Abstract
Objective:
The authors evaluate the anatomic subtleties of lumbar facets and assess the feasibility and effectiveness of use of ‘Goel facet spacer’ in the treatment of degenerative spinal canal stenosis.
Materials and Methods:
Twenty-five lumbar vertebral cadaveric dried bones were used for the purpose. A number of morphometric parameters were evaluated both before and after the introduction of Goel facet spacers within the confines of the facet joint.
Results:
The spacers achieved distraction of facets that was more pronounced in the vertical perspective. Introduction of spacers on both sides resulted in an increase in the intervertebral foraminal height and a circumferential increase in the spinal canal dimensions. Additionally, there was an increase in the disc space or intervertebral body height. The lumbar facets are more vertically and anteroposteriorly oriented when compared to cervical facets that are obliquely and transversely oriented.
Conclusions:
Understanding the anatomical peculiarities of the lumbar and cervical facets can lead to an optimum utilization of the potential of Goel facet distraction arthrodesis technique in the treatment of spinal degenerative canal stenosis.
Keywords: Distraction, Goel intraarticular spacer, lumbar degenerative disease, lumbar facets
INTRODUCTION
Multiple techniques have been described to treat lumbar spinal spondylosis-related neural foraminal and spinal canal stenosis using various approaches, with or without spinal fixation. The ease, safety, and biomechanical strength of pedicle screws have revolutionized the spinal stabilization techniques of the entire spine in general and lumbar spine in particular. Despite the popularity of pedicle screws, alternative methods of spinal stabilization have been explored. The strength of bone material of facets appears to be underutilized for spinal fixation. Interfacetal and transfacetal screws have been used, but have not gained their rightful status. Intraarticular spacer distraction and stabilization technique has recently been described by Goel et al. Jamming of the only true joint of the spine and blocking the movements at the fulcrum provides biomechanical superiority to the procedure.
There have been only a few studies which have dealt with the anatomy of the facet joints either using cadaveric vertebrae or radiological imaging. The authors evaluate the morphometric issues related to the lumbar facets and articular cavity and evaluate the feasibility of introduction of ‘Goel facet spacer’ within the articular cavity. The effects of these spacers on a number of spinal dimensions, particularly as it relates to spinal root and dural canal dimensions are evaluated. Moreover, in order to successfully execute the Goel facet distraction-arthrodesis technique, a detailed knowledge of the anatomy of the lumbar vertebral facet joints is essential.
MATERIALS AND METHODS
Twenty-five dried cadaveric lumbar vertebrae (five sets of lumbar vertebrae L1-5) were procured from the Department of Anatomy and a number of morphological parameters were evaluated. Both junior authors independently measured all the parameters to minimize errors.
Facetal height was measured as the maximum superoinferior extent of the facetal surface. The width of the facet was estimated as the maximum lateral diameter of the facetal surface, and the thickness was calculated by measuring the maximum anteroposterior dimension of the facet. Interspinous distance was measured as the distance between the inferior origin of the spinous process of each vertebra and the superior origin of the spinous process of the successive vertebra below it when stacked vertically in order from L1 to L5. Intervertebral foramen height was also measured for each pair of vertebrae as the maximum vertical distance between the pedicles of successive vertebrae. The measurements for interspinous distance and intervertebral foramen height were repeated after insertion of Goel intraarticular facetal spacers.
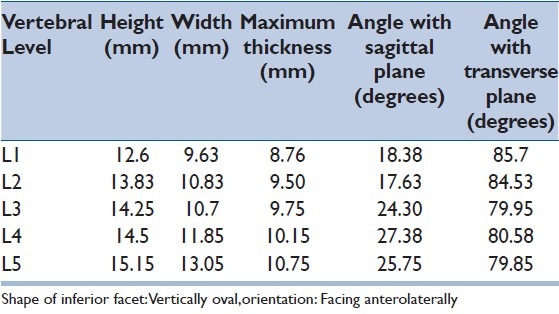
Additionally, the orientation of the vertebral facets was studied. The angles were measured with the vertebra held as in the human standing position. The angles of the facet with the transverse and sagittal planes were measured. The angle formed by the facet with the transverse plane was measured between a line running through the posterior margin of the respective articular process and a horizontal line drawn touching the inferior margin of the facet in the transverse plane. The angle formed by the facet with the sagittal plane was measured as the angle between a line running across the superior margin of the articular process and a line drawn in the sagittal plane through the middle of the vertebral body and the spinous process.
