Abstract
Background:
Blood loss is often a major complication in neurosurgery that requires transfusion of multiple units of blood. The purpose of this study was to assess the effect of tranexamic acid (TXA) on intraoperative blood loss and the need for blood transfusion in patients undergoing craniotomy for tumor excision.
Materials and Methods:
A total of 100 patients aged 18-60 years, with American Society of Anesthesiologists physical Status 1 and 2 scheduled to undergo elective craniotomy for tumor excision were enrolled. Patients received 10 mg/kg bolus about 20 min before skin incision followed by 1 mg/kg/h infusion of either TXA or saline. Hemodynamic variables, intravenous fluid transfused, amount of blood loss and blood given were measured every 2 h. Laboratory parameters such as serum electrolytes and fibrinogen values were measured every 3 h. On the 5th postoperative day hemoglobin (POD Hb5), Hb estimation was done and the estimated blood loss (EBL) calculated. Patients were also monitored for any complications.
Results:
The Mean heart rate in TXA group was significantly lower compared with the saline group. Mean arterial pressure and fibrinogen levels were higher in TXA group. The mean total blood loss in the TXA group was less than in the saline group. Blood transfusion requirements were comparable in two groups. The EBL and POD5 Hb were comparable in two groups.
Conclusion:
Even though, there is a significant reduction in the total amount of blood loss in TXA group. However, there was no reduction in intraoperative transfusion requirement.
Keywords: Intraoperative blood loss, neurosurgery, tranexamic acid
INTRODUCTION
Intraoperative blood loss is considered to be one of the major complications in neurosurgical operations and is directly related to the postoperative morbidity and mortality of the patients.[1] The substantial intraoperative bleeding that occurs often needs to be replaced with many units of blood and blood products in addition to the infusion of large volume of crystalloids. However, allogeneic red blood cell transfusion is associated with well-known adverse effects that can range from relatively mild allergic reactions, acidosis, citrate toxicity and hypocalcemia to severe anaphylactic reactions, transfusion associated lung injury, infectious disease transmission, circulatory overload and immunosuppression.[2,3] In addition, administering large amount of replacement fluids in the form of red blood cell or crystalloids are found to dilute the coagulation factors thereby resulting in disorder of coagulation and further increasing the surgical bleeding.[4]
To overcome these problems associated with massive blood loss requiring transfusions, several strategies have been devised and investigated to reduce blood loss and thus the transfusion requirements. These strategies include developing preoperative erythrocyte mass using erythropoietin,[5,6] perioperative blood salvage in the form of preoperative autologous blood donation or intraoperative blood salvage using the cell saver,[7,8] normovolemic hemodilution[9] and controlled hypotension.[10] However none of these techniques are without complications.[11] Complications associated with these techniques and considering the availability and cost-effectiveness, has led to the investigation of alternative hemostatic agents that include aminocaproic acid, tranexamic acid (TXA), desmopressin, aprotinin, and conjugated estrogens.[12]
Tranexamic acid (trans 4 amino methyl cyclohexane carboxylic acid), an antifibrinolytic drug, inhibits the conversion of inactive plasminogen to the active proteolytic enzyme plasmin by competitively blocking of high affinity lysine binding site of plasminogen.[13] This prevents plasmin from binding to fibrinogen and fibrin structures after clot formation.
Tranexamic acid has been successfully used in surgeries with high risk of blood loss such as cardiac, liver, vascular, and orthopedic surgeries.[14,15,16,17] Literature search did not reveal any randomized control trial that had used TXA as a means to reduce blood loss in neurosurgical patients undergoing craniotomy for excision of the tumor. Studies in neurosurgery are uncommon and limited.[18,19] Hence, we designed this study to know the efficacy of TXA in reducing blood loss in craniotomy for tumor excision surgery.
