Abstract
Context
Bystander cardiopulmonary resuscitation (CPR) improves the likelihood of surviving out-of-hospital cardiac arrest (OHCA), yet treatment rates differ by a community’s racial and income composition.
Objective
To determine if CPR training differs by the race and income of communities across the United States (U.S.).
Design, Setting, and Participants
We analyzed county-level CPR training rates from 2010–2011 using CPR training data from the American Heart Association, the American Red Cross, and the Health and Safety Institute. We utilized multivariable logistic regression models to examine the association of annual adult CPR training rates with a county’s proportion of black residents and median household income (categorized as tertiles), as well as other demographic, geographic, and healthcare characteristics.
Main Outcome Measure
CPR training rate.
Results
From 07/01/2010–06/30/2011, 13.1 million persons in 3143 U.S. counties received CPR training. The median county training rate ranged from 0.00%–1.29% (median=0.51%) in the lower tertile, 1.29%–4.07% (median=2.39%) in the middle tertile, and >4.07% (median=6.81%) in the upper tertile. Counties that were most likely to have CPR training rates in the lower tertile included those with a higher proportion of rural (odds ratio [OR] 1.12, 95% confidence interval [CI] 1.10, 1.15 per 5 percentage point [PP] change), black (OR 1.09, 95% CI 1.06, 1.13 per 5 PP change), and Hispanic residents (OR 1.06, 95% CI 1.02, 1.11 per 5 PP change); those with a lower median household income (OR 1.18, 95% CI 1.04, 1.34 per $10,000 decrease); those with a higher median age (OR 1.28, 95% CI 1.04, 1.53 per 10 year change); and those located in the South.
Conclusions
Counties with a higher proportion of rural, black, Hispanic, and lower income residents had lower CPR training rates. Differences in CPR training by race and income may contribute to recognized disparities in bystander CPR treatment and OHCA survival, and offer opportunities for future community interventions.
Keywords: out-of-hospital cardiac arrest, cardiopulmonary resuscitation training rates, racial disparities, income disparities
More than 350,000 Americans experience out-of-hospital cardiac arrest (OHCA) each year.1 In most United States (U.S.) communities, overall survival has remained 7%–9% per year for the past thirty years.2–5 Significant racial, ethnic, and socioeconomic disparities exist for OHCA incidence, treatment, and outcomes for individuals and communities.2,6–11 Early use of bystander cardiopulmonary resuscitation (CPR) is critical to surviving OHCA, but its use varies significantly from 10%–65% in observational cohorts.2,4,12–14 Blacks7,15 and low income individuals9,12 with OHCA are significantly less likely to receive bystander CPR. Furthermore, people with an OHCA event that occurs in predominantly black low income neighborhoods are the least likely group to receive bystander CPR treatment, compared with other racial and income neighborhood groups.14 A recent American Heart Association (AHA) consensus statement called for an increase in bystander CPR training among communities.16 Currently, very little is known about CPR training patterns in the U.S., but this information could be invaluable for understanding how to increase bystander CPR rates.
We believe our study is the first to use unique data from several major U.S. CPR training programs, sponsored by the AHA, the American Red Cross (ARC), and the Health and Safety Institute (HSI), to examine patterns of annual CPR training in the U.S. We also examined the degree to which county demographic, geographic, and healthcare factors were associated with low CPR training rates. We hypothesized that CPR training rates would be significantly lower among communities with a greater proportion of black and low income residents.
