Abstract
BACKGROUND AND OBJECTIVE:
Experts suggest family engagement in care can improve safety for hospitalized children. Family-centered rounds (FCRs) can offer families the opportunity to participate in error recovery related to children’s medications. The objective of this study was to describe family-initiated dialogue about medications and health care team responses to this dialogue during FCR to understand the potential for FCR to foster safe medication use.
METHODS:
FCR were video-recorded daily for 150 hospitalized children. Coders sorted family-initiated medication dialogue into mutually exclusive categories, reflecting place of administration, therapeutic class, topic, and health care team responses. Health care team responses were coded to reflect intent, actions taken by the team, and appropriateness of any changes.
RESULTS:
Eighty-three (55%) of the 150 families raised 318 medication topics during 347 FCR. Most family-initiated dialogue focused on inpatient medications (65%), with home medications comprising 35%. Anti-infectives (31%), analgesics (14%), and corticosteroids (11%) were the most commonly discussed medications. The most common medication topics raised by families were scheduling (24%) and adverse drug reactions (11%). Although most health care team responses were provision of information (74%), appropriate changes to the child’s medications occurred in response to 8% of family-initiated dialogue, with most changes preventing or addressing adverse drug reactions or scheduling issues.
CONCLUSIONS:
Most families initiated dialogue regarding medications during FCRs, including both inpatient and home medications. They raised topics that altered treatment and were important for medication safety, adherence, and satisfaction. Study findings suggest specific medication topics that health care teams can anticipate addressing during FCR.
Keywords: family, medication errors, physician-patient/parent communication, adverse drug reactions, patient safety
What’s Known on This Subject:
Family engagement in the care of hospitalized children may improve outcomes, including medication safety. Although family-centered rounds (FCRs) provide a venue for family engagement in care, how families use this venue to influence medication-related topics is unknown.
What This Study Adds:
Most families initiated medication-related dialogue during FCRs, discussing inpatient and home medications. Topics raised were important for medication adherence and safety, even altering treatment plans. Findings suggest specific medication topics that health care team members can anticipate addressing during FCR.
Pediatric patients are especially susceptible to medication safety issues, including medication errors as well as harm from use, nonuse, or misuse of medications, due in part to children’s incomplete physiologic development and the complexities of medication delivery systems.1–4 Medication errors in the inpatient pediatric population occur at 3 times the rate of adult counterparts.5 Although preventing errors is a laudable goal, the fact that health care delivery requires the involvement of human providers and patients suggests that preventing all errors is not realistic.6,7 Therefore, a process that identifies errors before they reach a patient and remediates errors to reduce harm is crucial.6
Error recovery describes this type of process and includes 3 stages: (1) detection; (2) explanation; and (3) correction.8 Detection involves identifying the error and can be done by the person committing the error or by others familiar with the care plan. Explanation involves understanding how the error occurred. Correction involves the implementation of a new or modified care plan. Although error recovery can be performed by a single health care team member, the most robust error recovery strategies reside at the level of the health care system and are dependent on the involvement of other team members and patients.6,9–11 Families, who are experts on the health and care of their children, could contribute meaningfully to any or all of these error recovery stages.
In the inpatient setting, the American Academy of Pediatrics recommends family-centered rounds (FCRs) in which the medical team, family, and patient are all present and encouraged to participate as standard of practice.12 FCRs represent an established venue in which several of the key features of successful error recovery are present.8,9,13 Specifically, FCRs often include monitoring medication outcomes and review of treatment plans under the watchful eyes of those most knowledgeable about the child’s care, such as attending physicians, nurses, pharmacists, and the family.14,15 The objective of the present study was to further understand the potential for FCRs to foster pediatric medication safety. To that end, the study describes and quantifies medication-related topics raised by families during FCR and how this dialogue affects the children’s treatment plans.
Methods
Participants and Data Collection
Participants were enrolled from October 2010 through May 2011 at a Midwestern, tertiary care, academic children’s hospital with 61 inpatient beds. Patients admitted to the general pediatric hospitalist, pulmonology, and hematology/oncology services were eligible to participate. Patients with sensitive reasons for admission (eg, child abuse, mental health issues) or without parents available to provide consent were ineligible.
