for invasive methods for diagnosis of the involved pathogen, but a higher recovery rate for tissue biopsy specimens was expected. The genus-specific PCR performed less well with tissue biopsy specimens. The M. avium-specific PCR also performed better with FNA but was positive for six tissue samples for which the genus-specific PCR remained negative. An NCBI BLAST search of the probe sequences in the human sequence database showed a higher homology of the genus-specific probe than of the M. avium-specific probe with human chromosomal sequences. As a result, less genus-specific probe will be available, resulting in reduced efficiency of the real-time PCR for tissue samples or FNA. This situation will mainly affect weak positive samples, as demonstrated by high threshold cycle values (between 38 and 45) for the 6 M. avium-positive samples with negative results in the genus-specific PCR, in contrast to low cycle threshold values (between 30 and 37) for 15 M. avium- and genus Mycobacterium-positive samples.
Traditionally, culturing has been regarded as the most appropriate “gold standard.” A definite diagnosis of mycobacterial lymphadenitis is made by recovery of the bacterium from lymph node material, but some causative pathogens may require a long incubation period (e.g., M. malmoense) or special culture conditions (M. haemophilum) (28). Skin tests may prove beneficial for the evaluation of mycobacterial lymphadenitis (29, 30). All children included in this study were investigated by one of the authors (J.A.L.), who also performed a skin test. Only children with a clinical syndrome suspected of being mycobacterial lymphadenitis and a positive skin test were further investigated. Since no other pathogens besides mycobacteria were detected in this study, a positive skin test can be considered indicative of mycobacterial infection. The skin test that we used is a well-standardized preparation from M. avium, M. scrofulaceum, and M. kansasii. Intradermal skin testing for the diagnosis of NTM lymphadenitis has been reported to have a sensitivity of 87%, but the specificity has not been well investigated (20). For instance, studies of asymptomatic healthy children in Sweden and Denmark with the same skin test that we used demonstrated that 6 to 32% had positive reactions (9, 16). NTM are common environmental isolates present in soil and water, and extensive cross-reactivity may exist among these mycobacteria. Therefore, a species-specific skin test is difficult to interpret, and more information on the incidence of a positive skin test in healthy Dutch children is needed to determine the diagnostic value of the skin test more precisely.
For staining- and culture-negative samples from eight patients, the genus-specific PCR results were positive, whereas the real-time PCR results for M. avium and M. tuberculosis were negative. In two cases, sufficient PCR product was obtained for sequence analysis, and M. haemophilum was identified in both cases. This species requires special culture conditions and was therefore not detected in routine mycobacterial cultures. Our next objective is to expand the real-time assay with an M. haemophilum-specific probe. Approximately 70% of NTM lymphadenitis cases are due to M. avium. The remaining species identified in this study were M. malmoense, M. kansasii, M. haemophilum, and M. tuberculosis. The real-time PCR assay developed in this study can be expanded with probes specific for other species because of the large sequence variations in the ITS region. These variations are much greater than those found in any other known region, including the 16S rRNA gene. This finding has also been demonstrated by the ability of the real-time PCR to distinguish M. avium from M. intracellulare, whereas several other molecular methods do not distinguish this difference. The M. avium-specific real-time PCR detects only M. avium subsp. avium, M. avium subsp. silvaticum, and M. avium subsp. paratuberculosis.
Mycobacterial culturing is not optimal. When DNA was isolated from 12 negative MGIT cultures of M. avium-specific real-time PCR-positive samples, 5 samples gave a weak positive signal in the PCR. This result indicates that mycobacteria were present in the MGIT cultures. In two MGIT cultures, contamination with other bacteria was apparent and could have caused this growth inhibition, but in the remaining three MGIT cultures, no growth was detected at all. For these cultures, it is possible that the bacteria were dead or the conditions were not optimal.
In summary, the 71.6% sensitivity and the 100% specificity of the real-time PCR assay for the detection of atypical mycobacteria in patients with lymphadenitis suggest that the real-time PCR is an important diagnostic test and is more sensitive than conventional acid-fast staining techniques and mycobacterial culturing. The development of a rapid diagnostic test for the identification of mycobacteria as the cause of lymphadenitis is important, since an increasing number of reports suggest that rapid initiation of drug therapy may be of benefit and may be able to replace surgical excision of the involved lymph node (2, 10, 17).
Acknowledgments
This work was supported by a grant from the Foundation Microbiology Leiden and by NWO.
We thank Kate Templeton for support in the development of the real-time PCR, Renate van den Berg for general support, and Janke Schinkel for statistical support. Dick van Soolingen (Laboratory of Mycobacteriology, National Institute of Public Health and the Environment) is gratefully acknowledged for providing mycobacterial reference strains.
