Abstract
PURPOSE
This study investigated the influence of surface conditioning procedures and repeated firings on monoclinic content and strength of zirconia before cementation.
MATERIALS AND METHODS
Sintered bar-shaped zirconia specimens were subjected to no surface treatment (control), air abrasion, or grinding (n=21). Their roughness was evaluated using a profilometer, and microscope analysis was performed on one specimen of each group. Then, 2 or 10 repeated firings (n=10) were executed, the monoclinic content of specimens was analyzed by X-ray diffraction, and a three-point flexural strength test was performed. Surface roughness values were compared using one-way analysis of variance (ANOVA) and Tukey honestly significant difference (HSD) tests, the monoclinic content values were tested using Kruskal-Wallis and Mann-Whitney U tests, and the flexural strength values were tested using two-way ANOVA and Tukey HSD tests (P=.05). Spearman's correlation test was performed to define relationships among measured parameters.
RESULTS
Surface-treated specimens were rougher than untreated specimens and had a higher monoclinic content (P<.005), and the relationship between roughness and monoclinic content was significant (P<.000). Neither surface treatment nor firing significantly affected the flexural strength, but Weibull analysis showed that for the air-abraded samples the characteristic strength was significantly lower after the 10th firing than after the 2nd firing.
CONCLUSION
After firing, a negligible amount of monoclinic content remained on the zirconia surfaces, and rougher surfaces had higher monoclinic contents than untreated surfaces. Multiple firings could be performed if necessary, but the fracture probability could increase after multiple firings for rougher surfaces.
Keywords: Surface Treatment, Zirconium Oxide, Ceramics, X-ray diffraction, Flexural Strength
INTRODUCTION
Zirconia-based ceramics, such as yttria-tetragonal zirconia polycrystals (Y-TZP), are used as core materials in dental restorations.1,2 They consist mainly of zirconia and partially of Y2O3. Zirconia can be present in different phases: cubic, tetragonal, and monoclinic.3,4 In Y-TZP ceramics, the tetragonal form can be stabilized at room temperature by Y2O3, but external stresses can trigger a transformation from the tetragonal to monoclinic phase. This transformation is related with volume enlargement that urges compressive forces, thereby preventing further crack propagation.5,6 This phenomenon makes zirconia potentially superior to other dental ceramics.6 Furthermore, these materials have additional advantages such as high flexural strength, fracture toughness,7 and high biocompatibility.2
To improve its aesthetic properties, the zirconia core is often veneered with conventional feldspathic porcelain to achieve an aesthetic appearance.8 For this purpose, clinical and laboratory processing procedures such as sandblasting or grinding are used to achieve better adhesion between zirconia core and veneering porcelain, to improve bond between luting and prosthetic material, and during final adjustments of the restorations.9 However, these procedures promote the tetragonal to monoclinic phase transformation5,9,10,11,12 and may generate surface flaws on zirconia that can serve as stress accumulation areas.13,14 In addition, in clinical procedures, all-ceramic restorations are sometimes fired several times to correct the form and color of the restorations to produce a natural appearance. It was reported that heat treatments in the temperature range of 900℃ -1,000℃ after surface treatments of Y-TZP induce reverse phase transformation from monoclinic to tetragonal.11,15,16
There have been controversial reports regarding the effects of surface3,5,17,18,19 or heat treatments16,20 on flexural strength of zirconia. In particular, evaluations of the effect of surface treatments have shown that the strength of the zirconia was increased3,19 or decreased5,17,18 depending on the surface damage introduced by the surface treatments. Similarly, investigations into the effects of heat treatments have reported increases20 or decreases16 in strength.
These studies3,5,16,17,18,19,20 focused either on the influence of surface treatment or on the influence of heat treatment on the microstructure and strength of zirconia. However, under clinical conditions, zirconia is exposed to a series of steps consisting of surface treatments and firings. Therefore, the objective of this work was to explore the effects of surface conditioning processes and repeated firings on monoclinic content and flexural strength of zirconia before cementation. The following null hypotheses were tested: (1) different surface treatments and repeated firings do not affect the monoclinic content of zirconia and (2) different surface treatments and repeated firings do not affect flexural strength of zirconia.
MATERIALS AND METHODS
Sixty-three bars (L: 20 mm, W: 4 mm, H: 1.2 mm) were produced by cutting and sintering presintered zirconium oxide blocks (VITA In-Ceram® YZ for in Lab®; VITA Zahnfabrik, Bad Säckingen, Germany). According to the surface conditioning procedures, they were divided into three groups (n=21).
