Abstract
Background:
The aim of this study was to determine the frequency of patients admitted to Intensive Care Unit (ICU) after elective interventional neuroradiology (INR) procedures under general anesthesia.
Materials and Methods:
We retrospectively evaluated 121 patients underwent INR procedures performed with general anesthesia within a 5-year period. Information including demographics, aneurysm/arteriovenous malformations pathology (ruptured or un-ruptured), preoperative neurological status, co-morbidities, complications during procedure and postoperative admission in ICU were recorded on a predesigned form.
Results:
Elective INR procedure for both ruptured (n = 29, 24%) and un-ruptured (n = 85, 70.25%) aneurysms was performed. Rate of postoperative admission in ICU was significantly high in patients with preoperative ruptured aneurysm (P < 0.01). High rate of neurological deficit, sub-arachnoid hemorrhage (SAH) and hypertension in patients were significant factors of postoperative admission in ICU (P < 0.05). Out of 24 patients, 12 were admitted to ICU postoperatively because of procedure-related complications and 11 were sent due to preexisting significant co-morbidities with added complication of SAH.
Conclusion:
The authors conclude that patients without major co-morbidities, intraoperative complications, or complex aneurysm morphology can be safely observed in a regular ward rather than being admitted to the ICU.
Keywords: General anesthesia, Intensive Care Unit, interventional neuroradiology, sub-arachnoid hemorrhage
INTRODUCTION
Neuroradiological techniques and expertise in the diagnosis and treatment of the central nervous system diseases have undergone significant advances and new diagnostic and therapeutic radiological procedures are introduced.[1] These procedures include coiling and embolization of intracranial aneurysm, arteriovenous malformations (AVMs) and balloon occlusion of arteries supplying aneurysms.[2]
The rapid advancement in the field of interventional neuroradiology (INR) leads to more anesthesiologist involvement in the care of patients undergoing these procedures. Anesthesiologists have several important concerns when providing care to patients who undergo INR procedures, including maintenance of patient immobility and physiologic stability, manipulating systemic or regional blood flow, managing anticoagulation and manage sudden unexpected complications during the procedure.[3] Sometimes, these procedures are postponed due to request of preoperative Intensive Care Unit (ICU) bed arrangement by anesthesia team. On the other hand, if serious complications occurred during the procedure, these patients need immediate transfer to ICU. At times, radiologist also request during procedure to keep these patients in ICU for 24 h. No standard guidelines are present that can facilitate both anesthesiologist and radiologist in making this decision of preoperative ICU bed arrangement in elective cases. The objective of our study was to determine the frequency of patients admitted to ICU after elective INR procedure under general anesthesia. The purpose is to prepare a clinical guideline in the next step which facilitates in decision making.
MATERIALS AND METHODS
This retrospective study was conducted in a tertiary care university hospital. After approval from departmental research committee, we included elective INR procedures under general anesthesia since January 2006 to December 2011. The medical records numbers of patients were obtained from interventional radiology section. The data comprised of all interventional radiology procedures (INR, percutaneous nephrostomy, percutaneous intravenous central catheter insertion, transjugular intrahepatic portosystemic shunt [TIPSS] etc.) and so it was first segregated into INR procedures and other types. Later, the INR procedures under general anesthesia were separated, and their files were retrieved from medical records. Emergency cases, Diagnostic angiography under sedation and patients already admitted in intensive care were excluded. All files were reviewed and crosschecked by primary and secondary author. Information was obtained from preanesthesia clinic notes, preoperative and intraoperative anesthesia forms and any other relevant primary physician's notes in the patient's file were recorded. The data were collected on a predesigned approved form and all statistical analysis was performed using Statistical Packages for Social Science version 19 (SPSS Inc., Chicago, IL, USA).
Age, weight, height, American Society of Anesthesiologists (ASA), gender, co-morbid, postoperative admission in ICU and complication was target observation of the patients. Frequency and percentage was computed for qualitative observation and analyzed by Chi-square test. Mean (±standard deviation) and median (interquartile range) were presented for quantitative variables and analyzed by independent sample t-test and Mann-Whitney test. Normality of quantitative data was also checked by Kolmogorov-Smirnov test.