RESULTS
Superior articular facets (Figures 1, 3 and 5)
Figure 1.
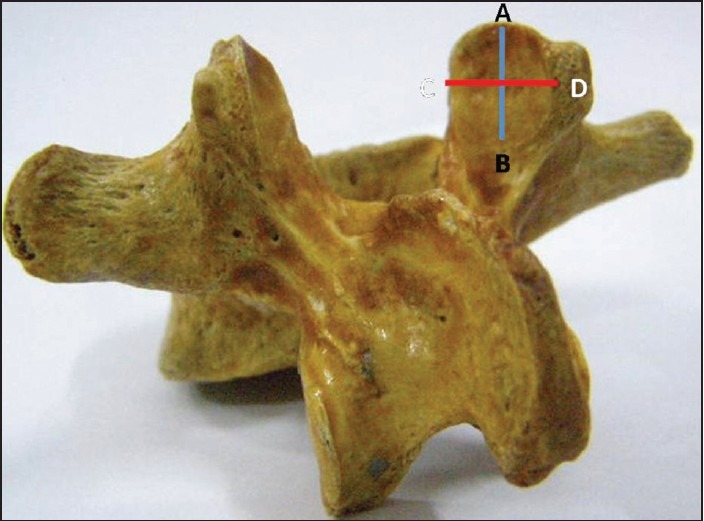
Posterior view of the lumbar vertebra showing the superior articular facets. Line AB denotes the height of the superior articular facet and line CD denotes the width
Figure 3.
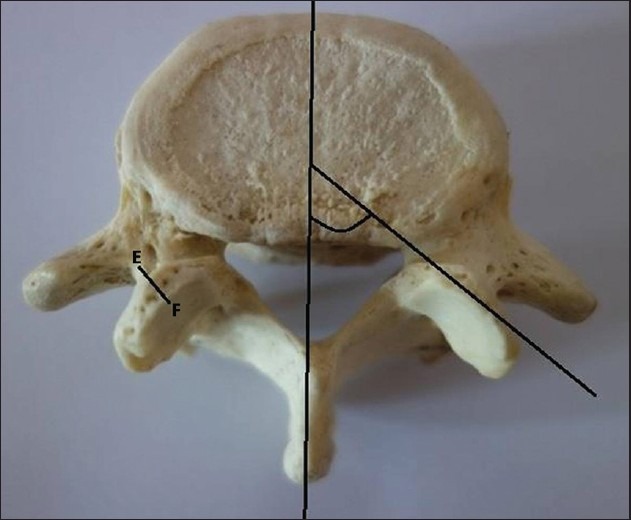
Superior view of the lumbar vertebra showing the thickness (line EF) of the facet and angle with sagittal plane (right) of the superior articular facet
Figure 5.