Control: No surface conditioning was applied.
Air abrasion: The surfaces were abraded with 110 µm Al2O3 particles (Korox; Bego, Bremen, Germany) from a distance of about 10 mm at a pressure of 3 bar for 10 seconds.
Grinding: The ceramic surfaces were ground using a hand-piece (Ultimate 500K; NSK, Kanuma, Japan) at a grinding speed of 20,000 rpm for 10 seconds. During the grinding procedure, a diamond bur with a 110 µm grain size (Bredent, Senden, Germany) was used without water-spray cooling. A gentle stroking motion was employed, in order to prevent the formation of high stress concentration areas. The burs were changed after the grinding of every five specimens. The dimensions were measured by an electronic digital micrometer (Mitutoyo Corporation, Kawasaki, Kanagawa, Japan).
A specimen from each surface treatment group was randomly selected, and its surface was examined in a scanning electron microscope (SEM; LEO 440; Zeiss, Cambridge, UK) at ×700 magnification to detect the morphological alterations of the zirconia following surface treatments.
A profilometer (Mitutoyo Surftest 402; Mitutoyo, Minatoku, Japan) was used to determine the surface roughness (Ra in µm) of each sample. Prior to measurement, the profilometer was calibrated. Five measurements were performed at different locations near the center of the specimen, and their average was calculated to obtain the mean roughness of each sample.
Then, all specimens were subjected to heat treatments in a ceramic oven (Vita Vacumat 40T, Vita Zahnfabrik, Bad Säckingen, Germany) either 2 or 10 times to mimic the glaze firing recommended by the manufacturer (Vita, Badsäckingen, Germany) with a starting temperature of 500℃, predrying time of 5 min, heating rate of 80℃, ending temperature of 900℃, and holding time of 1 min without a vacuum.
After heat treatment, X-ray diffraction (XRD) analysis was executed using an X-ray diffractometer (Bruker D8 Advance, Bruker, Germany) at 2θ range between 20° and 40° with a step size of 0.02° and a normalized count time of 1.8 s/step. The monoclinic phase content (%) on the surfaces was determined by using formulas (A)21 and (B)22 below:
| Xm = [Im(-111) + Im(111)] / [Im(-111) + Im(111) + It(101)] | (A) |
| Vm = 1.311 × Xm / 1 + (0.311 × Xm) | (B) |
In these formulas, Xm is the monoclinic peak intensity ratio, Vm is the monoclinic volume content (%), Im(-111) and Im(111) are the monoclinic peak intensities at 2θ=28.2° and 31.4°, respectively, and It(111) is the tetragonal peak intensity at 2θ=31.1°.23
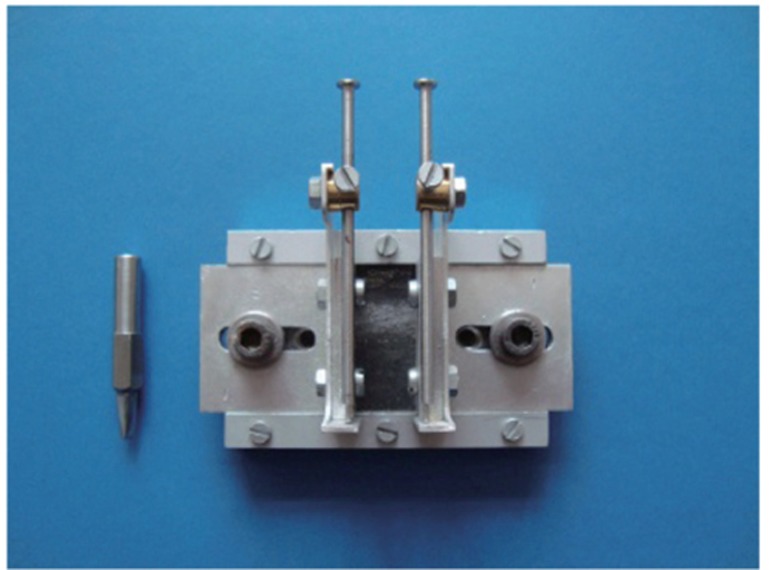
Finally, the flexural strengths of the bars were measured by a three-point flexural strength test apparatus (Fig. 1) according to ISO 6872:2008 at a loading rate of 1 mm/min in a universal testing machine (TSTM 02500; Elista Ltd. Şti., İstanbul, Turkey). The sample holder had a span of 15 mm between the two supports. The supports and loading piston were steel knife edges rounded to radii of 0.8 mm. The surface-treated sides were facing the loading piston, and the lower surfaces were facing the supporting device during the three-point bending test. The load was exerted at the middle of the sample. Failure load was recorded for each bar, and flexural strength data (σ in MPa) were calculated using the formula below.24
| σ = 3Fd / 2wh2 |
Fig. 1.
