Abstract
Context and Aims:
Little is known about onset and duration of sciatic block after 0.5% levobupivacaine (Levo) versus 0.5% ropivacaine (Ropi) for ultrasound-guided technique. We assessed these parameters in the ultrasound-guided block, to know for the practice.
Setting and Design:
A comparative randomized double-blind study was conducted in the University Hospital.
Materials and Methods:
Were included 35 adults of ASA I-II, scheduled for foot surgery, presenting clear imaging of their sciatic nerve at mid-thigh. A volume of 20 mL of either 0.5% Levo or 0.5% Ropi were injected around the sciatic nerve at mid-thigh using ultrasound guidance (out of the plane) followed by placement of a catheter to use, if necessary, for perioperative analgesia. A femoral single shot block was systematically performed to block the saphenous nerve. The onset times until complete foot block (primary outcome) and the sensory and motor block duration (secondary outcome) were assessed using Wilcoxon test. Values were expressed as medians (1st-3rd quartile).
Results:
Except for two delayed sciatic blocks in each group, the onset time otherwise was 35 min (20-60) in Ropi versus 40 min (30-60) in Levo, P = 0.5. Sensory block lasted longer in Levo, 17 h (14-27) compared with 15 h (10-17) in Ropi, P = 0.04. No significant between-group difference was found with motor block durations, 15 h (12-18) in Levo and 15 h (12-16) in Ropi, P = 0.3.
Conclusion:
No difference of onset times was found in ultrasound-guided sciatic block whether using Levo or Ropi. Levo induced a longer-lasting sensory block.
Keywords: Levobupivacaine, ropivacaine, sciatic, ultrasound
INTRODUCTION
0.5% ropivacaine (Ropi) and 0.5% levobupivacaine (Levo) are two levorotatory S-isomers of amide local anesthetics (LAs) available for peripheral nerve blocks. Onset and duration of sciatic nerve blocks are known to be statistically not different following a single dose of these LAs administered in the gluteal region, based on surface landmarks and nerve stimulation.[1] To the best of our knowledge, no comparison of these LAs has been made in terms of block onset and duration after ultrasound-guided sciatic block. We, therefore, conducted a comparative randomized double blind study of these LAs in sciatic blocks using the lateral mediofemoral approach,[2,3,4] ultrasound-guidance and electro-stimulation for nerve confirmation. The primary outcome was the onset times of sciatic block after a single dose of 0.5% Levo or Ropi. We were curious to see what values they took and how different they were to adapt our daily practice and address the concerns with a delay to the operating room.[5] The secondary outcome included the duration of motor and sensory block following a single dose of the LAs of interest, the subsequent pain rebound and the utility of the catheter placed around the sciatic nerve. As a technique of block was based in ultrasonic imaging, we took advantage of the imagery to comprehend the results and explore the relationship between the fibular and tibial nerves at mid-thigh.
MATERIALS AND METHODS
Subjects
This prospective, comparative, double-blind and randomized study obtained the authorization of the Ethics Committee (CPP OUEST II — ANGERS, Ref: BRD 08/5-D) for 3 years (November 2008 to November 2011). Written informed consent was obtained from all subjects. ASA I-II adult patients of both genders, scheduled for non-ambulatory foot surgery, were enrolled. The surgery was performed with the tourniquet placed above the malleoli. As pointed out,[6] ultrasonic identification of the sciatic nerve might be poor at mid-thigh in 37% of patients, we therefore, carried out a scout ultrasound scan before inclusion. Patients whose sciatic nerve was not clearly imaged, patients with a coagulation disorder, allergy to LAs, infection at the puncture site, pre-existing neurologic dysfunction, severe diabetes, and difficulty in understanding instructions were not included. Eligible patients were randomized via TENALEA (Trans European Networks for Clinical Trials Service; http://tenalea.net/) using an allocation ratio 1:1 and block size of 4. In the Ropi group, patients received Ropi 0.5% for surgical block followed by patient controlled analgesia (PCA) Ropi 0.2% for postoperative 48 h. In the Levo group, patients received Levo 0.5%, followed by Levo 0.2%.
