Abstract
Objective
Smoking is the most important modifiable risk factor for patients with vascular disease. The purpose of this study was to examine smoking cessation rates after vascular procedures and delineate factors predictive of postoperative smoking cessation.
Methods
The Vascular Study Group of New England registry was used to analyze smoking status preoperatively and at 1 year after carotid endarterectomy, carotid artery stenting, lower extremity bypass, and open and endovascular abdominal aortic aneurysm repair between 2003 and 2009. Of 10,734 surviving patients after one of these procedures, 1755 (16%) were lost to follow-up and 1172 (11%) lacked documentation of their smoking status at follow-up. The remaining 7807 patients (73%) were available for analysis. Patient factors independently associated with smoking cessation were determined using multivariate analysis. The relative contribution of patient and procedure factors including treatment center were measured by χ-pie analysis. Variation between treatment centers was further evaluated by calculating expected rates of cessation and by analysis of means. Vascular Study Group of New England surgeons were surveyed regarding their smoking cessation techniques (85% response rate).
Results
At the time of their procedure, 2606 of 7807 patients (33%) were self-reported current smokers. Of these, 1177 (45%) quit within the first year of surgery, with significant variation by procedure type (open abdominal aortic aneurysm repair, 50%; endovascular repair, 49%; lower extremity bypass, 46%; carotid endarterectomy, 43%; carotid artery stenting, 27%). In addition to higher smoking cessation rates with more invasive procedures, age >70 years (odds ratio [OR], 1.90; 95% confidence interval [CI], 1.30-2.76; P< .001) and dialysis dependence (OR, 2.38; 95% CI, 1.04-5.43; P = .04) were independently associated with smoking cessation, whereas hypertension (OR, 1.23; 95% CI, 1.00-1.51; P = .051) demonstrated a trend toward significance. Treatment center was the greatest contributor to smoking cessation, and there was broad variation in smoking cessation rates, from 28% to 62%, between treatment centers. Cessation rates were higher than expected in three centers and significantly lower than expected in two centers. Among survey respondents, 78% offered pharmacologic therapy or referral to a smoking cessation specialist, or both. The smoking cessation rate for patients of these surgeons was 48% compared with 33% in those who did not offer medications or referral (P< .001).
Conclusions
Patients frequently quit smoking after vascular surgery, and multiple patient-related and procedure-related factors contribute to cessation. However, we note significant influence of treatment center on cessation as well as broad variation in cessation rates between treatment centers. This variation indicates an opportunity for vascular surgeons to impact smoking cessation at the time of surgery.
Cigarette smoking is strongly associated with the development of vascular disease, including peripheral arterial disease (PAD)1,2 and abdominal aortic aneurysms (AAAs).3 In addition, smoking is associated with progression of vascular disease, including the expansion4 and rupture of AAA,5 an increased risk of ischemic stroke,6 and graft thrombosis after lower extremity bypass (LEB).7,8 Beyond the long-term benefits in primary and secondary prevention of vascular disease, a systematic review of randomized controlled trials for perioperative smoking cessation interventions demonstrated decreased complication rates after surgery.9 Similar findings were noted in a meta-analysis that demonstrated a 40% relative risk reduction in total complications with preoperative smoking cessation.10
In the United States, the prevalence of cigarette smoking has decreased from 42% in 1965 to 19% in 2010.11 As a result, former smokers have exceeded current smokers since 2002.12 From a population health standpoint, smoking cessation counseling has been demonstrated to be cost-effective,13-14 potentially even more cost-effective than treatment of hypertension and hypercholesterolemia.15
With this in mind, The Joint Commission has developed a Tobacco Cessation Performance Measure as a part of its hospital accreditation process.16 This emphasizes the point that hospitalization for medical or surgical illness can represent an opportunity to encourage smoking cessation and that use of smoking cessation interventions will potentially be tracked in the future as a measure of quality.
The aim of this study was to assess smoking cessation in patients after vascular operations. This included evaluating rates of cessation after surgery and understanding them in the context of patient factors and procedure type as well as evaluating variation in smoking cessation rates by treatment center across New England.
METHODS
Data were obtained from the Vascular Study Group of New England (VSGNE), a regional cooperative developed in 2002 to improve vascular surgery outcomes. Details of this database have been published previously.17 The use of deidentified research data from the VSGNE was approved by the Committee for the Protection of Human Subjects of Dartmouth Medical School. Patients undergoing carotid endarterectomy (CEA), carotid artery stenting (CAS), infrainguinal LEB, endovascular AAA repair (EVAR) and open AAA repair (oAAA) from 2003 to 2009 at 14 treatment centers participating in VSGNE were analyzed.