Our general pediatric hospitalist service admits children with acute concerns while the other services admit mostly children with ongoing illnesses (eg, cystic fibrosis, sickle cell disease, pediatric cancers). The attending or fellow, senior resident, 1 to 2 interns, 1 to 4 medical students, and the patient’s nurse participate in FCRs, with other team members as needed (eg, a social worker, pharmacist). The attending on the pediatric hospitalist service is a hospitalist; the other services have subspecialist attending physicians. FCRs routinely include the intern or student’s formal presentation of the child’s case by using lay language, any status updates, and the plans for the hospital day as well as discharge criteria and plans. Upon admission, families receive 1 page of information about FCRs as part of a standard 16-page packet of information. The purpose, who participates, what to expect, and how families can prepare for FCRs are discussed. Recommendations for preparation include: (1) writing down questions; (2) making the team aware of any sensitive issues; and (3) having the child’s medication schedule.
Of 233 parents of eligible admissions, 194 agreed to learn about the study from our research team; 172 (87%) agreed to participate. Participants provided written consent to have their FCRs video-recorded daily and completed surveys of demographic and hospitalization characteristics. Families were informed that the study would help the hospital understand how health care providers and families work together to provide care during FCRs. Health care team members also consented to being video-recorded for this study. The University of Wisconsin–Madison Health Sciences institutional review board approved this study.
Assessment of Family-Initiated Medication Dialogue
From the FCR videos, trained coders assessed family-initiated medication dialogue. Because we wanted to understand the medication topics that would arise from the perspective of the family, we evaluated only instances of family-initiated medication dialogue. We did not include family responses to medication topics initiated by the health care team. To describe family-initiated dialogue about medications, our goal was to understand the following: (1) the place of administration (inpatient or home); (2) the medication’s therapeutic class; and (3) the specific topic raised (eg, scheduling or route of the drug). Inpatient medications were subdivided into current (patient is receiving the medication) or new (a new order for this medication is being considered). For health care team responses to each instance of family-initiated medication dialogue, we wished to describe: (1) the type of response (eg, change to medication treatment plan, provision of information); (2) how the family’s initiation of this dialogue influenced the child’s medication treatment plan (eg, initiating a new medication or changing the route of a medication); and (3) whether the change in medication was inappropriate, reflecting overuse, underuse, or misuse.16
To develop the new coding scheme required for this work, a team of physicians, pharmacists, and doctorate of pharmacy students reviewed the literature on medication safety and pharmacist participation in rounds.17–20 From this literature, the team constructed a draft list of categories to describe each of the coding scheme elements. Team members applied this coding scheme to FCR videos and iteratively revised it to ensure an exhaustive set of options to describe family-initiated dialogue and health care team responses. Supplemental Table 6 provides descriptions of the full coding scheme, including codes and definitions. Revisions included adding descriptors to capture topics not initially recognized from the literature (eg, family dialogue seeking a medication suggestion) and selection of the 8 most common therapeutic classes used in our population. Coders received 25 hours of training over 5 weeks, using a training manual and pilot FCR videos.
Coding of Dialogue
A pair of trained coders reviewed each FCR video and categorized all family-initiated medication dialogue and health care team responses into mutually exclusive categories, using Noldus Observer.21 Discrepancies were resolved by consensus.
Analyses
Analyses including percentages, means, and SDs were used to describe our participants, the family-initiated medication dialogue, and health care team responses. Generalized estimating equations with the log link and robust SEs were used to compare parent, child, and hospitalization characteristics for families who initiated medication dialogue to those of all families who attended FCRs.
Results
Prevalence of Family-Initiated Medication Dialogue During FCR
Among 172 families who agreed to participate, 150 families had a video of their FCR for each day of their hospital stay and survey data. A total of 347 FCR videos from these 150 patients were examined for family-initiated medication dialogue. Parents were predominantly mothers (85%), white, non-Hispanic (85%), and had a range of educational attainment (Table 1). The mean age of the child was 5.7 years, and a wide variety of reasons for hospitalization were represented.
TABLE 1.