Anesthetic procedure and protocol
Premedicated patients were admitted to the operating theater 1 h before surgery. Regional techniques were conducted under aseptic conditions and in a dedicated room. The investigator performed the blocks, combining ultrasound guidance and neurostimulation. The following materials were used: M-Turbo® (Sonosite France, Courtaboeuf) and high resolution 38 mm linear transducer, insulated stimulating needle with corner-stone reflectors, SonoPlex® Stim cannula (22 G × 80 mm, Pajunk®, Germany, Geisingen) for single shot blocks, Stimulong® Sono kit (Pajunk®, Germany, Geisingen) containing a Plexolong® nanoline cannula (100 mm × 19 G) with the facet tip, a Stimulong® catheter (20 G × 50 cm), a Stimulong® adapter for a continuous block, and the PCA pump AmbIT® (Sorenson Medical, Inc. USA, Utah) for analgesia. In a sterile room, according to the randomization, the pharmacist prepared 120 mL of 600 mg of either Levo (Abbott France) or Ropi (Astra Zeneca France). The prepared 0.5% Ropi and 0.5% Levo were delivered in an unidentified Ecoflac® (nominal filling volume 250 mL).
The investigator first blocked the sciatic nerve using the lateral mid femoral approach.[2,3,4] With the probe placed on the lateral aspect of the mid-thigh and the orientation-marker up, the investigator scanned the cross-sectional image of the sciatic nerve. At mid-thigh, nerve separation is less likely.[7] After anesthetizing the skin, the investigator inserted the Sonoplex® Stim cannula out of the plane toward the sciatic nerve. The needle tip stimulated (0.1 ms, 0.8 mA) the half posterior and half anterior of the lateral aspect of the sciatic nerve successively, in search of a motor response from the foot (dorsal flexion for fibular or plantar flexion for the tibial nerve). The sciatic nerve was then infiltrated with 20 mL of unidentified LA retrieved from the Ecoflac®. The needle moved towards the lateral aspect of the nerve and reached the anterior or posterior pole by orienting the needle slightly oblique to reveal the medial aspect. The objective was to surround the nerve with LAs but avoid any intraneural injection.[8,9] Videoclips were systematically saved for further analysis. The injection ended on the lateral aspect of the nerve. The investigator then removed the needle and placed the Plexolong cannula into the expanded perineural space lateral to the nerve. The investigator immobilized the cannula, put aside the transducer and threaded a Stimulong catheter into the cannula, moving 5 cm past the cannula tip. Electro-stimulation of the catheter (0.1 ms up to 5 mA) was performed via the adapter in search of motor responses from the foot. The stimulating catheter was left in place with or without motor response.[10,11] Sutures secured the catheters in a position which was documented by ultrasound air contrast imaging, by flushing 2 mL of filtered air into the catheter. After catheter dressing, to block the sensory saphenous nerve, the femoral nerve was blocked with the previously used Sonoplex® Stim Cannula. A volume of 10 mL of lidocaine 1% with epinephrine (AstraZeneca France) was injected around the femoral nerve.
Data collection
Motor and sensory loss in the sciatic and femoral nerves was assessed every 10 min for 60 min. The assessment started at the end of LA injection. The sciatic nerve blockade was assessed through the force of dorsal and plantar flexion of the foot (motor testing), as well as, response to pinprick applied to the dorsal and plantar aspects of the foot (sensory testing). The femoral nerve blockade was assessed by the patient's ability to raise the extended leg above the plane of the bed (quadriceps motor testing), as well as, the response to pinprick applied to the anterior and medial aspect below the knee (sensory testing of the saphenous nerve). The assessment used the M.S. grading scale (M for motor and S for sensory) corresponding to a modification of Highet's method of grading.[12] Motor block was defined as no contraction (M0), isometric contraction but no motion (M1), complete motion possible without the action of gravity (M2), complete motion against gravity (M3), complete motion against resistance (M4), normal (M5). Sensory block was defined as no sensation at all (S0), sensation but inability to distinguish application of the head or point of a pin (S1), sharp tingling and stinging sensation (S2), correct localization of 2 points within 2 cm of each other (S3), normal sensation (S4). M≤1S0 scores characterized a complete block. M2S2 characterized an incomplete block leading to rescue by injecting 10 mL of lidocaine 2% with epinephrine via the catheter before surgery. If necessary, general anesthesia was carried out.