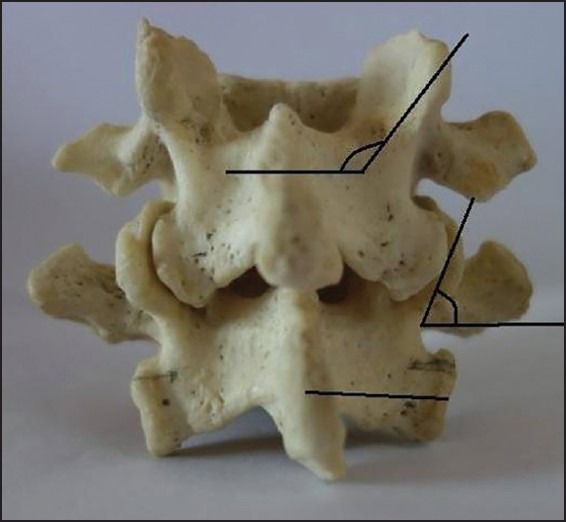
Measured angle with transverse plane formed by superior (upper angle) and inferior (lower angle) articular facets
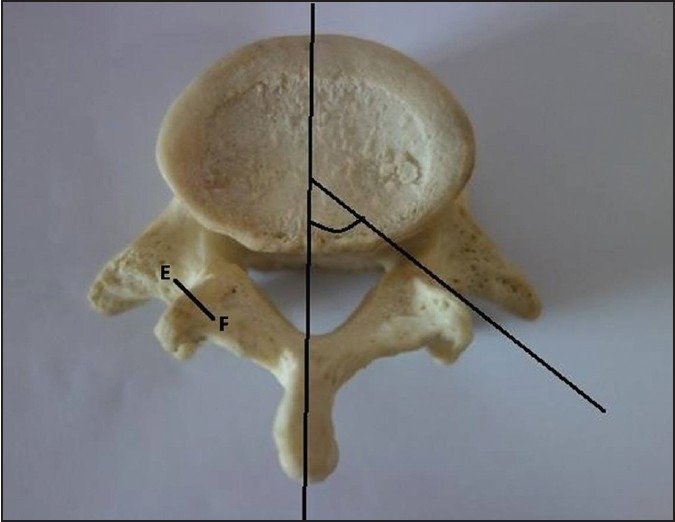
The facetal height varied between 11.63 and 14.78 mm. It was seen to increase from L1 to L5. It was maximum at L5, that is, 14.78 and minimum at L1, that is, 11.63 with the most abrupt increase being between L1 and L2. The width varied between 10.33 and 13.95 mm. It increased between L1 and L5. L5 had the maximum width of 13.95 mm, and L1, the minimum width of 10.33 mm. The most abrupt increase was between L1 (10.33 mm) and L2 (11.95 mm). Thickness of the facets varied from 7.83 to 8.85 and was noted to increase from L1 to L4 and was the maximum at L4. The maximum thickness measured was 8.85 mm at L4 and the minimum was 7.83 mm at L1.
The angle of the facets with the sagittal plane (α) was found to vary between 17.95 and 37.73 degrees. The angle of the facets with the transverse plane (β) was found to vary between 93.48 and 102.93 degrees. It was found to increase from L1 to L5. It was greatest at L5 and least at L1. The greatest difference in the angle β of the facets of two successive vertebrae was at L4-5. The least difference was at L3-4.
Inferior articular facets (Figures 2, 4 and 5)
Figure 2.
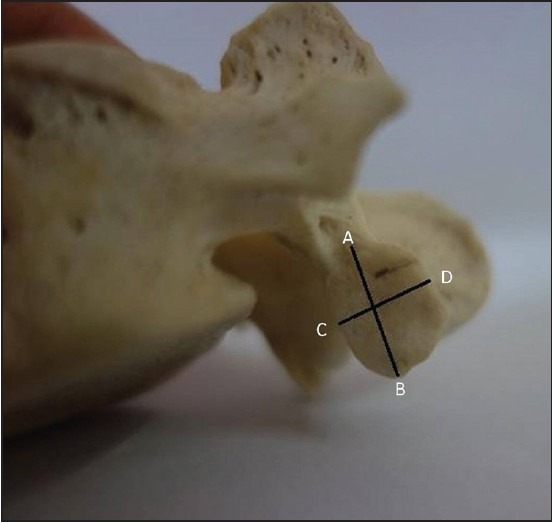
Posterior view of the lumbar vertebra showing the inferior articular facets. Line AB denotes the height of the inferior articular facet and line CD denotes the width
Figure 4.
Inferior view of the lumbar vertebra showing the thickness (line EF) of the facet and angle formed with sagittal plane (right) of the inferior articular facet
The facetal height varied between 12.6 and 15.15 mm. It was noted to increase from L1 to L5. It was maximum at L5, that is, 15.15 mm and minimum at L1, that is, 12.6 mm with the most abrupt increase being between L1 and L2 and the least between L3 and L4. The width varied between 9.63 and 13.05 mm. It increased between L1 and L5. L5 had the maximum width of 13.05 mm, and L1 had a minimum width of 9.63 mm. The most abrupt increase was between L1 and L2, and L4 and L5 (both 1.20 mm). Thickness of the facets varied from 8.76 to 10.75 mm and was noted to increase from L1 to L4 and was the maximum at L4. The maximum increase was at L1-2 and the least at L2-3.