Three-point flexural strength test apparatus.
In this formula, F is the fracture load (N), d is the distance between two supports (mm), w is the width of the sample (mm), and h is the height of the sample (mm).
In this study, roughness values were compared using one-way analysis of variance (ANOVA) and Tukey honestly significance difference (HSD) test, and monoclinic content values were compared by nonparametric analyses using Kruskal-Wallis and Mann-Whitney U tests. The flexural strength values were statistically tested by two-way ANOVA and Tukey HSD tests with the surface treatments and the number of firing cycles as the independent variables. In addition, variability of the flexural strength values was tested using Weibull distribution. The Weibull modulus was calculated using the following equation.25
| P(σ) = 1 - exp[-(σ/σ0)m] |
In this formula, P is probability of failure, σ is flexural strength at a given P, σ0 is characteristic strength or scale parameter at the fracture probability of 63.2%, and m is Weibull modulus which defines the structural reliability. Lower m values indicate lower reliability or vice versa.25 Wald tests and 95% confidence intervals were used for the comparisons of Weibull parameters.
In addition, the relationships between the roughness and monoclinic content, between the monoclinic content and flexural strength, and between the roughness and flexural strength were assessed by Spearman's correlation analysis. In all statistical analyses a significance level of P=.05 was used.
RESULTS
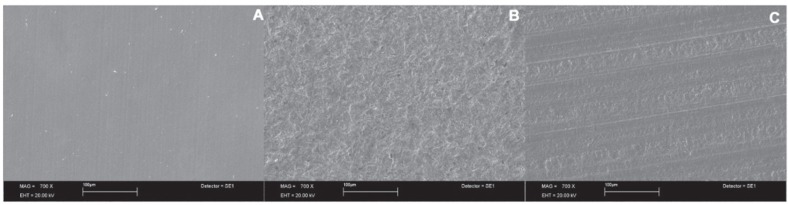
According to SEM evaluation, control sample had a smooth surface texture with no cracks (Fig. 2A). On the other hand, morphological surface changes such as the formation of microscale retentive grooves and uniformly oriented scratches were observed in the air-abraded and ground specimens, respectively (Fig. 2B, Fig. 2C).
Fig. 2.
SEM views of zirconia surfaces (×700). (A) Control, (B) Air-abraded, (C) Ground.
Table 1 lists the results of the one-way ANOVA and Tukey HSD test of roughness data. All surface-treated specimens were rougher than the control group, and prominent differences were observed between the air-abraded and ground groups (P<.005). Air-abraded group had the roughest surface.
Table 1.
Results of the statistical analysis of surface roughness values (Ra, µm)
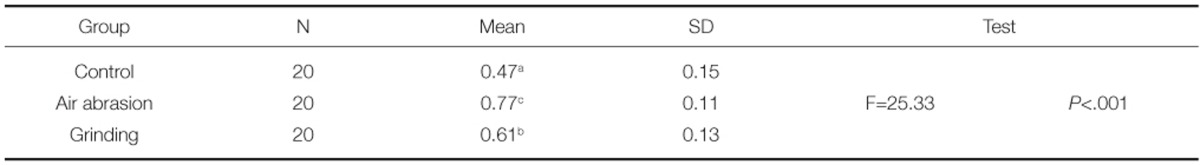
*Different superscript letters in the same column show significant differences (P<.05).
Table 2 summarizes the results of the Kruskal-Wallis and Mann-Whitney U tests of monoclinic content (%) values. Air-abraded or ground specimens showed higher monoclinic contents than control specimens (P<.005). However, in each surface treatment group, repeated firings did not affect the monoclinic content of the zirconia (P>.05).
Table 2.