Postoperatively, all the patients were transferred to the post-anesthesia care unit (PACU) where the sciatic nerve block was re-assessed by the investigator before the Ambit pump was connected. The pump was set with the following program: No infusion, 15 min lockout, 10 mL bolus of unknown local diluted to 0.2% (strictly aseptic addition of 150 mL normal saline to the remaining 100 mL LA in the Ecoflac®). All patients received a basal treatment (paracetamol 1,000 mg every 6 h and ketoprofen 100 mg every 12 h). Motor and sensory testing was performed by nurses every hour overnight (research constraints). Data were collected every 6 h for 48 h using the same MS grading scale. Patients and nurses were instructed to collaborate and note the time of recovery of foot movement (plantar or dorsal flexion) and the time of the first request for extra-analgesics (PCA-bolus of LAs via the perineural catheter associated or not with subcutaneous or oral morphine). The data collected were checked by the investigator every morning postoperatively. Motor block duration was the time elapsing from complete block to recovery of foot movement. Sensory block duration was the time elapsing from complete block to the first request for analgesics. Pain at rest was assessed by the nurses every 6 h based on a visual analogue score (VAS; 0: No pain — 100 mm: Unbearable) and assessed once on ambulation.
The primary outcome was onset time till complete block of the sciatic nerve. The secondary outcome included duration of motor and sensory blocks, pain scores, doses of analgesics for rescue, patient satisfaction (0/10-10/10), consumption of unidentified 0.2% LA and duration of postoperative regional analgesia (time elapsing from placement to removal of the catheter), early preoperative adverse events and results of neurostimulation of the sciatic nerve. A three-month follow-up was provided by the attending surgeon to detect any secondary neuropathy.
Statistics
The calculation of sample size was based on the onset times found by Casati et al.,[1] the sole data available at the time our study was designed. To demonstrate the difference of at least 10 min in sciatic block onset time between 0.5% Levo and 0.5% Ropi, in the knowledge that previously, Casati et al. had noted 15 min and 30 min respectively, assuming the same standard deviation of 17 and accepting alpha risk and beta risk at 5% and 20% respectively, we estimated that 21 patients were required in each group.
The baseline characteristics were only described in both groups of this randomized study. The comparability of the two groups regarding the quality of femoral nerve blocks was studied, based on a comparison of femoral block onset times (Wilcoxon test).
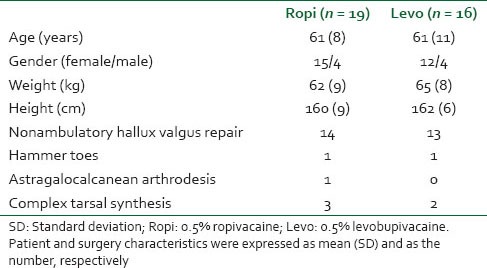
The onset times till complete block (M0S0) of the fibular and tibial components of the sciatic nerve were subjected to Kaplan–Meier survival statistics. Differences between groups were tested by Log-rank tests. Patients who did not have a complete block were considered to be censored observations at 60 min. To be practical, we considered and presented the onset times till complete sciatic nerve block of both groups. They were compared using the Wilcoxon test. The relationship between quality of the blocks and characteristics of the ultrasonic images was studied using Fisher's exact test.
Data of the secondary outcome were analyzed with Chi-square tests, Fisher's exact tests, Wilcoxon tests and the Wilcoxon signed rank test (for paired data). A boxplot was used to describe the evolution over time of the VAS score at rest.
Unless otherwise stated, the results were expressed as median values with 1st-3rd quartile in brackets.
All patients were analyzed by independent statisticians from the Clinical Research Administration, based on the Intention to Treat Principle. All reported P-values were two-sided, with a significance level of 0.05. SAS Statistical Software version 9.3 (SAS Institute Inc., Cary, North Carolina) was used.