REFERENCES
- 1.American Thoracic Society, Medical Section of the American Lung Association. 1997. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am. J. Respir. Crit. Care Med. 156:S1-S25. [DOI] [PubMed] [Google Scholar]
- 2.Berger, C., G. E. Pfyffer, and D. Nadal. 1996. Treatment of nontuberculous mycobacterial lymphadenitis with clarithromycin plus rifabutin. J. Pediatr. 128:383-386. [DOI] [PubMed] [Google Scholar]
- 3.Bergmans, A. M., J. W. Groothedde, J. F. Schellekens, J. D. van Embden, J. M. Ossewaarde, and L. M. Schouls. 1995. Etiology of cat scratch disease: comparison of polymerase chain reaction detection of Bartonella (formerly Rochalimaea) and Afipia felis DNA with serology and skin tests. J. Infect. Dis. 171:916-923. [DOI] [PubMed] [Google Scholar]
- 4.Boom, R., C. J. Sol, M. M. Salimans, C. L. Jansen, P. M. Wertheim-van Dillen, and J. van der Noordaa. 1990. Rapid and simple method for purification of nucleic acids. J. Clin. Microbiol. 28:495-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eishi, Y., M. Suga, I. Ishige, D. Kobayashi, T. Yamada, T. Takemura, T. Takizawa, M. Koike, S. Kudoh, U. Costabel, J. Guzman, G. Rizzato, M. Gambacorta, R. du Bois, A. G. Nicholson, O. P. Sharma, and M. Ando. 2002. Quantitative analysis of mycobacterial and propionibacterial DNA in lymph nodes of Japanese and European patients with sarcoidosis. J. Clin. Microbiol. 40:198-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eriksson, M., R. Bennet, and N. Danielsson. 2001. Non-tuberculous mycobacterial lymphadenitis in healthy children: another lifestyle disease? Acta Paediatr. 90:1340-1342. [DOI] [PubMed] [Google Scholar]
- 7.Falkinham, J. O. 1996. Epidemiology of infection by nontuberculous mycobacteria. Clin. Microbiol. Rev. 9:177-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grange, J. M., M. D. Yates, and A. Pozniak. 1995. Bacteriologically confirmed nontuberculous mycobacterial lymphadenitis in south east England: a recent increase in the number of cases. Arch. Dis. Childhood 72:516-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hansen, K. N., I. Heltberg, and K. Hjelt. 1989. Sensitivity to tuberculin and sensitins from atypical mycobacteria (M. chelonae subsp. abscessus, M. avium, M. intracellulare, M. scrofulaceum) in 100 Danish school children. Dan. Med. Bull. 36:399-401. [PubMed] [Google Scholar]
- 10.Hazra, R., C. D. Robson, A. R. Perez-Atayde, and R. N. Husson. 1999. Lymphadenitis due to nontuberculous mycobacteria in children: presentation and response to therapy. Clin. Infect. Dis. 28:123-129. [DOI] [PubMed] [Google Scholar]
- 11.Hsiao, P. F., C. Y. Tzen, H. C. Chen, and H. Y. Su. 2003. Polymerase chain reaction based detection of Mycobacterium tuberculosis in tissues showing granulomatous inflammation without demonstrable acid-fast bacilli. Int. J. Dermatol. 42:281-286. [DOI] [PubMed] [Google Scholar]
- 12.Kubica, G. P., W. E. Dye, M. L. Cohn, and G. Middlebrook. 1963. Sputum digestion and decontamination with N-acetyl-l-cysteine-sodium hydroxide for culture of mycobacteria. Am. Rev. Respir. Dis. 87:775-779. [DOI] [PubMed] [Google Scholar]
- 13.Kuth, G., J. Lamprecht, and G. Haase. 1995. Cervical lymphadenitis due to mycobacteria other than tuberculosis—an emerging problem in children? ORL J. Otorhinolaryngol. Relat. Spec. 57:36-38. [DOI] [PubMed] [Google Scholar]
- 14.Kvaerner, K. J., E. Kvestad, and M. Orth. 2001. Surgery required to verify atypical mycobacterial infections. Int. J. Pedriatr. Otorhinolaryngol. 61:121-128. [DOI] [PubMed] [Google Scholar]
- 15.Lachnik, J., B. Ackermann, A. Bohrssen, S. Maass, C. Diephaus, A. Puncken, M. Stermann, and F. Bange. 2002. Rapid-cycle PCR and fluorimetry for detection of mycobacteria. J. Clin. Microbiol. 40:3364-3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lind, A., L. O. Larsson, M. W. Bentzon, M. Magnusson, J. Olofson, I. Sjogren, I. L. Strannegard, and B. E. Skoogh. 1991. Sensitivity to sensitins and tuberculin in Swedish children. I. A study of schoolchildren in an urban area. Tubercle 72:29-36. [DOI] [PubMed] [Google Scholar]
- 17.Lindeboom, J. A., J. de Lange, and H. P. van den Akker. 1999. Clarithromycin as a single-modality treatment in mycobacterial avium-intracellular infections. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 87:50-54. [DOI] [PubMed] [Google Scholar]