MATERIALS AND METHODS
Institute Review Board and Ethics Committee approved the study. After obtaining written informed consent, 100 patients in the age group of 18-60 years belonging to American Society of Anesthesiologists (ASA) 1 and 2 physical status posted for elective craniotomy for excision of the supratentorial tumor were enrolled for the study. Patients with preexisting renal and hepatic disorders, with bleeding diathesis/abnormal coagulation parameters (abnormal prothrombin time [PT], platelet counts), patient on aspirin or any anticoagulants a week before surgery and patients undergoing intracranial vascular surgeries were excluded from the study. Demographic data such as age, weight, and height were noted. Preoperative investigations that included hemoglobin (Hb), PT-international normalized ratio (INR), serum electrolytes, platelet count, fibrinogen, and hematocrit (Hct) were measured and recorded as the baseline value.
Anesthetic management
In the operation theater, prior to induction of anesthesia, patients were continuously monitored with electrocardiography, non-invasive blood pressure, and pulse oximetry (SpO2). Baseline heart rate (HR), mean arterial pressure (MAP), temperature and SpO2 were recorded. General anesthesia was induced with fentanyl 2 mcg/kg and thiopental 5 mg/kg. Muscle relaxation was achieved with vecuronium 0.1 mg/kg. Monitoring following intubation included end tidal carbon dioxide (EtCO2), invasive blood pressure by cannulating radial artery. Central venous catheter was placed if required. Core temperature was monitored and maintained between 36°C and 37°C. About 20 min before the skin incision, patients were randomly allocated to one of the two groups based on computer generated randomization chart. Group TXA received TXA bolus of 10 mg/kg over a period of 10 min followed by 1 mg/kg/h. Saline group received an equal volume of saline. The patient and the anesthesiologist who performed the case were blinded to the study drug. Anesthesia was maintained with 1 ± 0.2 minimum alveolar concentration of isoflurane in 60% nitrous oxide and oxygen mixture. Ventilator parameters were adjusted to maintain an EtCO2 of 30-33 mmHg. Muscle relaxation was maintained with intermittent doses of vecuronium and morphine in a dose of 0.1 mg/kg was given for analgesia. HR, MAP, SpO2, urine output, temperature were recorded every 2 h. Two senior neurosurgeons, with experience of >10 years, operated on all study cases to avoid surgical technique bias. The infusion of the study drug was stopped at the end of the surgery.
Blood loss assessment and management
Intraoperatively, blood loss was determined from the surgical suction bottles, weighing sponges from the operative field and the volume of blood in surgical drapes. Meticulous care was taken to assess blood loss to avoid any observer bias. Blood loss was measured and recorded every 2 h. We also calculated an estimated blood loss (EBL) of each patient from Hb balance method[20] using blood volume, preoperative and postoperative day 5 Hb (POD5 Hb). In our calculation, one unit of packed cell was considered to contain 50 g of Hb (personal communication with the department of transfusion medicine).
The extravasation of Hb (g) was calculated according to the formula.
Hb loss = (Hb pre-Hbe) × BV + Hbt.
Where,
Hb pre = initial preoperative Hb conc.
Hbe = Hb conc on 5th postoperative day.
Hbt = total amount of allogenic transfused Hb (50 g)
The EBL was calculated using,
EBL (in mL) = 1000 × Hb loss/Hb pre.
Fluid therapy was managed by administration of crystalloid solution and colloid. Adequate replacement and maintenance of intravascular volume was guided by monitoring blood pressure, urine output (≥1 mL/kg/h), and central venous pressure whenever available. The amount of crystalloids and colloid given were recorded every 2 h. A uniform policy for transfusion of blood was followed. Blood was started in accordance with the practice guidelines for blood component therapy: A report by the ASA task force on blood transfusion and adjuvant therapy.[21] Amount of blood transfused in each patient was recorded.
Laboratory parameters
Laboratory parameters that included PT-INR, Hb%, serum, electrolytes, fibrinogen, and platelet count were measured every 3 h.
Postoperative management and follow-up
In the immediate postoperative period, vital parameters were noted and laboratory investigations for postoperative Hb, electrolytes, PT-INR, fibrinogen and platelet count were performed. Patients were either extubated or planned for elective ventilation based on the decision of consultant anesthesiologist. All patients were shifted and managed in neuro-intensive care unit and were followed-up for 5 days. On the 5th POD, Hb and Hct level estimation was done. We assumed the blood volume would normalize by 5th POD. Patients were monitored for any complications like allergic reactions to drug, any clinically evident deep vein thrombosis (DVT) or any other complications. Statistical analysis was carried out using SPSS (SPSS Inc.) statistical software version 16.