RESULTS
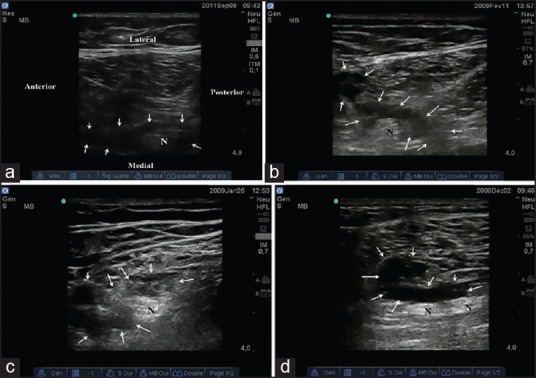
The study finally included 35 patients. Nineteen of them were assigned to Ropi and 16 to Levo. Patient and surgical characteristics are shown in Table 1. Both groups were comparable in terms of successful femoral block, as the median onset times till complete femoral nerve block were 15 min for both groups (P = 0.6).
Table 1.
Patient and surgery characteristics
Primary outcome
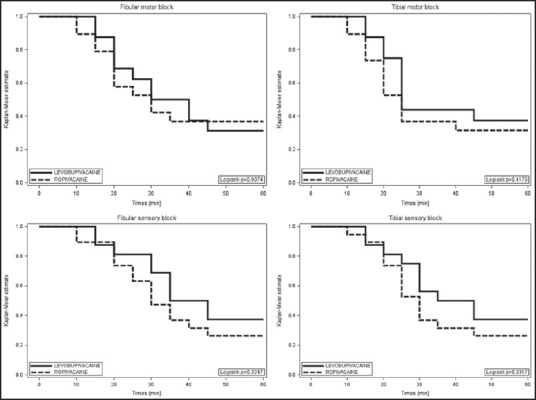
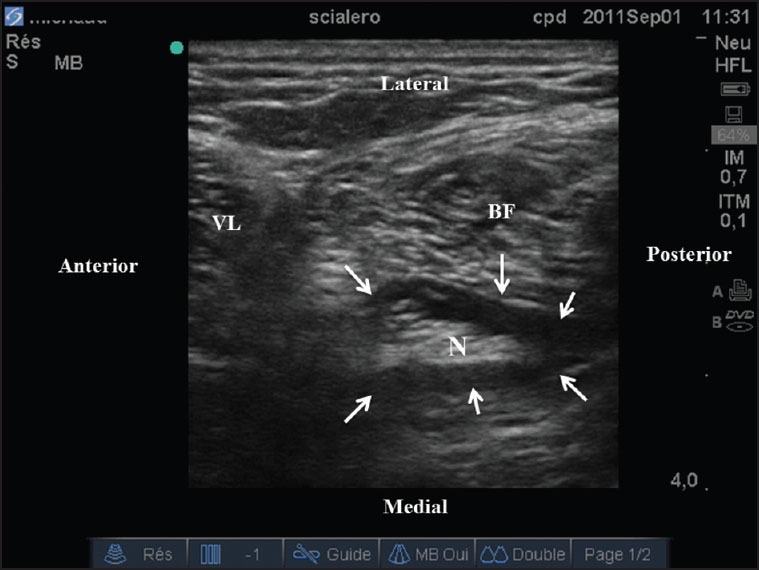
We found no between-group difference regarding block installation over time for the fibular and tibial components of the sciatic nerve [Figure 1]. The onset time till complete block was 35 min (20-60) for 17 out of 19 patients in Ropi versus 40 min (30-60) for 14 out of 16 in Levo (P = 0.5). These results corresponded to typical doughnut images [Figure 2]. Two patients in each group had incomplete block before surgery, despite 10 mL lidocaine 2% + epinephrine being injected into the catheter for rescue. General anesthesia was finally carried out. In PACU, these sciatic nerve blocks appeared to be finally complete. In these delayed blocks, the spread of 20 mL locals was aberrant, forming the atypical doughnut image [Figure 3]. There was a strong relationship between the block ready/unready to surgery and the typical/atypical image of the doughnut (P < 0.001).