Treatment center was defined as a single-surgeon group or hospital. For patients in the database undergoing multiple procedures, only the first procedure was analyzed. Smoking status was patient-reported and recorded preoperatively and at the 1-year follow-up. Current smokers (preoperatively defined as having smoked within the past year) were compared with never and prior smokers. Smoking cessation rate at follow-up was calculated, and factors associated with smoking cessation were determined.
A total of 11,519 patients underwent one of the above procedures in the evaluated timeframe. Of these, 217 patients (1.9%) died before hospital discharge and 568 (4.9%) died before their 1-year follow-up assessment. Among the surviving 10,734 patients (93% of all patients), 1755 (16%) were lost to follow-up and 1172 (11%) had 1-year follow-up but did not have documentation of their smoking status at that time. The remaining 7807 patients (73% of the total available for follow-up) had 1-year follow-up with smoking status recorded and comprised the study cohort.
Univariate analysis was performed on this cohort using χ2 analysis for categorical variables and the t test for continuous variables. A subsequent multivariable model was constructed from all preoperative, patient-level variables, including procedure type, using backward stepwise logistic regression. The relative contribution of patient characteristics, procedure type, and treatment center were further evaluated in a multivariable model using the Knaus/Wagner χ-pie method.18 In this analysis, one significant variable is sequentially removed and the model recalculated. The percentage of χ2 uniquely associated with each variable is then calculated. From this one can infer the relative contribution of each variable in the model.
For a detailed examination of variation in cessation rates between treatment center, our multivariable model of independent predictors of smoking cessation was used to calculate expected cessation rates at each institution with >30 data points (n = 10). This was compared with the observed rate by χ2 test. Recognizing that patient-related and procedure-related factors alone would incompletely predict smoking cessation, we concurrently compared smoking cessation rates across centers using analysis of means. This method provides an expected range around the mean of the entire cohort, corrects for sample size, and accounts for factors not present in the multivariable model.
The perspective of VSGNE surgeons about smoking cessation was evaluated with an informal eight-question survey. Questions focused on physicians’ impressions of smoking prevalence and rates of cessation in their patients as well as the methods that they use to promote smoking cessation. Of 54 surgeons sent a survey, 46 (85%) responded. Survey responses were compared with blinded surgeon-specific smoking cessation rates by χ2 analysis. The threshold of statistical significance for all analyses was P < .05.
RESULTS
Among the 7807 patients with known smoking status at the time of follow-up, the vascular operations performed were distributed as 12.8% oAAA repair (n = 999), 11.3% EVAR (n = 881), 21.6% LEB (n = 1684), 52.1% CEA (n = 4066), and 2.3% CAS (n = 177). Of these patients, 2606 (33%) were current smokers, 3881 (50%) were former smokers, and 1320 (17%) were never smokers. By type of procedure, the rates of current smoking were 41% for oAAA, 30% for EVAR, 41% for LEB, 29% for CEA, and 32% for CAS. The univariate analysis of patient characteristics is listed in Table I for smokers, never smokers, and former smokers. Current smokers tended to be younger than never or prior smokers. Although they were more likely to have undergone a previous percutaneous peripheral intervention, they were less likely to have undergone a coronary procedure. Current smokers were more likely to have chronic obstructive pulmonary disease (COPD) but less likely to have diabetes or hypertension. Further, current smokers were more likely to undergo a LEB or oAAA, were more likely to have longer hospital length of stay (LOS), and were more likely to require postoperative admission to the intensive care unit.
Table I.