The angle of the facets with the sagittal plane (α) was found to vary between 17.63 and 27.38 degrees. It was found to increase from L1 to L5. It was greatest at L5 and least at L2. The greatest difference in the angle α of the facets of two successive vertebrae was at L2-3. The least difference was at L1-2. The angle of the facets with the transverse plane (β) was found to be in a narrow range between 85.7 and 79.85°. It was greatest at L1 and least at L5. The greatest difference in the angle β of the facets of two successive vertebrae was at L2-3. The least difference was at L3-4.
The details of our findings have been presented in Tables 1 and 2.
Table 1.
Measurements of superior articular facets of lumbar vertebrae
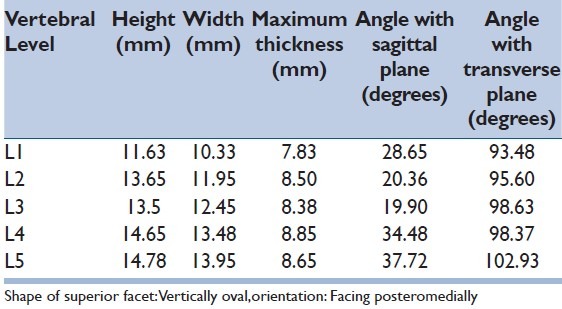
Table 2.
Measurements of inferior articular facets of lumbar vertebrae
Comparison with cervical vertebrae
As compared to the cervical facets, the lumbar facets were noted to have certain differences. The superior facetal height was 7-12 mm for the cervical vertebrae as against 11.6-14.8 mm for the lumbar vertebrae. The width was 7.5-12.0 mm for the cervical vertebrae as compared to 10.3-13.9mm for the lumbar vertebrae and the thickness ranged from 3.5 to 6 mm for the cervical vertebrae as against 7.83-8.85mm for the lumbar vertebrae. The superior cervical vertebral facets had a posterior-posteromedial orientation and were vertically to horizontally oval in shape, depending on the level; whereas, the superior lumbar vertebral facets had a posteromedial orientation and were vertically oval in shape at all levels.
The inferior facetal height was 7-13.5 mm for the cervical vertebrae as against 12.6-15.15 mm for the lumbar vertebrae. The width was 8-15mm for the cervical vertebrae as compared to 9.6-13.0mm for the lumbar vertebrae. The thickness ranged from 3 to 6mm for the cervical vertebrae as compared to 8.76-10.75mm for the lumbar vertebrae. The inferior cervical vertebral facets were posteromedially oriented and vertically to horizontally oval in shape, becoming progressively broader from higher to lower level, while the lumbar facets were oriented anterolaterally and were vertically oval in shape at all levels.
Measurements of intervertebral foraminal height and interspinous distance before and after Goel facetal spacer insertion
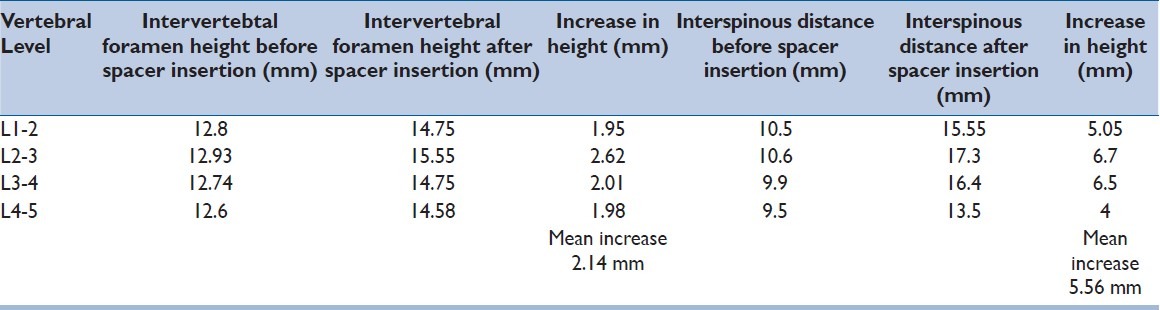
The intervertebral foraminal height was seen to range from 12.6 to 12.93 mm at the measured levels. Intervertebral foramen height before spacer insertion was seen to decrease slightly with each successive vertebral level, being greatest at L2-3 (12.93 mm) and lowest at L4-5 (12.6 mm). Interspinous distance between the different pairs of lumbar vertebrae showed no remarkable variation with spinal level. Maximum distance was seen between L2 and L3 (10.6 mm), and least distance between L4 and L5 (9.5 mm).
