Abstract
Background
Although Pay for Performance (P4P) has become common, many worry that P4P will lead providers to avoid offering surgical procedures to the sickest patients out of concern that poor outcomes will lead to financial penalties.
Methods and Results
We used Medicare data to compare change in rates of coronary artery bypass graft surgery (CABG) between 2002–03 and 2008–09 among patients with acute myocardial infarction (AMI) admitted to 126 hospitals participating in Medicare’s Premier Hospital Quality Incentive Demonstration P4P program (HQID) with patients in 848 control hospitals participating in public reporting alone. We examined rates for all AMI patients and those in the top decile of predicted mortality based on demographics, medical comorbidities and AMI characteristics. We identified 91,393 patients admitted for AMI in Premier hospitals and 502,536 Medicare patients admitted for AMI in control hospitals. CABG rates for AMI patients in Premier decreased from 13.6% in 2002–03 to 10.4% in 2008–09; there was a comparable decrease in non-Premier hospitals (13.6% to 10.6%, p-value for comparison of changes between Premier and non-Premier of 0.67). CABG rates for high-risk patients in Premier decreased from 8.4% in FY 2002–3 to 8.2% in 2008–9. Patterns were similar in non-Premier hospitals (8.4% to 8.3%, p-value for comparison of changes between Premier and non-Premier, 0.82).
Conclusions
Our results show no evidence of a deleterious impact of P4P on access to CABG for high-risk patients with AMI. These results should be reassuring to those concerned about the potential negative impact of P4P on high-risk patients.
Keywords: Pay-for-performance, coronary artery bypass graft surgery, acute myocardial infarction
Introduction
Providing financial incentives for higher quality of care (Pay for Performance or P4P) has become an important component of both government and private efforts to improve the quality of health care provided by U.S. hospitals. However, critics have worried that P4P will create a financial disincentive for hospitals to offer care – and in particular, high-risk procedures – to patients whose mortality rates may be high, potentially worsening access to care for a population who could benefit significantly from its receipt.1, 2 Despite the potential importance of these concerns, there are almost no data on access to procedures for high-risk patients under P4P programs.
However, P4P has been used by the Centers for Medicare and Medicaid Services (CMS) for almost a decade, and continues to expand. In fact, from 2003 through 2009, the CMS conducted the largest demonstration program of P4P to date, the Premier Hospital Quality Incentive Demonstration (HQID). The Premier HQID provided financial incentives based on quality of care for acute myocardial infarction (AMI), pneumonia, congestive heart failure (CHF), total hip replacement (THR), total knee replacement (TKR), and coronary artery bypass grafting (CABG), and on mortality rates for AMI and CABG. This program served as the model for the recently established federal P4P program known as Value-Based Purchasing (VBP). Introduced in October 2012, VBP establishes P4P for all Medicare patients hospitalized for treatment of AMI, pneumonia, or CHF. In future years, the VBP program is likely to expand to other conditions and procedures; at the same time, P4P programs are becoming increasingly common in the private insurance market.
If critics’ concerns about P4P are well-founded, and financial incentives for low mortality rates reduce access to care and procedures for high-risk patients, we are at risk of expanding this problem as VBP includes the large majority of U.S. hospitals. It is therefore critical to understand the impact of prior P4P programs on access to care for vulnerable patients. To address this data gap, we studied rates of CABG surgery for patients with AMI in the Premier HQID and a comparison group treated in non-Premier hospitals. We focused on patients with AMI to reduce heterogeneity among candidates for CABG in different settings and because the literature supports using CABG surgery in an important subset of such patients.3, 4 We sought to determine whether rates of CABG decreased over time under P4P compared to those in non-Premier hospitals. We examined differences in these patterns overall and for patients at high and low risk of mortality, hypothesizing that Premier hospitals would be more likely to show a relative decrease in CABG rates among high-risk patients.
Methods
Premier HQID Participants and Comparison Hospitals
In 2003, CMS invited 421 hospitals participating in the Premier Healthcare Informatics Program to join the HQID pay-for-performance program, and 255 (61%) agreed to do so. Participating hospitals were required to provide information on 33 quality measures for CABG, THR, TKR, AMI, CHF, and pneumonia). The quality indicators specific to CABG surgery included process measures (e.g., aspirin at discharge, prophylactic antibiotic received within 1 hour prior to surgery and antibiotic discontinued within 48 hours) and risk-adjusted mortality. Hospitals performing in the top decile for each condition received a bonus payment of 2% of Medicare payments for that condition. Hospitals scoring in the second decile received a 1% bonus. The lowest performing hospitals were liable for a 1–2% financial penalty, which was implemented in year 4 of the demonstration. During the course of the program, the Premier HQID modified its incentive structures to reward improvement as well as performance.