RESULTS
One hundred and twenty-one patients who underwent INR procedures with general anesthesia during the 5-year period were evaluated. The demographic characteristics of the patients are stated in Table 1. Of 121 patients, 51% are males and 49% are females. Majority of patients were ASA II and most common comorbidity was hypertension. Elective INR procedure for both ruptured (n = 29, 24%) and un-ruptured (n = 85, 70.25%) aneurysms was performed [Table 2]. Neurological deficit was found in 90 (74.4%) cases in which 50 (55.6%) patients reported motor and sensory block deficit, 37 (41.1%) complains about headache, 20 (22.2%) had seizures and 48 (39.7%) patients had preoperative sub-arachnoid hemorrhage (SAH). There were only 27 file records shows that an ICU bed was requested before procedure and 18 (75%) patients were shifted to ICU.
Table 1.
Demographic characteristics of patients (n = 121)
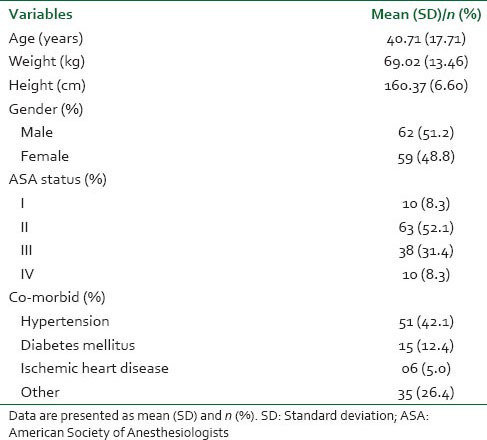
Table 2.
Comparison of preoperative factors with and without postoperative ICU admission (n = 121)
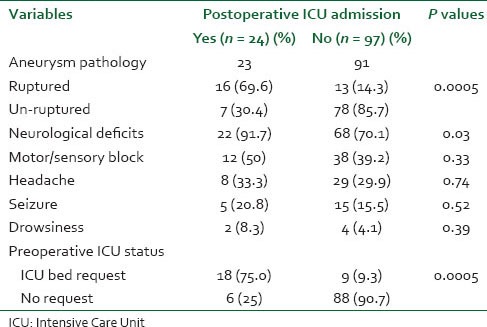
Rate of postoperative admission in ICU was significantly high in those cases that had a preoperative ruptured aneurysm when compared to un-ruptured (P < 0.01). High rate of neurological deficit, SAH and hypertension in patients were significant factors of postoperative admission in ICU (P < 0.05). There were 24 patients in total who required ICU admission and most pertinent reasons related to this are presented in Figure 1. Twelve patients had complications during the procedure and vasospasm was the commonest that is, 5 (41.6%) cases, while bleeding due to rupture was occurred in 2 (16.7%) cases. There were six patients in which other different complications were reported. Eleven patients were sent to ICU because of their significant co-morbidities and preoperative neurological deficits.
Figure 1.
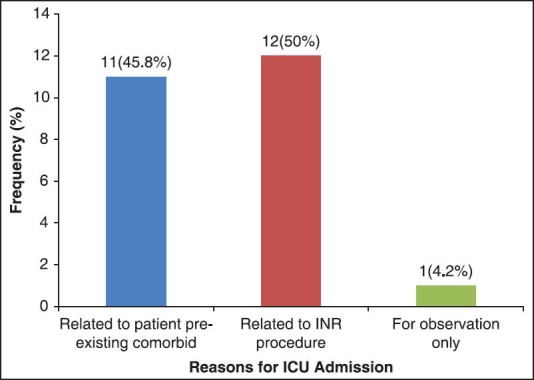
Reasons for Intensive Care Unit admission (n = 24) after elective interventional neuroradiology procedure under general anesthesia
DISCUSSION
In this study, we have retrospectively evaluated about patients needing intensive care admission after endovascular treatment of cerebral aneurysm or AVMs. The study was also undertaken to find out the percentage of cases postponed due to unavailability of ICU bed for INR procedures but, unfortunately, we could not find any pertinent data or notes that could reflect this aspect. This also made us think about collecting certain prospective data about these proportions of cases.
Interventional radiology is increasingly performed with the administration of anesthesia.[4] Escalating number of these procedures, as well as the variety in types and degrees of difficulty of interventional radiological practice, has brought about this occurrence. SAH is the unstable entities of the aneurysmal pathology, which carries the highest risk of morbidity because of re-rupture hydrocephalus, vasospasm and co-morbid diseases.[5] During endovascular treatment, the two serious potential complications are cerebral infarcts and SAH. There is increased tendency to develop medical complications after SAH notably hypertension, arrhythmias, myocardial ischemia, electrocardiography abnormalities, hyponatremia and pneumonia.[6] Hypertension and hyponatremia occurs in 27% and 30-40% cases respectively. Our study also detected hypertension as more frequent co-morbidity and present in about 42% of cases.
