Abstract
BACKGROUND:
Use of potentially hazardous bedding, as defined by the American Academy of Pediatrics (eg, pillows, quilts, comforters, loose bedding), is a modifiable risk factor for sudden infant death syndrome and unintentional sleep-related suffocation. The proportion of US infants sleeping with these types of bedding is unknown.
METHODS:
To investigate the US prevalence of and trends in bedding use, we analyzed 1993–2010 data from the National Infant Sleep Position study. Infants reported as being usually placed to sleep with blankets, quilts, pillows, and other similar materials under or covering them in the last 2 weeks were classified as bedding users. Logistic regression was used to describe characteristics associated with bedding use.
RESULTS:
From 1993 to 2010, bedding use declined but remained a widespread practice (moving average of 85.9% in 1993–1995 to 54.7% in 2008–2010). Prevalence was highest for infants of teen-aged mothers (83.5%) and lowest for infants born at term (55.6%). Bedding use was also frequently reported among infants sleeping in adult beds, on their sides, and on a shared surface. The rate of decline in bedding use was markedly less from 2001–2010 compared with 1993–2000. For 2007 to 2010, the strongest predictors (adjusted odds ratio: ≥1.5) of bedding use were young maternal age, non-white race and ethnicity, and not being college educated.
CONCLUSIONS:
Bedding use for infant sleep remains common despite recommendations against this practice. Understanding trends in bedding use is important for tailoring safe sleep interventions.
Keywords: accidental suffocation, infant mortality, safe sleep, sudden infant death syndrome, sudden unexpected infant death, surveillance
What’s Known on This Subject:
The American Academy of Pediatrics has identified bedding such as pillows, blankets, and quilts as potentially hazardous for the infant sleep environment. Bedding use is a modifiable risk factor for sudden infant death syndrome and unintentional sleep-related suffocation.
What This Study Adds:
Reported bedding use over or under the infant for infant sleep substantially declined from 1993 to 2010. However, about one-half of US infants are still placed to sleep with potentially hazardous bedding despite recommendations against this practice.
Rates of sudden infant death syndrome (SIDS), the leading cause of postneonatal mortality, have declined slowly in the United States since 2000, from 66.3 to 52.7 per 100 000 live births in 2010.1 Concurrently, infant mortality related to unintentional sleep-related suffocation, the leading cause of infant mortality from injury, has increased more than twofold, from 7.0 per 100 000 live births in 2000 to 15.9 per 100 000 live births in 2010. Blankets, quilts, and pillows are examples of bedding that can be potentially hazardous to infants if under or around them during sleep. Soft objects and loose bedding such as these items can obstruct the infant airway and pose a suffocation risk. In addition, this type of bedding is a recognized risk factor for SIDS. Because of these risks, the American Academy of Pediatrics (AAP) recommends that soft objects and loose bedding be removed from the infant sleep area.2,3 A US study showed that certain types of bedding increased the odds for SIDS approximately fivefold.4 This finding is consistent with studies from the United States, Europe, New Zealand, and Australia in which adjusted odds ratios (aORs) for SIDS and the use of these types of bedding ranged from 3.1 to 6.7.5–13
Recommendations about the avoidance of bedding in the sleep environment were first issued in 1996 when the AAP advised that infants be placed to sleep in environments free of soft surfaces and gas-trapping objects.14 In April 1999, the Consumer Product Safety Commission, the National Institute of Child Health and Human Development, and the AAP Task Force issued a safety alert recommending that infants “be placed to sleep on their backs on a firm, tight-fitting mattress in a crib that meets current safety standards and that pillows, quilts, comforters, sheepskins and other pillow-like soft products be removed from the crib.”15 In 2000, the AAP more strongly recommended against the use of bedding.16 The proportion of US infants who are placed to sleep with bedding such as pillows, blankets, and quilts is unknown. Understanding caregiver behavior related to infant sleep practices and how it has changed can inform the refinement and promotion of interventions aimed at reducing unsafe practices. In the present study, we used data from the NISP (National Infant Sleep Position) Study17,18 to estimate the prevalence of reported use of certain types of bedding and examine trends from 1993 to 2010 (overall and according to race/ethnicity). We also investigated characteristics associated with bedding use from 2007 to 2010.