Results of the statistical analysis of monoclinic content values (%)
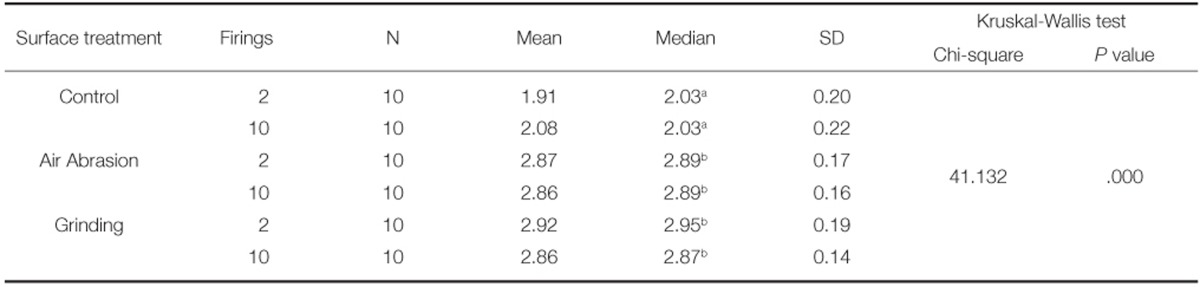
*Different superscript letters in the same column show significant differences (P<.05).
According to strength analysis, two-way ANOVA test revealed that neither the surface treatments nor the firing affected the flexural strength of zirconia. On the other hand, Weibull analysis showed that in the air-abraded group only, repeated firings had a considerable influence on the characteristic strength. In this group, characteristic strength of the specimens was decreased significantly after 10 firing cycles as compared to that obtained after 2 firing cycles. In addition, all groups had a similar Weibull modulus, because confidence bounds for Weibull modulus overlapped (P>.05; Table 3).
Table 3.
Mean, standard deviation, and Weibull statistics of flexural strength values (MPa)
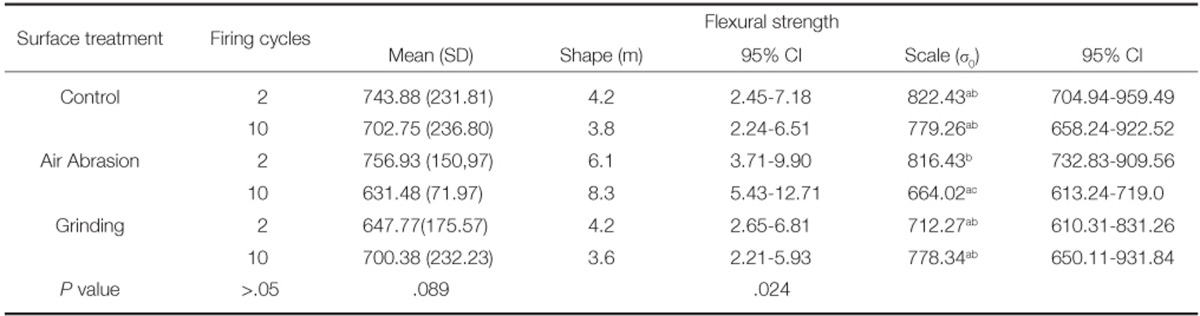
*Different superscript letters in the same column show significant differences (P<.05).
A meaningful positive correlation between the roughness and monoclinic content was observed (P<.000). However, no significant correlation was observed between the other pairs of values (either between the roughness and flexural strength or between the monoclinic content and flexural strength).
DISCUSSION
In clinical procedures, zirconia restorations are subjected to a series of steps including cutting, grinding, airborne-particle abrasion, firing of the veneering porcelain, and glazing. The surface treatments induce tetragonal-to-monoclinic phase transformation, whereas heat treatments induce reverse phase transformation (monoclinic to tetragonal). Hence, all of these procedures can cause stress concentration on the zirconia surface.16
Although the adaptation of the framework is performed in core trial, sometimes the inner surfaces of the restorations are adjusted minimally before glaze application,9 or surface treatments are applied before cementation to improve the bond between the resin cement and zirconia.26 The surface treatments used in this study were chosen to mimic the preparation steps before cementation. As in previous studies,17,27 layering with a veneering ceramic was omitted because the observed effects of the conditioning procedures on the framework material would be more complex if bilayer structures had been assessed. According to the statistical results on the monoclinic content data, the first hypothesis was partially rejected: only different surface treatments had an effect on the monoclinic phase content. After repeated firings, surface-treated specimens showed higher monoclinic contents than the control group (P<.005). Song et al.27 reported that after heat treatment, all of the monoclinic content transformed to the tetragonal phase. On the contrary, Sato et al.16 showed that after firing between 800℃ and 900℃, some monoclinic content remained on the surface. In this study, some negligible monoclinic content remained on the surface after the firing procedure, as was found by Sato et al.16 We think that whether monoclinic content remains depends on the material type. In addition, as in previous studies,28,29,30 the monoclinic phase content was significantly correlated with roughness values (P<.000).