Figure 1.
Onset of fibular and tibial blocks with 0.5% levobupivacaine and ropivacaine. Kaplan–Meier survival curves showed no between group difference regarding the block installation. There were 2 blocks delayed beyond 60 min in both groups
Figure 2.
Ultrasonic typical doughnut image. Hypo-echoic 20 mL local anesthetic typically surrounded the sciatic nerve at mid-thigh (arrows). VL: Vastus lateralis; BF: Biceps femoris; N: Nerve
Figure 3.
Ultrasonic atypical images of four incomplete blocks. Hypo-echoic 20 mL local anesthetic had aberrant spreads (arrows). Images b, c and d use the orientation shown in image a. N: Nerve
Secondary outcome
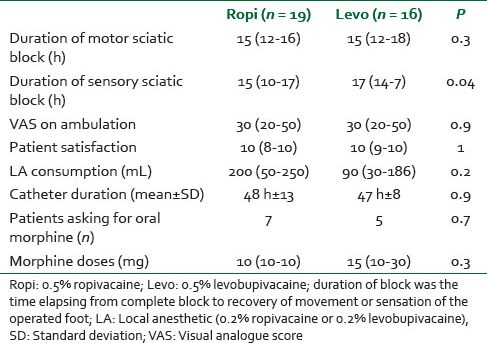
Data were shown in Table 2. We found no between-group difference regarding the duration of motor block of the sciatic nerve. However, we found significant between-group differences regarding sensory block duration. In the Levo group, sensory block of the sciatic nerve lasted longer than motor block (P = 0.02, paired data). By contrast, motor block and sensory block lasted for comparable times in the Ropi group (P = 0.1, paired data).
Table 2.
Secondary outcome
Neither did we find any difference in pain scores at rest during hospitalization [Figure 4]. Neither were there any between-group differences in pain scores for ambulation, patient satisfaction, LA consumption, duration of postoperative regional analgesia and doses of morphine for rescue [Table 2]. We found one patient in each group for whom paracetamol + ketoprofen sufficed postoperatively. These two patients had recovered normal movement and sensation on the operated foot, but they did not ask for extra-analgesics (LA consumption = 0, morphine = 0).
Figure 4.
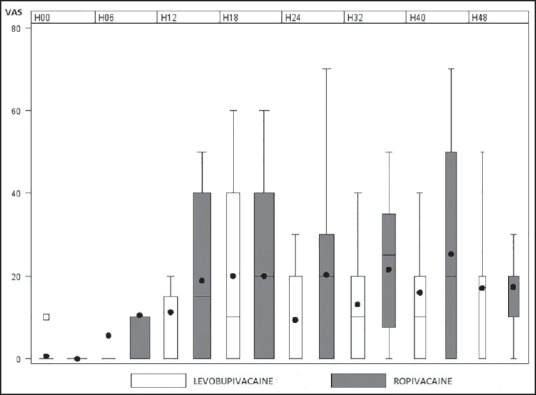
Evolution of postoperative pain scores at rest. The evolution of pain scores is illustrated from H0, the time of arrival on the ward, till 48 h postoperative (H48). There was no between group difference overtime. Note the pain rebound followed by stabilization at acceptable level of visual analogue score scores. The bottom and top of the box represent 1st and 3rd quartile, respectively. The bar inside the box represents median values. The whiskers represent 10th and 90th percentile. The black dots represent mean values
For 34 patients, electrostimulation of the lateral aspect of the posterior half of the sciatic nerve evoked plantar flexion (tibial nerve) and lateral electrostimulation of the anterior half evoked dorsal flexion (fibular nerve). An opposite response was found in one patient. No separation of the sciatic nerve was observed using ultrasound resolution.
No patients showed signs of LA systemic toxicity, either intra-operatively or postoperatively. There was no secondary neuropathic feedback by the attending surgeon.