As a comparison group, we identified the national sample of hospitals not participating in Premier but participating in public reporting of processes and outcomes of care for AMI, congestive heart failure, and pneumonia through the Hospital Quality Alliance (HQA). We chose hospitals reporting data in the HQA because we felt that they had sufficient patients for reporting, and had demonstrated potential interest in quality improvement activities, thus reducing the selection bias associated with choosing to participate in Premier. During the time period of our study the HQA collected data on a number of process and outcome measures, but none of these were directly related to CABG. The only control or Premier hospitals with publicly reported data on CABG were those located in three states with state-based CABG mortality reporting systems (New York, Pennsylvania, and Massachusetts). Below we describe sensitivity analyses eliminating these three states from our analyses.
By linking data on both the Premier and the comparison group to Medicare cost reports and the American Hospital Association (AHA) annual survey, we identified hospitals’ key characteristics including number of beds, regional location, profit status, teaching status, eligibility for large bonuses (i.e., having a high proportion Medicare patients), Medicare margins, and location in a competitive market (as measured by the Herfindahl-Hirschman Index). The latter three characteristics have been shown to be associated with greater improvements in process quality in response to P4P.5
Access to CABG
To examine access to CABG we used Part A Medicare data from January 1, 2002 through September 30, 2009 on all patients older than 65 years discharged with a principal diagnosis of AMI (International Classification of Diseases, Ninth Revision (ICD-9) codes 410.x1). Transferred patients were assigned to the receiving hospital, consistent with CMS practice in calculating mortality rates for CABG within the Premier program. We only included patients with AMI who were admitted or transferred to a CABG-capable hospital in each of the study years (126 Premier and 848 non-Premier hospitals); in sensitivity analyses, we excluded transfer patients and our results were qualitatively very similar. Our primary endpoint was receipt of an isolated CABG (procedure codes 3610–3619).
Risk of 30-Day Mortality
We estimated each patient’s risk of 30-day mortality using a logistic regression model that included age, sex, and the presence of 28 comorbidities used in the Elixhauser risk-adjustment scheme (we dropped a 29th comorbidity, AIDS, because its prevalence was too low in our population), a validated,6–8 widely-used9–14 tool, developed for use with administrative data. Consistent with prior work,15 we also adjusted for characteristics of the AMI: we identified patients with non-ST-segment elevation myocardial infarction (NSTEMI) as patients with a primary diagnosis of subendocardial AMI (ICD-9 code 410.71), patients with ST-segment elevation myocardial infarction (STEMI) as those with a diagnosis of STEMI (ICD-9 codes 410.x1 excluding 410.71), and patients with cardiogenic shock or cardiac arrest as those with additional codes for those conditions (ICD-9 codes 785.51 and 427.5, respectively).
Data Analysis
We first compared characteristics of Premier and non-Premier hospitals, the characteristics of patients who received care for AMI at those hospitals, and how patient characteristics changed between 2002–3 and 2008–9. We calculated patients’ predicted risk of mortality with the logistic regression model described above and examined the association between each decile of predicted mortality and observed 30-day mortality rates and CABG rates.
Our primary outcome was receipt of CABG surgery. We expected that rates at Premier hospitals would decrease more over time under P4P and hypothesized that Premier hospitals would seek to avoid performing CABG on high risk patients (i.e. those in the top decile of predicted mortality) to avoid high mortality rates and consequent financial penalties. We first plotted out annual, unadjusted rates of CABG surgery among patients at Premier and non-Premier hospitals for high-risk patients (those in the highest decile of predicted risk of 30-day mortality) and low-risk patients (the remainder of the population) separately. To formally examine changes over time, we compared the rate from January 1, 2002 through September 30, 2003 (the 21 month time period just before P4P was initiated) to the rate from January 1, 2008 through September 30, 2009 (the last 21 months of the program). Changes were examined using a patient-level hierarchical logistic regression model clustered by hospital, adjusting for age, sex, 28 Elixhauser medical comorbidities, and characteristics of the AMI. We also included variables for hospital characteristics (size, region, profit status, teaching status, proportion of Medicare patients, margin, and location in a competitive market), time (2008–9 versus 2002–3), Premier status, and a two-way interaction between time and Premier status. The p value from this interaction term was used to assess whether changes in rates of CABG over time were statistically different in Premier versus non-Premier hospitals.
We repeated this analysis for the high-risk group and the low-risk group separately. We then extended this analysis focusing on additional variables shown to be more highly associated with improvement in process of care in response to P4P—proportion of patients with Medicare coverage, margin, and location in a competitive market. Three-way interactions between each of these variables, Premier status and time were used to determine whether any of them modified the relationship between Premier status and change in access to CABG. As a sensitivity analysis we defined “high risk” as those patients in the top two deciles of predicted mortality. To address concerns that Premier hospitals may code comorbid conditions more aggressively to make their patients appear sicker than similar patients in non-P4P hospitals, we repeated the analyses without adjusting for comorbidity. Finally, as a sensitivity analysis, we eliminated hospitals in the three states with public reporting for risk-adjusted CABG mortality and repeated our analyses. All analyses were performed using SAS software, Version 9.3 (SAS Institute, Inc., Cary, NC). The study was granted exemption by the Harvard School of Public Health Institutional Review Board.