Methods
The NISP Study
The NISP methods have been reported previously.17,18 Briefly, NISP was an annual, cross-sectional telephone survey conducted from 1993 to 2010. A random sample of households in the continental United States with infants aged <8 months was chosen from a purchased list containing public information from birth records, infant photography companies, and formula companies. During a telephone interview, nighttime caregivers answered questions about infant sleeping practices (eg, sleep position, location for sleep, use of potentially hazardous bedding) and sociodemographic characteristics. Most respondents (80%) were mothers. Given the increased risk of sleep-related infant deaths in certain racial and ethnic groups,2,4 all respondents were asked to self-report maternal race and ethnicity. The NISP sample underrepresented mothers of black race and Hispanic ethnicity, teenagers, and those with less than a high school education.17 Annual sample size ranged from 1012 to 1188, but an exact response rate could not be calculated because the eligibility status for those refusing the interview was unknown. However, assuming those who refused had the same eligibility proportion as those who participated, the average response rate would be 71% (ranging from 78% in 1993 to 46% in 2010).
Main Outcome and Measures
The main outcome for this analysis was reported usual use of certain types of bedding under the infant or covering the infant while sleeping in the last 2 weeks. Caregivers were asked, “During the past 2 weeks, which of the following items were usually under [infant] while [he/she] slept? Please answer yes or no to each one.” Based on the guidelines from the AAP,2 affirmative responses for blanket, bean bag, waterbed, rug, sheepskin, cushion, sleeping bag, or pillow were classified as having used bedding under the infant. Caregivers were also asked, “During the past 2 weeks, which of the following were usually used to cover [infant] when [he/she] slept at night? Please answer yes or no to each one.” Affirmative responses to sheet, blanket, quilt/comforter, sheepskin, pillow, or other were classified as bedding over the infant or used to cover the infant. Caregivers who answered “blanket” were also asked if the blanket was thicker than a receiving blanket. If the caregiver responded that any of these items were used (excluding sheets and blankets not thicker than a receiving blanket), the infant was classified as having used bedding as a cover. Our definition excluded thin blankets because the AAP had not recommended the removal of thin blankets during the study period.
Statistical Analysis
For each year, the prevalence of bedding use in the sleeping environment was calculated. We further examined the frequency of use according to type, race and ethnicity, and survey year. Trends for bedding use by race or ethnicity were calculated and plotted by using 3-year moving averages. To test if the trend was statistically significant, logistic regression was used to model the association between the year and bedding use. Because the decline in SIDS rates that occurred after the launch of the Back to Sleep Campaign in 1994 has been less dramatic after 2000,19 we investigated if trends in bedding use differed in 1993–2000 compared with 2001–2010. To perform this analysis, we used piecewise logistic regression with a term modeling a change in the odds ratio (OR) for survey year. To investigate these trends according to race and ethnicity, we included an interaction term into the piecewise model and estimated the differences with corresponding contrasts.
Finally, to understand current bedding practices, the most recently available data (2007–2010) were examined. First, we investigated the bedding use in conjunction with other unsafe sleep practices. We calculated the proportion of infants using bedding over or under them by sleep location (crib, bassinet, adult bed, or other), usual sleep position (side, stomach, or back), and whether the infant was in bed alone (yes or no). Second, we examined the independent association of the bedding use with maternal age, education, race and ethnicity, parity, and geographic region; infant gender, age, and preterm birth (<37 weeks); and survey year. We calculated crude ORs and adjusted ORs (aOR) and 95% confidence intervals (CIs) by using multivariable logistic regression. All variables listed were included in the adjusted model. We also looked at factors for all study years but did not observe any major changes in the importance of sociodemographic factors and their association with the bedding use.
All analyses were conducted with commercially available software (SAS version 9.2; SAS Institute, Inc, Cary, NC). Two-sided P values <.05 were considered statistically significant. Because simple random sampling is considered a self-weighted design, sample weights were not applied. The study was reviewed and approved by the institutional review boards of Boston University School of Medicine and Yale University School of Medicine.
Results
Sample Characteristics
From 1993 to 2010, a total of 18 952 participants completed the NISP questionnaire. At interview, nearly two-thirds of the infants were aged ≥16 weeks (62.5%) and most had white mothers (83.3%) (Table 1). About one-half of the infants’ mothers were aged ≥30 years (47.2%), had at least a college education (45.3%), and had a previous child (51.9%). The distributions of these characteristics were similar across study years. Over time, the average prevalence of bedding use varied according to sociodemographic characteristics; prevalence was highest for infants of teen-aged mothers (83.5%) and lowest for infants born at term (55.6%). The most notable differences occurred for maternal age, race and ethnicity, and education, as well as preterm birth status.