Parent, Child, and Hospitalization Characteristics
| Characteristic | All Families (n = 150) | Families Initiating Medication Dialogue (n = 83) |
|---|---|---|
| Mother | 85% (127) | 86% (72) |
| White, non-Hispanic | 85% (125) | 86% (71) |
| Parent education | ||
| High school or less | 19% (28) | 14% (12) |
| Some college | 35% (53) | 34% (28) |
| Bachelor's degree or more | 47% (70) | 52% (43) |
| Parent age, y | 35 ± 7.8 | 36 ± 7.8 |
| Female child | 49% (73) | 49% (41) |
| Child age, y | 5.7 ± 5.6 | 6.2 ± 5.5 |
| Child health status | ||
| Excellent to good | 87% (131) | 88% (73) |
| Admitting service | ||
| Pulmonary | 14% (21) | 19% (16) |
| Hematology/oncology | 14% (21) | 13% (11) |
| General pediatrics | 72% (108) | 67% (56) |
| Reason for hospitalizationa | ||
| Breathing problem | 29% (44) | 31% (26) |
| Stomach or intestinal problem | 22% (33) | 25% (21) |
| Fever | 17% (26) | 16% (13) |
| Asthmab | 12% (18) | 17% (14) |
| Seizure or headache | 6% (9) | 5% (4) |
| Cancer | 6% (9) | 6% (5) |
| Hematologic disease | 5% (7) | 6% (5) |
| Cystic fibrosis | 4% (6) | 7% (6) |
| Other | 22% (33) | 18% (15) |
| Length of stay | ||
| 1 d | 63% (94) | 50% (41) |
| 2–3 d | 18% (27) | 24% (20) |
| 4–7 d | 10% (15) | 12% (10) |
| >1 wk | 9% (14) | 15% (12) |
Data are presented as % (n) or mean ± SD. Values may not add to 100% due to rounding.
The number of reasons for hospitalization is greater than the number of families because parents could indicate multiple reasons for hospitalization.
P < .05.
Among the 347 FCR videos, 132 (38%) contained at least 1 instance of family-initiated medication dialogue. In total, 318 such instances occurred in the 132 FCR videos. These 132 FCRs came from 83 families (ie, 55% of the families enrolled). Families who initiated medication-related dialogue were not significantly different from the overall group of families who attended FCR, with the exception that families of children hospitalized for asthma were more likely to initiate medication-related dialogue (Table 1).
Place-of Medication Administration
Discussion of inpatient medications comprised 65% of the instances of family-initiated medication dialogue and home medications comprised 35%. Most family-initiated dialogue about inpatient medications focused on current medications while consideration of new medications comprised only 15% of this dialogue.
Therapeutic Class of Medications About Which Families Initiated Dialogue
Families most often initiated medication dialogue regarding anti-infectives (31%), analgesics (14%), and corticosteroids (11%) (Supplemental Table 7). Other common medications raised for discussion were β-agonists (6%) and antiemetic agents (5%).
Medication Topics Raised by Families
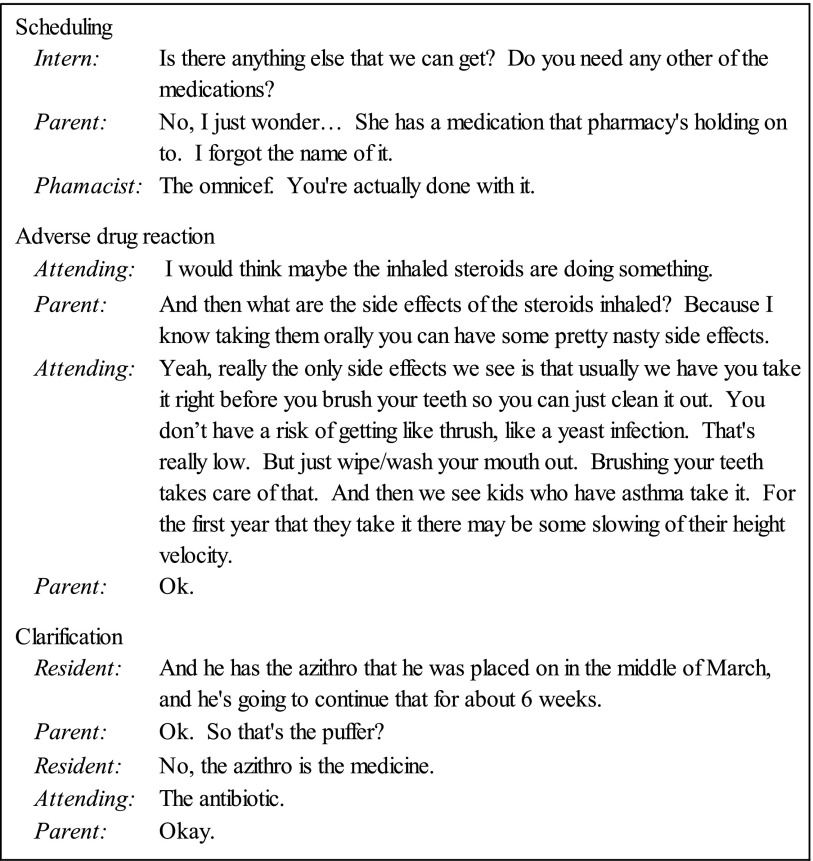
The most common medication topic raised by families was scheduling (medication timing, frequency, or duration), comprising 77 (24%) of the 318 instances of family initiated dialogue (Table 2). Other common topics included adverse drug reactions (ADRs; 11%), clarifications about the drug (10%), and drug indication (9%). Illustrative examples of common topics in family-initiated medication dialogue are given in Figure 1.