Results
Hospital and Patient Characteristics
Hospitals participating in the Premier HQID were more often private, non-profit institutions than non-Premier hospitals (Table 1). Patients with AMI admitted to Premier hospitals were younger, more often black, less often low-income, more likely to have an NSTEMI or COPD and less likely to have cardiogenic shock (Table 2).
Table 1.
Characteristics of Premier versus Non-Premier Hospitals§
| Hospital Characteristics | Premier | Non-Premier | P-Value | |
|---|---|---|---|---|
| Number of Hospitals | 126 | 848 | N/A | |
| Size | ||||
| Small | 0.0% | 1.7% | 0.13 | |
| Medium | 55.6% | 61.0% | ||
| Large | 44.4% | 37.4% | ||
| Region | ||||
| Northeast | 13.5% | 13.4% | 0.09 | |
| Midwest | 23.0% | 28.3% | ||
| South | 48.4% | 37.3% | ||
| West | 15.1% | 21.0% | ||
| Ownership | ||||
| For-profit | 0.8% | 18.6% | <0.001 | |
| Private non-profit | 90.5% | 70.1% | ||
| Public | 8.7% | 11.3% | ||
| Teaching | ||||
| Major | 23.8% | 22.3% | 0.90 | |
| Minor | 36.5% | 36.1% | ||
| Not Teaching | 39.7% | 41.6% | ||
| RUCA* | ||||
| Urban | 75.3% | 73.9% | 0.90 | |
| Sub-Urban | 7.2% | 9.6% | ||
| Large Rural Town | 8.3% | 7.7% | ||
| Small Town/Isolated Rural | 9.3% | 8.8% | ||
| Median (IQR)Percent Medicare | 42.6% (37.8% – 48.9%) | 42.8% (37.5% – 48.2%) | 0.59 | |
| Median (IQR)Percent Medicaid | 16.9% (11.8% – 20.8%) | 16.8% (11.3% – 21.3%) | 0.56 | |
| Median(IQR)Proportion Black | 4.5% (1.6% – 11.8%) | 3.8% (1.3% – 9.9%%) | 0.86 | |
| Median(IQR)County Income† | $46,299 ($41,586 – $53,934) | $47,792 ($41852 – $54,375) | 0.30 | |
| Median(IQR)County Poverty Rate† | 15.3% (12.6% – 17.1%) | 15.3% (12.4% – 17.6%) | 0.71 | |
RUCA=Rural Urban Commuting Area
Income and poverty rate refer to the county where hospitals are located.
Chi-square tests were performed for categorical variables, while, for continuous variables, the table shows medians and inter-quartile ranges, along with p-values from a Mann-Whitney U test.
Table 2.
Patient Characteristics in Premier and Non-Premier Hospitals§
| Patient Characteristics | Premier | Non-Premier | P-Value | |
|---|---|---|---|---|
| Number of Patients | 91,393 | 502,537 | N/A | |
| Age (Median, IQR) | 77, (71 – 83) | 77, (71 – 83) | <0.001 | |
| Gender (% female) | 47.7% | 47.8% | 0.94 | |
| African American | 7.7% | 7.2% | <0.001 | |
| Hispanic | 1.4% | 1.4% | 0.28 | |
| Acute Myocardial Infarction | Non ST-Elevation MI (NSTEMI) | 62.0% | 61.3% | <0.001 |
| ST-Elevation MI (STEMI) | 31.0% | 31.3% | 0.07 | |
| Cardiogenic Shock / Cardiac Arrest | 7.1% | 7.4% | <0.001 | |
| Comorbid Conditions | Average Number of Comorbidities | 1.84 | 1.85 | 0.14 |
| Congestive Heart Failure | 0.9% | 1.0% | 0.22 | |
| Diabetes | 26.6% | 26.4% | 0.36 | |
| Hypertension | 55.7% | 55.6% | 0.73 | |
| COPD | 20.1% | 19.6% | <0.001 | |
| Low Income* (Median, IQR) | 14.0%(11.1% – 17.0%) | 13.5%(10.1% – 16.3%) | <0.001 | |
Lowincome is defined as the proportion of people below the poverty line in the patients’ county of residence
Chi-square tests were performed for categorical variables, while, for continuous variables, the table shows medians and inter-quartile ranges, along with p-values from a Mann-Whitney U test.