Univariate analysis of smokers, never smokers, and prior smokers at the time of surgery
| Variable | Smoking status
|
P | ||
|---|---|---|---|---|
| Current, %
|
Never, %
|
Prior, %
|
||
| (n = 2060) | (n = 1320) | (n = 3881) | ||
| Total | 33 | 17 | 50 | |
| Male | 65 | 54 | 71 | <.001 |
| Age, yearsa | <.001 | |||
| <50 | 6 | 1 | 1 | |
| 50-59 | 22 | 7 | 8 | |
| 60-69 | 39 | 21 | 28 | |
| ≥70 | 33 | 72 | 63 | |
| Previous cardiovascular procedure | ||||
| LEB, CEA, AAA | 17 | 12 | 17 | <.001 |
| CABG/PCI | 23 | 30 | 36 | <.001 |
| Comorbidity | ||||
| Diabetes | 26 | 35 | 33 | <.001 |
| Hypertension | 81 | 86 | 87 | <.001 |
| Dialysis dependent | 1 | 2 | 1 | .004 |
| COPD | 40 | 9 | 24 | <.001 |
| Living at home preadmission | 99 | 98 | 99 | .21 |
| Procedure type | <.001 | |||
| AAA repair | ||||
| Open | 41 | 9 | 50 | |
| Endovascular | 30 | 12 | 58 | |
| LEB | 41 | 15 | 44 | |
| CEA | 29 | 21 | 50 | |
| CAS | 32 | 16 | 52 | |
| Perioperative | ||||
| Urgent or emergent procedure | 13 | 12 | 11 | .044 |
| Length of stay >2 days | 42 | 32 | 37 | <.001 |
| Intensive care unit stay | 45 | 32 | 37 | <.001 |
| Discharge destinationa | <.001 | |||
| Home | 92 | 87 | 90 | |
| Rehabilitation unit | 6 | 8 | 6 | |
| Nursing home | 3 | 5 | 4 | |
AAA, Abdominal aortic aneurysm; CABG, coronary artery bypass grafting; CAS, carotid artery stenting; CEA, carotid endarterectomy; COPD, chronic obstructive pulmonary disease; LEB, lower-extremity bypass; PCI, percutaneous coronary intervention.
Column percent. Values have been rounded and may not sum to 100%.
Patients lost to follow-up
Comparison of the 2927 patients without follow-up smoking status with the 7807 patients with follow-up smoking status demonstrated no difference between these two groups in prevalence of smoking, sex, and age, or in rates of diabetes, hypertension, or COPD. Patients without follow-up were slightly more likely to have dialysis-dependent renal failure (1% vs 2%; P = .002) or to have undergone a previous vascular procedure (18% vs 16%; P= .004).
Patient and procedure factors associated with smoking cessation
The 2606 currently smoking patients were followed up at a mean interval of 12 ± 5.9 (standard deviation) months. Of these, 1177 (45%) reported smoking cessation by the time of follow-up. The patients who quit smoking are compared in Table II with those who continued smoking. Smoking cessation was associated with multiple patient-related and procedure-related factors. In particular, there was significant variability in smoking cessation rates depending on patient age, comorbidity (hypertension, diabetes, COPD), and procedure. The procedure-specific variability in cessation rate is shown in Fig 1. Smoking cessation was also associated with LOS >2 days and discharge to a rehabilitation center or nursing home.
Table II.
Univariate analysis of patients who quit compared with patients who continued to smoke at 1 year after surgery
| Variable | Smoking status
|
P | |
|---|---|---|---|
| Quit, %
|
Continued, %
|
||
| (n = 1429) | (n = 1177) | ||
| Total | 45 | 55 | |
| Male | 67 | 65 | .33 |
| Age, yearsa | <.001 | ||
| <50 | 5 | 7 | |
| 50-59 | 20 | 24 | |
| 60-69 | 38 | 40 | |
| ≥70 | 38 | 30 | |
| Previous cardiovascular procedure | |||
| LEB, CEA, AAA | 15 | 18 | .085 |
| CABG/PCI | 24 | 23 | .674 |
| Comorbidity | |||
| Diabetes | 26 | 25 | .692 |
| Hypertension | 83 | 80 | .026 |
| Dialysis dependent | 1.4 | 0.6 | .038 |
| COPD | 38 | 42 | .021 |
| Living at home preadmission | 99 | 99 | .122 |
| Procedure type | .003 | ||
| AAA repair | |||
| Open | 50 | 50 | |
| Endovascular | 49 | 51 | |
| LEB | 46 | 54 | |
| CEA | 43 | 57 | |
| CAS | 27 | 73 | |
| Perioperative | |||
| Urgent or emergent procedure | 13 | 12 | .319 |
| Length of stay >2 days | 45 | 38 | <.001 |
| Intensive care unit stay | 45 | 45 | .96 |
| Discharge destinationa | <.001 | ||
| Home | 89 | 94 | |
| Rehabilitation unit | 7 | 4 | |
| Nursing home | 3 | 2 | |
AAA, Abdominal aortic aneurysm; CABG, coronary artery bypass grafting; CAS, carotid artery stenting; CEA, carotid endarterectomy; COPD, chronic obstructive pulmonary disease; LEB, lower-extremity bypass; PCI, percutaneous coronary intervention.
Column percent. Values have been rounded and may not sum to 100%.
Fig 1.