TABLE 2.
Family-Initiated Medication Dialogue Topics During FCRS (N = 318)
| Dialogue Topic | % | N |
|---|---|---|
| Scheduling | 24.2 | 77 |
| ADR | 11.0 | 35 |
| Clarification | 10.1 | 32 |
| Indication | 9.4 | 30 |
| Dose or rate | 8.2 | 26 |
| Route | 7.9 | 25 |
| Suggestion | 6.9 | 22 |
| Formulation | 4.1 | 13 |
| Missing medication | 3.8 | 12 |
| Contraindication or interaction | 1.6 | 5 |
| Monitoring | 1.3 | 4 |
| Duplication | <0.1 | 2 |
| Other | 11.0 | 35 |
Values may not add to 100% due to rounding.
FIGURE 1.
Examples of common medication topics initiated by families.
Health Care Team Member Responses to Family-Initiated Medication Dialogue
The majority (74%) of health care team responses to family-initiated medication dialogue involved providing information to the family (Table 3). In some instances, the health care team simply acknowledged the dialogue (13%). Occasionally, the health care team deferred responding to family-initiated medication dialogue (5%), often waiting for additional information from other health care team members. Only rarely did the health care team not respond to family-initiated medication dialogue (1% of instances).
TABLE 3.
Health Care Team Responses to Family-Initiated Medication-Related Dialogue (N = 318)
| Response | % | N |
|---|---|---|
| Inform | 73.6 | 234 |
| Acknowledgment | 12.6 | 40 |
| Change | 7.9 | 25 |
| Defer | 4.7 | 15 |
| No response | 1.3 | 4 |
Values may not add to 100% due to rounding.
Changes to Treatment Resulting From Family-Initiated Medication Dialogue
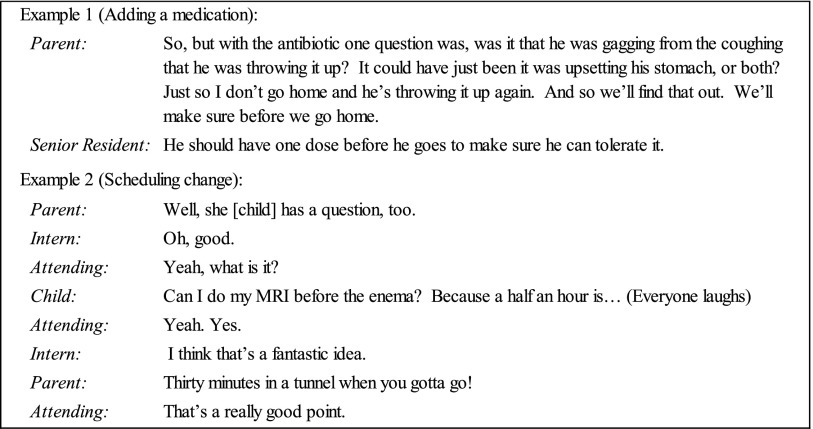
In response to 8% of instances in which families initiated medication-related dialogue, a change to the medication treatment plan occurred (Table 3). Figure 2 contains examples of family-initiated dialogue that resulted in changes to the child’s medications. Of the 25 medication treatment plans that were changed, most were changed by adding a medication (44%) or through scheduling changes (24%) (Table 4). Typical medication additions in response to family-initiated dialogue included prevention or treatment of antibiotic-related diarrhea by adding probiotics. Similarly, a test dose of oral antibiotic before discharge could be added to ensure the child tolerated oral antibiotics at home. Medications were stopped in 12% of instances. The remaining changes involved the medication’s dose or rate, route, or formulation. On review, none of the changes was found to be inappropriate.
FIGURE 2.
Examples of changes to medications as a result of family-initiated dialogue.
TABLE 4.
Health Care Team Medication Treatment Plan Changes (n = 25)
| Treatment Plan Change | % | N |
|---|---|---|
| Add medication | 44 | 11 |
| Scheduling change | 24 | 6 |
| Stop medication | 12 | 3 |
| Dose or rate change | 8 | 2 |
| Route change | 8 | 2 |
| Formulation change | 4 | 1 |
Family-Initiated Medication Topics Resulting in Changes to Treatment Plan
Changes to the child’s medications were prompted by a variety of topics raised by families during FCRs. ADRs were the most commonly raised topic that resulted in changes to the child’s medications (20% of changes). Other topics that commonly resulted in changes included family-initiated dialogue about the scheduling of medications (16%) and dialogue requesting that the team make a suggestion for a medication for the child (16%) (Table 5).