METHODS
Data Sources
For this study, we utilized data from the AHA, ARC, and HSI to determine CPR training rates throughout the U.S. To access this information, data use agreements were obtained according to Duke University research practices. Training data from the AHA, which were available at the county-level, were based on course completion cards and community CPR products sold in the U.S. Since 97% of the AHA training data were course completion cards that are distributed to a single individual (for advance cardiac life support [ACLS], pediatric advanced life support [PALS], basic life support [BLS], or HeartSaver [workplace training]), we assumed one card sold equated to one person trained. The AHA also has two community-based CPR products: (1) the Family and Friends CPR Course; and (2) the Family & Friends® CPR Anytime® Personal Learning Program (a home training kit). For the Family and Friends CPR Course, a book is distributed to participants; therefore, we assumed that one book sold equated to one person trained. For the Family & Friends CPR Anytime Personal Learning Program, a training kit is provided; it is estimated that 2.5 persons are trained per kit. As a result, the AHA standardly applies a multiplier of 2.5 to each kit sold in order to estimate regional training.17,18
The ARC database tracks persons trained in CPR; these data are collected by 616 regional offices, are maintained by the National Headquarters (http://www.redcross.org/find-your-local-chapter), are available at the zip code-level, and are largely divided by professional (CPR/Automated External Defibrillator [AED] for Professional Rescuer and Health Care Provider) versus lay (First Aid/CPR/AED) rescuer programs. The professional program provides BLS training, whereas the lay rescuer program provides certification for the work place and for lay responders who require certification.
Data that we obtained from HSI were based on product sales data distributed to regions in the U.S. The HSI is comprised of two training companies: the American Health and Safety Institute and Medic FirstAid. All HSI products are based on certification cards; therefore, we assumed that one product sold equated to one person trained. Training is based on lay person BLS, PALS, and ACLS certifications. The lay training program is largely based on workplace training. These data were available at the zip code-level.
For the primary analysis, we assumed that persons trained in ACLS or PALS concomitantly received BLS training in the same year, so in order to limit the chances of a single individual’s training being counted twice, we excluded ACLS and PALS training provided by the AHA and HSI. We did not apply these exclusions to the ARC, since BLS training is the most advanced level of training offered by this organization. To account for alternate possibilities, we performed a sensitivity analysis, which included the entire dataset of ACLS and PALS.
County-level demographic, geographic, and healthcare information were obtained from the Area Resource File19, the 2010 Decennial Census, and the Centers for Disease Control. Similar to Census data, Area Resource File data were not collected in the same year (e.g., percent rural data were collected in the year 2000, hospital data in 2007, and physician data in 2008).
Definitions
Cardiopulmonary resuscitation training rates for each county were calculated as the estimated number of residents trained by the AHA, ARC, and the HSI, divided by the overall county population that was between 15 and 80 years of age. We chose this age group in order to exclude children and the elderly, as they would not typically be targets of CPR educational programs. We considered all counties in each of the 50 U.S. states, as well as Washington, DC. We excluded counties in Puerto Rico and the U.S. Virgin Islands. We also excluded AHA and ARC training data that could not be mapped to a specific county or zip code (13.1% of the dataset).
Statistical Analysis
We defined tertiles by consecutively ordering counties (based on CPR training rates) from the lowest to highest. We then grouped our findings into three tertiles (lower, middle, and upper). A chloropelth map was created using county-level concentrations of CPR training by tertiles.
We compared county-level characteristics across tertiles. A Pearson χ2 test was used for all categorical variables; a Wilcoxon Rank Sum test was used for continuous and ordinal variables. To account for outliers, counties with CPR training rates >15% were truncated at 15% (3.3% of the primary analysis dataset)—the point at which only a few counties were represented in each training rate category. This cut-point was determined after examining the training rate histogram.
Logistic regression modeling was used to determine if black race and median household income were associated with counties in the lower tertile of CPR training rates. Other variables included in the analysis were sex, age, race (aside from black) and ethnicity, percent education attainment, percent rural population, heart disease mortality, number of physicians, and region. Poverty and geographic densities were not included in the final model due to high correlation to median household income and rural population, respectively. Rate and income variables in the regression analysis were modeled continuously and are reported by percentage point change in variable, which was defined as the arithmetic (absolute) difference between two percentages. A Wald χ2 test was used to determine the strength of each variable’s association with the outcome. Missing rates for each variable included in the model were minimal (<0.3%). Missing values were imputed as the group-specific median. The primary analysis was performed without accounting for ACLS and PALS training (as discussed previously); the secondary sensitivity analysis included all CPR training.