We took all the measurements before and after insertion of the Goel facetal spacer. The spacers used were 8 mm in diameter and 2 mm in thickness. The selected spacers had a surface area less than that of the vertebral facet joints to avoid injury to the exiting nerve roots.
After spacer insertion, intervertebral foramen height at each level was seen to increase by an average of 2.14 mm. Spacer insertion dramatically increased interspinous distance by an average of 5.56 mm across all spinal levels. The greatest increase was seen at L2-3 (6.7 mm), and the lowest increase was seen at L4-5 (4 mm).
The details of the changes seen in the various vertebral parameters after spacer insertion have been presented in Table 3.
Table 3.
Effect of spacer insertion on intervertebral foramen height and interspinous distance
DISCUSSION
Degenerative spondylosis can be defined as a series of soft tissues — ligaments, cartilage, and disc — alterations that has genesis from facetal instability related to muscular weakness due to their misuse or disuse and subsequent ‘aging’.[1,2] Ligamentous buckling, osteophyte formation, and disc space reduction that are hallmarks of spondylotic spinal disease appear to be secondary consequences to primary facetal instability. The standing posture of human body lays an unusual and constant stress on the paraspinal muscles of the back. Facetal articulation is the only true joint of the spine on which the entire burden of the spinal pillar of motion, stability, and shape rests. Vertical facetal instability is a result of relative incompetence of the muscles due to ‘aging’ or due to inadequate nurture of its strength. Facetal instability or incompetence leads to ‘vertical instability’ or ‘facetal over-riding’, a phenomenon that is poorly appreciated on radiological imaging due to relatively inadequate delineation on conventional imaging and lack of anatomical and radiological studies. Vertical facetal instability leads to crowding or telescoping of spinal vertebrae. Such an event leads to reduction of space for spinal dural tube in spinal canal and nerve roots during their course in the intervertebral foramina.
The shape, size, orientation, and alignment of lumbar facets are remarkably different when compared to that of cervical facets. The lumbar facets are strong and bulky and are oriented vertically when compared to cervical facets that are more transversely placed. It is difficult to analyze, evaluate, and describe in a three-dimensional (3D) perspective the facets and its angulations due to the complex turns and twists of its structure. Due to the profiling of the facets, both anatomical and radiological studies have inherent limitations and a uniform pattern of assessment and evaluation is difficult if not impossible.
The articular surface of the lumbar vertebral facets is oval in shape. The superior facets are oriented (with the articular surface facing posteromedially) vertically in respect to transverse and coronal planes. The inferior facets were oval in shape with the articular surfaces facing anterolaterally and almost at right angles to the transverse plane and at an angle of about 10-20° to the coronal plane. The lumbar vertebral facets were concave (superior facet) and convex (inferior facet) rather than near flat, like those of the cervical vertebrae. The shape of the superior as well as inferior lumbar vertebral facets was vertically oval at all levels, while that of the cervical ones was vertically oval at higher levels and horizontally oval at lower levels.[3]
Other studies done on lumbar vertebral facet anatomy have measured some of the parameters measured in this study as well as various other parameters such as facet joint surface area, etc. Panjabi found the average height of the vertebral facets from C3 to L5 to be (10.2-18.4 mm), width to be (9.6-16.3 mm), angle with sagittal plane to be (67-154°), and angle with transverse plane to be (41-86°).[4] Another study by Su et al., has found height to be 15.7-17.5 mm.[5]
On inserting of spacers intraoperatively, a tightening of the ligaments is expected as well as an increase in interfacetaland interspinous height. On anatomical examination of the bones, height of the intervertebral foramen was found to increase by (1.77 mm), thereby allowing an increased space for the traverse of the nerve root.