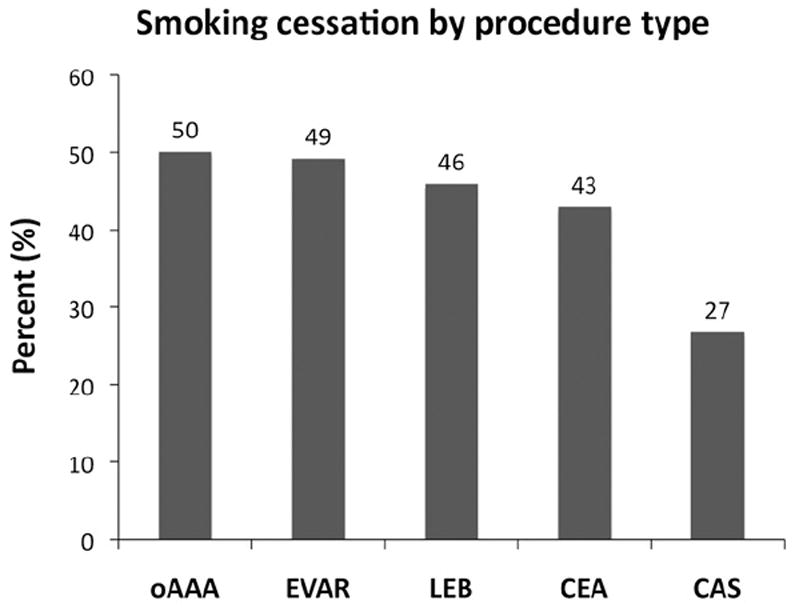
Rates of smoking cessation shown by procedure type (P = .003). CAS, Carotid artery stenting; CEA, carotid endarterectomy; EVAR, endovascular aneurysm repair; LEB, lower extremity bypass; oAAA, open abdominal aortic aneurysm.
Multivariate analysis of patient characteristics demonstrated that patients were more likely to quit smoking if they had hypertension, dialysis-dependent renal failure, or were aged >70 years. In contrast, patients who had COPD were less likely to quit smoking (Table III). Consistent with smoking cessation rates by procedure type, patients undergoing oAAA repair had a significantly higher likelihood of smoking cessation at 1 year, and patients undergoing EVAR or LEB had a strong trend toward increased smoking cessation. In contrast, patients undergoing CAS were less likely to quit smoking after their procedure. The area under the receiver operating characteristic curve for this logistic model was 0.58, demonstrating that smoking cessation can only partially be explained by patient characteristics or procedure type.
Table III.
Multivariate analysis of patient factors and procedure type associated with smoking cessationa
| Variable | OR (95% CI) | P |
|---|---|---|
| Age, years | ||
| <50 | Reference | |
| 50-59 | 1.20 (0.82-1.75) | .356 |
| 60-69 | 1.42 (0.98-2.05) | .065 |
| ≥70 | 1.90 (1.30-2.76) | <.001 |
| Comorbidity | ||
| Dialysis | 2.38 (1.04-5.43) | .040 |
| Hypertension | 1.23 (1.00-1.51) | .051 |
| COPD | 0.76 (0.65-0.90) | .001 |
| Procedure type | ||
| Carotid endarterectomy | Reference | |
| AAA repair | ||
| Open | 1.30 (1.03-1.63) | .027 |
| Endovascular | 1.23 (0.94-1.62) | .136 |
| Lower-extremity bypass | 1.19 (0.98-1.44) | .086 |
| Carotid artery stenting | 0.50 (0.27-0.92) | .025 |
AAA, Abdominal aortic aneurysm; CI, confidence interval; COPD, chronic obstructive pulmonary disease; OR, odds ratio.
Area under the curve = 0.58.
Variation in cessation rates by treatment center
We considered the contribution of the treatment center to better understand the significance of processes of care in smoking cessation. The χ-pie analysis of a multivariable model that includes treatment center demonstrated that of the significant variables within the model, 75% of the variation in cessation rates could be attributed to the treatment center and only 25% to patient factors (Fig 2).
Fig 2.
