Abstract
Living kidney donation is declining in the United States. We examined longitudinal trends in living donation as a function of median household income and donor relation to assess the effect of financial barriers on donation in a changing economic environment. The zip code–level median household income of all 71,882 living donors was determined by linkage to the 2000 US Census. Longitudinal changes in the rate of donation were determined in income quintiles between 1999 and 2004, when donations were increasing, and between 2005 and 2010, when donations were declining. Rates were adjusted for population differences in age, sex, race, and ESRD rate using multilevel linear regression models. Between 1999 and 2004, the rate of growth in living donation per million population was directly related to income, increasing progressively from the lowest to highest income quintile, with annualized changes of 0.55 (95% confidence interval [95% CI], 0.14 to 1.05) for Q1 and 1.77 (95% CI, 0.66 to 2.77) for Q5 (P<0.05). Between 2005 and 2010, donation declined in Q1, Q2, and Q3; was stable in Q4; and continued to grow in Q5. Longitudinal changes varied by donor relationship, and the association of income with longitudinal changes also varied by donor relationship. In conclusion, changes in living donation in the past decade varied by median household income, resulting in increased disparities in donation between low- and high-income populations. These findings may inform public policies to support living donation during periods of economic volatility.
Keywords: Epidemiology and outcomes, kidney donation, economic impact
For patients with ESRD, living-donor kidney transplantation is the preferred therapy because it allows for timely transplantation and is associated with superior outcomes compared with deceased-donor transplantation or dialysis.1,2 The expanded use of living-donor transplantation in the 1990s (a 125% increase between 1990 and 19993) was an important strategy to address the increasing demand for kidney transplantation, while efforts to expand deceased-donor kidney transplantation provided a more modest (10%3) increase in transplantable organs during the same time period. Since 2005, however, living-donor transplantation has declined in the United States for uncertain reasons.
Given that lower-income populations have lower rates of live kidney donation4 and >20% of living kidney donors report financial hardship after donation,5 it is possible that the financial implications of living donation may have contributed to the decline in living-donor transplantation. The costs of living donation include travel, lodging, and services, such as child or elder care, as well as lost wages. Costs as high as $20,000 have been reported, with an average estimated cost of $5000.6 Although many states have developed mechanisms to at least partially reimburse these costs, these initiatives have been inconsistently associated with an increase in living donation.7 To further understand the recent retraction in living donation and inform future health policy initiatives to address the financial costs of living donation, we determined the association of donor income with longitudinal changes in living kidney donation.
Results
Income Quintiles
The 33,178 zip codes in the US Census were grouped into the following income quintiles: Q1 (<$30,962; n=9610 zip codes); Q2 ($30,962–$37,314; n=7815 zip codes); Q3 ($37,315–%44,723; n=6098 zip codes); Q4 ($44,724–$56,580; n=4814 zip codes); Q5 (>$56,580; n=3759 zip codes).
Table 1 compares the characteristics of living donors between 1999–2004 and 2005–2010 by income quintiles. In all income quintiles, the proportion of living related donors declined while the proportion of unrelated donors increased and the proportion of spousal donors remained unchanged. In each income category, most donors donated to recipients within the same income category (data not shown).
Table 1.