Radiological studies done on the vertebral facet joints have attempted to accurately measure various parameters of the joints. Algorithms have been designed to predict various parameters in vivo as well and computer software has been used to measure various vertebral facet joint parameters.[6] Radiological imaging shows an error of 5-23° in the estimation of facet joint angles as compared to actual measured angles.[7]
Ebraheim et al., in their study[8] on relations of the facet joints reported the distance of the nerve root from the pedicle to be (5.3 mm superiorly and 1.5 mm inferiorly). Attar et al., have also studied the relations of the pedicle, which can help to protect the structures surrounding the facet joints.[9] These can help estimate the position of the nerve root so as to protect it during insertion of the spacers.
The Goel facetalspacers have been used by the senior author for the distraction of cervical and lumbar vertebrae for the treatment of ‘degenerative’ spinal canal issues. The suitability for use in cervical spondylosis has been studied in a morphometric analysis of the cervical facet joints.[3] Biomechanics of interfacetal spacers have been studied and this technique of distraction has been shown to be sound from the biomechanical point of view.
During our study, we were unable to achieve fully accurate measurement of the various parameters due to the fact that we worked on dried bones, where the absence of soft tissue made it difficult to recreate the in vivo anatomy of the vertebrae. The spacers are available in various sizes and it is our suggestion that thorough preoperative imaging could be used to determine the size needed in individual cases as improper selection of spacers could lead to misalignment of the vertebrae following insertion.
Spondylosis is a series of changes that take place in both the bony and the cartilaginous elements of the vertebral facet joints, as well as the surrounding ligaments and vertebral bodies due to aging and lifestyle-related stresses, which cause weakness of muscles of the back. There is vertical displacement of the two articular surfaces of the facet joints with respect to each other, due to vertebral instability arising due to muscular weakness and laxity of ligamentumflavum and the posterior longitudinal ligament. This buckling of ligaments causes some degree of buckling of the spinal column as a whole, resulting in crowding of the vertebrae, leaving less space for the neural elements. This gives rise to symptoms of spinal and nerve root compression. Some of the pathological changes seen are osteophyte formation, thinning of facet joint articular cartilage discs, and change in water content of articular cartilage discs. We believe that the root cause of all these changes is spinal instability, which causes some degree of vertebral facet joint dislocation resulting in secondary effects on the various tissues due to alterations in local dynamics. We feel that this is the reason for symptom relief obtained by physiotherapy, which improves the strength of muscles, which buttress the vertebral column. The correction of the primary abnormality, that is, instability of the spine improves or reverses the other changes and causes symptom relief. Various nonsurgical methods of traction presumably work by similar means, and have been used in the past.[1]
Advantages of our technique are that it gives us the ability to directly visualize the facet joints intraoperatively and get an idea of the degree of instability and corrective measures required. Moreover, the technique is relatively noninvasive as it does not deform the vertebral bones or create permanent defects. By correctly choosing spacers, it is possible to avoid injury to surrounding neurovascular structures.[2]
The role of vertebral facet joint instability in spondylosis is suggested in the study by Don et al.,[10] which showed that a more coronal facet joint orientation might be linked to eventual spondylolisthesis. Masharawi et al., have hinted at a possible relation between the development of symptoms and parameters such as area and orientation of facet joints.[11] The increase in facet area with age is seen to be more pronounced in cases of spondylosis.[12] The study of vertebral facet curvature by van Schaik and van Pinxteren.[13] can help to estimate the technical aspects of spacer insertion in the joint. Moreover, there have been studies showing that there is an inherent asymmetry of facet joint surface curvature bilaterally which might be an area for further study.[14,15]
