Abstract
Context:
Anxiety and distress regarding dental treatment is a major issue for dental patients and can be exaggerated in pediatric dental patients.
Aims:
The aim was to investigate how different methods of induction for general anesthesia affect children's distress for dental procedures such as extraction of teeth.
Subjects and Methods:
This was an observational clinical study conducted at Manchester University Dental Hospital. The induction of anesthesia in children was achieved with either intravenous (I.V.) or a gaseous induction. The Modified Child Smiley Faces Scales were completed for children at various times intervals.
Statistical Analysis Used:
There were statistically significant differences between the mean distress scores for the I.V. and inhalation groups (P values from independent t-test: P < 0.001) was applied.
Results:
In gaseous induction group, the number of children who scored severe and very severe distress was greater than those who were in I.V. group. Gaseous induction was used for 23 children. Preoperatively, 56.5% children were in very severe distress, 17.4% in severe distress, 13% in moderate distress, 8.7% in mild distress and only one (4.3%) showed no distress. For I.V. induction, 11.2% children were in very severe distress, 9% in severe distress, and 9.6% in moderate distress, 24.2% in mild distress and 46.1% showed no distress.
Conclusions:
Gaseous induction anesthesia for extractions of teeth does produce high levels of distress than I.V. induction in children for dental extractions. There was no significant difference between both induction methods in terms of distress levels at the time of recovery and 15 min postoperatively.
Keywords: Extraction, dental anxiety, dental phobia, distress
INTRODUCTION
Dental anxiety and fear of dental treatment are considered one of the most disturbing problems, for both the dental team in managing such patients and for the patient. Moreover, dental fear or phobia still considered a major obstacle to the acceptance of dental treatment.[1] This kind of phobic conditions has made management of such patient nearly impossible without the use of general anesthesia (GA). However, the children's experiences of having teeth extracted under GA have been reported recently.[2,3] These were notably negative outcomes of such treatment such as hunger, disturbed eating, being scared/worried and experiencing discomfort from the intravenous (I.V.) cannula. In spite of all these factors, the admission of children in hospitals in the UK for teeth extraction using GA has been increased.[4] The use of sedative drugs may be helpful for the management of anxiety in certain patients.[5]
Considering the increased applications of using GA for the management of such phobic dental patients, removal of teeth in children in the UK will continue to be carried out for the foreseeable future.[6] It is, therefore, important to ensure that the induction of GA and extractions are achieved safely and comfortably. An association among preoperative dental anxiety and apprehension, anesthetic induction distress and postoperative morbidity has been established.[7] Anesthetic induction affects not only children, but it can also cause anxiety and stress in parents. Some parents become very concerned about the procedure.[8]
Kain, et al.,[9] described that extreme anxiety and angst during induction of anesthesia is also related with an increase of these postoperative negative behavioral changes such as nightmares, separation anxiety, and aggression toward authority. It has been reported that children undergoing dental or medical techniques experience fluctuating stages of distress, chiefly in the situation of techniques where the experience may possibly involve pain and invasion of child's psychosomatic, psychological and physical space.[10] The children having a greater incidence of caries and experience of toothache are probably affected by psychological trauma during their treatment under GA (a common treatment solution is extraction of teeth under GA) which in turn leads to a lifetime fretfulness and anxiety about dental treatment.[11] The emotional/sensitive distress generated by a surgical experience is intensified by the severity of post invasive pain.[12] Diminution of distress is seen if the child is prepared before continuing operative procedure. This enhances the child's ability to cope with events which follow unexpected stress which, in turn, is more anxiety provoking and difficult to deal with than anticipated or predictable stress. Furthermore, progenies/kids have a tendency to rely on their guardians and close relatives for help and so as to manage with a fearful condition instead of having their strategies for adapting and coping. Hence suggestively that parent has a significant and essential role to play in backing up their children through traumatic situations.[13]
In summary, the knowledge that a child is in severe pain, and there is nothing that can be done to relieve it is very distressing for the family, and also for medical staff.[14] Morbidity related with the removal of teeth in children treated in GA is standard and has been accounted for as a component creating fear of the dental specialist in later life.[15] Morbidity comprises blood loss; postoperative ache and distress, which can result in disliking dental or medical care.[16] In view of these findings, the present study was planned and designed to investigate whether the type of induction used for GA in children having teeth extraction could play a role controlling the level of distress postoperatively.