Characteristics of living kidney donors between 1999–2004 and 2005–2010 in each income quintile
| Characteristic | 1999–2004 | 2005–2010 | P Value |
|---|---|---|---|
| Q1 (n=11,100 living donors) | a | ||
| Mean age±SD (yr) | 38±11 | 39±11 | <0.001 |
| Women (%) | 58 | 58 | 0.75 |
| Race (%) | <0.001 | ||
| White | 51 | 52 | |
| Black | 26 | 22 | |
| Other | 23 | 26 | |
| Donor relation (%) | <0.001 | ||
| Related | 76 | 64 | |
| Spousal | 10 | 12 | |
| Unrelated | 14 | 24 | |
| Q2 (n=12,655 living donors) | |||
| Mean age±SD (yr) | 39±11 | 40±11 | <0.001 |
| Women (%) | 59 | 60 | 0.10 |
| Race (%) | <0.001 | ||
| White | 72 | 70 | |
| Black | 15 | 14 | |
| Other | 13 | 16 | |
| Donor relation (%) | <0.001 | ||
| Related | 72 | 59 | |
| Spousal | 11 | 13 | |
| Unrelated | 17 | 28 | |
| Q3 (n=14,390 living donors) | |||
| Mean age±SD (yr) | 39±11 | 40±11 | <0.001 |
| Women (%) | 59 | 60 | 0.02 |
| Race (%) | <0.001 | ||
| White | 73 | 73 | |
| Black | 13 | 12 | |
| Other | 14 | 15 | |
| Donor relation (%) | <0.001 | ||
| Related | 70 | 60 | |
| Spousal | 11 | 12 | |
| Unrelated | 19 | 28 | |
| Q4 (n=16,353 living donors) | |||
| Mean age±SD (yr) | 40±10 | 41±11 | <0.001 |
| Women (%) | 59 | 61 | 0.08 |
| Race (%) | <0.001 | ||
| White | 76 | 74 | |
| Black | 11 | 11 | |
| Other | 13 | 15 | |
| Donor relation (%) | <0.001 | ||
| Related | 69 | 58 | |
| Spousal | 12 | 13 | |
| Unrelated | 19 | 29 | |
| Q5 (n=17,384 living donors) | |||
| Mean age±SD (yr) | 42±11 | 43±11 | <0.001 |
| Women (%) | 58 | 61 | <0.001 |
| Race (%) | <0.001 | ||
| White | 79 | 77 | |
| Black | 9 | 9 | |
| Other | 12 | 14 | |
| Donor relation (%) | <0.001 | ||
| Related | 67 | 56 | |
| Spousal | 14 | 15 | |
| Unrelated | 19 | 29 | b |
Where not stated, missing values comprised <5% of all values.
Donor income categories based on 2000 US Census data.
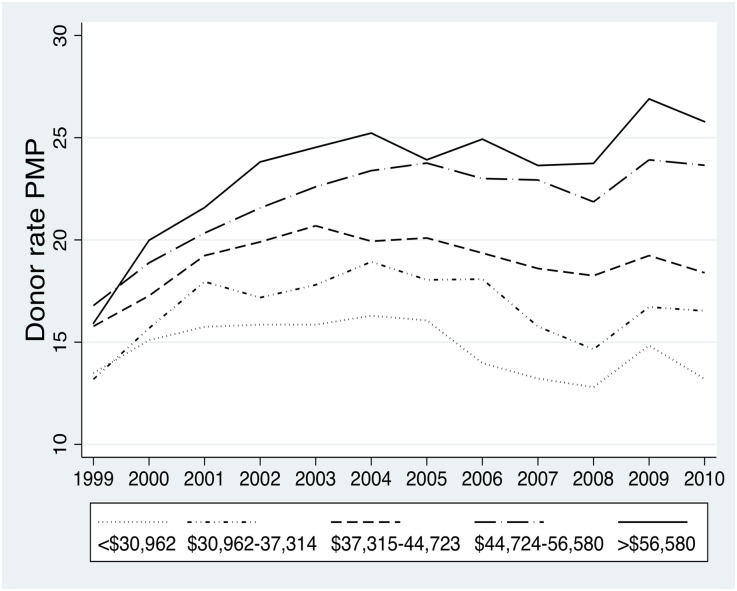