Patient populations of both Premier and non-Premier hospitals changed modestly over time (Table 3). For example, in both sets of hospitals the patient population became older. The average number of comorbid medical conditions increased comparably in Premier and non-Premier hospitals.
Table 3.
Change in Patient Characteristics in Premier and Non-Premier Hospitals
| Patient Characteristics | Premier | Non-Premier | Difference in Change (Premier vs. Non- Premier) |
|||||
|---|---|---|---|---|---|---|---|---|
| 2002– 2003 |
2008– 2009 |
P-Value | 2002– 2003 |
2008– 2009 |
P-Value | P-Value | ||
| Number of Patients | 51,555 | 39,838 | N/A | 281,876 | 220,661 | N/A | N/A | |
| Age (mean) | 76.8 | 77.7 | <0.001 | 76.9 | 77.8 | <0.001 | 0.60 | |
| Gender (% female) | 47.8% | 47.7% | 0.72 | 48.0% | 47.5% | 0.00 | 0.32 | |
| African American | 7.6% | 7.8% | 0.30 | 6.9% | 7.6% | <0.001 | 0.004 | |
| Hispanic | 1.3% | 1.5% | 0.05 | 1.4% | 1.5% | 0.14 | 0.22 | |
| Acute Myocardial Infarction Type | Non ST Elevation MI (NSTEMI) | 57.3% | 68.1% | <0.001 | 56.3% | 67.7% | <0.001 | 0.08 |
| ST Elevation MI (STEMI) | 35.4% | 25.2% | <0.001 | 36.3% | 24.9% | <0.001 | 0.001 | |
| Shock / Cardiac Arrest | 7.3% | 6.7% | <0.001 | 7.5% | 7.4% | 0.54 | 0.01 | |
| Comorbid Conditions | Average Number of Comorbidities | 1.8 | 1.9 | <0.001 | 1.8 | 1.9 | <0.001 | 0.14 |
| Congestive Heart Failure | 1.2% | 0.6% | <0.001 | 1.2% | 0.7% | <0.001 | 0.09 | |
| Diabetes | 26.7% | 26.4% | 0.27 | 26.9% | 25.8% | <0.001 | 0.01 | |
| Hypertension | 54.3% | 57.5% | <0.001 | 54.0% | 57.7% | <0.001 | 0.16 | |
| COPD | 22.1% | 17.6% | <0.001 | 21.4% | 17.3% | <0.001 | 0.15 | |
| Low Income* | 14.6% | 14.4% | <0.001 | 13.6% | 13.7% | 0.008 | <0.001 | |
Low-income is defined as the proportion of people below the poverty line