SUBJECTS AND METHODS
An informed consent was obtained from all the parents. Patients who were unwilling to take part were excluded. The classification of American Society of Anesthesiology I or II patients who were meeting the selection criteria were recruited for this study: Children aged 2-12 years of age, scheduled for extraction of between 1 and 14 teeth and parents who were ready and willing to cooperate, a proper written up-to-date consent were included in the study. Each child received a weight-dosed volume of analgesic, either paracetamol or ibuprofen as a minimum 1 h before administration of the general anesthetic agent. Topical anesthetic (Emla)® paste (Astra USA, Westborough, MA) to all patients were spread over equally on hands at least 1 h prior to induction. It is a routine clinical exercise. Inside a casualty theatre with a connected recovery chamber/room GA was administered. All children were assigned to I.V. group unless the anesthetists decided that child was unsuitable for I.V. induction. At that point, the child was considered in the gaseous group I induction using proprofol and maintenance of inhalational by means of nitrous oxide, O2 and volatile agent as enflurane remained the standard anesthetic process. The airway was sustained with the laryngeal mask. All teeth were extracted with a minimum of surgical trauma in an uncomplicated fashion. In the operating room, once the exodontia was finished, the patient was moved into the nearby recovery room. As the child started to make progress from the anesthetics, the swab was detached from his/her mouth. Parents were called to come and look after their children. Every single child was noted for signs of suffering and distress and these findings were detailed and documented using the Modified Smiley Faces Scale[17] as shown in Figure 1.
Figure 1.
Five-face scale for assessing distress in children modified smiley faces scale[17]
Evaluation and calculation of distress was made pre-surgically, on retrieval from anesthesia (on sitting up then speaking), and once more after 15 min. The researcher who made all the distress observation was skilled, qualified and entirely independent of the whole process. All data was analyzed using SPSS Statistics for Windows, version 20 (IBM Corp. Armonk, NY).
RESULTS
A total of 212 children were assigned to the study. Eleven children were excluded as they were not fit for GA on that day of surgery (5 children had undiagnosed cardiac ailments, 3 had cold with congested nose as well as trouble in breathing, 1 of the child was weighty and 2 children were exceptionally terrified). The total sample size, therefore, included 201 children.
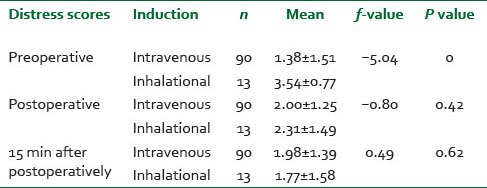
Gaseous induction was used for 23 children. Preoperatively, 13 (56.5%) children were in very severe distress, 4 (17.4%) in severe distress, 3 (13%) in moderate distress, 2 (8.7%) in mild distress and only one (4.3%) showed no distress. However, 178 children with I.V. induction were categorized according to their levels of distress preoperatively into: 20 children were in very severe distress, 16 in severe distress, 17 in moderate distress, 43 in mild distress and 82 showed no distress [Table 1]. The distress levels were also compared at various intervals including preoperatively, postoperatively (at recovery) and 15 min postoperatively [Figure 2]. There were statistically significant differences between the mean distress scores for the I.V. and inhalation groups immediately preoperatively (P values from independent t-test: P < 0.001, [Table 2]). Children who had inhalation type of GA induction scored higher distress scores than those in I.V. group. However, for inhalation group there were no significant differences in mean distress scores at postoperative and 15 min postoperative comparing with the I.V. group (P values from independent t-test: P > 0.05, 0.422, 0.620, [Table 2]).
Table 1.
Preoperative distress assessment for pediatric dental procedures
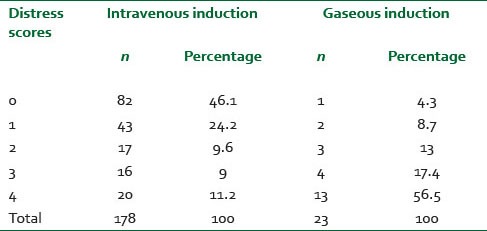
Figure 2.