Age- and Sex-Standardized Rates of Living Donation by Income Quintile during the Study Period
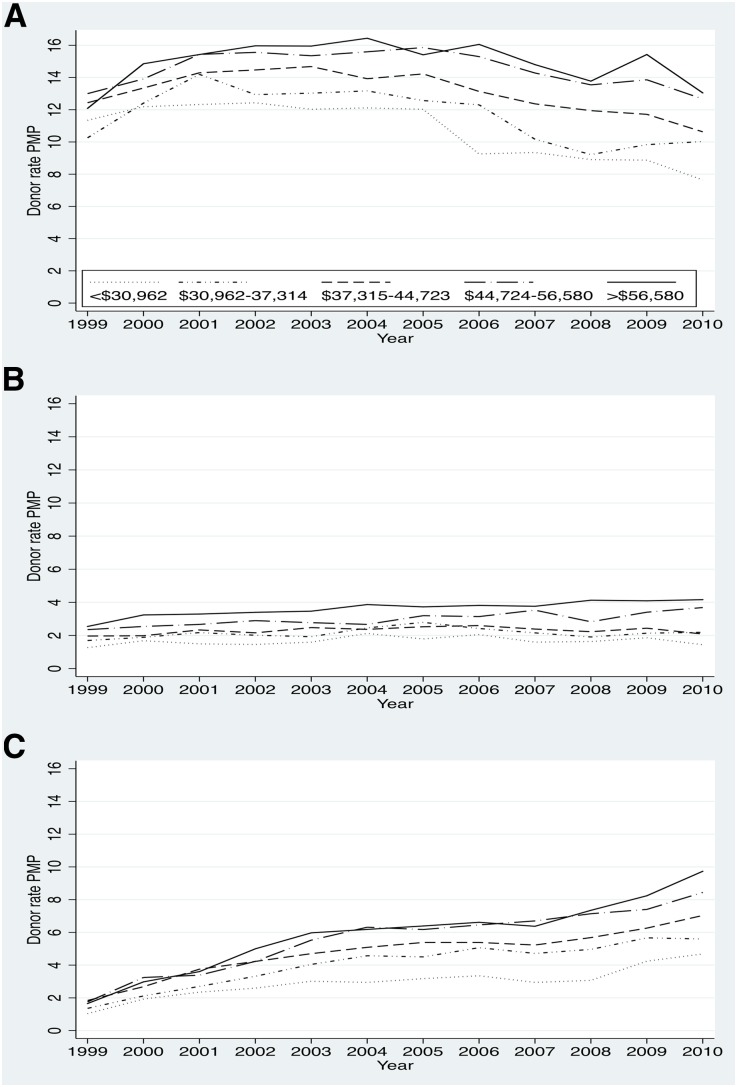
The rate of living donation (per million population) was sequentially higher in each income quintile (Q1–Q5) (Figure 1), and this pattern was consistent for living-related (LRD), living-unrelated (LURD) and spousal donations (Figure 2). The difference in living-donor rates between Q1 and Q5 increased dramatically between 1999 and 2010 (Figure 1). When stratified by race, these findings were consistent in both African American and white populations (data not shown).
Figure 1.
The difference in living donation rates per million population between the highest and lowest income quintile populations increased over time and was largest in 2010. Age- and sex-standardized living donor rates per million population (PMP) per year over time, by income quintile.
Figure 2.
Living related donation rates per million population (A) increased between 1999–2004 and then retracted between 2005–2010 in all income quintiles. Spousal donation rates (B) remained relatively stable throughout the study period, but differed by income quintile. Living unrelated donation rates (C) increased between 1999–2004 and continued to increase after 2004, but the rate of growth after 2004 appeared greater in higher income populations. Age- and sex-standardized rates of living-related donation, living-unrelated donation, and spousal unrelated donation over time, by income quintile. PMP, per million population.
Between 1999 and 2004, the adjusted annualized change in living donation increased in all income quintiles (Table 2). In a combined model that directly compared the change in living donation between income quintiles, the increase in living donation was statistically higher (P<0.05) in Q2, Q3, Q4, and Q5 compared with Q1 (Supplemental Table 1).
Table 2.