Statistical analysis
Statistical analysis was carried out using SPSS statistical software version 16. Patients demographic, clinical and laboratory parameters were recorded. All continuous variables were tested for normality by using Kolmogorov-Smirnov test. Mean with a standard deviation were used to express the normally distributed variables. Patients demographic, clinical and laboratory variables were compared between TXA and saline groups by using Chi-square test for proportions and independent student's t-test for mean values. The number of patients who required blood transfusion was reported as percentages in each group and was compared by using Chi-square test. All statistical analysis was carried out at 5% level of significance and P < 0.05 was considered as statistically significant.
RESULTS
Tranexamic acid, an antifibrinolytic drug is found to decrease blood loss significantly in major orthopedic surgeries and has been proven in a large number of studies. The present study was designed to know the efficacy of TXA in reducing blood loss and intraoperative transfusion requirements in neurosurgical patients undergoing elective craniotomy for tumor excision.
In total 100 neurosurgical patients belonging to ASA 1 and 2 in the age group of 18-60 years undergoing craniotomy were included and randomized into two groups to receive either TXA or saline (50 each).
Demographics
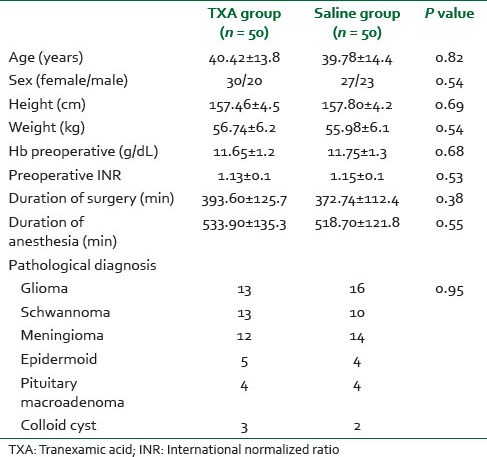
Patient demographic characteristics such as age, weight, and height were comparable in two groups. There were 57 female patients and 43 male patients presented in the study. The mean age of patient was 40.4 ± 13.8 in the TXA group and 39.78 ± 14.4 years in the saline group (P = 0.82). Preoperative Hb and INR were comparable in two groups. The pathological type of tumor of the study subjects was comparable in both the groups. The mean duration of surgery and anesthesia were comparable [Table 1].
Table 1.
Patient characteristics
Hemodynamic parameters
The mean HR at 4, 6, and 8 h in TXA group was significantly less compared to saline group (P < 0.05). The mean HR (bpm) in immediate postoperative period was 88.06 ± 8.5 and 96.74 ± 8.3 in the saline group (P < 0.001) [Graph 1]. MAP was higher in the TXA group compared with the saline group. There was a statistically significant difference in MAP between two groups at 4, 6, 8, and 10 h and immediate postoperative period (P < 0.05) [Graph 2].
Graph 1.
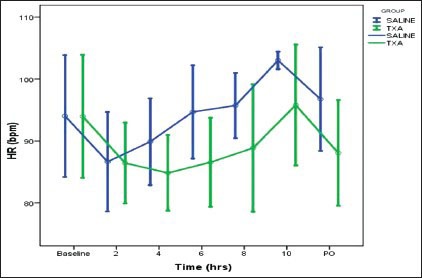
Comparison of heart rate (bpm) in two groups (*P < 0.05). HR significant (P value < 0.05) at 4, 6, 8 and postoperative period
Graph 2.
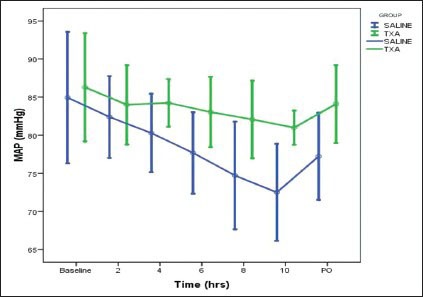
Comparison of mean arterial pressure (mmHg) in two groups (*P < 0.05). MAP significant (P value < 0.05) at 4, 6, 8, 10 hours and post operative period
Perioperative blood loss and intravenous fluid management
Fluid input and output were comparable between the groups. There was no significant difference in crystalloid or colloid given or blood transfused in two groups. However, the total blood loss between the groups showed a statistically significant difference (P = 0.012) [Table 2].