TABLE 1.
Characteristics of Study Population and Prevalence of Bedding Use, NISP Study, 1993 to 2010b
| Characteristic | Study Population | Prevalence of Bedding Use,a % | |
|---|---|---|---|
| N | %c | ||
| Mother’s age, y | |||
| <20 | 909 | 4.8 | 83.5 |
| 20–29 | 9053 | 48.0 | 68.4 |
| ≥30 | 8096 | 47.2 | 60.8 |
| Mother’s race and ethnicity | |||
| Other | 816 | 4.3 | 74.6 |
| Hispanic | 1160 | 6.1 | 76.1 |
| Black | 1172 | 6.2 | 75.3 |
| White | 15 728 | 83.3 | 63.5 |
| Mother’s education | |||
| Less than high school | 1050 | 5.6 | 81.9 |
| High school or GED test | 4280 | 22.6 | 73.9 |
| Some college | 5005 | 26.5 | 68.3 |
| College or more | 8569 | 45.3 | 57.7 |
| Infant age, wk | |||
| <8 | 1141 | 7.8 | 68.1 |
| 8–15 | 5456 | 29.7 | 68.1 |
| ≥16 | 11 488 | 62.5 | 64.3 |
| Infant gender | |||
| Female | 9238 | 48.4 | 66.9 |
| Male | 9697 | 51.2 | 64.2 |
| Preterm birth, <37 wk | |||
| Yes | 2171 | 11.5 | 65.2 |
| No | 16 727 | 88.5 | 55.6 |
| First child | |||
| Yes | 8948 | 48.1 | 64.9 |
| No | 9658 | 51.9 | 65.9 |
| Geographic region | |||
| West | 2805 | 14.8 | 75.3 |
| New England | 1030 | 5.4 | 67.3 |
| Mid-Atlantic | 2579 | 13.6 | 65.8 |
| South | 6640 | 35.0 | 61.0 |
| Midwest | 5898 | 31.1 | 65.6 |
GED, General Educational Development.
Refers to certain types of bedding under the infant (blanket, bean bag, waterbed, rug, sheepskin, cushion, sleeping bag, or pillow) or covering the infant (blanket, quilt/comforter, sheepskin, pillow, or other) while sleeping in last 2 weeks. Covers exclude sheets and blankets not thicker than a receiving blanket.
Data include 18 952 participants.
Percentages have been rounded and might not total 100.
Types of Bedding Used
From 1993 to 2010, the prevalence of bedding use varied by type (Table 2). The most frequently reported types of bedding covers were thick blankets (37.6%) and quilts/comforters (19.9%). Blankets (29.2%) and cushions (3.7%) were the most frequently reported type of bedding placed under the infant. The percentage of infants covered with thick blankets or quilts/comforters declined significantly (P < .0001) from 1993 through 2010. Using 3-year moving averages and comparing 1993–1995 versus 2008–2010, use of thick blanket coverings declined from 56.0% to 27.4% and use of quilt/comforter coverings declined from 39.2% to 7.9%. For blankets and cushions under infants, prevalence ranged from 25.5% to 31.9% for blankets and 3.1% to 4.6% for cushions, but no statistically significant declines were observed. Other items under or covering infants were reported <2% of the time for each year.
TABLE 2.
Frequency of Bedding Covering or Under the Infant for Sleep by Type, 1993 to 2010
| Type of Bedding | Total | % |
|---|---|---|
| Covering infant | ||
| Thick blanket | 7084 | 37.6 |
| Quilt/comforter | 3757 | 19.9 |
| Other blanket | 231 | 1.2 |
| Sheepskin | 6 | <0.1 |
| Pillow | 7 | <0.1 |
| Other | 208 | 1.1 |
| Under infant | ||
| Blanket | 5532 | 29.2 |
| Cushion | 695 | 3.7 |
| Pillow | 176 | 0.9 |
| Waterbed | 169 | 0.9 |
| Rug | 150 | 0.8 |
| Sheepskin | 148 | 0.8 |
| Bean bag | 60 | 0.3 |
| Sleeping bag | 8 | <0.1 |
| Other | 109 | 0.5 |
Infants could be categorized in >1 bedding type.