DISCUSSION
In this monocenter randomized double-blind study, after administration of 20 mL of 0.5% Levo and Ropi, the median onset times till complete block of the sciatic nerve were not significantly different. They corresponded to the typical doughnut image obtained after LA infiltration around the sciatic nerve. Our results approached the values reported in 2010 by Pujol et al.[13] These authors used ultrasound-guided popliteal sciatic block on unselected patients with 30 mL of locals. In the same year, Fournier et al. reported onset times averaging 15 min for 0.5% Ropi and Levo in sciatic nerve blocks based on a modified Labat approach and nerve stimulation.[14] There was definitely no statistical difference in terms of onset times between the two locals studied. This agrees with the pharmacology. Ropi and Levo have the same pKa 8.1.[15,16] Given this absence of statistical difference repeated in the literature,[1,13,14] and given the approaching expiry of the authorization for this study, an interim analysis for futility[17] was conducted after 35 patients were included. This analysis will not increase the alpha risk, but they allows to stop the recruitment if there is no chance to reject the null hypothesis at the planned end of the study. In this futility analysis, the post power test calculated was 13%. Hence, to demonstrate a significant difference between the 2 groups with a 5% alpha value, considering our results, 204 patients would have been needed in each group. Instead of continuing the enrolment of 7 more patients, we preferred to use available data. These data were controlled by ultrasound imaging, the originality of this study. They were applicable to our daily practice as they were obtained by consecutive assessment of all patients eligible in this study.
Thirty-five or 40 min for the onset of sciatic block is too long and may delay to the operating room.[5] To hasten block installation as recommended,[5] shorter acting locals or other concentrations[18,19] must be used. The video-clips of the four delayed blocks showed atypical images which could have been improved by injecting more locals around the nerve. To avoid failure, two suggestions can be made. Do not accept any atypical image, but adjust the needle and inject more locals around the nerve if not restricted by 20 mL of locals as imposed by the protocol. Do not rely on block troubleshooting by injecting lidocaine into the catheter. Hence, keeping these suggestions in mind, we can use 0.5% Ropi or 0.5% Levo indifferently. At least 40 min are required to block and test before surgery.
Considering the various values with onset times without statistical difference found in our study and reported in the literature[1,13,14] we speculate that other factors might influence block installation. Firstly, it could be a technique used to deposit locals on the nerve. For the ultrasound technique, it may be interesting to test the studied LAs using unconventional deposition techniques recently described.[20,21] Secondly, it might be the approaches to the sciatic nerve (from distal to proximal) as reported by Taboada et al. with neurostimulation.[22] It might be interesting to test the LAs studied while using ultrasound-guided sciatic blocks for these different approaches.
As for secondary outcome, we focused on the duration of sensory and motor block. Unlike Pujol et al.[13] we found that the sensory block lasted 2 h longer with Levo than with Ropi [Table 2]. The longer duration of sensory block is perhaps because Levo is 10 times more lipophilic than Ropi.[15,16] It was recently demonstrated that Levo is more lipophilic and is a more potent vasoconstrictor than Ropi.[23] We conjecture that these two properties can lead to greater delay in vascular absorption of 0.5% Levo versus its comparator.
Like Piangatelli et al. although they used surface landmarks and neurostimulation,[24] we found a longer time between motor and sensory resolution after 0.5% Levo. This allows for the treatment of pain rebound, anticipated and organized on the basis of motor recovery.
All the patients except one in each group experienced pain rebound. According to our results [Table 2 and Figure 4], the sciatic catheter appears to be helpful as a relay to the postoperative ending effect of a single dose of long-acting LA.
The relationship between the two components of the sciatic nerve at mid-thigh has not been clearly explored.[2,3,4,6] It is now established in this study. The tibial component mostly runs closely posterior to the fibular.
In conclusion, as the onset times of sciatic block using an ultrasound-guided technique are not different whether using 0.5% Levo or Ropi there is no organizational advantage to favor one or the other local for block induction. However, the preferred choice may be for 0.5% Levo for postoperative analgesia.
Footnotes
Source of Support: The study was funded by GRACE of Nantes and sponsored by University Hospital of Nantes
Conflict of Interest: None declared.