Risk of Mortality
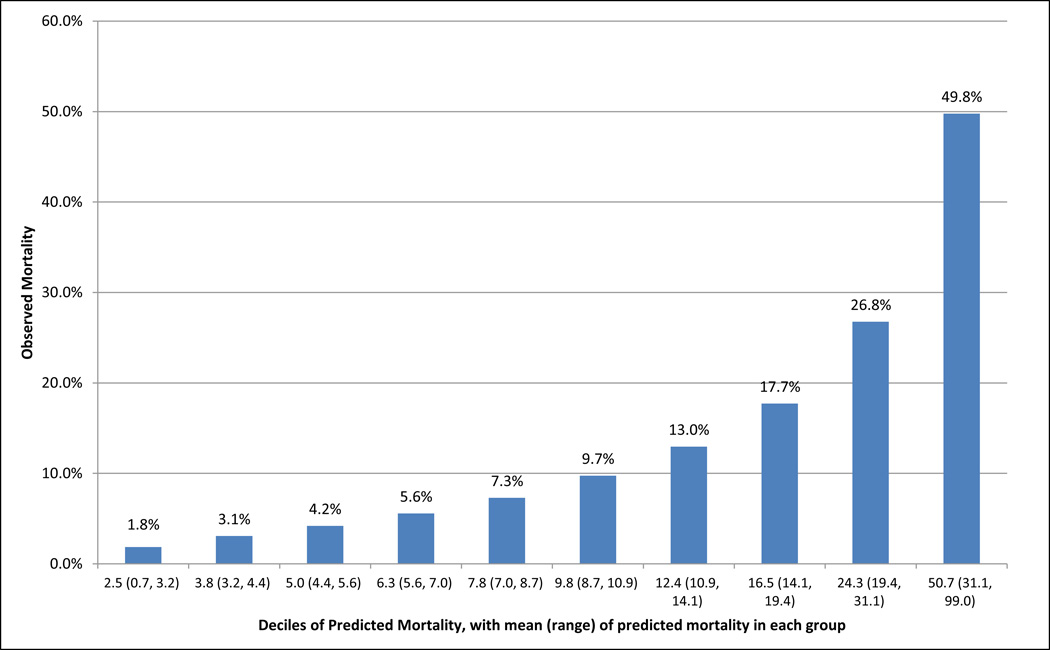
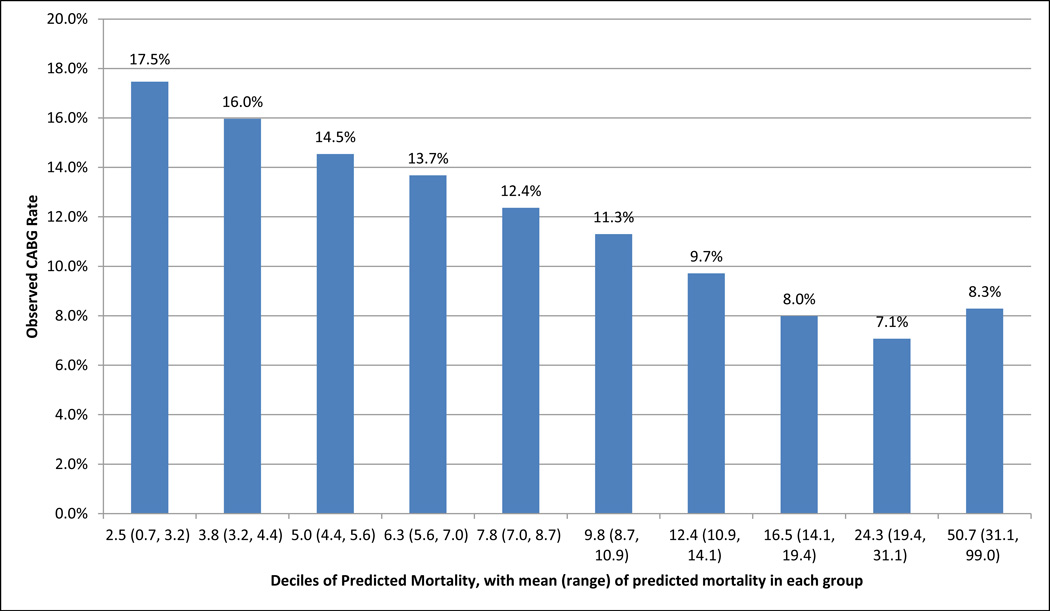
The mean observed mortality among AMI patients spanned from 1.8% among those assigned to the lowest decile of predicted risk of mortality to nearly 50% among patients assigned to the highest decile of predicted risk (Figure 1). We found that procedure rates were inversely related to risk (except for the highest decile) with 17.5% of patients in the lowest-risk decile receiving CABG surgery compared to 8.3% in the highest-risk group (Figure 2).
Figure 1.
Observed 30-day Mortality by Predicted Mortality Risk Deciles
Figure 2.
Observed CABG Rates by Predicted Mortality Risk Deciles
Change in Use of CABG Surgery after Initiation of P4P
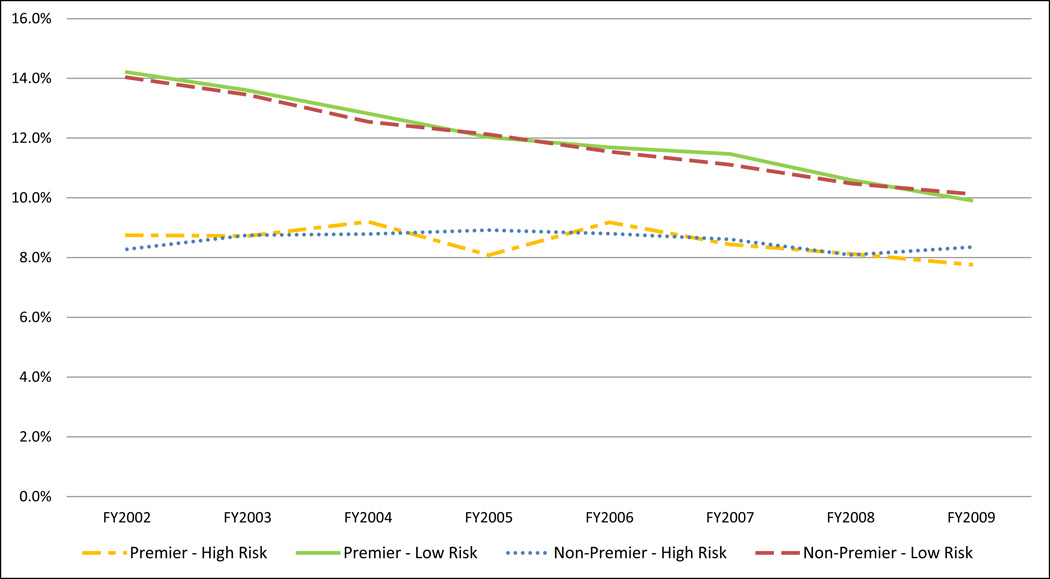
Crude rates of CABG surgery for both high-risk and low-risk patients with AMI decreased between FY2002–3 and FY2008–9 in both Premier and non-Premier hospitals (Figure 3), and the changes were comparable in both types of hospital. After adjusting for patient and hospital characteristics, CABG rates at Premier hospitals decreased by 3.2% between FY2002–3 and FY2008–09 (p<0.001) and by 3.0% at non-Premier hospitals (p<0.001; difference 0.2%, 95% confidence interval (CI) −0.6% to 0.9%, p= 0.67, Table 4). Rates of CABG surgery for high-risk patients decreased minimally over time for both Premier (8.4% to 8.2%) and non-Premier (8.4% to 8.3%) hospitals and the difference in change between Premier and non-Premier hospitals was small (0.2%, 95% CI −1.2% to 1.5%, p-value 0.82). Rates for low-risk patients decreased substantially in Premier (14.0% to 10.5%) and non-Premier hospitals (14.0% to 10.6%, both p<0.001) but the changes were comparable in the two groups of hospitals (difference 0.2% 95% CI −0.6% to 0.9%, p=0.66).