All statistical tests were two-sided, with a p-value of 0.05 indicating statistical significance. Analyses were performed using SAS 9.2 (SAS Institute, Cary, NC) and ArcGIS 10 (Esri, Redlands, CA)
RESULTS
Our analysis included CPR training data from 3143 counties in the U.S. (i.e., 100% of all U.S. counties). An estimated 13,123,113 persons received CPR training between July 1, 2010 and June 30, 2011. The AHA provided training to 8,293,401 persons (63.2% of all trained); of which, 55.6% was BLS training, 40.0 % was Heart Saver training, and 4.4% was Friends and Family training. The ARC provided training to 3,638,169 persons (27.7% of all trained); of which, 80.4% were lay rescuers and 19.6% were professionals. The HSI provided training to 1,191,543 persons (9.1% of all trained); of which, 17.9% was BLS training and 82.1% was lay/workplace training.
The median annual CPR training rate in our cohort for all U.S. counties was 2.39% (25th and 75th percentiles: 0.88 and 5.31) and ranged from 0.00%–1.29% (median = 0.51%) in the lower tertile counties, 1.29%–4.07% (median = 2.39%) in the middle tertile counties, and >4.07% (median = 6.81%) in the upper tertile counties. Of those counties in the lower tertile of CPR training, 57.0% were located in the Southern U.S. (Table 1). As illustrated by the Figure, there is substantial and important geographic variability in CPR training across the country.
Table 1.
Characteristics of U.S. Counties by Tertiles of CPR Training Rates
| Overall N=3143 |
Lower Tertile N=1047 |
Middle Tertile N=1048 |
Upper Tertile N=1048 |
p-value | |
|---|---|---|---|---|---|
| Baseline characteristics a | |||||
| Population density (persons per sq. mile) |
42.8 (16.5, 107.6) |
24.0 (7.7, 46.7) |
44.1 (20.0, 96.6) |
92.7 (32.8, 282.1) |
<0.001 |
| Percent white | 89.1 (75.2, 95.5) |
89.1 (72.6, 96.3) |
90.4 (78.2, 96.0) |
87.8 (74.9, 94.1) |
0.001 |
| Percent black | 2.0 (0.5, 10.2) |
1.3 (0.3, 15.0) |
1.7 (0.5, 7.1) |
2.8 (0.8, 9.8) |
<0.001 |
| Percent Hispanic | 3.3 (1.6, 8.2) |
2.5 (1.4, 6.2) |
3.2 (1.6, 8.5) |
4.1 (2.0, 9.5) |
<0.001 |
| Percent Asian | 0.5 (0.3, 1.0) |
0.3 (0.2, 0.5) |
0.5 (0.3, 1.0) |
0.9 (0.5, 2.1) |
<0.001 |
| Percent male | 49.5 (48.9, 50.4) |
49.7 (49.0, 50.7) |
49.6 (49.0, 50.3) |
49.4 (48.7, 50.1) |
<0.001 |
| Age, years | 40.3 (37.4, 43.4) |
41.4 (38.9, 44.8) |
40.4 (37.6, 43.4) |
39.3 (36.1, 41.9) |
<0.001 |
| Percent rural population | 60.4 (35.8, 90.2) |
82.8 (60.3, 100.0) |
60.7 (38.8, 82.3) |
38.6 (18.0, 60.0) |
<0.001 |
| Percent college degree, % | 14.5 (11.2, 19.3) |
12.1 (10.0, 15.4) |
14.4 (11.3, 18.8) |
17.7 (13.7, 24.8) |
<0.001 |
| Median household income, $ | 42,390 (36,518, 49,241) |
38,087 (33,551, 43,693) |
43,358 (37,630, 50,332) |
45,267 (40,135, 52,386) |
<0.001 |
| Percent in poverty | 14.3 (10.9, 18.3) |
16.3 (12.3, 21.0) |
13.5 (10.6, 17.8) |
13.5 (10.4, 16.7) |
<0.001 |
| Number of physicians | 20.0 (5.0, 93.0) |
6.0 (2.0, 15.0) |
22.0 (7.0, 76.0) |
94.0 (24.5, 405.5) |
<0.001 |
| Heart disease mortality rate (persons per 100,000) |
197.4 (170.6, 228.9) |
208.0 (176.2, 246.4) |
195.8 (170.6, 226.1) |
191.2 (164.4, 215.4) |
<0.001 |
| Region, % | <0.001 | ||||
| West | 14.3 | 11.1 | 14.4 | 17.3 | |
| South | 45.3 | 57.0 | 43.9 | 34.9 | |
| Midwest | 33.6 | 31.1 | 34.6 | 34.9 | |
| Northeast | 6.9 | 0.8 | 7.1 | 12.9 |
Abbreviations: CPR, cardiopulmonary resuscitation; sq, square; U.S., United States
For all variables, except region, medians and 25th and 75th percentiles (in parentheses) are reported. Each race and ethnicity were collected independently via U.S. Census and represent the percentage of persons within the county. Percentages will not sum to 100%.