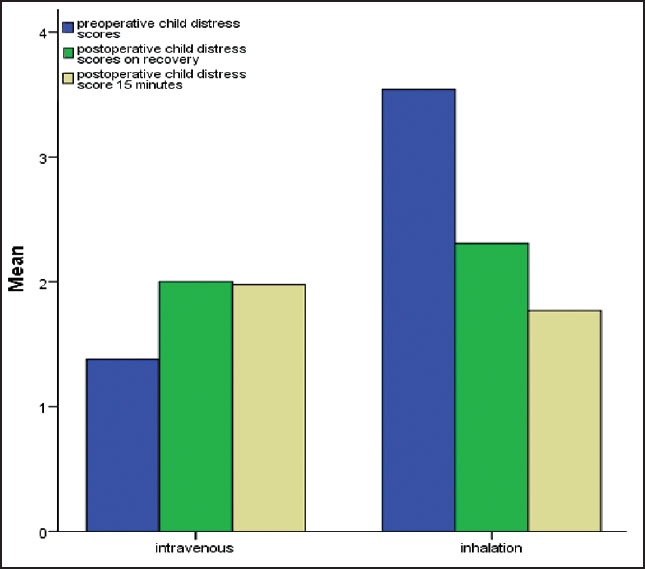
A comparison of preoperative, recovery and postoperative distress scale mean values in child dental patients
Table 2.
Comparisons between mean distress scores for the intravenous and inhalation groups preoperatively, postoperatively and 15 min postoperatively
DISCUSSION
The induction of anesthesia in the children was achieved with either I.V. or a gaseous induction. It is very clear that children who had a gaseous induction were more distressed compared with those who had I.V. induction. Parris et al.,[18] stated that the anxiety is a common emotional reaction to having any surgical procedure and occurs in response to physically threatening situations. Patients undergoing surgery often report the fear, worry, apprehension, and uncertainly. Such feelings are frequently related to anticipate the loss of control and feelings of helplessness. Some patients fear that they may die or never fully recover from the anesthesia; others anticipate significant discomfort and pain following the operations. Finally, Winston concluded from his study that patients who experience elevated levels of anxiety before their surgery are more likely to experience anxiety, as well as physical discomfort, immediately after surgery.
Pediatric patients who are exceptionally anxious might get benefit from pretreatment of the injection area with a topical anesthetic “eutectic mixture of local anesthetics (EMLA)”. Pretreatment reduces the early pain that happens when the needle pricks the skin. In the study children routinely had “EMLA” placed at the clerking session. However, it was detected by the author that the anesthetists were sometimes encountering difficulties with some children who had no clear venous access, and the anesthetists were obliged to do more than one attempt to insert the needle through the skin. This action might have negatively affected the child's psyche especially when the child was anxious, and the anesthetist attempted to give venous access in a vein where there had been no “EMLA” applied to the skin.
The children should always be laid supine to minimize the chance of a vasovagal attack during venipuncture and to maximize the venous return from the extremities.[19] In the theatre, some young children were scared and refused to lie down. Their anxiety made them less likely to respond to the distraction tools used by nurses such as reading books and the children tried to look at the anesthetist while he/she tried to insert the needle. As a consequence, the children became distressed.
Further research
It will be of interest if future research shifts its emphasis to what close relative actually do in the course of the induction of anesthesia instead of simply focusing on their presence and existence. Permitting a relative/parent into an operation theater without significant preparation may be counter-productive because some parent behavior for instance criticism and commands, are associated with increased distress.
This prospective study showed that the I.V. induction for GA is the lesser distress than the gaseous induction before teeth extraction in children (preoperatively). However, the distress levels at the time of recovery and 15 min postoperatively; there was no significant difference between both induction methods.