REFERENCES
- 1.Casati A, Borghi B, Fanelli G, Cerchierini E, Santorsola R, Sassoli V, et al. A double-blinded, randomized comparison of either 0.5% levobupivacaine or 0.5% ropivacaine for sciatic nerve block. Anesth Analg. 2002;94:987–90. doi: 10.1097/00000539-200204000-00039. [DOI] [PubMed] [Google Scholar]
- 2.Naux E, Pham-Dang C, Petitfaux F, Bodin J, Blanche E, Hauet P, et al. Sciatic nerve block: An new lateral mediofemoral approach. The value of its combination with a "3 in 1" block for invasive surgery of the knee. Ann Fr Anesth Reanim. 2000;19:9–15. doi: 10.1016/s0750-7658(00)00129-5. [DOI] [PubMed] [Google Scholar]
- 3.Pham Dang C, Gouraud D. Ultrasound imaging of the sciatic nerve in the lateral midfemoral approach. Reg Anesth Pain Med. 2009;34:281–2. doi: 10.1097/AAP.0b013e3181a32a1f. [DOI] [PubMed] [Google Scholar]
- 4.Domingo-Triadó V, Selfa S, Martínez F, Sánchez-Contreras D, Reche M, Tecles J, et al. Ultrasound guidance for lateral midfemoral sciatic nerve block: A prospective, comparative, randomized study. Anesth Analg. 2007;104:1270–4. doi: 10.1213/01.ane.0000221469.24319.49. [DOI] [PubMed] [Google Scholar]
- 5.Oldman M, McCartney CJ, Leung A, Rawson R, Perlas A, Gadsden J, et al. A survey of orthopedic surgeons’ attitudes and knowledge regarding regional anesthesia. Anesth Analg. 2004;98:1486–90. doi: 10.1213/01.ane.0000113549.98873.b1. [DOI] [PubMed] [Google Scholar]
- 6.Barrington MJ, Lai SL, Briggs CA, Ivanusic JJ, Gledhill SR. Ultrasound-guided midthigh sciatic nerve block-a clinical and anatomical study. Reg Anesth Pain Med. 2008;33:369–76. doi: 10.1016/j.rapm.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Floch H, Naux E, Pham Dang C, Dupas B, Pinaud M. Computed tomography scanning of the sciatic nerve posterior to the femur: Practical implications for the lateral midfemoral block. Reg Anesth Pain Med. 2003;28:445–9. doi: 10.1016/s1098-7339(03)00230-x. [DOI] [PubMed] [Google Scholar]
- 8.Chan VW, Brull R, McCartney CJ, Xu D, Abbas S, Shannon P. An ultrasonographic and histological study of intraneural injection and electrical stimulation in pigs. Anesth Analg. 2007;104:1281–4. doi: 10.1213/01.ane.0000250915.45247.24. [DOI] [PubMed] [Google Scholar]
- 9.Lupu CM, Kiehl TR, Chan VW, El-Beheiry H, Madden M, Brull R. Nerve expansion seen on ultrasound predicts histologic but not functional nerve injury after intraneural injection in pigs. Reg Anesth Pain Med. 2010;35:132–9. doi: 10.1097/AAP.0b013e3181d25cfe. [DOI] [PubMed] [Google Scholar]
- 10.Pham Dang C, Lelong A, Guilley J, Nguyen JM, Volteau C, Venet G, et al. Effect on neurostimulation of injectates used for perineural space expansion before placement of a stimulating catheter: Normal saline versus dextrose 5% in water. Reg Anesth Pain Med. 2009;34:398–403. doi: 10.1097/AAP.0b013e3181b48648. [DOI] [PubMed] [Google Scholar]
- 11.Gandhi K, Lindenmuth DM, Hadzic A, Xu D, Patel VS, Maliakal TJ, et al. The effect of stimulating versus conventional perineural catheters on postoperative analgesia following ultrasound-guided femoral nerve localization. J Clin Anesth. 2011;23:626–31. doi: 10.1016/j.jclinane.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Highet WB. Memorandum addressed to the nerve injuries committee: Quoted by Zachary RB. In: Seddon HJ, editor. Peripheral Nerve Injuries Medical Research Council. Special Report Series, No. 282. Ch. 8. London: Her Majesty's Stationnery Office; 1954. pp. 354–5. [Google Scholar]