Trends in Any Type of Bedding Use
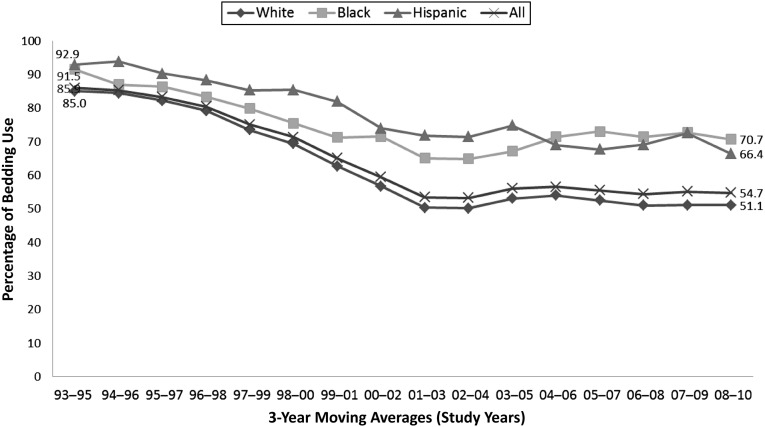
There was a statistically significant decline in reported bedding use (over or under the infant) from 1993 to 2010. Figure 1 shows a decrease in a 3-year moving average from 85.9% to 54.7% over the study period. This finding corresponds to a 10% decline in the odds of bedding use per year (OR: 0.90 [95% CI: 0.89–0.90]). For each racial and ethnic group, we also observed a significant decreasing trend.
FIGURE 1.
Prevalence of the use of bedding according to race and ethnicity: 3-year moving averages, NISP, 1993 to 2010. Bedding refers to certain types of bedding reported under the infant (blanket, bean bag, waterbed, rug, sheepskin, cushion, sleeping bag, or pillow) or covering the infant (blanket, quilt/comforter, sheepskin, pillow, or other) while sleeping in last 2 weeks. Covers exclude sheets and blankets not thicker than a receiving blanket.
To determine if the trend differed in the 1993–2000 period compared with the 2001–2010 period, piecewise analyses were conducted. For each racial and ethnic group, the rate of decline of bedding use over or under the infant was significantly greater from 1993–2000 compared with 2001–2010 (P < .001 for white and black subjects, P = .02 for Hispanic subjects). From 1993 to 2000, each racial and ethnic group had statistically significant declines (22% to 23% per year) in the odds of bedding use. In contrast, from 2001 to 2010, the declines were less apparent. White and Hispanic infants showed a statistically significant but modest decline (5% to 7% per year) in the latter decade. Among black infants, there was no significant decline during this period.
Bedding Use and Other Unsafe Sleep Factors
To describe characteristics related to recent infant sleep practices, we restricted our analyses to 2007 to 2010. During this time, most respondents reported that infants slept with some type of bedding (54.2%), slept in a crib or bassinet (74.2%), were placed to sleep supine (72.6%), and did not share a sleep surface (ie, they slept alone) (86.5%) (Table 3). When we examined bedding use in conjunction with other sleep practices, we found that regardless of sleep location, sleep position, and bed-sharing status, bedding use was consistently close to ≥50%. Bedding use was most prevalent among infants sleeping in adult beds (71.5%), placed to sleep on their sides (66.1%), and sharing a sleep surface (70.0%).
TABLE 3.
Frequency of Different Sleep Practices and Specific Sleep Practice By Bedding Use, NISP, 2007 to 2010
| Type | Sleep Practice (n = 4280) | Sleep Practice by Bedding Usea (n = 2324) | ||
|---|---|---|---|---|
| N | % | N | % | |
| Bedding use | ||||
| Yes | 2324 | 54.2 | ||
| No | 1956 | 45.8 | ||
| Sleep location | ||||
| Crib | 2396 | 56.2 | 1142 | 47.7 |
| Bassinet | 767 | 18.0 | 450 | 58.7 |
| Adult bed | 471 | 11.0 | 337 | 71.5 |
| Other | 633 | 14.8 | 385 | 60.8 |
| Usual sleep position | ||||
| Side | 528 | 12.3 | 349 | 66.1 |
| Stomach | 569 | 13.3 | 323 | 56.8 |
| Back | 3108 | 72.6 | 1603 | 51.6 |
| Other | 75 | 1.8 | 49 | 65.3 |
| In bed alone | ||||
| Yes | 3689 | 86.5 | 1910 | 51.8 |
| No | 576 | 13.5 | 403 | 70.0 |
Refers to certain types of bedding under the infant (blanket, bean bag, waterbed, rug, sheepskin, cushion, sleeping bag, or pillow) or covering the infant (blanket, quilt/comforter, sheepskin, pillow, or other) while sleeping in last 2 weeks. Covers exclude sheets and blankets not thicker than a receiving blanket.