CONCLUSION
The anatomical analysis of the physical issues relating to facets, its orientation, and strength can be exploited in understanding the dynamics of the spine and in formulation of suitable treatment strategy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Goel A. Facet distraction spacers for treatment of degenerative disease of the spine: Rationale and an alternative hypothesis of spinal degeneration. J Craniovertebral Junction Spine. 2010;1:65–6. doi: 10.4103/0974-8237.77669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goel A. Facet distraction-arthrodesis technique: Can it revolutionize spinal stabilization methods? J Craniovertebral Junction Spine. 2011;2:1–2. doi: 10.4103/0974-8237.85306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah A. Morphometric analysis of the cervical facets and the feasibility, safety, and effectiveness of Goel inter-facet spacer distraction technique. J Craniovertebral Junction Spine. 2014;5:9–14. doi: 10.4103/0974-8237.135208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Panjabi MM, Oxland T, Takata K, Goel V, Duranceau J, Krag M. Articular facets of the human spine. Quantitative three-dimensional anatomy. Spine (Phila Pa 1976) 1993;18:1298–310. doi: 10.1097/00007632-199308000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Su BW, Cha TD, Kim PD, Lee J, April EW, Weidenbaum M, et al. An anatomic and radiographic study of lumbar facets relevant to percutaneous transfacet fixation. Spine (Phila Pa 1976) 2009;34:E384–90. doi: 10.1097/BRS.0b013e3181a39665. [DOI] [PubMed] [Google Scholar]
- 6.Kunkel ME, Schmidt H, Wilke HJ. Prediction of the human thoracic and lumbararticular facet joint morphometry from radiographic images. J Anat. 2011;218:191–201. doi: 10.1111/j.1469-7580.2010.01323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Senoglu N, Senoglu M, Safavi-Abbasi S, Shedd SA, Crawford NR. Morphologic evaluation of cervical and lumbar facet joints: Intra-articular facet block considerations. Pain Pract. 2010;10:272–8. doi: 10.1111/j.1533-2500.2010.00365.x. [DOI] [PubMed] [Google Scholar]
- 8.Ebraheim NA, Xu R, Darwich M, Yeasting RA. Anatomic relations between the lumbar pedicle and the adjacent neural structures. Spine. 1997;22:2338–41. doi: 10.1097/00007632-199710150-00003. [DOI] [PubMed] [Google Scholar]
- 9.Attar A, Ugur HC, Uz A, Tekdemir I, Egemen N, Genc Y. Lumbar pedicle: Surgical anatomic evaluation and relationships. Eur Spine J. 2001;10:10–5. doi: 10.1007/s005860000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Don AS, Robertson PA. Facet joint orientation in spondylolysis and isthmic spondylolisthesis. J Spinal Disord Tech. 2008;21:112–5. doi: 10.1097/BSD.0b013e3180600902. [DOI] [PubMed] [Google Scholar]
- 11.Masharawi YM, Alperovitch-Najenson D, Steinberg N, Dar G, Peleg S, Rothschild B, et al. Lumbar facet orientation in spondylolysis: A skeletal study. Spine. 2007;32:E176–80. doi: 10.1097/01.brs.0000257565.41856.0f. [DOI] [PubMed] [Google Scholar]
- 12.Otsuka Y, An HS, Ochia RS, Andersson GBJ, Espinoza Orías AA, Inoue N. In vivo measurement of lumbar facet joint area in asymptomatic and chronic low back pain subjects. Spine. 2010;15(35):924–8. doi: 10.1097/BRS.0b013e3181c9fc04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Schaik JP, van Pinxteren B. Curvature of the lower lumbar facet joints: Variations at different levels and relationship with orientation. J Spinal Disord. 1999;12:341–7. [PubMed] [Google Scholar]
- 14.Mahato NK. Facet dimensions, orientation, and symmetry at L5-S1 junction in lumbosacral transitional States. Spine (Phila Pa 1976) 2011;20(36):E569–73. doi: 10.1097/BRS.0b013e3181f6ecb2. [DOI] [PubMed] [Google Scholar]
- 15.Tulsi RS, Hermanis GM. A study of the angle of inclination and facet curvature of superior lumbar zygapophyseal facets Spine. (Phila Pa 1976) 1993;18:1311–7. doi: 10.1097/00007632-199308000-00010. [DOI] [PubMed] [Google Scholar]