Figure 3.
Unadjusted CABG Procedure Rates
*FY 2002 includes nine months from January 1, 2002 through September 30, 2002.
Table 4.
Change in CABG Rates by Risk of Mortality and Overall in Premier vs. Non-Premier Hospitals
| Premier Hospitals | Non-Premier Hospitals | Difference in Change (Premier vs. Non- Premier) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2002–2003 | 2008–2009 | Change | P-Value | 2002–2003 | 2008–2009 | Change | P-Value | Difference (95% CI) |
P-Value | |
| High Risk | 8.4% | 8.2% | −0.2% | 0.70 | 8.4% | 8.3% | −0.1% | 0.77 | 0.2 (−1.2, 1.5) | 0.82 |
| Low Risk | 14.0% | 10.5% | −3.5% | <0.001 | 14.0% | 10.6% | −3.3% | <0.001 | 0.2 (−0.6, 0.9) | 0.66 |
| All | 13.6% | 10.4% | −3.2% | <0.001 | 13.6% | 10.6% | −3.0% | <0.001 | 0.2 (−0.6, 0.9) | 0.67 |
Results adjusted for age, sex, 28 Elixhauser comorbidities, type of myocardial infarction, and hospital characteristics (size, region, profit status, teaching status, proportion of Medicare patients, margin and location in a competitive market)
We performed additional analyses examining whether there was significant effect modification in hospitals characterized by a higher proportion of Medicare patients, higher margins, or location in a competitive market; but there was none. We repeated our analyses with no adjustment for comorbidity and found qualitatively similar results. Sensitivity analyses in which we defined the high–risk group as those patients in the top two deciles of predicted mortality gave qualitatively similar results as well. Finally, when we repeated our analyses dropping hospitals in the three states with public reporting for CABG outcomes (Massachusetts, New York and Pennsylvania), the results were nearly identical and the conclusions unchanged.
Discussion
We examined the impact of P4P on receipt of CABG surgery among patients with AMI and found no evidence that being under financial incentives led hospitals to restrict access for patients overall or those at particularly high risk of mortality. Even among hospitals that have been previously found to be more responsive to P4P (those with a large proportion of Medicare patients, higher margin, or location in a more competitive market), we found no evidence that patients were less likely to receive CABG surgery under P4P.
There are a number of potential explanations for our findings. One possibility is that the overall decline in use of CABG for high-risk patients over the study period overwhelmed any impact of P4P on patient selection. Our study period corresponds with a time in which the use of multivessel and left main percutaneous coronary interventions grew significantly, and this secular trend may have reduced our ability to see a difference between the two groups. It is also possible that, in contrast to prior studies examining risk aversion in selection for CABG under public reporting,16 the fact that both AMI and CABG mortality were explicitly incented provided protection against underuse of this procedure. In AMI patients for whom CABG was clearly the treatment of choice, financial incentives for AMI mortality may have acted to reduce risk aversive behavior.
Our findings likely have implications for VBP, the recently introduced federal P4P program modeled on Premier. As in Premier, there are incentives in VBP for both improvement and attainment, and the amount of money at risk is relatively small17—set in statute as 1% in the initial year and rising to only 2% in 2017. Also as in Premier, there is overlap in the targeted conditions and surgical procedures (CHF, AMI, pneumonia and next year CABG), and in the condition-based quality indicators used to measure performance (both process indicators and risk-adjusted mortality). Thus, our results should be reassuring to those concerned about the federal program’s potential impact on access.