Strength is an important parameter to determine the clinical success of the restoration.25 It is affected by the sizes of flaws and defects on the material's surface, and it can be described as the maximum stress that is essential to cause fracture of a material.31 There are different testing methods available to assess the strength of ceramic materials: the three-point bending test,3,11,32,33 four-point bending test,25 and biaxial flexural strength test.34,35,36 As in previous studies,3,11,32,33 the three-point bending test was used in this study, according to the ISO 6872:2008 standard.37
Some authors11,16 reported that the increases in the strength of zirconia observed after surface treatments seemed to result mainly from the increase in monoclinic phase content. Other studies8,38 reported that subjecting a Y-TZP ceramic to various surface treatments resulted in distinct degrees of phase transformation (tetragonal to monoclinic), but statistically similar biaxial flexural strength values. On the other hand, Oh et al.39 studied the effects of different firing techniques on the flexural strength of pressable all-ceramic materials and reported no noteworthy differences in the flexural strength values among the various groups. According to strength analysis, the second hypothesis was rejected that neither surface treatments nor repeated firings had an effect on flexural strength of zirconia (P>.05). However, according to Weibull analysis, the characteristic strength of zirconia was significantly decreased in the air-abrasion group after the 10th firing (Table 3). In general, the firing procedures did not have a negative effect on the strength of zirconia. However, we assume that in the air-abraded group, microcracks might be formed on the surface during surface treatment and after the 10th firing. This is because compared to the characteristic strength of the 2nd firing group, the characteristic strength of air-abraded zirconia fired 10 times was decreased significantly.
Based on these results, the clinician should be careful when working with zirconia, because surface treatment affects its monoclinic phase content, and depending on the material type, a negligible amount of monoclinic content could be present on the surface after heat treatment. Under clinical conditions, multiple firings could be performed if necessary. However, it should not be forgotten that for rougher surfaces, the fracture probability could increase after multiple firings. The influence of loading under simulated oral conditions should be investigated in further studies to determine how the mechanical properties evolve under these conditions.
CONCLUSION
According to the findings of current study, after heat treatment, a negligible amount of monoclinic phase remained on zirconia surface. The monoclinic content of the zirconia was affected by surface treatments, and surface-treated ceramic specimens (air-abraded or ground) had higher monoclinic contents than the untreated (control) ones (P<.005). Surface treatments or multiple firings did not influence a decrease in flexural strength of zirconia, but for rougher surfaces, the failure probability could increase after multiple firings.
Footnotes
This study was self-funded study. The authors thank Prof. Dr. Bora Öztürk (Department of Restorative Dentistry, Selcuk University) and Assist. Prof. Dr. Mustafa Semiz (Department of Statistics, Selcuk University) for the statistical analysis; and Dr. Faruk Özel for the XRD analysis.
Part of this work was presented at International Association for Dental Research (IADR) General Session and Exhibition, June 25-28, 2014, Cape Town/South Africa.
