Abstract
This manuscript outlines the history, need, and evolution of gender medicine in emergency care research. Clinical examples are used where sex and gender play a role in diagnosis, management, or prognosis of patients in the emergency department (ED). The ED serves as an ideal setting to advance sex- and gender-specific research as the primary access point for health care for much of the U.S. population, with more than 136 million annual visits. Gender medicine provides the biological and social framework to provide high-quality, safe, equitable, and cost-effective sex- and gender-specific care in the ED. With a 24-hour hospital presence, and with access to high-acuity patients, emergency physicians are well positioned to lead sex- and gender-specific clinical studies for time-sensitive conditions and also to serve as vital partners in interdisciplinary research projects. The ED also provides the primary access point for less life threatening conditions such as substance abuse, mental health, and pain management (both acute and chronic). Because a fifth of the U.S. population is without health insurance, and many more lack a regular provider or rapid access to their providers, the ED is often the only point of contact for advancing gender medicine in this population.
Evolution of Gender Medicine as a New Science
Gender medicine was born out of a 1993 legislation that required researchers funded by the National Institutes of Health (NIH) to include appropriate numbers of women and minorities in clinical research, and when scientifically appropriate, to perform valid analyses of the role of biological sex in clinical trials.1 The new science was further validated by a 2001 evidence report by the Institute of Medicine (IOM) entitled “Exploring the Biological Contributions to Human Health: Does Sex Matter?” that verified that research data when analyzed by sex and gender often leads to differential treatment decisions.2 These initial works sowed the seeds for gender medicine to grow as a new science. In 2011, the IOM further explored and publicized the advances made in gender medicine in multiple specialties. Of note, emergency medicine was absent in this report. Coinciding with this report, the NIH Office of Research on Women's Health put forth its strategic plan for the next decade in “Moving into the Future with New Dimensions and Strategies: A Vision for 2020 for Women's Health Research.”3 This 2011 report provided a framework for research within NIH and throughout the scientific community. It not only articulated new priorities within women's health research, but also strongly reinforced existing areas such as interdisciplinary, gender-specific research.
Over the past two decades, advancement of gender medicine has required systematic dissipation of two myths. First, gender medicine is not akin to women's health, even though it was originally derived through advocacy of women's health initiatives. As is evident from the examples described below, advancing gender medicine improves outcomes for both men and women. Second, sex and gender medicine is not restricted to reproductive organs – so-called ‘bikini medicine’. Every cell has a sex and influences the biological manifestation of disease. It is important to consider sex/gender in the clinical setting as well as in research in order to better understand the differences and the effect of these factors on patient outcomes. The newest NIH mandate in May 2014 requiring all basic science research to include both male and female cells further validates this concept.4
Applying the Gender Lens to Emergency Care – From Bench to Bedside
Emergency physicians (EPs) have observed consistent examples where sex and gender influences diagnosis, management, prognosis, and safety of their patients. For example, while taking care of patients with acute ST-elevation myocardial infarction, EPs are often surprised to see that some have negative angiograms despite meeting clinical criteria. This pattern seems to be more common in women as compared to men. We now understand that alternate forms of atherosclerosis that seem to be sex-specific5 influence the care and prognosis of such patients. This biological difference likely also explains the higher prevalence of angina in women as compared to men.6 And yet, current emergency department (ED) evaluation protocols are not sensitive enough to detect the alternate forms of atherosclerosis. Comparative effectiveness studies of current standard care compared with gender-specific algorithms are needed to optimize cost-effectiveness and clinical outcomes as has been done for coronary artery disease.