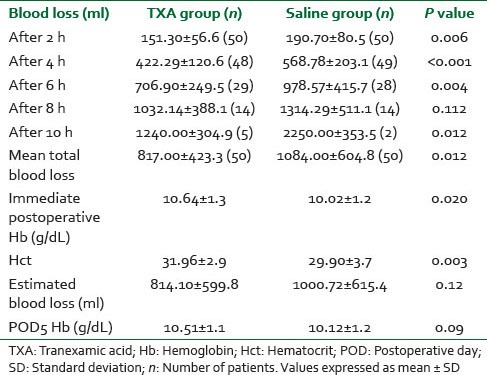
Table 2.
Comparison of perioperative blood loss and intravenous fluid management in two groups
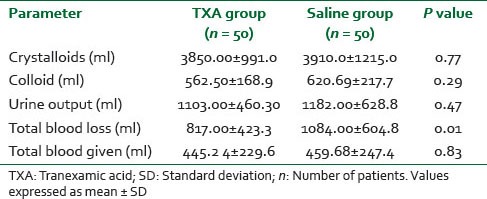
There was a statistically significant difference in blood loss between two groups after 2, 4, 6, and 8 h (P < 0.05). The mean total blood loss in the TXA group was 817.00 ± 423.3 mL and 1084.00 ± 604.8 mL in the saline group (P = 0.012) [Table 3]. Of 100 patients, 21 patients in TXA group and 30 patients in saline group received blood transfusions, which were comparable in two groups (P = 0.109).
Table 3.
Comparison of perioperative blood loss (ml) and Hct in two groups
Laboratory parameters
Serum electrolytes
Serum sodium, potassium, and calcium were measured at 3, 6, 9 h and immediate postoperative period and it was found that there was no difference in the two groups.
Fibrinogen
Baseline fibrinogen level between two groups was comparable. Fibrinogen levels were significantly higher in TXA group compared to saline group at 3, 6 and 9 h (P < 0.05). In the immediate postoperative period, the fibrinogen level in TXA group was 370.6 ± 57.1 mg/dL and 308.2 ± 69.4 mg/dL in the saline group (P < 0.001) [Graph 3].
Graph 3.
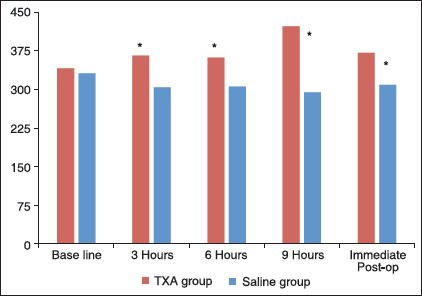
Comparison of fibrinogen (mg/dL) in two groups (*P < 0.05)
Others
In the immediate postoperative period, Hb in the TXA group was 10.64 ± 1.3 whereas in the saline group was 10.02 ± 1.2 (P = 0.02). Comparison of postoperative Hct showed a significant difference between two groups (P = 0.003). The EBL and POD5 were comparable (P = 0.09) [Table 3].
DISCUSSION
Intraoperative hemorrhage in neurosurgery often requires substantial intraoperative blood transfusion. Transfusion of homologous blood and blood products subjects patients to risks of infectious disease transmission, transfusion reaction, and immunosuppression.[2,3] Furthermore, replacement of massive intraoperative bleeding (>50% TBV) with crystalloids and packed erythrocytes during the surgery can dilute the coagulation factors and further increase surgical bleeding.[4]
Several strategies to reduce blood loss and transfusion requirements have been investigated.[5,6,7,8,9,10] However, none of these techniques are free of complications and the most important factor to consider would be the availability and cost effectiveness in use of these strategies. Hemodilution and controlled hypotension may compromise tissue oxygen delivery during rapid blood loss.[11]
Tranexamic acid (trans 4 amino methyl cyclohexane carboxylic acid), an antifibrinolytic drug inhibits the conversion of inactive plasminogen to the active proteolytic enzyme plasmin by competitively blocking of high affinity lysine binding site of plasminogen.[13] This prevents plasmin from binding to fibrinogen and fibrin structures after clot formation.