There is limited information about the need and indications for ICU admission in patients undergoing elective endovascular procedures. Studies on neurosurgical patients after craniotomy have suggested that ICU care after craniotomy may not be necessary. Zimmerman et al.[7] conducted a multicenter analysis of 3000 patients admitted to ICU care for neurosurgical diseases and found that among patients who were only observed in the ICU, <10% were likely to need any ICU treatments. Their analysis highlighted the need for comprehensive admission guidelines to the ICU.
Two studies are found in the literature relevant to this topic. Burrows et al.[8] analyzed a prospective consecutive series of 200 elective unselected un-ruptured aneurysms treated over a 40-month period. Decisions about postprocedure disposition (ICU step-down unit versus regular ward) were made at the end of the procedure, and 65% of patients were triaged to routine (non-Intensive Care Unit) floor care based on case complexity and intra procedural findings. Only one patient (0.5%) required subsequent transfer to the ICU for management of a perioperative complication. The authors conclude that patients without major co-morbidities, intraoperative complications, or complex aneurysm morphology can be safely observed in a regular ward. In our study, 12 patients had complications during the procedure that requires ICU admission. In their retrospective study about factors associated with ICU admission after elective endovascular treatment of un-ruptured intracranial aneurysms, Eisen et al.[9] studied 170 patients charts, which revealed immediate postoperative ICU admission occurred after 41 of 170 (24%) procedures; 6 patients (15%) remained intubated, and 3 (7%) were on vasopressors. They conclude that the primary determinants of immediate postoperative ICU admission were intraoperative thromboembolic events and administration of supplemental anticoagulants. Patient co-morbidities were not major factors and in most cases, the need for ICU admission cannot be ascertained until the procedure is largely completed.
Our study has limitations. It is a single center study but advance interventional radiology services are only offered by our tertiary care hospital with anesthesia and intensive care support. The results will be applicable and can be used to make some guidelines. Second, the most important information about case cancellation or postponement due to nonavailability of ICU bed was missing. To rectify this problem in the future, the authors are in the process of developing a template to gather all information.
CONCLUSION
Serious complications after endovascular elective aneurysm treatment are most often evident during the procedure or immediately on awakening. The presence of intraoperative complications, complex aneurysm morphology, or severe medical comorbidities may predispose to ICU admission. In the absence of these complications or predisposing factors, patients may safely be observed on the floor.
ACKNOWLEDGMENTS
The authors would like to acknowledge the contribution and efforts of Mr. Amir Raza, Research Coordinator, Department of Anesthesiology for helping out in statistical analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Varma MK, Price K, Jayakrishnan V, Manickam B, Kessell G. Anaesthetic considerations for interventional neuroradiology. Br J Anaesth. 2007;99:75–85. doi: 10.1093/bja/aem122. [DOI] [PubMed] [Google Scholar]
- 2.Young WL, Pile-Spellman J. Anesthetic considerations for interventional neuroradiology. Anesthesiology. 1994;80:427–56. doi: 10.1097/00000542-199402000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Sinha PK, Neema PK, Rathod RC. Anesthesia and intracranial arteriovenous malformation. Neurol India. 2004;52:163–70. [PubMed] [Google Scholar]
- 4.Dorairaj IL, Hancock SM. Anesthesia for interventional neuroradiology. Contin Educ Anaesth Crit Care Pain. 2008;8:86–9. [Google Scholar]
- 5.Osborn IP. Anesthetic considerations for interventional neuroradiology. Int Anesthesiol Clin. 2003;41:69–77. doi: 10.1097/00004311-200341020-00009. [DOI] [PubMed] [Google Scholar]
- 6.Luoma A, Reddy U. Acute management of aneurysmal subarachnoid haemorrhage. Contin Educ Anaesth Crit Care Pain. 2013;13:52–8. [Google Scholar]
- 7.Zimmerman JE, Junker CD, Becker RB, Draper EA, Wagner DP, Knaus WA. Neurological intensive care admissions: Identifying candidates for intermediate care and the services they receive. Neurosurgery. 1998;42:91–101. doi: 10.1097/00006123-199801000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Burrows AM, Rabinstein AA, Cloft HJ, Kallmes DF, Lanzino G. Are routine intensive care admissions needed after endovascular treatment of unruptured aneurysms? AJNR Am J Neuroradiol. 2013;34:2199–201. doi: 10.3174/ajnr.A3566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eisen SH, Hasan DM, Bayman EO, Hindman BJ. Factors associated with ICU admission after elective endovascular treatment of unruptured intracranial aneurysms. Anesthesiology. 2013;119:A4121. [Google Scholar]