The benefits of advancing gender medicine in emergency care are not restricted to women only. Trauma resuscitation is one example where we see higher mortality in men compared to women across all age groups.7 This is partly attributed to high-risk behaviors in men, but is also related to the hormonal milieu that exists at the time of insult. The immune response to the traumatic insult seems to be shaped by genetic polymorphism related to expression of the reproductive hormones. Estrogen boosts the immune response while testosterone suppresses it as is evident from the higher rates of post-traumatic pneumonia and multi-system organ failure in men as compared to women.8 An excellent translation of the biological role of hormones on patient outcomes was seen in the ProTECT (Progesterone For the Treatment of Traumatic Brain Injury) trial that was spearheaded by emergency physicians.9 The trial bridged the gap between basic science and clinical science by investigating the neuro-protective role of progesterone after traumatic brain injury.
Similar to disease processes, sex- and gender-specific differences have also been documented in areas of public health that form the core of emergency care. For instance, sex and gender differences have been documented in alcohol toxicity for similar levels of consumption due to differential rates of alcohol dehydrogenase activity in men versus women.10 Gender also affects treatment for substance use disorders: women have more barriers to access, have more severe problems at treatment entry, and have lower rates of completion of substance use treatments.11,12 Specifically, the rate of opioids abuse has increased, and while men are more likely to have drug dependence, the escalation of drug use (especially prescription abuse) has been more dramatic over time in women.13,14 Women are also more likely to use opioids consistent with their prescription instructions, are more likely to use via the intended route of administration, and are more likely than men to use opioids to cope with psychiatric symptoms and negative affect.15 Future efforts targeting opioid abuse will need to take these gender factors into account to ensure success. Similarly, with the closure of mental health institutions, the burden of acute psychiatric care has increased in emergency care. The rates of suicides have remained persistently higher in men compared to women.16 Yet depressed women are not being hospitalized at the same rate as men after ED visits, identifying potential disparities in the delivery of crisis care for a potentially life-threatening disorder.17 Further research with concomitant exploration of the causes and consequences of this practice pattern is necessary to move toward comparable treatment for individuals regardless of gender.
Emergency departments also provide a good forum to study the safety and efficacy of drugs. For example, the U.S. Food and Drug Administration recently reduced the dose of zolpidem in women, but not men, when new data highlighted an increased risk of driving-related accidents in women compared to men.18
And last but not the least, a sharp increase has been noted in the use of advanced medical imaging in the ED; for example, ED computed tomography (CT) use increased by 330% from 1996 through 2007, with an estimated 13.9% increase in 2007 alone.19 While the rates of CT use increased at similar rates for both male and female ED patients, women are more susceptible to the dangers of ionizing radiation from CT scanning. It is estimated that as many as 29,000 future malignancies may result from CT scans performed in the United States in 2007 alone, with malignancies in females accounting for a disproportionate amount (18,000 out of 29,000, or 62% of estimated future cancers).20,21 Furthermore, while men and women seem to receive CT scanning in equal numbers in the ED, ultrasound is often a more appropriate (and safer) initial diagnostic approach, particularly in the case of female pelvic pain.22 The Affordable Care Act prioritized quality measures that address safety, effectiveness, patient-centeredness, appropriateness, and timeliness of care. To achieve these goals, sex-specific appropriateness criteria are needed for diagnostic imaging in the ED for common complaints.
The ED is the primary access point for health care for much of the U.S. population, with more than 136 million patient visits annually, and health care reform may not reduce ED volume.23 EPs are clinicians who have the opportunity to apply gender medicine and observe significant trends in clinical care, generating important research questions and clinical trials. Gender medicine provides the biological and social framework to provide high-quality, safe, equitable, and cost-effective gender-specific care in the ED. With a 24-hour hospital presence and access to high-acuity patients, EPs are ideally positioned to lead gender-specific clinical studies for acute conditions and also to serve as vital partners in interdisciplinary research projects. Some collaborative networks (e.g. the Neurological Emergencies Treatment Trial Network) already exist; however, the science of gender medicine remains largely unexplored in emergency care.24,25
The ED also provides the primary access point for less life-threatening conditions such as substance abuse, mental health, and pain management (both acute and chronic).26-28 Since a fifth of the US population is without health insurance and many more lack regular providers or rapid access to their providers,29 the ED is often the only point of contact for studying this population.30,31 These and other examples provide a clear basis of why gender-specific research needs to be an integral part of emergency care.