We randomized 100 neurosurgical patients undergoing craniotomy to receive either TXA or placebo. TXA was given in a dose of 10 mg/kg bolus followed by 1 mg/kg/h throughout the duration of surgery in the TXA group and an equal volume of saline in the control group. This dose is similar to dosage regimens used by Wong et al.[22] and Kim and Bae[23] in patients undergoing spinal fusion surgery. The same dose was utilized in our study to evaluate the efficacy of TXA in reducing intraoperative blood loss. The dose of TXA used by Sethna et al. in pediatric patients undergoing scoliosis surgery[24] was much higher compared to our study.
Patient demographic characteristics were comparable in two groups. The mean age of patients in TXA group was 40.4 ± 13.8 in the TXA group and 39.78 ± 14.4 years in saline group (P = 0.82). The mean height and weight were comparable in two groups. Patients in two groups were also similar in preoperative laboratory variables (Hb and INR). There was no significant difference between the groups in terms of duration of surgery or anesthesia.
After the start of surgery 2 hourly recording of clinical parameters were performed which included HR, MAP, SpO2, blood loss, blood given and amount of intravenous (IV) fluid transfused. We found that the mean HR in TXA group was significantly lower compared with the saline group at 4, 6 and 8 h. The mean HR in immediate postoperative period was 88.06 ± 8.5 in TXA acid group and 96.74 ± 8.3 in the saline group (P < 0.001). Similarly, the MAP remained high in TXA group as compared to the saline group (P < 0.05). This difference could probably be explained by action of TXA that reduced blood loss and thus maintained a better hemodynamics in TXA group. In a study by Goobie et al.[19] tranexamic acid was used to reduce perioperative blood loss in children undergoing craniosynostosis surgery. In contrast to our study, they found the measured HR, systolic blood pressure, diastolic blood pressure and MAP to be comparable between the two groups.
Although visual estimation of blood loss is considered imprecise,[25] it continues to be the easiest, cost free, acquirable and most practiced method of blood loss estimation. It has been used in a large number of studies as a means of measuring blood loss and evaluating the need for blood transfusion.[16,22,26,27] Blood loss was determined intraoperatively from surgical suction bottles, weighing sponges from the operative field and the volume of blood in surgical drapes. Utmost care was taken in assessing blood loss to avoid any observer bias. We found a significant reduction in blood loss in the TXA group compared to saline group at 2, 4, and 6 h of surgery (P < 0.05). At the end of 8 h, though blood loss was less in TXA group compared to saline group, it was not statistically significant. This could partially be explained by the fact that fibrinolytic activation is a cascade process that is most easily inhibited in its earlier phase and has little effect when heavy blood loss has already occurred.[27]
The mean total blood loss in TXA group was 817.00 ± 423.3 and 1084.00 ± 604.8 mL in the saline group (P = 0.012). Our finding of reduced blood loss with TXA is consistent with previous randomized trials in a large number of orthopedic[28,29] (Spine, total hip replacement, total knee replacement), craniosynostosis[19] and obstetrics.[30]
A uniform transfusion policy was followed in our study to avoid any transfusion bias. Blood was started in accordance with the practice guidelines for blood component therapy: A report by the ASA task force on blood transfusion and adjuvant therapy.[21]
Although prevention of allogenic blood transfusion was not the primary outcome of our study, we performed an analysis to determine the potential benefit conferred by TXA. It was found that the administration of TXA did not seem to reduce the incidence of allogenic blood transfusion. TXA group patients received 445.2 4 ± 229.6 mL of blood whereas it was 459.68 ± 247.4 mL in the saline group. However, the number of patients who received blood in the TXA group was less compared with the saline group. Out of 100 patients, 21 patients in TXA group and 30 in saline group received transfusion (P = 0.109). Our findings were similar to a study done by Wong et al. in patients undergoing spinal fusion surgery.[22] Sethna et al.[24] also found TXA to significantly reduce blood loss in pediatric patients undergoing scoliosis surgery (P < 0.01), but the amount of blood transfused did not differ between groups. The reason for no reduction in blood transfusion requirements could probably be because of TXA that was used at a low dose in our study. In contrast, Goobie et al.[19] had used a higher dose (50 mg/kg and 5 mg/kg/h) and thus found a significant reduction in the amount of blood transfused (P < 0.01).