TABLE 5.
Family-Initiated Medication Dialogue Topics That Prompted Changes to the Child's Treatment Plan (n = 25)
| Dialogue Topic | % | N |
|---|---|---|
| Adverse drug reaction | 20 | 5 |
| Scheduling | 16 | 4 |
| Suggestion | 16 | 4 |
| Dose or rate | 12 | 3 |
| Other | 12 | 3 |
| Route | 8 | 2 |
| Indication | 8 | 2 |
| Clarification | 4 | 1 |
| Formulation | 4 | 1 |
Discussion
The potential benefits of FCRs include greater satisfaction with care and better family understanding of treatment plans.22–24 Our data go further, describing families’ contributions to FCRs and the impact on treatment. Families commonly used FCRs to engage with the health care team regarding children’s medications. Furthermore, 8% of these instances resulted in medication changes, suggesting families may raise topics that facilitate the process of identifying and addressing potential adverse drug events (error recovery). In general, families who initiated medication dialogue were not demographically distinct from families who simply attended rounds. Their medication dialogue referenced both inpatient medications and home medications. Many different medication topics were raised, including scheduling of medications and potential ADRs. Our findings suggest the importance of FCRs as a system-level process to promote pediatric medication safety, adherence, and satisfaction with care.
Medication Safety
By actively raising medication topics, families contributed meaningfully to FCRs in ways that mirror the medication error recovery stages of detection and correction. Without these contributions, errors in families’ understanding of the medication plan may not have been detected, ultimately resulting in medication misuse, underuse, or overuse. For example, in Figure 1, had the family not questioned the attending’s instructions for the use of the child’s antibiotic or the inhaler, they might not have given the prescribed course of antibiotics but mistakenly continued the inhaler for weeks. FCRs provide a venue to clarify information, supporting detection and correction of medication errors before they reach the child.
Furthermore, in response to 8% of the instances of family-initiated medication dialogue, the child’s medications were changed. This activity is reflective of the correction stage of error recovery. Although changes initiated by the family could result in inappropriate medication use, there was no evidence of this outcome within our data. In fact, consistent with the examples in Figure 2, often the family’s contribution prompted creation of a better treatment plan. In those examples, families prompted a test of whether their child could tolerate oral medication before discharge and ensured that an enema was scheduled in a manner that did not interfere with the child’s MRI. In addition, a recent study found that no differences existed in the number of medications ordered for children who did or did not participate in FCRs, suggesting that FCRs are not associated with increased medication use.24
Medication Adherence
The topics raised by families have important implications for medication adherence, especially after discharge. Concerns about adverse drug events, including ADRs, reduce adherence25,26 and family-initiated dialogue about ADRs was the most common reason for changing the child’s medications. Because patient reports of ADRs and other adverse events are often indicative of actual adverse events,27 when families raise these concerns, health care team members should consider the information carefully. In addition, families also raised concerns about ADRs that may occur in the future. For example, the family member in Figure 1 who expressed concern about adverse effects of inhaled corticosteroids created an opportunity to prevent a potential medication error in the form of underuse of the inhaled corticosteroids. Lack of adherence to this medication could have even resulted in future asthma exacerbations and health care utilization.
Family-initiated medication dialogue also promoted adherence by prompting changes to medication schedules. Scheduling of home medications, especially ensuring medications do not conflict with activities such as school, is critical to adherence.28–30 With much of the family-initiated dialogue regarding medication scheduling revolving around medications used after discharge, FCRs provide a structured opportunity to close the communication loop with families, with the goal of reducing medication errors upon transition to the home environment.