Demographic and Other Factors Associated With Bedding Use
The prevalence of bedding use over or under the infant and the results of the multivariable analysis for 2007 to 2010 are shown in Table 4. The prevalence exceeded 50% for all groups, except for infants with mothers who had a college education or more (46.4%). Infants of mothers who were teenagers and with less than a high school education had the highest prevalence of bedding use (77.1% and 72.6%, respectively). The strongest independent factors associated with bedding use (aOR: ≥1.5) were maternal age (<20 years, aOR of 2.09 [95% CI: 1.33–3.30] compared with ≥30 years), race and ethnicity (black subjects: aOR of 2.00 [95% CI: 1.53–2.61], Hispanic subjects: aOR of 1.63 [95% CI: 1.24–2.16], and others: aOR of 2.06 [95% CI: 1.53–2.77] compared with white subjects), and education (less than high school: aOR of 2.32 [95% CI: 1.62–3.33], high school or GED: aOR of 1.77 [95% CI: 1.48–2.13], and some college: aOR of 1.53 [95% CI: 1.31–1.80] compared with college or higher).
TABLE 4.
Prevalence and aOR of Factors Associated With the Use of Bedding, NISP Study, 2007 to 2010b
| Characteristic | % Beddinga Use (n = 4280) | Crude OR | aOR (95% CI)c |
|---|---|---|---|
| Mother’s age, y | |||
| <20 | 77.1 | 3.33 | 2.09 (1.33–3.30) |
| 20–29 | 56.7 | 1.30 | 1.14 (0.99–1.31) |
| ≥30 | 50.3 | Ref | Ref |
| Mother’s race and ethnicity | |||
| Other | 66.7 | 1.96 | 2.06 (1.53–2.77) |
| Hispanic | 67.8 | 2.06 | 1.63 (1.24–2.16) |
| Black | 70.9 | 2.38 | 2.00 (1.53–2.61) |
| White | 50.5 | Ref | Ref |
| Mother’s education | |||
| Less than high school | 72.6 | 3.06 | 2.32 (1.62–3.33) |
| High school or GED test | 63.0 | 1.96 | 1.77 (1.48–2.13) |
| Some college | 58.7 | 1.64 | 1.53 (1.31–1.80) |
| College and/or more | 46.4 | Ref | Ref |
| Infant age, wk | |||
| <8 | 59.4 | 1.37 | 1.37 (1.10–1.70) |
| 8–15 | 57.6 | 1.27 | 1.30 (1.13–1.50) |
| ≥16 | 51.8 | Ref | Ref |
| Infant gender | |||
| Female | 55.4 | 1.09 | 1.13 (1.00–1.29) |
| Male | 53.3 | Ref | Ref |
| Preterm birth, <37 wk | |||
| Yes | 54.8 | 1.03 | 1.00 (0.82–1.20) |
| No | 54.2 | Ref | Ref |
| First child | |||
| Yes | 52.7 | Ref | Ref |
| No | 54.6 | 1.08 | 1.16 (1.01–1.33) |
| Geographic region | |||
| West | 63.5 | 1.65 | 1.35 (1.09–1.68) |
| New England | 53.0 | 1.07 | 1.13 (0.84–1.53) |
| Mid-Atlantic | 50.8 | 0.98 | 0.93 (0.75–1.16) |
| South | 54.9 | 1.15 | 1.01 (0.87–1.18) |
| Midwest | 51.3 | Ref | Ref |
| Survey year | |||
| 2010 | 51.7 | 0.96 | 0.93 (0.78–1.12) |
| 2009 | 55.5 | 1.12 | 1.07 (0.89–1.29) |
| 2008 | 57.0 | 1.18 | 1.15 (0.96–1.38) |
| 2007 | 52.8 | Ref | Ref |
GED, General Educational Development.