- 13.Pujol E, Faulí A, Anglada MT, López A, Pons M, Fàbregas N. Ultrasound-guided single dose injection of 0.5% levobupivacaine or 0.5% ropivacaine for a popliteal fossa nerve block in unilateral hallux valgus surgery. Rev Esp Anestesiol Reanim. 2010;57:288–92. doi: 10.1016/s0034-9356(10)70229-2. [DOI] [PubMed] [Google Scholar]
- 14.Fournier R, Faust A, Chassot O, Gamulin Z. Levobupivacaine 0.5% provides longer analgesia after sciatic nerve block using the Labat approach than the same dose of ropivacaine in foot and ankle surgery. Anesth Analg. 2010;110:1486–9. doi: 10.1213/ANE.0b013e3181d3e80b. [DOI] [PubMed] [Google Scholar]
- 15.Casati A, Putzu M. Bupivacaine, levobupivacaine and ropivacaine: Are they clinically different? Best Pract Res Clin Anaesthesiol. 2005;19:247–68. doi: 10.1016/j.bpa.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Leone S, Di Cianni S, Casati A, Fanelli G. Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed. 2008;79:92–105. [PubMed] [Google Scholar]
- 17.Schoenfeld DA. Pro/con clinical debate: It is acceptable to stop large multicentre randomized controlled trials at interim analysis for futility. Pro: Futility stopping can speed up the development of effective treatments. Crit Care. 2005;9:34–6. doi: 10.1186/cc3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Casati A, Fanelli G, Borghi B, Torri G. Ropivacaine or 2% mepivacaine for lower limb peripheral nerve blocks. Study Group on Orthopedic Anesthesia of the Italian Society of Anesthesia, Analgesia, and Intensive Care. Anesthesiology. 1999;90:1047–52. doi: 10.1097/00000542-199904000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Casati A, Vinciguerra F, Santorsola R, Aldegheri G, Putzu M, Fanelli G. Sciatic nerve block with 0.5% levobupivacaine, 0.75% levobupivacaine or 0.75% ropivacaine: A double-blind, randomized comparison. Eur J Anaesthesiol. 2005;22:452–6. doi: 10.1017/s0265021505000773. [DOI] [PubMed] [Google Scholar]
- 20.Buys MJ, Arndt CD, Vagh F, Hoard A, Gerstein N. Ultrasound-guided sciatic nerve block in the popliteal fossa using a lateral approach: Onset time comparing separate tibial and common peroneal nerve injections versus injecting proximal to the bifurcation. Anesth Analg. 2010;110:635–7. doi: 10.1213/ANE.0b013e3181c88f27. [DOI] [PubMed] [Google Scholar]
- 21.Tran de QH, Dugani S, Pham K, Al-Shaafi A, Finlayson RJ. A randomized comparison between subepineural and conventional ultrasound-guided popliteal sciatic nerve block. Reg Anesth Pain Med. 2011;36:548–52. doi: 10.1097/AAP.0b013e318235f566. [DOI] [PubMed] [Google Scholar]
- 22.Taboada M, Alvarez J, Cortés J, Rodríguez J, Rabanal S, Gude F, et al. The effects of three different approaches on the onset time of sciatic nerve blocks with 0.75% ropivacaine. Anesth Analg. 2004;98:242–7. doi: 10.1213/01.ANE.0000093311.29111.59. [DOI] [PubMed] [Google Scholar]
- 23.Sung HJ, Ok SH, Sohn JY, Son YH, Kim JK, Lee SH, et al. Vasoconstriction potency induced by aminoamide local anesthetics correlates with lipid solubility. J Biomed Biotechnol 2012. 2012 doi: 10.1155/2012/170958. 170958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piangatelli C, De Angelis C, Pecora L, Recanatini F, Testasecca D. Levobupivacaine versus ropivacaine in psoas compartment block and sciatic nerve block in orthopedic surgery of the lower extremity. Minerva Anestesiol. 2004;70:801–7. [PubMed] [Google Scholar]