ACKNOWLEDGMENTS
Authors would like to thank all the anesthetists, dental practitioners, medical caretakers and pediatric staff at the Manchester University Dental Hospital, UK.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Newton JT. Interpreting pain as ‘catastrophic’ makes it worse: The neurological basis. J Dent Res. 2013;92:107–8. doi: 10.1177/0022034512470138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodd H, Hall M, Deery C, Gilchrist F, Gibson BJ, Marshman Z. ‘I felt weird and wobbly.’ Child-reported impacts associated with a dental general anaesthetic. Br Dent J. 2014;216:E17. doi: 10.1038/sj.bdj.2014.333. [DOI] [PubMed] [Google Scholar]
- 3.Thomson WM. Summary of: ‘I felt weird and wobbly.’ Child-reported impacts associated with a dental general anaesthetic. Br Dent J. 2014;216:470–1. doi: 10.1038/sj.bdj.2014.331. [DOI] [PubMed] [Google Scholar]
- 4.Welbury R. Summary of: Why are children still having preventable extractions under general anaesthetic? A service evaluation of the views of parents of a high caries risk group of children. Br Dent J. 2011;210:360–1. doi: 10.1038/sj.bdj.2011.289. [DOI] [PubMed] [Google Scholar]
- 5.Gazal G, Fareed WM, Zafar MS, Al-Samadani KH. Pain and anxiety management for pediatric dental procedures using various combinations of sedative drugs: A review. Saudi Pharm J. 2014 doi: 10.1016/j.jsps.2014.04.004. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atan S, Ashley P, Gilthorpe MS, Scheer B, Mason C, Roberts G. Morbidity following dental treatment of children under intubation general anesthesia in a day-stay unit. Int J Paediatr Dent. 2004;14:9–16. doi: 10.1111/j.1365-263x.2004.00520.x. [DOI] [PubMed] [Google Scholar]
- 7.Hosey MT, Macpherson LM, Adair P, Tochel C, Burnside G, Pine C. Dental anxiety, distress at induction and postoperative morbidity in children undergoing tooth extraction using general anesthesia. Br Dent J. 2006;200:39–43. doi: 10.1038/sj.bdj.4813123. [DOI] [PubMed] [Google Scholar]
- 8.McCann ME, Kain ZN. The management of preoperative anxiety in children: An update. Anesth Analg. 2001;93:98–105. doi: 10.1097/00000539-200107000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Kain ZN, Wang SM, Mayes LC, Caramico LA, Hofstadter MB. Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesth Analg. 1999;88:1042–7. doi: 10.1097/00000539-199905000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Jay SM, Ozolins M, Elliott CH, Caldwell S. Assessment of children's distress during painful medical procedures. Health Psychol. 1983;2:133. [Google Scholar]
- 11.Burns MT, Blinkhorn AS, Asbury AJ. An evaluation of the behaviour of children undergoing dental extraction under general anesthesia. Anesthesia. 1992;47:1073–4. doi: 10.1111/j.1365-2044.1992.tb04208.x. [DOI] [PubMed] [Google Scholar]
- 12.Pendeville PE, Von Montigny S, Dort JP, Veyckemans F. Double-blind randomized study of tramadol vs. paracetamol in analgesia after day-case tonsillectomy in children. Eur J Anaesthesiol. 2000;17:576–82. doi: 10.1046/j.1365-2346.2000.00729.x. [DOI] [PubMed] [Google Scholar]
- 13.Peterson L, Shigetomi C. The use of coping techniques to minimize anxiety in hospitalized children. Behav Ther. 1981;12:1–14. [Google Scholar]
- 14.Eiser C. Psychological effects of chronic disease. J Child Psychol Psychiatry. 1990;31:85–98. doi: 10.1111/j.1469-7610.1990.tb02274.x. [DOI] [PubMed] [Google Scholar]
- 15.Shaw AJ, Meechan JG, Kilpatrick NM, Welbury RR. The use of inhalation sedation and local anesthesia instead of general anesthesia for extractions and minor oral surgery in children: A prospective study. Int J Paediatr Dent. 1996;6:7–11. doi: 10.1111/j.1365-263x.1996.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 16.Al-Bahlani S, Sherriff A, Crawford PJ. Tooth extraction, bleeding and pain control. J R Coll Surg Edinb. 2001;46:261–4. [PubMed] [Google Scholar]
- 17.McGrath PJ, Cunningham SJ, Goodman JT, Unruh A. The clinical measurement of pain in children: A review. Clin J Pain. 1985;1:221–8. [Google Scholar]
- 18.Parris WC, Matt D, Jamison RN, Maxson W. Anxiety and postoperative recovery in ambulatory surgery patients. Anesth Prog. 1988;35:61–4. [PMC free article] [PubMed] [Google Scholar]
- 19.Girdler NM, Hill CM, Wilson KE. UK: Wiley-Blackwell; 2009. Clinical Sedation in Dentistry. [Google Scholar]