Adjusted annualized change in living kidney donation (per million population per year) between 1999–2004 and 2005–2010, stratified by income quintile
| Income Quintilesa | 1999–2004 | 2005–2010 |
|---|---|---|
| Q1 (<$30,962) | 0.55 (0.14 to 1.05)b | −0.56 (−1.01 to −0.14)b |
| Q2 ($30,962–$37,314) | 1.03 (0.48 to 1.57)b | −0.50 (−0.97 to −0.18)b |
| Q3 ($37,315–$44,723) | 1.10 (0.76,1.43)b | −0.40 (−0.56 to −0.32)b |
| Q4 ($44,724–$56,580) | 1.40 (1.33 to 1.49)b | 0.11 (−0.21 to 0.31) |
| Q5 (>$56,580) | 1.77 (0.66 to 2.27)b | 0.23 (0.17 to 0.45)b |
Multilevel linear regression model adjusted for donor age, sex, and race; population age, sex, and race; ESRD rate standardized for age and sex; and RUCA, clustered by state of residence. Values in parentheses are 95% confidence intervals.
Donor income categories based on 2000 US Census data.
P<0.05.
Between 2005 and 2010, living donation declined in Q1, Q2, and Q3 (Table 2); was stable in Q4; and increased in Q5 (Table 2). When directly compared with Q1, the change in living donation in Q4 and Q5 differed significantly (P<0.05) from that in Q1 (Supplemental Table 1).
Changes in LRD, LURD, and Spousal Donation between 1999–2004 and 2005–2010, by Income Quintile
Between 1999 and 2004, the adjusted annualized change in LRD increased in all income quintiles except Q3, in which donation remained stable (Table 3). In contrast, between 2005 and 2010, LRD decreased in all income quintiles with the exception of Q2 and Q5 (Table 3). In a direct comparison between income quintiles, the change in LRD did not significantly differ between income groups during 1999–2004 and 2005–2010 except Q5 during the 1999–2004 period (Supplemental Table 2).
Table 3.
Adjusted annualized in living-related donation, living-unrelated donation, and spousal donation (per million population per year) between 1999–2004 and 2005–2010, stratified by income quintile
| Income Quintilesa | Living-Related Donation | Living-Unrelated Donation | Spousal Donation | |||
|---|---|---|---|---|---|---|
| 1999–2004 | 2005–2010 | 1999–2004 | 2005–2010 | 1999–2004 | 2005–2010 | |
| Q1 (<$30,962) | 0.32 (0.22 to 0.64)b | −1.05 (−1.61 to −0.50)b | 0.37 (−0.22 to 0.96) | 0.24 (−0.01,0.49) | 0.06 (−0.19 to 0.31) | −0.21 (−0.53 to −0.13)b |
| Q2 ($30,962–$37,314) | 0.82 (0.27 to 1.78)b | −0.49 (−1.61 to 0.64) | 0.50 (0.28 to 0.71)b | 0.21 (−0.14 to 1.87) | 0.07 (−0.18 to 0.33) | −0.25 (−0.47 to −0.03)b |
| Q3 ($37,315–$44,723) | 0.22 (−0.41 to 0.65) | −1.01 (−2.52 to −0.48)b | 1.04 (0.32 to 1.76)b | 0.22 (−0.88 to 0.43) | 0.08 (−0.10 to 0.28) | −0.15 (−0.45 to 0.15) |
| Q4 ($44,724–$56,580) | 1.12 (0.40 to 1.85)b | −0.57 (−1.09 to −0.08)b | 1.00 (0.76 to 1.24)b | 0.62 (0.16 to 1.08)b | 0.07 (−0.09 to 0.22) | 0.21 (−0.04 to 0.47) |
| Q5 (>$56,580) | 0.94 (0.47 to 1.46)b | −0.38 (−1.19 to 0.43) | 2.03 (0.53 to 3.54)b | 1.10 (0.75 to 1.46)b | 0.27 (0.07 to 0.48)b | 0.31 (0.00 to 0.62)b |
Multilevel linear regression model adjusted for donor age, sex, and race; population age, sex, and race; ESRD rate standardized for age and sex; and RUCA, clustered by state of residence. Values in parentheses are 95% confidence intervals.
Donor income categories based on 2000 US Census data.
P<0.05.
Between 1999 and 2004, LURD increased in all income quintiles except Q1 (Table 3). Between 2005 and 2010, LURD continued to increase in Q4 and Q5 and was stable in Q1, Q2, and Q3 (Table 3). In a direct comparison between income quintiles, the increase in LURD in Q5 was statistically higher (P<0.05) than that in Q1 in both time periods (1999–2004 and 2005–10) (Supplemental Table 2).