Figure. Geographic Distribution of Counties by CPR Training Tertile in the United States Community CPR Training Cohort.
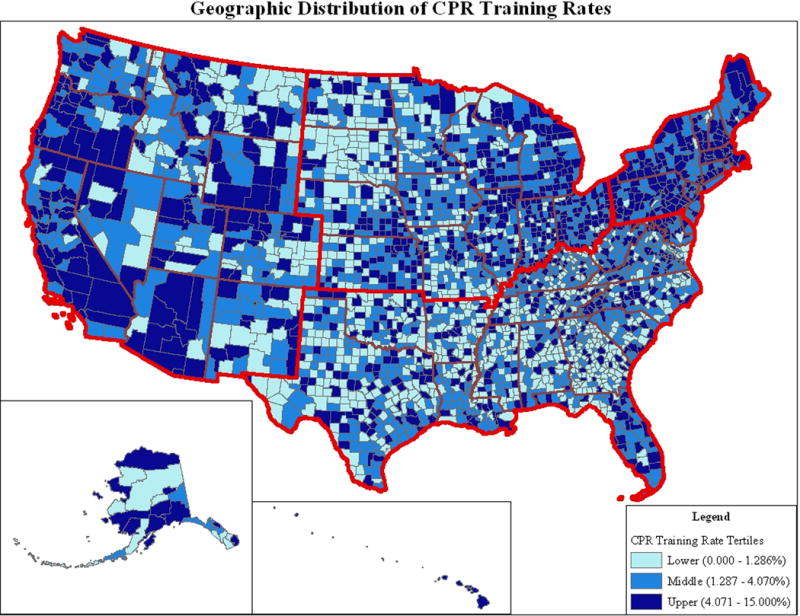
This map shows the CPR training tertile for each county in the United States. Light blue represents lower tertile counties with CPR training rates ranging from 0.00 to 1.29% (median = 0.39%). Medium blue represents middle tertile counties with training rates ranging from 1.29 to 4.07% (median = 2.39%). Dark blue represents upper tertile counties with CPR training rates >4.07% (median = 6.81%).
Using univariable analyses, we compared counties in the lower tertile of CPR training rates with counties in the middle and upper tertiles. We found that counties in the lower tertile had a lower median percentage of blacks (1.3% vs. 2.2%, p<0.001) and Hispanics (2.5% vs. 3.7%, p<0.001), a greater proportion of rural populations (median = 82.8% vs. 49.5%, p<0.001), and a lower median household income (median = $38,087 vs. $44,362, p<0.001). In addition, lower tertile counties had a significantly lower median percentage of residents having at least a college degree, a higher median percentage of residents living in poverty, lower population densities, significantly fewer physicians and hospitals, and higher heart disease mortality rates (Table 1).