Status of Gender Medicine in Emergency Care Research: Identifying a Gap
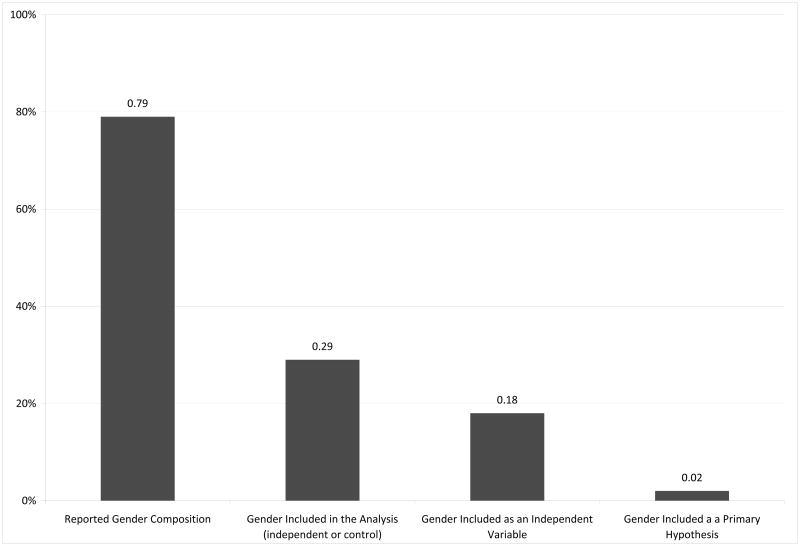
Despite a clear need, a 2011 review showed that EM is out of pace with other specialties such as cardiology, psychiatry, and oncology in applying the gender lens to its research. The review showed that only 2% of all EM studies reported gender-specific outcomes, and only 10% incorporated gender in their analyses (Figure 1).25 Twenty-one percent of EM studies did not report the gender of the participants. This manuscript alerted EPs to the absence of reporting of gender-specific outcomes for acute conditions.25
Figure 1.
Percent of studies based on a MEDLINE search of EM articles published between January 2006 and April 2009 (n=750 articles) that reported gender composition, included gender in the study design, as an independent variable, or in a primary hypothesis.
Figure originally published in AEM 2011;18:e1-4.25
2014 AEM Consensus Conference – Filling a Critical Gap
The 2014 AEM conference on sex- and gender-specific research is culmination of a 3-year concerted effort by a dedicated team that wants to change these statistics. The organization, planning, and measures that led to its success are described elsewhere in this issue.32 The conference and its agenda on May 13, 2014 proved timely with the announcement by the NIH on May 14, 2014 mandating basic science research to include both male and female cells. This issue of AEM is devoted to the consensus recommendations put forth by leaders in emergency care research aiming to promote research in sex and gender medicine.
Conclusions
The 2014 AEM consensus conference on sex- and gender-specific research was a multi-stakeholder symposium that was put together to fill a critical gap in emergency care research. On behalf of the conference organizing committee and the journal's editorial board, we thank the conference participants, patients, speakers, federal partners, and our generous supporters for making this day possible. We hope that the reader finds this AEM issue with the conference proceedings and original research stimulating and informative, and that these articles will catalyze research in these important areas.