We are unaware of prior U.S. work that has directly examined whether hospitals that are under financial incentives restrict access to care for medically high-risk or severely ill populations. In the only other study of P4P and access, Ryan examined the impact of the Premier HQID on access for minority patients, focusing on AMI, CHF, pneumonia, and CABG after admission for AMI.18 He found little evidence of impact; only “other race” beneficiaries had a reduction in use rates relative to white patients and only for AMI. However, there is more evidence on the impact of public reporting on access to care. Several studies have documented that physicians perceive public reporting to create access problems for patients who might benefit from care.19, 20 Further, evidence from New York State suggests that disparities in rates of CABG surgery increased for black and Hispanic patients relative to white patients after implementation of public reporting,21 and evidence from Massachusetts shows that access to PCI decreased, especially for severely ill patients, after the introduction of public reporting.15 Additional studies have shown mixed results.22–24
Our study has limitations. First, the data come from a single voluntary P4P program, although the Premier HQID is in many ways a model for the federal program. Prior studies suggest that the Premier HQID had a modest impact on process quality, at least in the short run.5, 25 It is possible that programs constructed differently might have both a greater impact on quality improvement and a deleterious impact on access to care. The small size of the incentives in Premier may have been insufficient to make hospitals risk adverse. Premier hospitals participated in the program voluntarily and may differ from other hospitals in their willingness to maintain access for high risk patients; it is possible that in a universal program the results would differ. We caution readers not to generalize our findings to all P4P programs, although the program we studied shares many similar features with the existing federal program, which makes our findings particularly relevant to policy concerns.
Our assessment of comorbidities and patients’ risk is based on administrative data and the Elixhauser risk algorithm, whereas physicians judging risk have information about a broader array of physiologic and clinical variables that may have enabled more accurate assessments. The type of AMI as defined by the ICD codes used in this study produced strata with heterogeneous cohorts of patients, so unrecognized confounders may still have affected our results. We cannot determine whether our data showing modest changes in comorbidity reflect actual changes in comorbidity or changes in patterns of coding. Because we had no information on appropriateness of care, we could only evaluate access on the basis of use rates. Finally, our findings were limited to Medicare patients older than 65 and may not generalize to a younger population.
In summary, our study suggests that P4P did not lead to lower access to CABG for patients with AMI in the Premier HQID, the largest demonstration of hospital P4P to date. These results should be reassuring to those concerned about the potential negative impact of VBP, the P4P program recently introduced by CMS, on access to care for high-risk populations.
Supplementary Material
Acknowledgments
Funding:
This work was supported by a grant from the Robert Wood Johnson Foundation. The funder had no role in the design or conduct of the study, the analysis or interpretation of the results, or the creation of the manuscript. Dr. Joynt was additionally supported by grant 1K23HL109177-01 from the National Heart, Lung, and Blood Institute.
Footnotes
Disclosures:
The authors have no potential conflicts of interest to disclose.
References
- 1.Casalino LP, Elster A, Eisenberg A, Lewis E, Montgomery J, Ramos D. Will pay-for-performance and quality reporting affect health care disparities? Health Aff. 2007;26:w405–w414. doi: 10.1377/hlthaff.26.3.w405. [DOI] [PubMed] [Google Scholar]
- 2.Chien AT, Chin MH, Davis AM, Casalino LP. Pay for performance, public reporting, and racial disparities in health care how are programs being designed? Med Care Res Rev. 2007;64:283S–304S. doi: 10.1177/1077558707305426. [DOI] [PubMed] [Google Scholar]
- 3.Eagle KA, Guyton RA, Davidoff R, Ewy GA, Fonger J, Gardner TJ, Parker Gott J, Herrmann HC, Marlow RA, Nugent W. Acc/aha guidelines for coronary artery bypass graft surgery: Executive summary and recommendations. Circulation. 2000;100:1464–1480. doi: 10.1161/01.cir.100.13.1464. [DOI] [PubMed] [Google Scholar]
- 4.Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, DiSesa VJ, Hiratzka LF, Hutter AM, Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 accf/aha guideline for coronary artery bypass graft surgery: A report of the american college of cardiology foundation/american heart association task force on practice guidelines. Circulation. 2011;124:e652–e735. doi: 10.1161/CIR.0b013e31823c074e. [DOI] [PubMed] [Google Scholar]