References
- 1.Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008;24:299–307. doi: 10.1016/j.dental.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Kelly JR, Denry I. Stabilized zirconia as a structural ceramic: an overview. Dent Mater. 2008;24:289–298. doi: 10.1016/j.dental.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Papanagiotou HP, Morgano SM, Giordano RA, Pober R. In vitro evaluation of low-temperature aging effects and finishing procedures on the flexural strength and structural stability of Y-TZP dental ceramics. J Prosthet Dent. 2006;96:154–164. doi: 10.1016/j.prosdent.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Manicone PF, Rossi Iommetti P, Raffaelli L. An overview of zirconia ceramics: basic properties and clinical applications. J Dent. 2007;35:819–826. doi: 10.1016/j.jdent.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Luthardt RG, Holzhüter M, Sandkuhl O, Herold V, Schnapp JD, Kuhlisch E, Walter M. Reliability and properties of ground Y-TZP-zirconia ceramics. J Dent Res. 2002;81:487–491. doi: 10.1177/154405910208100711. [DOI] [PubMed] [Google Scholar]
- 6.Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999;20:1–25. doi: 10.1016/s0142-9612(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 7.Vagkopoulou T, Koutayas SO, Koidis P, Strub JR. Zirconia in dentistry: Part 1. Discovering the nature of an upcoming bioceramic. Eur J Esthet Dent. 2009;4:130–151. [PubMed] [Google Scholar]
- 8.Yamaguchi H, Ino S, Hamano N, Okada S, Teranaka T. Examination of bond strength and mechanical properties of Y-TZP zirconia ceramics with different surface modifications. Dent Mater J. 2012;31:472–480. doi: 10.4012/dmj.2011-237. [DOI] [PubMed] [Google Scholar]
- 9.Kosmac T, Oblak C, Jevnikar P, Funduk N, Marion L. Strength and reliability of surface treated Y-TZP dental ceramics. J Biomed Mater Res. 2000;53:304–313. doi: 10.1002/1097-4636(2000)53:4<304::aid-jbm4>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 10.Curtis AR, Wright AJ, Fleming GJ. The influence of surface modification techniques on the performance of a Y-TZP dental ceramic. J Dent. 2006;34:195–206. doi: 10.1016/j.jdent.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 11.Guazzato M, Quach L, Albakry M, Swain MV. Influence of surface and heat treatments on the flexural strength of Y-TZP dental ceramic. J Dent. 2005;33:9–18. doi: 10.1016/j.jdent.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Guazzato M, Albakry M, Quach L, Swain MV. Influence of grinding, sandblasting, polishing and heat treatment on the flexural strength of a glass-infiltrated alumina-reinforced dental ceramic. Biomaterials. 2004;25:2153–2160. doi: 10.1016/j.biomaterials.2003.08.056. [DOI] [PubMed] [Google Scholar]
- 13.Karakoca S, Yilmaz H. Influence of surface treatments on surface roughness, phase transformation, and biaxial flexural strength of Y-TZP ceramics. J Biomed Mater Res B Appl Biomater. 2009;91:930–937. doi: 10.1002/jbm.b.31477. [DOI] [PubMed] [Google Scholar]
- 14.Guess PC, Zhang Y, Kim JW, Rekow ED, Thompson VP. Damage and reliability of Y-TZP after cementation surface treatment. J Dent Res. 2010;89:592–596. doi: 10.1177/0022034510363253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denry IL, Peacock JJ, Holloway JA. Effect of heat treatment after accelerated aging on phase transformation in 3Y-TZP. J Biomed Mater Res B Appl Biomater. 2010;93:236–243. doi: 10.1002/jbm.b.31580. [DOI] [PubMed] [Google Scholar]
- 16.Sato H, Yamada K, Pezzotti G, Nawa M, Ban S. Mechanical properties of dental zirconia ceramics changed with sandblasting and heat treatment. Dent Mater J. 2008;27:408–414. doi: 10.4012/dmj.27.408. [DOI] [PubMed] [Google Scholar]
- 17.Manawi M, Ozcan M, Madina M, Cura C, Valandro LF. Impact of surface finishes on the flexural strength and fracture toughness of In-Ceram Zirconia. Gen Dent. 2012;60:138–142. [PubMed] [Google Scholar]
- 18.Işeri U, Ozkurt Z, Yalnız A, Kazazoğlu E. Comparison of different grinding procedures on the flexural strength of zirconia. J Prosthet Dent. 2012;107:309–315. doi: 10.1016/S0022-3913(12)60081-X. [DOI] [PubMed] [Google Scholar]