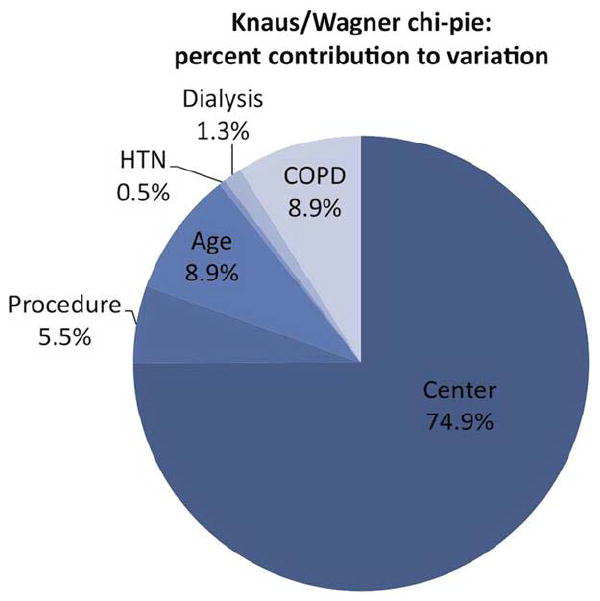
The relative contribution of factors included in the multi-variable model to explain the variation in rates of smoking cessation. The treatment center explains nearly 75% of the variation within the model, whereas patient factors and procedure type explain the remaining portion of the variation in the model. COPD, Chronic obstructive pulmonary disease; HTN, hypertension.
Observed smoking cessation rates varied significantly between centers, from 28% to 62%, whereas the expected rates of smoking cessation based on patient characteristics and procedure type showed little variation among centers (43% to 47%). Supporting this comparison with analysis of means, which provides an expected range around the mean, demonstrated cessation rates that were significantly below expected for two centers (centers 1 and 2) and were above expected for three centers (centers 7, 9, and 10; Fig 3).
Fig 3.
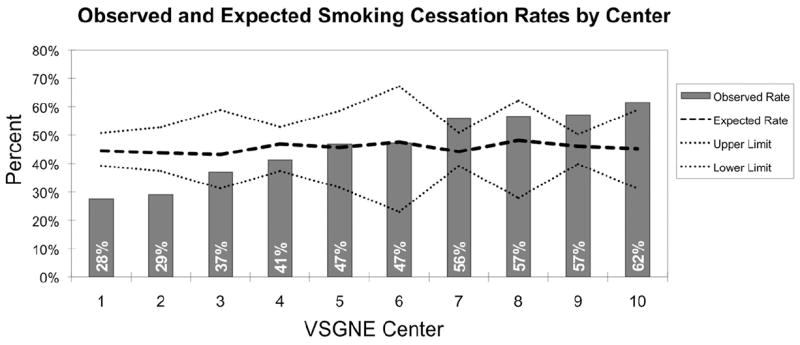
Treatment center level comparisons are shown using observed/expected and analysis of means. The treatment center number is arbitrarily assigned in this graph. P < .05 for values outside of upper and lower limits. VSGNE, Vascular Study Group of New England.
Our provider survey further explored surgeon-specific variation in cessation rates. In the survey, 82% of surgeons estimated that more than half of their patients were current smokers, in contrast with a 33% smoking prevalence in the study cohort. When asked about postoperative smoking cessation, half of respondents estimated a cessation rage of <25% compared with the actual cessation rate of 45%. All respondents reported that they discussed smoking cessation with their patients during one or more clinical encounters in the perioperative period.
There was broad variation in cessation interventions the surgeons offered to patients: 15% offered referral to a smoking cessation specialist, 33% offered pharmacotherapy, 30% offered a combination of referral and pharmacotherapy, and 22% left all smoking cessation treatment to the primary care provider. A univariate comparison using these survey responses demonstrated significantly higher cessation rates for patients offered pharmacotherapy or referral to a specialist than for patients sent back to their primary care provider for smoking cessation treatment (48% vs 33%; P < .004).
DISCUSSION
Cigarette and tobacco smoking is a complex public health problem with significant implications for the secondary prevention of cardiovascular disease. Although the population prevalence of smoking has decreased in the last 45 years, the cessation rate (defined as 6-months abstinence from tobacco) was estimated to be only ~6% in 2010.19 In this study, we demonstrate a smoking cessation rate of 45% within 1 year of patients undergoing vascular surgery, markedly exceeding the estimated cessation rate for the population. Importantly, this cessation rate occurs in the context of a 33% smoking prevalence among patients in our cohort, which exceeds the estimated population prevalence of 19%. Although this is the first such report in vascular surgery patients, the 1-year cessation rate is consistent with rates observed in studies of other surgery patients. Two observational studies of cardiac surgery patients demonstrated smoking cessation rates of 50% and 55% at 1 year.20,21 In a randomized trial, smoking cessation before general or orthopedic procedures resulted in a 40% smoking cessation rate.22
Our analysis has delineated multiple factors associated with perioperative smoking cessation. Of these, the two most important are (1) that more invasive procedures tend to have higher cessation rates and (2) that for multiple reasons, there is a significant variation in cessation rates between treatment centers. The effect of procedure invasiveness is seen in raw cessation rates by procedure as well as in multivariate analysis, where more invasive procedures—oAAA in particular—have higher odds ratios for smoking cessation. Not surprisingly, the strong covariates of procedure invasiveness, LOS, and discharge destination were also significant on univariate analysis.