Family and Patient Satisfaction
FCR provided a forum for better information sharing, which can ultimately result in increased satisfaction with care.24,31,32 Specifically, in our second example in Figure 2, had the child not proactively raised concerns about scheduling an enema before her MRI, unanticipated harms could have occurred, such as emotional distress and delays in receiving diagnostic information. Furthermore, families commonly raised topics that reflected their need for clarification regarding medications. Previous literature indicates that patients have increased satisfaction with their care when they are able to engage in a dialogue about their medications.33 FCRs present opportunities for the health care team to provide family-centered care by addressing information needs as identified by the family.12
Guidance for Health Care Team Members Performing FCRs
Several of our findings provide health care teams with guidance for responding to family-initiated medication dialogue during FCRs. First, families who initiated medication-related dialogue were no different demographically than those who did not; therefore, health care team members cannot predict which families may initiate medication topics. However, because families of children with asthma were more likely to initiate this dialogue, healthcare teams can anticipate and prepare for a discussion of asthma medications. These discussions have a multitude of potential benefits given the high readmission rate for asthma patients often caused by nonadherence.34 Second, given the commonplace nature of family-initiated dialogue regarding home medications, having an efficient process for addressing questions about home medications is crucial. After discharge, families become responsible for administering and monitoring children’s medications. Adverse drug events, defined as harm resulting from use, nonuse, or misuse of medication, occur in 14% of pediatric outpatient receiving a prescription.35 The majority of preventable adverse drug events (70%) occur during parental administration rather than in earlier stages such as medication ordering. Thus, discussion about home medications is crucial to partnering with families regarding safe medication use. To facilitate this, our institution provides families with written medication information in a patient/family-friendly format.36
For our population, which included children hospitalized for acute and chronic illnesses, there may be specific types of medications that health care team members can anticipate arising during FCRs. Not surprisingly, families most often initiated dialogue about medications such as anti-infectives and analgesics. These medications are frequently used during pediatric hospitalizations for acute conditions and in our study’s chronic disease populations, such as children with cystic fibrosis exacerbations or with chemotherapy-associated fever and neutropenia. These medications are known to be common sources of pediatric medication errors.5,37 Furthermore, analgesics include narcotics, a common cause of harm from medication use or misuse in children.38–40
For some medications such as inhaled steroids, the frequency with which families raise these medications for discussion may be influenced by perceptions of potential adverse reactions (eg, irritability or stunted growth), by the multiple potential administration routes (eg, oral steroids versus inhaled steroids), or by their complicated administration techniques (eg, nebulizers and dry powder or metered-dose inhalers).25,41,42 In addition, confusion can occur regarding the purpose of a rescue inhaler versus a maintenance inhaler, which can lead to misuse.43 These topics can be anticipated and responded to during the FCRs, allowing trainees to practice their responses to common family-initiated medication-related topics.
Limitations
Although we recruited patients from multiple different services, our data arise from a single Midwestern institution and many participants were admitted for acute disease; the findings may therefore not be generalizable broadly to other institutions or diverse populations. However, families who initiated medication-related dialogue did not differ on demographic characteristics or health status from those who did not initiate such a dialogue. In addition, while our recruitment rate was high, families who did not participate may hold less favorable views of FCRs, leading to potential overestimation of the amount of family-initiated medication dialogue. Also, families were aware they were being video-recorded, but whether this awareness could increase or decrease the initiation of medication-related dialogue is unknown; previous literature has suggested, however, that video-recorded interactions in the health care setting do not differ from nonrecorded interactions.44,45
Conclusions
Most families initiated dialogue regarding medications during FCRs. The families who initiated medication dialogue did not differ in terms of demographic or health status from those who did not initiate medication dialogue. Family-initiated medication dialogue typically referenced both inpatient medications and home medications. Families’ contributions resulted in appropriate changes to treatment plans. Our findings suggest the importance of FCRs as a system-level process to promote medication safety, adherence, and satisfaction with care.