- 19.Souza RO, Valandro LF, Melo RM, Machado JP, Bottino MA, Ozcan M. Air-particle abrasion on zirconia ceramic using different protocols: effects on biaxial flexural strength after cyclic loading, phase transformation and surface topography. J Mech Behav Biomed Mater. 2013;26:155–163. doi: 10.1016/j.jmbbm.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 20.Denry IL, Holloway JA, Tarr LA. Effect of heat treatment on microcrack healing behavior of a machinable dental ceramic. J Biomed Mater Res. 1999;48:791–796. doi: 10.1002/(sici)1097-4636(1999)48:6<791::aid-jbm5>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 21.Garvie RC, Nicholson PS. Phase analysis in zirconia systems. J Am Ceram Soc. 1972;55:303–305. [Google Scholar]
- 22.Toraya H, Yoshimura M, Somiya S. Calibration curve for quantitative analysis of the monoclinic-tetragonal ZrO2 system by X-ray diffraction. J Am Ceram Soc. 1984;67:C119–C121. [Google Scholar]
- 23.Chintapalli RK, Marro FG, Jimenez-Pique E, Anglada M. Phase transformation and subsurface damage in 3Y-TZP after sandblasting. Dent Mater. 2013;29:566–572. doi: 10.1016/j.dental.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Kosmac T, Oblak C, Jevnikar P, Funduk N, Marion L. The effect of surface grinding and sandblasting on flexural strength and reliability of Y-TZP zirconia ceramic. Dent Mater. 1999;15:426–433. doi: 10.1016/s0109-5641(99)00070-6. [DOI] [PubMed] [Google Scholar]
- 25.Bona AD, Anusavice KJ, DeHoff PH. Weibull analysis and flexural strength of hot-pressed core and veneered ceramic structures. Dent Mater. 2003;19:662–669. doi: 10.1016/s0109-5641(03)00010-1. [DOI] [PubMed] [Google Scholar]
- 26.Kern M, Wegner SM. Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater. 1998;14:64–71. doi: 10.1016/s0109-5641(98)00011-6. [DOI] [PubMed] [Google Scholar]
- 27.Song JY, Park SW, Lee K, Yun KD, Lim HP. Fracture strength and microstructure of Y-TZP zirconia after different surface treatments. J Prosthet Dent. 2013;110:274–280. doi: 10.1016/S0022-3913(13)60376-5. [DOI] [PubMed] [Google Scholar]
- 28.Monaco C, Tucci A, Esposito L, Scotti R. Microstructural changes produced by abrading Y-TZP in presintered and sintered conditions. J Dent. 2013;41:121–126. doi: 10.1016/j.jdent.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 29.Denry IL, Holloway JA. Microstructural and crystallographic surface changes after grinding zirconia-based dental ceramics. J Biomed Mater Res B Appl Biomater. 2006;76:440–448. doi: 10.1002/jbm.b.30382. [DOI] [PubMed] [Google Scholar]
- 30.Deville S, Chevalier J, Gremillard L. Influence of surface finish and residual stresses on the ageing sensitivity of biomedical grade zirconia. Biomaterials. 2006;27:2186–2192. doi: 10.1016/j.biomaterials.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 31.Mecholsky JJ., Jr Fracture mechanics principles. Dent Mater. 1995;11:111–112. doi: 10.1016/0109-5641(95)80044-1. [DOI] [PubMed] [Google Scholar]
- 32.Seghi RR, Sorensen JA. Relative flexural strength of six new ceramic materials. Int J Prosthodont. 1995;8:239–246. [PubMed] [Google Scholar]
- 33.Guazzato M, Albakry M, Ringer SP, Swain MV. Strength, fracture toughness and microstructure of a selection of allceramic materials. Part II. Zirconia-based dental ceramics. Dent Mater. 2004;20:449–456. doi: 10.1016/j.dental.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Curtis AR, Wright AJ, Fleming GJ. The influence of simulated masticatory loading regimes on the bi-axial flexure strength and reliability of a Y-TZP dental ceramic. J Dent. 2006;34:317–325. doi: 10.1016/j.jdent.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 35.Itinoche KM, Ozcan M, Bottino MA, Oyafuso D. Effect of mechanical cycling on the flexural strength of densely sintered ceramics. Dent Mater. 2006;22:1029–1034. doi: 10.1016/j.dental.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 36.Yilmaz H, Aydin C, Gul BE. Flexural strength and fracture toughness of dental core ceramics. J Prosthet Dent. 2007;98:120–128. doi: 10.1016/S0022-3913(07)60045-6. [DOI] [PubMed] [Google Scholar]
- 37.ISO 6872:2008. Dentistry-ceramic materials. Geneva; Switzerland: ISO; 2008. [Google Scholar]
- 38.Borchers L, Stiesch M, Bach FW, Buhl JC, Hübsch C, Kellner T, Kohorst P, Jendras M. Influence of hydrothermal and mechanical conditions on the strength of zirconia. Acta Biomater. 2010;6:4547–4552. doi: 10.1016/j.actbio.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 39.Oh SC, Dong JK, Lüthy H, Schärer P. Strength and microstructure of IPS Empress 2 glass-ceramic after different treatments. Int J Prosthodont. 2000;13:468–472. [PubMed] [Google Scholar]