- 18.Mijs, W., K. De Vreese, A. Devos, H. Pottel, A. Valgaeren, C. Evans, J. Norton, D. Parker, L. Rigouts, F. Portaels, U. Reischl, S. Watterson, G. Pfyffer, and R. Rossau. 2002. Evaluation of a commercial line probe assay for identification of Mycobacterium species from liquid and solid culture. Eur. J. Clin. Microbiol. Infect. Dis. 21:794-802. [DOI] [PubMed] [Google Scholar]
- 19.Miller, N., T. Cleary, G. Kraus, A. K. Young, G. Spruill, and H. J. Hnatyszyn. 2002. Rapid and specific detection of Mycobacterium tuberculosis from acid-fast bacillus smear-positive respiratory specimens and BacT/ALERT MP culture bottles by using fluorogenic probes and real-time PCR. J. Clin. Microbiol. 40:4143-4147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rahal, A., A. Abela, P. H. Arcand, M. C. Quintal, M. H. Lebl, and B. F. Tapier. 2001. Nontuberculous mycobacterial adenitis of the head and neck in children. Laryngoscope 111:1791-1796. [DOI] [PubMed] [Google Scholar]
- 21.Robson, C., R. Hazra, P. D. Barnes, R. L. Robertson, D. Jones, and R. N. Husson. 1999. Nontuberculous mycobacterial infection of the head and neck in immunocompetent children: CT and MR findings. Am. J. Neuroradiol. 20:1829-1835. [PMC free article] [PubMed] [Google Scholar]
- 22.Romanus, V., H. O. Hallander, and P. Wahlen. 1995. Atypical mycobacteria in extrapulmonary disease among children. Incidence in Sweden from 1969 to 1990, related to changing BCG-vaccination coverage. Tuber. Lung Dis. 76:300-310. [DOI] [PubMed] [Google Scholar]
- 23.Roth, A., M. Fischer, M. E. Hamid, S. Michalke, W. Ludwig, and H. Mauch. 1998. Differentiation of phylogenetically related slowly growing mycobacteria based on 16S-23S rRNA gene internal transcribed spacer sequences. J. Clin. Microbiol. 36:139-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roth, A., U. Reischl, A. Streubel, L. Naumann, R. M. Kroppenstedt, M. Habicht, F. Fischer, and H. Mauch. 2000. Novel diagnostic algorithm for identification of mycobacteria using genus-specific amplification of the 16S-23S rRNA gene spacer and restriction endonucleases. J. Clin. Microbiol. 38:1094-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rozen, S., and H. J. Skaletsky. 2000. Primer3 on the WWW for general users and for biologist programmers, p. 365-386. In S. Krawetz and S. Misener (ed.), Bioinformatics methods and protocols: methods in molecular biology. Humana Press, Totowa, N.J. [DOI] [PubMed]
- 26.Templeton, K., S. A. Scheltinga, J. Crielaard, J. van Schie, A. W. Graffelman, P. Sillekens, P. J. van den Broek, H. Goossens, M. F. C Beersma, and E. C. J. Claas. 2003. Comparison and evaluation of real-time PCR, real-time nucleic acid sequence-based amplification, conventional PCR, and serology for diagnosis of Mycoplasma pneumoniae. J. Clin. Microbiol. 41:4366-4371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tötsch, M., W. Böcker, E. Brömmelkamp, M. Fille, A. Kreczy, D. Öfner, K. Werner, K. W. Schmid, and B. Dockhorn-Dworniczak. 1996. Diagnostic value of different PCR assays for the detection of mycobacterial DNA in granulomatous lymphadenopathy. J. Pathol. 178:221-226. [DOI] [PubMed] [Google Scholar]
- 28.van de Griendt, E. J., P. J. Rietra, and R. N. van Andel. 2003. Mycobacterium haemophilum als veroorzaker van lymphadenitis colli bij een niet-zieke jongen Ned. Tijdschr. Geneeskd. 147:1367-1369. [PubMed] [Google Scholar]
- 29.von Reyn, C. F., P. A. Green, D. McCormick, G. A. Huitt, B. J. Marsh, M. Magnusson, and T. W. Barber. 1994. Dual skin testing with Mycobacterium avium sensitin and purified protein derivative: an open study of patients with M. avium complex infection or tuberculosis. Clin. Infect. Dis. 19:15-20. [DOI] [PubMed] [Google Scholar]
- 30.von Reyn, C. F., D. E. William, C. R. Horsburgh, Jr., A. S. Jaege, B. J. Mars, K. Haslov, and M. Magnusson. 1998. Dual skin testing with Mycobacterium avium sensitin and purified protein derivative to discriminate pulmonary disease due to M. avium complex from pulmonary disease due to Mycobacterium tuberculosis. J. Infect. Dis. 177:730-736. [DOI] [PubMed] [Google Scholar]
- 31.Yuen, K. Y., W. C. Yam, L. P. Wong, and W. H. Seto. 1997. Comparison of two automated DNA amplification systems with a manual one-tube nested PCR assay for diagnosis of pulmonary tuberculosis. J. Clin. Microbiol. 35:1385-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]