Fluid therapy was managed by administration of crystalloids and colloid. Decision regarding adequate replacement and maintenance of intravascular volume was guided by monitoring blood pressure and urine output. There was no difference in the total amount of IV fluids transfused between the two groups, which were similar to study by Neilipovitz et al.[16] where total volume of crystalloids and colloids did not differ between the groups.
Laboratory parameters were recorded every 3 h and included Hb, PT-INR, platelet count, serum electrolytes and fibrinogen levels. We found fibrinogen levels to be significantly higher in the TXA group at 3, 6 and 9 h followed by immediate postoperative period. This occurs probably due to the action of TXA that inhibits fibrinolysis activation by blocking the conversion of inactive plasminogen to plasmin. This prevents plasmin from binding to fibrinogen and fibrin structures thus increasing the concentration of fibrinogen. Our findings were similar to study by Jansen et al.[27] in patients undergoing total knee arthroplasty in which coagulation and fibrinolysis values were measured before administration and 8 h after the end of surgery and 24, 72 h after the operation. TXA treated patients showed increased fibrinogen concentration. In contrast, Wong et al.[22] demonstrated no difference in coagulation profile, including fibrinogen levels between TXA and placebo group.
Serum electrolytes were comparable both preoperatively and intraoperatively at various time points. In the immediate postoperative period, patients in the TXA group had higher postoperative Hb and Hct levels than the saline group. This could be due to the reduction in blood loss by TXA and thus better hemodynamics. Results were similar to that found by Wong et al.[22] who had studied the effect of TXA in 151 adult patients undergoing spinal fusion surgery and found the postoperative Hb to be significantly higher in the TXA group.
In our study, in addition to visual estimation of blood loss, we also calculated an EBL of each patient from Hb balance method using blood volume, preoperative and POD5 Hb.[20] EBL showed no difference in two groups in our study. This was similar to EBL compared between two groups who received epsilon-aminocaproic acid and placebo by Cardenas et al.[31] who found the difference in calculated blood loss between two groups were not significant. This is because of the variability in fluid status of an individual who was influenced by intravascular volume, shift of fluid to third space, fluids given, and urine output. Patients were clinically assessed daily for occurrence of any adverse effects or clinical symptoms of DVT. Similar to previous studies,[16,32] no patient in the study experienced a complication directly attributable to the use of TXA.
A limitation of our study is the assessment of intraoperative blood loss, which was susceptible to interobserver variability and bias. TXA was used at a low dose in our study that could probably be a reason for no reduction in blood transfusion requirements. Future dose ranging studies are necessary to determine the dose dependent benefits of TXA.