Refers to certain types of bedding under the infant (blanket, bean bag, waterbed, rug, sheepskin, cushion, sleeping bag, or pillow) or covering the infant (blanket, quilt/comforter, sheepskin, pillow, or other) while sleeping in last 2 weeks. Covers exclude sheets and blankets not thicker than a receiving blanket.
Data include 4280 participants and are adjusted for study year. Population characteristics did not change over time; overall characteristics for this population in 2007–2010 were similar to those presented in Table 1 for the full population 2003–2010.
Adjusted for caregiver age, education, race and ethnicity, parity, geographic region, infant gender, infant age, preterm birth (<37 weeks), and survey year; does not include thin blanket.
Discussion
Despite a substantial decline in reported use of bedding from 1993 to 2010, this potentially hazardous practice remains common, with ∼50% of US caregivers reportedly placing their infants to sleep with some type of bedding. To the best of our knowledge, the prevalence of US infants placed to sleep in environments with bedding has not been previously reported. Depending on sociodemographic characteristics, this practice ranged from 46% to 77% during 2007 to 2010. The lowest prevalence occurred in infants with college-educated mothers and the highest occurred in infants with teen-aged mothers; however, nearly one-half of college-educated mothers put their infants to bed with some type of bedding. Racial and ethnic differences were also observed; infants with black or Hispanic mothers had higher rates than infants with white mothers. Notably, use of bedding was most prevalent among infants in adult beds, while side sleeping, and on shared sleep surfaces. Interestingly, Colson et al,17 by using these same data, reported that 86% of infants who usually shared a bed did so on an adult mattress. Finally, the strongest independent predictors of bedding use were young maternal age, non-white race and ethnicity, and not being college educated.
Reasons for the high prevalence of bedding use, even with recommendations against this potentially hazardous sleep practice dating back to 1996, are unknown. However, caregiver beliefs and perceptions likely play a role. In a small, qualitative study of black parents from Washington, DC, and Maryland,20 perceived infant comfort (warmth and softness) was the most frequently reported reason to use certain types of bedding, regardless of socioeconomic status or educational level. Although some black mothers expressed that blanket use might increase suffocation risk, these same mothers believed that blankets could be used safely if placed away from the infant’s head or neck or if they had breathing holes (eg, crocheted). Another reason that mothers used bedding was to prevent falls from a bed or a sofa by having pillows act as barricades. Media messages targeted toward pregnant women and mothers of infants may also be related to the high prevalence of using certain types of bedding. Joyner et al21 evaluated images from popular magazines targeted to women of childbearing age and found that more than two-thirds of these images showed infants sleeping with potentially hazardous bedding (eg, blankets, pillows). Seeing images such as these may reinforce beliefs and perceptions that having these items in the infant sleep area is not only a favorable practice but also the norm.
It is noteworthy that the rate of decline in bedding use was markedly less from 2001–2010 compared with 1993–2000. This pattern of an early decline followed by a plateau is similar to that observed for sleep position, as well as SIDS rates.17,19 Although we cannot explain why the decline was greater in the earlier period than in the later period, the decline follows 1996 AAP recommendations to avoid potentially hazardous bedding (ie, keep the infant sleep environment free of soft surfaces and gas-trapping objects).14 In 1999 and 2000, several national organizations explicitly stated that pillows, quilts, comforters, sheepskins, and other pillow-like soft products be removed from the crib.15 The lack of further emphasis after 2000 through 2010 may explain differences in the rate of decline during the 2 periods. Interestingly, we also observed a greater decline in bedding use over the infants (quilts/comforters and thick blankets) compared with bedding (blankets) under the infants. This finding raises a concern that parents may incorrectly perceive the recommendations as only pertaining to items covering or around the infant and not include items under the infant.
We found that Hispanic and black infants had a higher prevalence of bedding use compared with white infants. Similar racial and ethnic patterns are noted for other strong risk factors for SIDS, such as prone sleep and bed-sharing.2 Why Hispanic infants have infant mortality rates of SIDS and sleep-related suffocation that are similar to white infants, but not black infants, is unclear. Some possible reasons for differences in mortality are that black mothers, relative to Hispanic mothers, have lower breastfeeding, higher smoking, and higher preterm birth and low birth weight rates, which are all risk factors for SIDS.2,22 Future studies directed at better understanding this inconsistency may provide important clues about new or poorly understood risk factors for SIDS and sleep-related suffocation, especially among black subjects.