Supplementary Material
Footnotes
Dr Benjamin conceived and designed the study; oversaw all data collection, coding, and analyses; and drafted and revised the manuscript; Dr Cox secured funding, conceived and designed the study, oversaw all data collection and analyses, and revised the manuscript; Dr Trapskin, Mr Jorgenson, Dr Carayon, and Dr Lubcke assisted with development of the coding scheme and revised the manuscript; Ms Rajamanickam performed analyses and revised the manuscript; and Dr Weber and Dr Pearson assisted with development of the coding scheme, coded the data, and revised the manuscript. All authors approved the final version for submission.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders. The funders had no role in designing, conducting, or reporting the results of this study.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This work was funded through an Agency for Healthcare Research and Quality Health Services Research Dissemination and Demonstration grant (R18 HS018680) to Dr Cox. The project described was also supported by the Clinical and Translational Science Award program, previously through the National Center for Research Resources (grant 1UL1RR025011) and now by the National Center for Advancing Translational Sciences (grant 9U54TR000021). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Ghaleb MA, Barber N, Franklin BD, Wong ICK. The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child. 2010;95(2):113–118 [DOI] [PubMed] [Google Scholar]
- 2.Stucky ER, American Academy of Pediatrics Committee on Drugs. American Academy of Pediatrics Committee on Hospital Care . Prevention of medication errors in the pediatric inpatient setting. Pediatrics. 2003;112(2):431–436 [DOI] [PubMed] [Google Scholar]
- 3.Institute for Safe Medication Practices (ISMP) Canada. Definitions of terms. Available at: www.ismp-canada.org/definitions.htm. Accessed October 23, 2014
- 4.Committee of Experts on Management of Safety and Quality in Health Care (SP-SQS) Expert Group on Safe Medication Practices. Glossary of terms related to patient and medication safety. Available at: www.bvs.org.ar/pdf/seguridadpaciente.pdf. Accessed October 23, 2014
- 5.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–2120 [DOI] [PubMed] [Google Scholar]
- 6.Wetterneck TB. Error recovery in health care. In: Carayon P, ed. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2nd ed. Boca Raton, FL: CRC Press; 2012:449–461 [Google Scholar]
- 7.Alper SJ, Karsh BT. A systematic review of safety violations in industry. Accid Anal Prev. 2009;41(4):739–754 [DOI] [PubMed] [Google Scholar]
- 8.Kanse L, van der Schaaf TW, Vrijland ND, van Mierlo H. Error recovery in a hospital pharmacy. Ergonomics. 2006;49(5–6):503–516 [DOI] [PubMed] [Google Scholar]
- 9.Kontogiannis T, Embrey D. A user-centred design approach for introducing computer-based process information systems. Appl Ergon. 1997;28(2):109–119 [DOI] [PubMed] [Google Scholar]
- 10.Leplat J. Error analysis, instrument and object of task-analysis. Ergonomics. 1989;32(7):813–822 [Google Scholar]
- 11.Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. J Gen Intern Med. 2005;20(9):830–836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Committee on Hospital Care. American Academy of Pediatrics . Family-centered care and the pediatrician’s role. Pediatrics. 2003;112(3 pt 1):691–697 [PubMed] [Google Scholar]
- 13.Sellen AJ. Detection of everyday errors. Appl Psychol. 1994;43(4):475–498 [Google Scholar]
- 14.Kelly MM, Xie A, Carayon P, DuBenske LL, Ehlenbach ML, Cox ED. Strategies for improving family engagement during family-centered rounds. J Hosp Med. 2013;8(4):201–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muething SE, Kotagal UR, Schoettker PJ, Gonzalez del Rey J, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829–832 [DOI] [PubMed] [Google Scholar]
- 16.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–543 [PubMed] [Google Scholar]
- 17.Rothschild JM, Churchill W, Erickson A, et al. Medication errors recovered by emergency department pharmacists. Ann Emerg Med. 2010;55(6):513–521 [DOI] [PubMed] [Google Scholar]
- 18.Leape LL, Cullen DJ, Clapp MD, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282(3):267–270 [DOI] [PubMed] [Google Scholar]
- 19.Kucukarslan SN, Peters M, Mlynarek M, Nafziger DA. Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Arch Intern Med. 2003;163(17):2014–2018 [DOI] [PubMed] [Google Scholar]
- 20.Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):481–493 [DOI] [PubMed] [Google Scholar]
- 21.Noldus Information Technology. The Observer Basic. Version 5.0 ed. Leesburg, VA: Noldus Information Technology; 2004
- 22.Mittal VS, Sigrest T, Ottolini MC, et al. Family-centered rounds on pediatric wards: a PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126(1):37–43 [DOI] [PubMed] [Google Scholar]