After multivariable adjustment, several factors remained independently associated with counties in the lower tertile (Table 2), with the strongest factor being the proportion of rural residents in a given county. For every 5 percentage point increase in the rural population composition, the odds of being in a lower tertile county increased (odds ratio [OR] 1.12; 95% confidence interval [CI] 1.10, 1.15, χ2=106.8. Race and ethnicity were also strongly associated with counties in the lower tertile for CPR training. For every 5 percentage point increase in the proportion of black race or Hispanic ethnicity residents, the adjusted OR of being in a lower tertile county was 1.09 (95% CI 1.06, 1.13; χ2=23.78) and 1.06 (95% CI 1.02, 1.11; χ2=9.23), respectively. Finally, counties with lower median household incomes were significantly more likely to be in the lower tertile for CPR training. For every $10,000 decrease in median household income, the adjusted OR of being in the lower tertile was 1.18 (95% CI 1.04, 1.34; χ2=6.68). Other factors associated with the lower tertile for CPR training were counties located in the South, median age, and number of physicians (Table 2).
Table 2.
Factors Associated with a County Being in the Lower Tertile of CPR Training
| Variable | OR (95% CI) | Chi Square | p-value |
|---|---|---|---|
| Percent rural (per 5 PP increase) | 1.12 (1.10, 1.15) | 106.85 | <0.001 |
| Region | 32.43 | <0.001 | |
| South (vs. Northeast) | 7.78 (3.66, 16.53) | 28.43 | <0.001 |
| Midwest (vs. Northeast) | 5.56 (2.63,-11.75) | 20.14 | <0.001 |
| West (vs. Northeast) | 5.39 (2.48, 11.72) | 18.01 | <0.001 |
| Percent Black (per 5 PP increase) | 1.09 (1.06, 1.13) | 23.79 | <0.001 |
| Number of physicians (per 100 MDs decrease) | 1.59 (1.32, 1.92) | 23.61 | <0.001 |
| Percent Hispanic (per 5 PP increase) | 1.06 (1.02, 1.11) | 9.23 | 0.002 |
| Median household income (per $10,000 decrease) | 1.18 (1.04, 1.34) | 6.68 | 0.010 |
| Median age (per 10 year decrease) | 1.28 (1.04, 1.58) | 5.35 | 0.021 |
| Percent without college education (per 5 PP decrease) | 1.09 (0.97, 1.21) | 2.24 | 0.135 |
| Percent male (per 5 PP increase) | 1.07 (0.88, 891.30) | 0.42 | 0.519 |
| Percent Asian (per 5 PP increase) | 1.06 (0.73, 1.53) | 0.10 | 0.758 |
| Heart disease mortality (per 100,000 people) | 1.000(0.997, 1.002) | 0.09 | 0.768 |
Abbreviations: CI, confidence interval; CPR, cardiopulmonary resuscitation; MD, medical doctor; OR, odds ratio; PP, percentage point; vs, versus
After including training in ACLS and PALS, the total number of residents having received CPR training increased by 1,217,858 to a total of 14,340,961 persons trained; of which, ACLS represented 9.5% of AHA training and 0.9% of HSI training, while PALS represented 3.2% of AHA training and 0.4% of HSI training. The median training rate for counties in the U.S. increased to only 2.45% with lower, middle, and upper tertile median CPR training rates of 0.52%, 2.45%, and 7.18%, respectively. Multivariable factors associated with the lower tertile of CPR training remained unchanged from the primary analysis (Appendix).
COMMENT
To our knowledge, this is the first national study of CPR training rates in the U.S. Notably, rural communities, as well as those with a high proportion of black race, Hispanic ethnicity, and lower median household incomes, had the lowest CPR training rates. Our findings may help explain racial and income differences in bystander CPR treatment rates and consequent overall survival post-OHCA.
Previously published data on regional CPR training in the U.S. have primarily been limited to small household population-based survey data.20–23 Nevertheless, these data only examine prevalent training rates, and most respondents had their last CPR training more than 10 years prior to survey administration. In contrast, our study examined current incident patterns of annual training, thereby making our data more likely to assist in the identification of geographical CPR training gaps, as well as inform public policy about future training efforts.