This relationship between procedure invasiveness and smoking cessation was also demonstrated in study of patients treated for coronary artery disease, where a higher rate of smoking cessation was shown after CABG (55%) than after a percutaneous coronary intervention (25%) and angiography alone (14%) at 1 year.20 Another study found that patients undergoing major surgery had a higher likelihood of smoking cessation than those undergoing an outpatient procedure (odds ratio, 2.02 vs 1.28).23 Indeed, a number of studies have shown a higher rate of smoking cessation with counseling around the time of a hospital admission or surgical intervention, highlighting what has been described as a “teachable moment.”23,24
The broad variation in cessation rates across treatment centers is the second key point of our analysis. The low area under the curve in our multivariable analysis of patient factors and procedure type clearly indicates that diverse factors are associated with smoking cessation that are not explained by our model. Indeed, subsequent analysis demonstrated that 75% of the variation in cessation rate could be attributed to the treatment center, far more significant than patient factors or procedure type. This is further demonstrated in looking at treatment centers individually and noting cessation rates in two centers that were lower than predicted, which strongly contrasts with the high cessation rates in other centers. Although direct comparison of this finding to physician practices is not possible, the provider survey does offer some additional insight into these observations. In particular, it appears that that surgeons offering more aggressive smoking cessation interventions, such as referral to a specialist or offering pharmacotherapy or both, are more likely to have patients that quit smoking.
Unfortunately, the survey also suggests that many surgeons think the problem is more daunting than it is in the way that respondents overestimated the smoking prevalence in the population. Further, underestimating the rate of perioperative smoking cessation suggests that many surgeons misjudge the effect they can have on smoking cessation for their patients.
Although there are no studies from prospectively collected data regarding smoking cessation in the vascular surgical population, a study of medical patients with PAD found treatment with intensive counseling and medication resulted in a cessation rate of 21.3% at 6 months compared with a cessation rate of 6.8% in a minimal intervention group.25 A study in medical patients demonstrated a higher likelihood of receiving and perhaps recalling smoking cessation counseling after a major medical illness.26
The regional variation in cessation rates and the importance of the physician and treatment center in smoking cessation are particularly important when considered in the context of the additional significant elements in our multi-variable model. In particular, patients aged >70 years and patients with additional comorbidities of hypertension and dialysis-dependence were more likely to quit smoking. The one contrast to this assessment is that having COPD appears to decrease the odds of smoking cessation. Although this particular finding is not well delineated by the available data, it may reflect a patient cohort refractory to cessation interventions; that is, patients with a diagnosis of COPD who were able to quit smoking would already have done so upon diagnosis of their pulmonary disease. However, in total, our analysis suggests that in younger patients with fewer comorbidities—the patients who have the greatest potential to benefit from smoking cessation—are the patients least likely to quit. This represents a high-impact opportunity for targeted secondary prevention.
This study has several important limitations, the most important of which is that smoking cessation in this data set is self-reported by the patient and no confirmatory biochemical testing was performed. This method of data collection can lead to patient under-reporting of current smoking. However, there are four particular factors that support the validity of this methodology in this study:
First, a high sensitivity of patient-reported smoking status was demonstrated by a meta-analysis of studies examining smoking status and by a large population-based study of smoking.27,28
Second, because the data are collected as part of a clinical encounter, they are likely less susceptible to the potential dishonesty that is noted to be more likely in survey-based studies.27
Third, collection of data from a clinical encounter also provides additional clinical relevance to the clinical practice of vascular surgery, particularly when considering that a performance measure similar to the one being implemented by The Joint Commission would be based on patient-reported data.16
Fourth, the perceived gold standard of biochemical testing has been questioned in the literature because there is a significant portion of false-negative reports, likely due to the insensitivity of the most widely available assay methods.28 Importantly, even if smoking status were underestimated in this cohort, there are no data to suggest a systematic bias that would invalidate the relative changes and effects of different operations and centers.