CONCLUSION
The administration of TXA in a low dose resulted in a significant reduction in blood loss with better intraoperative hemodynamics. The fibrinogen levels were higher in patients who received TXA. However, there was no reduction in intraoperative blood transfusion requirements.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Deogaonkar A, De Georgia M, Mascha E, Todd M, Schubert A IHAST Investigators. Intraoperative blood loss is associated with worse outcome after aneurysmal subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2006;18:302–3. [Google Scholar]
- 2.Marcucci C, Madjdpour C, Spahn DR. Allogeneic blood transfusions: Benefit, risks and clinical indications in countries with a low or high human development index. Br Med Bull. 2004;70:15–28. doi: 10.1093/bmb/ldh023. [DOI] [PubMed] [Google Scholar]
- 3.Soldan K, Barbara J. The risks of infection transmission by blood transfusion in England. J Clin Pathol. 1999;52:405–8. doi: 10.1136/jcp.52.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray DJ, Pennell BJ, Weinstein SL, Olson JD. Packed red cells in acute blood loss: Dilutional coagulopathy as a cause of surgical bleeding. Anesth Analg. 1995;80:336–42. doi: 10.1097/00000539-199502000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Fearon JA, Weinthal J. The use of recombinant erythropoietin in the reduction of blood transfusion rates in craniosynostosis repair in infants and children. Plast Reconstr Surg. 2002;109:2190–6. doi: 10.1097/00006534-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Meneghini L, Zadra N, Aneloni V, Metrangolo S, Faggin R, Giusti F. Erythropoietin therapy and acute preoperative normovolaemic haemodilution in infants undergoing craniosynostosis surgery. Paediatr Anesth. 2003;13:392–6. doi: 10.1046/j.1460-9592.2003.01091.x. [DOI] [PubMed] [Google Scholar]
- 7.Dahmani S, Orliaguet GA, Meyer PG, Blanot S, Renier D, Carli PA. Perioperative blood salvage during surgical correction of craniosynostosis in infants. Br J Anesth. 2000;85:550–5. doi: 10.1093/bja/85.4.550. [DOI] [PubMed] [Google Scholar]
- 8.Deva AK, Hopper RA, Landecker A, Flores R, Weiner H, McCarthy JG. The use of intraoperative autotransfusion during cranial vault remodeling for craniosynostosis. Plast Reconstr Surg. 2002;109:58–63. doi: 10.1097/00006534-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Hans P, Collin V, Bonhomme V, Damas F, Born JD, Lamy M. Evaluation of acute normovolemic hemodilution for surgical repair of craniosynostosis. J Neurosurg Anesthesiol. 2000;12:33–6. doi: 10.1097/00008506-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Rosenblatt MA. Strategies for minimizing the use of allogeneic blood during orthopedic surgery. Mt Sinai J Med. 2002;69:83–7. [PubMed] [Google Scholar]
- 11.Kuppurao L, Wee M. Perioperative cell salvage. Contin Educ Anaesth Crit Care Pain. 2010;10:104–8. [Google Scholar]
- 12.Erstad BL. Systemic hemostatic medications for reducing surgical blood loss. Ann Pharmacother. 2001;35:925–34. doi: 10.1345/aph.10337. [DOI] [PubMed] [Google Scholar]
- 13.Dunn CJ, Goa KL. Tranexamic acid: A review of its use in surgery and other indications. Drugs. 1999;57:1005–32. doi: 10.2165/00003495-199957060-00017. [DOI] [PubMed] [Google Scholar]
- 14.Faraoni D, Willems A, Melot C, De Hert S, Van der Linden P. Efficacy of tranexamic acid in paediatric cardiac surgery: A systematic review and meta-analysis. Eur J Cardiothorac Surg. 2012;42:781–6. doi: 10.1093/ejcts/ezs127. [DOI] [PubMed] [Google Scholar]
- 15.Aguilera X, Videla S, Almenara M, Fernandez JA, Gich I, Celaya F. Effectiveness of tranexamic acid in revision total knee arthroplasty. Acta Orthop Belg. 2012;78:68–74. [PubMed] [Google Scholar]
- 16.Neilipovitz DT, Murto K, Hall L, Barrowman NJ, Splinter WM. A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg. 2001;93:82–7. doi: 10.1097/00000539-200107000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Elwatidy S, Jamjoom Z, Elgamal E, Zakaria A, Turkistani A, El-Dawlatly A. Efficacy and safety of prophylactic large dose of tranexamic acid in spine surgery: A prospective, randomized, double-blind, placebo-controlled study. Spine (Phila Pa 1976) 2008;33:2577–80. doi: 10.1097/BRS.0b013e318188b9c5. [DOI] [PubMed] [Google Scholar]