Our study found that several county-level demographic and geographic factors are associated with the odds of being in a lower tertile of CPR training. The strongest factor associated with low CPR training rates was high proportions of rural residents. Rural areas are defined in the Census by a process of exclusion; all population, housing, and territory not included within an urban area, and typically being inhabited by <2500 persons (http://www.census.gov/geo/www/ua/uafaq.html). Studies of OHCA in rural areas have consistently shown uniformly poor survival after cardiac arrest—a finding usually attributed to the lack of consistently available paramedic and central dispatcher services. In addition, longer emergency medical services response and transport times contribute to poorer survival.24,25 In this context, singly focusing on efforts to improve CPR and AED community education programs26 may not improve survival without also addressing longer ambulance arrival times. Rather, policy efforts by national associations and federal organizations are needed to address the entire “chain of survival” for pre-hospital care including transfer to a tertiary care hospital for rural community residents who experience OHCA. Future trials are needed to determine cost-effective and efficacious interventions for rural communities.
Communities with higher proportions of black residents have been shown to deliver bystander CPR less frequently, despite the higher incidence of OHCA in this population.15,30 Our study found that counties with higher proportions of blacks are significantly less likely to be trained, which may account for the lower use of bystander CPR in this population. Simple target interventions could improve the recognition of OHCA and the availability of citizens to perform this life-saving intervention.
Individual and neighborhood socioeconomic status is associated with bystander CPR use. In a prior study, Vaillancourt et al. found that OHCA victims who experienced arrest inside their homes, and were of lower socioeconomic status (measured by individual property value), were significantly less likely to receive bystander CPR compared with those of higher socioeconomic status.9 Recent data found an additive effect between race and neighborhood median household income: black communities comprised of lower-income households are more likely to have lower rates of bystander CPR than white communities comprised of higher-income households. Specifically, compared with high-income white neighborhoods, high-income black neighborhoods had an OR of 0.77 (95% CI 0.68–0.86), low income white neighborhoods had an OR of 0.65 (95% CI 0.51, 0.82), and low income black neighborhoods had an OR of 0.49 (95% CI 0.41, 0.58) for receipt of bystander CPR.14 In our study, counties with lower median household incomes were also significantly associated with lower CPR training. This finding may be driven by the fact that lower median household incomes often parallel with lower education levels, non-CPR required jobs, and the lack of CPR awareness campaigns.
In prior studies, when compared with whites, Hispanics have been significantly less likely to receive bystander CPR and have poorer survival.31,32 Similarly, in our study, counties with a greater proportion of Hispanics were more likely to have lower CPR training rates. While all of the major training organizations in our study report Spanish CPR program availability, these programs may not be adequately publicized in areas with a high density of Hispanics.
Additionally, in our study, counties with a higher median resident age had lower rates of CPR training. Perhaps older populations are not traditional targets for CPR training, or may have had training in the distant past and do not understand the need for repeat training. Finally, in our study, counties with a lower number of physicians had lower rates of CPR training. Limited physician availability may reflect areas without major healthcare institutions and CPR programs.
There is significant regional variation in the incidence and outcomes of OHCA.8,12,33 Interestingly, the variability in OHCA outcomes is far greater than the variability in stroke or ST-segment elevation myocardial infarction outcomes across the U.S.34 In our study, we demonstrated significant variability in incident CPR training rates, ranging from 0% to 15%. Some of the factors associated with this variability overlap with factors previously found to be associated with variation in bystander CPR use (black race, Hispanic ethnicity, and median household income). As a result, it is plausible that lower county-level CPR training rates may, in part, contribute to the lower use of bystander CPR, and consequent lower OHCA survival.
Currently, there are not county-level data on OHCA or OHCA survival rates in the U.S.; however, we found that counties with low CPR training had disproportionately higher heart disease mortality rates. While these data cannot directly link low training with low OHCA survival rates, they suggest that CPR training may not be occurring more intensively in populations with a high density of heart disease (i.e., populations at highest risk for OHCA). Given population data which show that bystander CPR could potentially double survival,3 programs providing simple and inexpensive CPR training that target vulnerable populations, could markedly reduce inequalities in outcomes after OHCA.16
Our study had several limitations. First, we assumed that people lived in the county in which they were trained. Second, we were unable to link 13% of data due to lack or invalid mapping of data (e.g., zip code or county name); this may have slightly underestimated training rates. Third, while we think that our estimates are accurate measures of persons trained for AHA BLS and HeartSaver, it is possible that the AHA Family and Friends program trained more people per training session than was estimated (e.g., if Family and Friends kits are used in mass community training events). Fourth, our data do not account for CPR training provided by other organizations, nor do our data account for those trained via social media or the internet. Finally, we did not have the ability to discriminate between participants who received first time training versus those who recertified.