The second study limitation is the lack of follow-up data regarding smoking status in 27% of the patients. The likelihood of this introducing a bias within the entire cohort is limited by the lack of disparity in the patient level data between those who did and did not have follow-up. However, there is potential for introduction of bias at the center level, and we did note a degree of inverse correlation between centers that had higher follow-up among current smokers and lower cessation rates (r = −0.57; P = .087). This limitation has three potential components: (1) decreased reporting of continued smoking by patients at follow-up, (2) decreased follow-up by patients who continue smoking, or (3) decreased reporting by physicians and centers for patients who continue smoking. Each component is relevant for future quality improvement within our regional study group. However, the significant influence of center in our analysis of smoking cessation and the broad variation in cessation rates by center are very unlikely to be abrogated by more uniform follow-up in our cohort.
The final study limitation is the lack of external validation of our provider survey before administration. The survey had excellent response rates, but the lack of validation limited our ability to standardize the responses using the full multivariable model. However, none of these limitations diminish the key findings from this data.
CONCLUSIONS
Our study shows that the magnitude of vascular surgical reconstruction is directly related to the chance that the patient will stop smoking. Of greater significance, however, is the broad variation in smoking cessation rates between centers participating in the VSGNE. This analysis suggests that center-specific strategies are important determinants of success or failure in getting patients to quit smoking. The need for greater attention to smoking and, by extension, smoking cessation at the center level is further highlighted by the variable follow-up observed among smokers at each center. Using the framework built by our regional quality collaborative, our future work will identify how those centers and surgeons with both high follow-up rates and high smoking cessation rates accomplish this task. This will facilitate expansion of these techniques to all centers in our region.
Footnotes
AUTHOR CONTRIBUTIONS
Conception and design: AH, BN, PG, JC
Analysis and interpretation: AH, BN, PG, YZ, AS, JC
Data collection: BN, PG, AS, ACS, JE, JC
Writing the article: AH, JC
Critical revision of the article: AH, BN,PG, A S, JC
Final approval of the article: AH, BN, PG, YZ, AS, ACS, JE, JC
Statistical analysis: AH, BN, YZ
Obtained funding: Not applicable
Overall responsibility: AH
Author conflict of interest: none.
Presented at the Thirty-sixth Annual Meeting of the Midwestern Vascular Surgical Society, Milwaukee, Wise, September 6-8, 2012.
Additional material for this article may be found online at www.jvascsurg.org.
References
- 1.Meijer WT, Grobbee DE, Hunink MG, Hofman A, Hoes AW. Determinants of peripheral arterial disease in the elderly: the Rotterdam study. Arch Intern Med. 2000;160:2934–8. doi: 10.1001/archinte.160.19.2934. [DOI] [PubMed] [Google Scholar]
- 2.Murabito JM, Evans JC, Nieto K, Larson MG, Levy D, Wilson PW. Prevalence and clinical correlates of peripheral arterial disease in the Framingham Offspring Study. Am Heart J. 2002;143:961–5. doi: 10.1067/mhj.2002.122871. [DOI] [PubMed] [Google Scholar]
- 3.Lee AJ, Fowkes FG, Carson MN, Leng GC, Allan PL. Smoking, atherosclerosis and risk ofabdominal aortic aneurysm. Eur Heart J. 1997;18:671–6. doi: 10.1093/oxfordjournals.eurheartj.a015314. [DOI] [PubMed] [Google Scholar]
- 4.Brady AR, Thompson SG, Fowkes FG, Greenhalgh RM, Powell JT. Abdominal aortic aneurysm expansion: risk factors and time intervals for surveillance. Circulation. 2004;110:16–21. doi: 10.1161/01.CIR.0000133279.07468.9F. [DOI] [PubMed] [Google Scholar]
- 5.Strachan DP. Predictors of death from aortic aneurysm among middle-aged men: the Whitehall study. Br J Surg. 1991;78:401–4. doi: 10.1002/bjs.1800780407. [DOI] [PubMed] [Google Scholar]
- 6.Shinton R, Beevers G. Meta-analysis of relation between cigarette smoking and stroke. BMJ. 1989;298:789–94. doi: 10.1136/bmj.298.6676.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ameli FM, Stein M, Provan JL, Prosser R. The effect of postoperative smoking on femoropopliteal bypass grafts. Ann Vase Surg. 1989;3:20–5. doi: 10.1016/S0890-5096(06)62380-7. [DOI] [PubMed] [Google Scholar]
- 8.Wiseman S, Kenchington G, Dain R, Marshall CE, McCollum CN, Greenhalgh RM, et al. Influence of smoking and plasma factors on patency of femoropopliteal vein grafts. BMJ. 1989;299:643–6. doi: 10.1136/bmj.299.6700.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomsen T, Tonnesen H, Moller AM. Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. Br J Surg. 2009;96:451–61. doi: 10.1002/bjs.6591. [DOI] [PubMed] [Google Scholar]
- 10.Mills E, Eyawo O, Lockhart I, Kelly S, Wu P, Ebbert JO. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med. 2011;124:144–54.el48. doi: 10.1016/j.amjmed.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Smoking and tobacco use: trends in current cigarette smoking among high school students and adults, United States, 1965–2010. [March 25,2012];2011 Available at: http://www.cdcgov/tobacco/data_statistics/tables/trends/cig_smoking/index.htm.