- 18.CRASH-2 Collaborators, Intracranial Bleeding Study. Effect of tranexamic acid in traumatic brain injury: A nested randomised, placebo controlled trial (CRASH-2 Intracranial Bleeding Study) BMJ. 2011;343:d3795. doi: 10.1136/bmj.d3795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goobie SM, Meier PM, Pereira LM, McGowan FX, Prescilla RP, Scharp LA, et al. Efficacy of tranexamic acid in pediatric craniosynostosis surgery: A double-blind, placebo-controlled trial. Anesthesiology. 2011;114:862–71. doi: 10.1097/ALN.0b013e318210fd8f. [DOI] [PubMed] [Google Scholar]
- 20.Johansson T, Engquist M, Pettersson LG, Lisander B. Blood loss after total hip replacement: A prospective randomized study between wound compression and drainage. J Arthroplasty. 2005;20:967–71. doi: 10.1016/j.arth.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 21.American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Practice Guidelines for Perioperative Blood Transfusion and Adjuvant Therapies: An Updated Report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology. 2006;105:198–208. doi: 10.1097/00000542-200607000-00030. [DOI] [PubMed] [Google Scholar]
- 22.Wong J, El Beheiry H, Rampersaud YR, Lewis S, Ahn H, De Silva Y, et al. Tranexamic acid reduces perioperative blood loss in adult patients having spinal fusion surgery. Anesth Analg. 2008;107:1479–86. doi: 10.1213/ane.0b013e3181831e44. [DOI] [PubMed] [Google Scholar]
- 23.Kim MO, Bae SW. Tranexamic acid versus a placebo in decreasing blood loss in patients undergoing spine surgery. Korean J Anesthesiol. 2000;39:645–50. [Google Scholar]
- 24.Sethna NF, Zurakowski D, Brustowicz RM, Bacsik J, Sullivan LJ, Shapiro F. Tranexamic acid reduces intraoperative blood loss in pediatric patients undergoing scoliosis surgery. Anesthesiology. 2005;102:727–32. doi: 10.1097/00000542-200504000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Meiser A, Casagranda O, Skipka G, Laubenthal H. Quantification of blood loss. How precise is visual estimation and what does its accuracy depend on? Anesthesist. 2001;50:13–20. doi: 10.1007/s001010050957. [DOI] [PubMed] [Google Scholar]
- 26.Ekbäck G, Axelsson K, Ryttberg L, Edlund B, Kjellberg J, Weckström J, et al. Tranexamic acid reduces blood loss in total hip replacement surgery. Anesth Analg. 2000;91:1124–30. doi: 10.1097/00000539-200011000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Jansen AJ, Andreica S, Claeys M, D’Haese J, Camu F, Jochmans K. Use of tranexamic acid for an effective blood conservation strategy after total knee arthroplasty. Br J Anesth. 1999;83:596–601. doi: 10.1093/bja/83.4.596. [DOI] [PubMed] [Google Scholar]
- 28.Dhillon MS, Bali K, Prabhakar S. Tranexamic acid for control of blood loss in bilateral total knee replacement in a single stage. Indian J Orthop. 2011;45:148–52. doi: 10.4103/0019-5413.77135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Claeys MA, Vermeersch N, Haentjens P. Reduction of blood loss with tranexamic acid in primary total hip replacement surgery. Acta Chir Belg. 2007;107:397–401. doi: 10.1080/00015458.2007.11680081. [DOI] [PubMed] [Google Scholar]
- 30.Sekhavat L, Tabatabaii A, Dalili M, Farajkhoda T, Tafti AD. Efficacy of tranexamic acid in reducing blood loss after cesarean section. J Matern Fetal Neonatal Med. 2009;22:72–5. doi: 10.1080/14767050802353580. [DOI] [PubMed] [Google Scholar]
- 31.Cardenas R, Wadhwa R, Haydel J, Nanda A, Rao A, Caldito G. Pre-operative amicar (epsilon-aminocaproic acid): Does it reduce total blood loss in lumbar pedicle screw spinal fusion? Internet J Neurosurg. 2010;7:3. [Google Scholar]
- 32.Gillette BP, DeSimone LJ, Trousdale RT, Pagnano MW, Sierra RJ. Low risk of thromboembolic complications with tranexamic acid after primary total hip and knee arthroplasty. Clin Orthop Relat Res. 2013;471:150–4. doi: 10.1007/s11999-012-2488-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