In summary, current annual CPR training rates in the U.S. are low, with significant variability among counties. Efforts are needed to improve CPR training rates in all counties, but particularly in those with high proportions of residents living in rural areas, of black race or Hispanic ethnicity, and with lower median household incomes. Future research should be directed at understanding if targeted and intensive CPR training will narrow existing disparities in rates of bystander CPR and OHCA survival in these vulnerable communities. With regard to rural areas, more studies are needed on interventions that target the entire chain of survival.
Supplementary Material
Acknowledgments
The authors would like to thank Linda Davidson-Ray, Vladimir Demyanenko, and Erin LoFrese of the Duke Clinical Research Institute; John Thompson of the American Red Cross; Steve Barnett and Jeff Myers of the Health and Safety Institute; and Tim Williams of the American Heart Association, for their expertise and data support. Those acknowledged did not receive compensation for their contributions, apart from employment at the institution where this study was conducted.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance — Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60(8):1–19. [PubMed] [Google Scholar]
- 3.Bobrow BJ, Spaite DW, Berg RA, et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304(13):1447–1454. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- 4.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 6.Cowie MR, Fahrenbruch CE, Cobb LA, Hallstrom AP. Out-of-hospital cardiac arrest: racial differences in outcome in Seattle. Am J Public Health. 1993;83(7):955–959. doi: 10.2105/ajph.83.7.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med. 1993;329(9):600–606. doi: 10.1056/NEJM199308263290902. [DOI] [PubMed] [Google Scholar]
- 8.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166(5):534–543. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 9.Vaillancourt C, Lui A, De Maio VJ, Wells SA, Stiell IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79(3):417–423. doi: 10.1016/j.resuscitation.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Hallstrom A, Boutin P, Cobb L, Johnson E. Socioeconomic status and prediction of ventricular fibrillation survival. Am J Public Health. 1993;83(2):245–248. doi: 10.2105/ajph.83.2.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reinier K, Thomas E, Andrusiek DL, et al. Socioeconomic status and incidence of sudden cardiac arrest. CMAJ. 2011;183(15):1705–1712. doi: 10.1503/cmaj.101512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sasson C, Keirns CC, Smith DM, et al. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation. 2011;82(6):674–679. doi: 10.1016/j.resuscitation.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13(6):596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 14.Sasson C, Magid DJ, Chan P, et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367(17):1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brookoff D, Kellermann AL, Hackman BB, Somes G, Dobyns P. Do blacks get bystander cardiopulmonary resuscitation as often as whites? Ann Emerg Med. 1994;24(6):1147–1150. doi: 10.1016/s0196-0644(94)70246-2. [DOI] [PubMed] [Google Scholar]
- 16.Sasson C, Meischke H, Abella BS, et al. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a Science Advisory from the American Heart Association for Healthcare Providers, Policymakers, Public Health Departments, and Community Leaders. Circulation. 2013;127(12):1342–1350. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
- 17.Isbye DL, Rasmussen LS, Ringsted C, Lippert FK. Disseminating cardiopulmonary resuscitation training by distributing 35,000 personal manikins among school children. Circulation. 2007;116(12):1380–1385. doi: 10.1161/CIRCULATIONAHA.107.710616. [DOI] [PubMed] [Google Scholar]