Acknowledgments
The success of this conference is due to the efforts of a large group of people. The organizing team thanks Dr. David Cone and the AEM editorial board for recognizing the time-sensitive need to select sex- and gender-specific research as the topic for the 2014 consensus conference. We appreciate the AWAEM's vote of sponsorship and its leadership who volunteered substantial time and support to the project, in particular Kathleen Clem, Stephanie Abbuhl, Gloria Kuhn, and Esther Choo. We acknowledge the significant organizational support of our respective institutions, Yale University and Lehigh Valley Health Network. We also thank the editorial staff of the journal and the staff at SAEM for their administrative and logistic support. We acknowledge Stephen Post for lending his artistic talents in creating the conference logo. We also thank Robert Duprey for his diligence in developing a strategic plan for consistent consensus methodology. We thank the Emergency Medicine Residents' Association (EMRA) for sponsoring travel scholarships to support these young minds. Finally, we thank SAEM for its leadership, and the SAEM board for working closely with us in moving our conference agenda forward.
Funding: The consensus conference was supported by grant 1R13NS087861-01 from the National Institute of Neurological Disorders and Stroke and the Office of Research on Women's Health at the NIH. Additional funding was provided by several organizational, institutional, and individual donors. Non-CME events were supported by Janssen Pharmaceuticals and Besins Critical Care/BH Pharma. See the Executive Summary elsewhere in this issue for full funding information.
References
- 1.Woosley RL, Anthony M, Peck CC. Biological sex analysis in clinical research. J Womens Health Gend Based Med. 2000;9:933–4. doi: 10.1089/15246090050199919. [DOI] [PubMed] [Google Scholar]
- 2.Legato MJ. Does sex matter? The institute of medicine answers “yes”. J Gend Specif Med. 2001;4:4–5. [PubMed] [Google Scholar]
- 3.National Institutes of Health, Office of Research on Women's Health. Moving into the Future with New Dimensions and Strategies: A Vision for 2020 for Women's Health Research. Strategic Plan. [Accessed Sep 19, 2014]; Available at: http://orwh.od.nih.gov/research/strategicplan/ORWH_StrategicPlan2020_Vol1.pdf.
- 4.Clayton JA, Collins FS. Policy: NIH to balance sex in cell and animal studies. Nature. 2014;509:282–3. doi: 10.1038/509282a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hemingway H, McCallum A, Shipley M, Manderbacka K, Martikainen P, Keskimaki I. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA. 2006;295:1404–11. doi: 10.1001/jama.295.12.1404. [DOI] [PubMed] [Google Scholar]
- 6.Safdar B, Nagurney JT, Anise A, et al. Gender-specific research for emergency diagnosis and management of ischemic heart disease: proceedings from the 2014 AEM consensus conference cardiovascular research group. Acad Emerg Med. 2014 doi: 10.1111/acem.12527. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American College of Surgeons. National Trauma Data Bank 2013 Annual Pediatric Report. [Accessed Sep 19, 2014]; Available at: https://www.facs.org/∼/media/files/quality%20programs/trauma/ntdb/ntdb%20annual%20report%202013.ashx.
- 8.Sperry JL, Minei JP. Gender dimorphism following injury: making the connection from bench to bedside. J Leukocyte Biol. 2008;83:499–506. doi: 10.1189/jlb.0607360. [DOI] [PubMed] [Google Scholar]
- 9.Attella MJ, Nattinville A, Stein DG. Hormonal state affects recovery from frontal cortex lesions in adult female rats. Behav Neural Biol. 1987;48:352–67. doi: 10.1016/s0163-1047(87)90918-6. [DOI] [PubMed] [Google Scholar]
- 10.Baraona E, Abittan CS, Dohmen K, et al. Gender differences in pharmacokinetics of alcohol. Alcohol Clin Exp Res. 2001;25:502–7. [PubMed] [Google Scholar]
- 11.Arfken CL, Klein C, di Menza S, Schuster CR. Gender differences in problem severity at assessment and treatment retention. J Subst Abuse Treat. 2001;20:53–7. doi: 10.1016/s0740-5472(00)00155-0. [DOI] [PubMed] [Google Scholar]