- 23.Rappaport DI, Ketterer TA, Nilforoshan V, Sharif I. Family-centered rounds: views of families, nurses, trainees, and attending physicians. Clin Pediatr (Phila). 2012;51(3):260–266 [DOI] [PubMed] [Google Scholar]
- 24.Kuo DZ, Sisterhen LL, Sigrest TE, Biazo JM, Aitken ME, Smith CE. Family experiences and pediatric health services use associated with family-centered rounds. Pediatrics. 2012;130(2):299–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winnick S, Lucas DO, Hartman AL, Toll D. How do you improve compliance? Pediatrics. 2005;115(6) . Available at: www.pediatrics.org/cgi/content/full/115/6/e718 [DOI] [PubMed] [Google Scholar]
- 26.Wandstrat TL, Kaplan B. Pharmacoeconomic impact of factors affecting compliance with antibiotic regimens in the treatment of acute otitis media. Pediatr Infect Dis J. 1997;16(suppl 2):S27–S29 [DOI] [PubMed] [Google Scholar]
- 27.Zhu J, Stuver SO, Epstein AM, Schneider EC, Weissman JS, Weingart SN. Can we rely on patients’ reports of adverse events? Med Care. 2011;49(10):948–955 [DOI] [PubMed] [Google Scholar]
- 28.Ho J, Taylor DM, Cabalag MS, Ugoni A, Yeoh M. Factors that impact on emergency department patient compliance with antibiotic regimens. Emerg Med J. 2010;27(11):815–820 [DOI] [PubMed] [Google Scholar]
- 29.Fenerty SD, O’Neill JL, Gustafson CJ, Feldman SR. Maternal adherence factors in the treatment of pediatric atopic dermatitis. JAMA Dermatol. 2013;149(2):229–231 [DOI] [PubMed] [Google Scholar]
- 30.Brown KK, Rehmus WE, Kimball AB. Determining the relative importance of patient motivations for nonadherence to topical corticosteroid therapy in psoriasis. J Am Acad Dermatol. 2006;55(4):607–613 [DOI] [PubMed] [Google Scholar]
- 31.Byczkowski TL, Fitzgerald M, Kennebeck S, et al. A comprehensive view of parental satisfaction with pediatric emergency department visits. Ann Emerg Med. 2013;62(4):340–350 [DOI] [PubMed] [Google Scholar]
- 32.Magaret ND, Clark TA, Warden CR, Magnusson AR, Hedges JR. Patient satisfaction in the emergency department—a survey of pediatric patients and their parents. Acad Emerg Med. 2002;9(12):1379–1388 [DOI] [PubMed] [Google Scholar]
- 33.Kassam R, Collins JB, Berkowitz J. Patient satisfaction with pharmaceutical care delivery in community pharmacies. Patient Prefer Adherence. 2012;6:337–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sadatsafavi M, FitzGerald M, Marra C, Lynd L. Costs and health outcomes associated with primary vs secondary care after an asthma-related hospitalization: a population-based study. Chest. 2013;144(2):428–435 [DOI] [PubMed] [Google Scholar]
- 35.Zandieh SO, Goldmann DA, Keohane CA, Yoon C, Bates DW, Kaushal R. Risk factors in preventable adverse drug events in pediatric outpatients. J Pediatr. 2008;152(2):225–231 [DOI] [PubMed] [Google Scholar]
- 36.Lexicomp. Patient Education. Databases & Modules. Available at: www.lexi.com/institutions/products/online/database-module-descriptions/patient-education/. Accessed October 23, 2014
- 37.Wang JK, Herzog NS, Kaushal R, Park C, Mochizuki C, Weingarten SR. Prevention of pediatric medication errors by hospital pharmacists and the potential benefit of computerized physician order entry. Pediatrics. 2007;119(1). Available at: www.pediatrics.org/cgi/content/full/119/1/e77 [DOI] [PubMed] [Google Scholar]
- 38.Ferranti J, Horvath MM, Cozart H, Whitehurst J, Eckstrand J. Reevaluating the safety profile of pediatrics: a comparison of computerized adverse drug event surveillance and voluntary reporting in the pediatric environment. Pediatrics. 2008;121(5). Available at: www.pediatrics.org/cgi/content/full/121/5/e1201 [DOI] [PubMed] [Google Scholar]
- 39.Sharek PJ, McClead RE, Jr, Taketomo C, et al. An intervention to decrease narcotic-related adverse drug events in children’s hospitals. Pediatrics. 2008;122(4). Available at: www.pediatrics.org/cgi/content/full/122/4/e861 [DOI] [PubMed] [Google Scholar]
- 40.Lee BH, Lehmann CU, Jackson EV, et al. Assessing controlled substance prescribing errors in a pediatric teaching hospital: an analysis of the safety of analgesic prescription practice in the transition from the hospital to home. J Pain. 2009;10(2):160–166 [DOI] [PubMed] [Google Scholar]
- 41.Bukstein DA, Luskin AT, Bernstein A. “Real-world” effectiveness of daily controller medicine in children with mild persistent asthma. Ann Allergy Asthma Immunol. 2003;90(5):543–549 [DOI] [PubMed] [Google Scholar]
- 42.Kelloway JS, Wyatt RA, Adlis SA. Comparison of patients’ compliance with prescribed oral and inhaled asthma medications. Arch Intern Med. 1994;154(12):1349–1352 [PubMed] [Google Scholar]
- 43.Partridge MR, van der Molen T, Myrseth SE, Busse WW. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med. 2006;6:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Penner LA, Orom H, Albrecht TL, et al. Camera-related behaviors during video recorded medical interactions. J Nonverbal Behav. 2007;31(2):99–117 [Google Scholar]
- 45.Pringle M, Stewart-Evans C. Does awareness of being video recorded affect doctors’ consultation behaviour? Br J Gen Pract. 1990;40(340):455–458 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.