- 18.Potts J, Lynch B. The American Heart Association CPR Anytime Program: the potential impact of highly accessible training in cardiopulmonary resuscitation. J Cardiopulm Rehabil. 2006;26(6):346–354. doi: 10.1097/00008483-200611000-00002. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Health Resources and Services Administration. Bureau of Health Professions. Rockville, MD: U.S. Department of Health and Human Services; 2010. [producer]. Fairfax, Va: Quality Resource Systems, Inc., 2010 [distributor]. Codebook: HE-001 (2010). Cornell University web site. http://ciser.cornell.edu/ASPs/search_athena.asp?IDTITLE=2551. Accessed April 9, 2013. [Google Scholar]
- 20.Sipsma K, Stubbs BA, Plorde M. Training rates and willingness to perform CPR in King County, Washington: a community survey. Resuscitation. 2011;82(5):564–567. doi: 10.1016/j.resuscitation.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Mandel LP, Cobb LA. CPR training in the community. Ann Emerg Med. 1985;14(7):669–671. doi: 10.1016/s0196-0644(85)80885-4. [DOI] [PubMed] [Google Scholar]
- 22.Murphy RJ, Luepker RV, Jacobs DR, Jr, Billum RF, Folsom AR, Blackburn H. Citizen cardiopulmonary resuscitation training and use in a metropolitan area: the Minnesota Heart Survey. Am J Public Health. 1984;74(5):513–515. doi: 10.2105/ajph.74.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naughton MJ, Luepker RV, Sprafka JM, McGovern PG, Burke GL. Community trends in CPR training and use: the Minnesota Heart Survey. Ann Emerg Med. 1992;21(6):698–703. doi: 10.1016/s0196-0644(05)82782-9. [DOI] [PubMed] [Google Scholar]
- 24.Bachman JW. Cardiac arrest in the community. How to improve survival rates. Postgrad Med. 1984;76(3):85–90. 92–95. doi: 10.1080/00325481.1984.11698715. [DOI] [PubMed] [Google Scholar]
- 25.Killien SY, Geyman JP, Gossom JB, Gimlett D. Out-of-hospital cardiac arrest in a rural area: a 16-year experience with lessons learned and national comparisons. Ann Emerg Med. 1996;28(3):294–300. doi: 10.1016/s0196-0644(96)70028-8. [DOI] [PubMed] [Google Scholar]
- 26.Stiell IG, Wells GA, Field B, et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):647–656. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 27.Steinhaus DA, Vittinghoff E, Moffatt E, Hart AP, Ursell P, Tseng ZH. Characteristics of sudden arrhythmic death in a diverse, urban community. Am Heart J. 2012;163(1):125–131. doi: 10.1016/j.ahj.2011.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilde ET, Robbins LS, Pressley JC. Racial differences in out-of-hospital cardiac arrest survival and treatment. Emerg Med J. 2012;29(5):415–419. doi: 10.1136/emj.2010.109736. [DOI] [PubMed] [Google Scholar]
- 29.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104(18):2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 30.Iwashyna TJ, Christakis NA, Becker LB. Neighborhoods matter: a population-based study of provision of cardiopulmonary resuscitation. Ann Emerg Med. 1999;34(4 Pt 1):459–468. doi: 10.1016/s0196-0644(99)80047-x. [DOI] [PubMed] [Google Scholar]
- 31.Sadosty A, Kruse B, Vadeboncoeur T. Five simple steps to improve an emergency physician’s efficiency. Am J Emerg Med. 2008;26(9):1056–1057. doi: 10.1016/j.ajem.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 32.Benson PC, Eckstein M, McClung CD, Henderson SO. Racial/ethnic differences in bystander CPR in Los Angeles, California. Ethn Dis. 2009;19(4):401–406. [PubMed] [Google Scholar]
- 33.Dunne RB, Compton S, Zalenski RJ, Swor R, Welch R, Bock BF. Outcomes from out-of-hospital cardiac arrest in Detroit. Resuscitation. 2007;72(1):59–65. doi: 10.1016/j.resuscitation.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 34.Sidney S, Rosamond WD, Howard VJ, Luepker RV, National Forum for Heart Disease and Stroke Prevention The “heart disease and stroke statistics–2013 update” and the need for a national cardiovascular surveillance system. Circulation. 2013;127(1):21–23. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