- 5.Werner RM, Kolstad JT, Stuart EA, Polsky D. The effect of pay-for-performance in hospitals: Lessons for quality improvement. Health Aff. 2011;30:690–698. doi: 10.1377/hlthaff.2010.1277. [DOI] [PubMed] [Google Scholar]
- 6.Hcup comorbidity software. 2010;2010 [Google Scholar]
- 7.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Southern DA, Quan H, Ghali WA. Comparison of the elixhauser and charlson/deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42:355–360. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 9.Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of charlson and elixhauser comorbidities in icd-9 and icd-10 administrative databases. BMC Health Serv Res. 2008;8:12. doi: 10.1186/1472-6963-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pine M, Jordan HS, Elixhauser A, Fry DE, Hoaglin DC, Jones B, Meimban R, Warner D, Gonzales J. Enhancement of claims data to improve risk adjustment of hospital mortality. JAMA. 2007;297:71–76. doi: 10.1001/jama.297.1.71. [DOI] [PubMed] [Google Scholar]
- 11.Volpp KG, Rosen AK, Rosenbaum PR, Romano PS, Even-Shoshan O, Canamucio A, Bellini L, Behringer T, Silber JH. Mortality among patients in va hospitals in the first 2 years following acgme resident duty hour reform. JAMA. 2007;298:984–992. doi: 10.1001/jama.298.9.984. [DOI] [PubMed] [Google Scholar]
- 12.Volpp KG, Rosen AK, Rosenbaum PR, Romano PS, Even-Shoshan O, Wang Y, Bellini L, Behringer T, Silber JH. Mortality among hospitalized medicare beneficiaries in the first 2 years following acgme resident duty hour reform. JAMA. 2007;298:975–983. doi: 10.1001/jama.298.9.975. [DOI] [PubMed] [Google Scholar]
- 13.Jha AK, Orav EJ, Li Z, Epstein AM. The inverse relationship between mortality rates and performance in the hospital quality alliance measures. Health Aff. 2007;26:1104–1110. doi: 10.1377/hlthaff.26.4.1104. [DOI] [PubMed] [Google Scholar]
- 14.Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg. 2007;204:383–391. doi: 10.1016/j.jamcollsurg.2006.12.031. [DOI] [PubMed] [Google Scholar]
- 15.Joynt KE, Blumenthal DM, Orav EJ, Resnic FS, Jha AK. Association of public reporting for percutaneous coronary intervention with utilization and outcomes among medicare beneficiaries with acute myocardial infarctionpublic reporting of patient outcomes. JAMA. 2012;308:1460–1468. doi: 10.1001/jama.2012.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Werner RM, Asch DA, Polsky D. Racial profiling: The unintended consequences of coronary artery bypass graft report cards. Circulation. 2005;111:1257–1263. doi: 10.1161/01.CIR.0000157729.59754.09. [DOI] [PubMed] [Google Scholar]
- 17.Werner RM, Dudley RA. Medicare’s new hospital value-based purchasing program is likely to have only a small impact on hospital payments. Health Aff. 2012;31:1932–1940. doi: 10.1377/hlthaff.2011.0990. [DOI] [PubMed] [Google Scholar]
- 18.Ryan AM. Has pay-for-performance decreased access for minority patients? Health Serv Res. 2010;45:6–23. doi: 10.1111/j.1475-6773.2009.01050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Narins CR, Dozier AM, Ling FS, Zareba W. The influence of public reporting of outcome data on medical decision making by physicians. Arch Intern Med. 2005;165:83. doi: 10.1001/archinte.165.1.83. [DOI] [PubMed] [Google Scholar]
- 20.Schneider EC, Epstein AM. Influence of cardiac-surgery performance reports on referral practices and access to care—a survey of cardiovascular specialists. New Eng J Med. 1996;335:251–256. doi: 10.1056/NEJM199607253350406. [DOI] [PubMed] [Google Scholar]
- 21.Werner RM, Asch DA, Polsky D. Racial profiling the unintended consequences of coronary artery bypass graft report cards. Circulation. 2005;111:1257–1263. doi: 10.1161/01.CIR.0000157729.59754.09. [DOI] [PubMed] [Google Scholar]
- 22.Omoigui NA, Miller DP, Brown KJ, Annan K, Cosgrove D, Lytle B, Loop F, Topol EJ. Outmigration for coronary bypass surgery in an era of public dissemination of clinical outcomes. Circulation. 1996;93:27–33. doi: 10.1161/01.cir.93.1.27. [DOI] [PubMed] [Google Scholar]
- 23.Peterson ED, DeLong ER, Jollis JG, Muhlbaier LH, Mark DB. The effects of new york’s bypass surgery provider profiling on access to care and patient outcomes in the elderly. J Am Coll Cardiol. 1998;32:993–999. doi: 10.1016/s0735-1097(98)00332-5. [DOI] [PubMed] [Google Scholar]
- 24.Moscucci M, Eagle KA, Share D, Smith D, De Franco AC, O’Donnell M, Kline-Rogers E, Jani SM, Brown DL. Public reporting and case selection for percutaneous coronary interventionsan analysis from two large multicenter percutaneous coronary intervention databases. J Am Coll Cardiol. 2005;45:1759–1765. doi: 10.1016/j.jacc.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 25.Lindenauer PK, Remus D, Roman S, Rothberg MB, Benjamin EM, Ma A, Bratzler DW. Public reporting and pay for performance in hospital quality improvement. New Eng J Med. 2007;356:486–496. doi: 10.1056/NEJMsa064964. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.