Although the present study fills a knowledge gap regarding the US prevalence of and characteristics associated with bedding that is potentially hazardous, there are some limitations. First, generalizability of our findings may be limited due to the overrepresentation of white, higher educated, and older age mothers in the study sample. Second, the declining response rate in the later years may not only limit generalizability but may also result in biased prevalence estimates. Concerns about declining response rates for telephone surveys have increased in recent years.23 As with other surveys with low response rates, our findings, especially in the later years, should be interpreted with caution. Nonetheless, our study did show that the use of bedding in the sleeping environment was high regardless of socioeconomic status (ie, ∼50% even for white, higher educated, and older age mothers). Third, because the measure of bedding use relied on self-report, actual practices may not be reflected; however, it is likely that we have underestimated prevalence. Fourth, our study was limited to questions about nighttime practices, and we do not know if daytime caregivers have different behaviors or practices. Finally, although we were unable to ascertain the specific softness of each bedding item reported, the AAP recommendations2 specifically mention quilts and thick blankets, which are unambiguously soft. Moreover, cushions or waterbeds, which may be of uncertain softness, were relatively few in number and unlikely to change the study conclusions.
Conclusions
This large cross-sectional survey is the only data source currently available to monitor US infant sleep practices at a national level. The use of certain types of bedding in the infant sleep environment is a modifiable risk factor for SIDS and unintentional sleep-related suffocation. To reduce risk, the AAP recommends that soft objects and loose bedding such as pillows and pillow-like toys, quilts, comforters, and sheepskin not be placed in an infant’s sleeping environment.2 However, despite such recommendations, the use of bedding over and under the infant for sleep seems to have remained a common practice. Understanding trends and characteristics associated with bedding use is important for tailoring prevention strategies to reach those at highest risk. Interventions that focus on the safe sleep environment, such as the Safe to Sleep campaign,24 need to be implemented and evaluated to see if they reduce the risks of sleep-related infant deaths.
Acknowledgments
We thank Cheryl L. Robbins, PhD, MS, for review and editing feedback of the manuscript, as well as Timothy Heeren, PhD, for his statistical advice.
Footnotes
Dr Shapiro-Mendoza led the conceptualization and design of the study, analyzed and interpreted the data, drafted the initial manuscript, and revised the manuscript; Drs Colson, Willinger, and Camperlengo conceptualized and designed the study, participated in interpretation of the data, and critically reviewed the manuscript for important intellectual content; Mr Rybin conceptualized and designed the study, analyzed the data, participated in interpretation of the data, and critically reviewed the manuscript for important intellectual content; and Dr Corwin obtained study funding, coordinated and supervised data collection, conceptualized and designed the study, participated in analysis and interpretation of the data, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted.
This work was presented in abstract form at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research (SPER) on June 26, 2012 in Minneapolis, Minnesota and at the International Conference on Stillbirth, SIDS and Infant Survival on October 6, 2012 in Baltimore, Maryland.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Also, the views expressed in this article are those of the authors and do not necessarily reflect the views of the National Institutes of Health or the Eunice Kennedy Shriver National Institute of Child Health and Development.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant U10 HD029067-09A1). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found on page 178, and online at www.pediatrics.org/cgi/doi/10.1542/peds.2014-3218.