- 12.Lynch WJ, Roth ME, Carroll ME. Biological basis of sex differences in drug abuse: Preclinical and clinical studies. Psychopharmacol. 2002;164:121–37. doi: 10.1007/s00213-002-1183-2. [DOI] [PubMed] [Google Scholar]
- 13.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care. 2013;51:646–53. doi: 10.1097/MLR.0b013e318293c2c0. [DOI] [PubMed] [Google Scholar]
- 14.Becker JB, Hu M. Sex differences in drug abuse. Front Neuroendocrinol. 2008;29:36–47. doi: 10.1016/j.yfrne.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katz C, El-Gabalawy R, Keyes KM, Martins SS, Sareen J. Risk factors for incident nonmedical prescription opioid use and abuse and dependence: results from a longitudinal nationally representative sample. Drug Alcohol Depend. 2013;132:107–13. doi: 10.1016/j.drugalcdep.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–54. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rost K, Hsieh YP, Xu S, Harman J. Gender differences in hospitalization after emergency room visits for depressive symptoms. J Womens Health (Larchmt) 2011;20:719–24. doi: 10.1089/jwh.2010.2396. [DOI] [PubMed] [Google Scholar]
- 18.Farkas RH, Unger EF, Temple R. Zolpidem and driving impairment--identifying persons at risk. N Engl J Med. 2013;369:689–91. doi: 10.1056/NEJMp1307972. [DOI] [PubMed] [Google Scholar]
- 19.Kocher KE, Meurer WJ, Fazel R, Scott PA, Krumholz HM, Nallamothu BK. National trends in use of computed tomography in the emergency department. Ann Emerg Med. 2011;58:452–62. doi: 10.1016/j.annemergmed.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 20.Berrington de Gonzalez A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071–7. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078–86. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andreotti RF, Lee SI, Choy G, et al. ACR Appropriateness Criteria® on acute pelvic pain in the reproductive age group. J Am Coll Radiol. 2009;6:235–41. doi: 10.1016/j.jacr.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Health disparities and inequalities report (CHDIR) MMWR Morbid Mortal Wkly Rep. 2011;60(Supp):1–116. [Google Scholar]
- 24.Barsan B. NETT: Neurological Emergencies Treatment Trials Network. Homepage. [Accessed Sep 19, 2014]; Available at: http://www.nett.umich.edu/nett/welcome.
- 25.Safdar B, McGregor AJ, McKee SA, et al. Inclusion of gender in emergency medicine research. Acad Emerg Med. 2011;18:e1–4. doi: 10.1111/j.1553-2712.2010.00978.x. [DOI] [PubMed] [Google Scholar]
- 26.Marx J, Hockberger R, Walls R, editors. Rosen's emergency medicine-concepts and clinical practice. Philadelphia, PA: Elsevier; 2009. [Google Scholar]
- 27.Woodruff SI, Eisenberg K, McCabe CT, Clapp JD, Hohman M. Evaluation of California's alcohol and drug screening and brief intervention project for emergency department patients. West J Emerg Med. 2013;14(3):263–70. doi: 10.5811/westjem.2012.9.11551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu S, Nagurney J, Chang Y, et al. 440 frequent users of the emergency department: do they make visits that can be addressed in a primary care setting? [Abstract] Ann Emerg Med. 2012;604(Suppl):S155. [Google Scholar]
- 29.DeNavas-Walt C, Proctor BD, Smith JC U.S. Census Bureau. Income, poverty, and health insurance coverage in the United States: 2009. Washington, DC: U.S. Government Printing Office; 2010. [Google Scholar]
- 30.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of us emergency department visits, 1997-2007. JAMA. 2010;304:664–70. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ginde AA, Lowe RA, Wiler JL. Health insurance status change and emergency department use among us adults. Arch Intern Med. 2012;172:642–7. doi: 10.1001/archinternmed.2012.34. [DOI] [PubMed] [Google Scholar]
- 32.Safdar B, Greenberg MR. Conference on gender-specific research in emergency care. An executive summary. Acad Emerg Med. 2014 doi: 10.1111/acem.12530. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]