- 12.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults–United States, 2002. MMWR Morb Mortal Wkly Rep. 2004;53:427–31. [PubMed] [Google Scholar]
- 13.Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA. 1997;278:1759–66. [PubMed] [Google Scholar]
- 14.Oster G, Huse DM, Delea TE, Colditz GA. Cost-effectiveness of nicotine gum as an adjunct to physician’s advice against cigarette smoking. JAMA. 1986;256:1315–8. [PubMed] [Google Scholar]
- 15.Cummings SR, Rubin SM, Oster G. The cost-effectiveness of counseling smokers to quit. JAMA. 1989;261:75–9. [PubMed] [Google Scholar]
- 16.Fiore MC, Goplerud E, Schroeder SA. The Joint Commission’s new tobacco-cessation measures–will hospitals do the right thing? N Engl J Med. 2012;366:1172–4. doi: 10.1056/NEJMp1115176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cronenwett JL, Likosky DS, Russell MT, Eldrap-Jorgensen J, Stanley AC, Nolan BW. A regional registry for quality assurance and improvement: the Vascular Study Group of Northern New England (VSGNNE) J Vase Surg. 2007;46:1093–101. doi: 10.1016/j.jvs.2007.08.012. discussion: 1101-2. [DOI] [PubMed] [Google Scholar]
- 18.Knaus WA, Wagner DP, Zimmerman JE, Draper EA. Variations in mortality and length of stay in intensive care units. Ann Intern Med. 1993;118:753–61. doi: 10.7326/0003-4819-118-10-199305150-00001. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) Quitting smoking among adults—United States, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60:1513–9. [PubMed] [Google Scholar]
- 20.Crouse JR, 3rd, Hagaman AP. Smoking cessation in relation to cardiac procedures. Am J Epidemiol. 1991;134:699–703. doi: 10.1093/oxfordjournals.aje.a116146. [DOI] [PubMed] [Google Scholar]
- 21.Gjeilo KH, Stenseth R, Klepstad P, Lydersen S, Wahba A. Patterns of smoking behaviour in patients following cardiac surgery. A prospective study. Scand Cardiovasc J. 2010;44:295–300. doi: 10.3109/14017431.2010.500395. [DOI] [PubMed] [Google Scholar]
- 22.Lindstrom D, Sadr Azodi O, Wladis A, Tonnesen H, Under S, Nasell H, et al. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg. 2008;48:739–45. doi: 10.1097/SLA.0b013e3181889d0d. [DOI] [PubMed] [Google Scholar]
- 23.Shi Y, Warner DO. Surgery as a teachable moment for smoking cessation. Anesthesiology. 2010;112:102–7. doi: 10.1097/ALN.0b013e3181c61cf9. [DOI] [PubMed] [Google Scholar]
- 24.van Domburg RT, Meeter K, van Berkel DF, Veldkamp RF, van Herwerden LA, Bogers AJ. Smoking cessation reduces mortality after coronary artery bypass surgery: A 20-year follow-up study. J Am Coll Cardiol. 2000;36:878–83. doi: 10.1016/s0735-1097(00)00810-x. [DOI] [PubMed] [Google Scholar]
- 25.Hennrikus D, Joseph AM, Lando HA, Duval S, Ukestad L, Kodl M, et al. Effectiveness of a smoking cessation program for peripheral artery disease patients: a randomized controlled trial. J Am Coll Cardiol. 2010;56:2105–12. doi: 10.1016/j.jacc.2010.07.031. [DOI] [PubMed] [Google Scholar]
- 26.Anda RF, Remington PL, Sienko DG, Davis RM. Are physicians advising smokers to quit? The patient’s perspective. JAMA. 1987;257:1916–9. [PubMed] [Google Scholar]
- 27.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84:1086–93. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Caraballo RS, Giovino GA, Pechacek TF, Mowery PD. Factors associated with discrepancies between self-reports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2001;153:807–14. doi: 10.1093/aje/153.8.807. [DOI] [PubMed] [Google Scholar]