References
- 1.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2012 on CDC WONDER Online Database, released October 2014. Data are from the Compressed Mortality File 1999–2012 Series 20 No. 2R, 2014, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Available at: http://wonder.cdc.gov/cmf-icd10.html. Accessed November 3, 2014
- 2.Moon RY, Darnall RA, Goodstein MH, et al. Task Force on Sudden Infant Death Syndrome . SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5). Available at: www.pediatrics.org/cgi/content/full/128/5/e1341 [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome . The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 2005;116(5):1245–1255 [DOI] [PubMed] [Google Scholar]
- 4.Hauck FR, Herman SM, Donovan M, et al. Sleep environment and the risk of sudden infant death syndrome in an urban population: the Chicago Infant Mortality Study. Pediatrics. 2003;111(5 pt 2):1207–1214 [PubMed] [Google Scholar]
- 5.Fu LY, Moon RY, Hauck FR. Bed sharing among black infants and sudden infant death syndrome: interactions with other known risk factors. Acad Pediatr. 2010;10(6):376–382 [DOI] [PubMed] [Google Scholar]
- 6.Schlaud M, Dreier M, Debertin AS, et al. The German case-control scene investigation study on SIDS: epidemiological approach and main results. Int J Legal Med. 2010;124(1):19–26 [DOI] [PubMed] [Google Scholar]
- 7.Brooke H, Gibson A, Tappin D, Brown H. Case-control study of sudden infant death syndrome in Scotland, 1992-5. BMJ. 1997;314(7093):1516–1520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carpenter RG, Irgens LM, Blair PS, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004;363(9404):185–191 [DOI] [PubMed] [Google Scholar]
- 9.Mitchell EA, Scragg L, Clements M. Soft cot mattresses and the sudden infant death syndrome. N Z Med J. 1996;109(1023):206–207 [PubMed] [Google Scholar]
- 10.Mitchell EA, Thompson JM, Ford RP, Taylor BJ, New Zealand Cot Death Study Group . Sheepskin bedding and the sudden infant death syndrome. J Pediatr. 1998;133(5):701–704 [DOI] [PubMed] [Google Scholar]
- 11.Ponsonby AL, Dwyer T, Couper D, Cochrane J. Association between use of a quilt and sudden infant death syndrome: case-control study. BMJ. 1998;316(7126):195–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ponsonby AL, Dwyer T, Gibbons LE, Cochrane JA, Wang YG. Factors potentiating the risk of sudden infant death syndrome associated with the prone position. N Engl J Med. 1993;329(6):377–382 [DOI] [PubMed] [Google Scholar]
- 13.Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Sauerland C, Mitchell EA, GeSID Study Group . Sleep environment risk factors for sudden infant death syndrome: the German Sudden Infant Death Syndrome Study. Pediatrics. 2009;123(4):1162–1170 [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Pediatrics Task Force on Infant Positioning and SIDS . Positioning and sudden infant death syndrome (SIDS): update. Pediatrics. 1996;98(6 pt 1):1216–1218 [PubMed] [Google Scholar]
- 15.US Consumer Product Safety Commission. Recommendations Revised To Prevent Infant Deaths from Soft Bedding (news release #99091). 1999. Available at: www.cpsc.gov/en/Newsroom/News-Releases/1999/Recommendations-Revised-To-Prevent-Infant-Deaths-from-Soft-Bedding/. Accessed November 3, 2014
- 16.American Academy of Pediatrics. Task Force on Infant Sleep Position and Sudden Infant Death Syndrome. Changing concepts of sudden infant death syndrome: implications for infant sleeping environment and sleep position. Pediatrics. 2000;105(3 pt 1):650–656 [DOI] [PubMed] [Google Scholar]
- 17.Colson ER, Willinger M, Rybin D, et al. Trends and factors associated with infant bed sharing, 1993-2010: the National Infant Sleep Position Study. JAMA Pediatr. 2013;167(11):1032–1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Willinger M, Ko CW, Hoffman HJ, Kessler RC, Corwin MJ, National Infant Sleep Position study . Trends in infant bed sharing in the United States, 1993-2000: the National Infant Sleep Position study. Arch Pediatr Adolesc Med. 2003;157(1):43–49 [DOI] [PubMed] [Google Scholar]
- 19.Shapiro-Mendoza CK, Tomashek KM, Anderson RN, Wingo J. Recent national trends in sudden, unexpected infant deaths: more evidence supporting a change in classification or reporting. Am J Epidemiol. 2006;163(8):762–769 [DOI] [PubMed] [Google Scholar]
- 20.Ajao TI, Oden RP, Joyner BL, Moon RY. Decisions of black parents about infant bedding and sleep surfaces: a qualitative study. Pediatrics. 2011;128(3):494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joyner BL, Gill-Bailey C, Moon RY. Infant sleep environments depicted in magazines targeted to women of childbearing age. Pediatrics. 2009;124(3). Available at: www.pediatrics.org/cgi/content/full/124/3/e416 [DOI] [PubMed] [Google Scholar]
- 22.Martin JA, Hamilton BE, Osterman JK, et al. Births: Final Data for 2012. National Vital Statistics Reports. Vol 62, No 9. Hyattsville, MD: National Center for Health Statistics; 2013 [PubMed] [Google Scholar]
- 23.Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17(9):643–653 [DOI] [PubMed] [Google Scholar]
- 24.Safe to Sleep. Public education campaign. Available at: www.nichd.nih.gov/sts/Pages/default.aspx. Accessed January 29, 2014