Between 1999 and 2004, spousal donation increased in Q5 and was stable in all other income quintiles (Table 3). Between 2005 and 2010, spousal donation declined in Q1 and Q2, was stable in Q3 and Q4, and increased in Q5 (Table 3). In a direct comparison between income quintiles, the change in spousal donation between 1999 and 2004 was not statistically different between income quintiles. Between 2005 and 2010, the change in spousal donation in Q4 and Q5 was statistically higher (P<0.05) than that in Q1 (Supplemental Table 2).
Discussion
The benefits of living donation to patients with ESRD and the health care system have been well described, with one living kidney donation estimated to result in a net increase of 2–3.5 quality-adjusted life-years and a net health care savings of $100,000.5 Therefore, understanding the recent decline in living donation is important.
In this analysis of all living kidney donors in the United States between 1999 and 2010, income was strongly associated with donation, with higher rates of donation observed in higher income populations throughout the entire study period. Between 1999 and 2004, when living donation was increasing, the rate of increase was slowest in low-income populations; however, between 2005 and 2010, when living donation was decreasing, the decline in donation was most rapid among low-income populations. As a result, the difference in living donation rates between low- and high- income populations substantially increased over time. This volatility in living donation rates, particularly in low-income populations, suggests that health policies are needed to protect against rapid declines in donation.
Factors contributing to the growth of living donation between 1999 and 2004 included advancement of minimally invasive surgical techniques allowing for more rapid postsurgical recovery, increased patient education, and insufficient numbers of deceased donors to meet the demand for kidney transplantation. The marked differences in the growth of living donation between income groups suggest that the financial implications of living donation were a significant barrier to donation even during this period of economic prosperity. Additional factors that may have contributed to the disparate growth in living donation between income groups during this time period include a higher prevalence of obesity, diabetes, and other chronic health conditions, which are relative or absolute contraindications to living donation in low-income populations8–14; a higher proportion of individuals without health insurance in low-income populations; and differences in health literacy between income groups15—with variable penetrance of initiatives to increase living donation in different income groups.
Between 2005 and 2010, the actual retraction in living donation was confined to the lowest three income groups (Q1–Q3), while donation was maintained in Q4—and continued to grow, albeit at a reduced rate—in the highest income group (Q5). Although the retraction in living donation began to occur during a period of economic stability, its ongoing retraction may be related to the increased economic volatility in the United States. During this period of economic uncertainty, the costs of living donation, which amount to more than 1 month’s salary for most donors, may deter otherwise willing individuals in lower-income groups from pursuing donation.
In addition to financial constraints of donors, recipient factors may also have contributed to the decline in living donation. As in a previous analysis,16 we found that most donors and recipients had similar median household incomes. Therefore, potential recipients may not have been in a position to assist with donation-related expenses due to their own financial concerns. Recipients may also be less able to proactively work toward a living-donor transplant and may be less willing to approach potential donors if they believe donation will subject the donor to financial hardship.
While lower-income populations experienced the most dramatic retraction in donation, higher-income populations still experienced a slowdown in donation after 2005. In these more affluent populations, the actual costs of donation may not have been a deterrent, but instead factors such as uncertainty regarding job security and the feasibility of taking time off from work may have been a factor.
In 2007, the National Living Donor Assistance Center was established with the support of the US Health Resources and Services Administration and the American Society of Transplant Surgeons to support persons who want to donate a kidney but cannot afford the travel or subsistence expense associated with donation. In October 2007, transplant programs across the United States were invited to register with the program. Since inception of the Center, nearly 240 programs have enrolled and support has been provided to >2000 donors. However, this initiative is limited to persons with low incomes and is restricted to travel and lodging, while compensation for lost wages is not permitted. On the basis of our findings, more broad-based mechanisms of removing financial disincentives, including those that reimburse lost wages for all donors or ensure job stability after donation, may alleviate some of the financial stressors related to donation, particularly during periods of economic stress. Although it is tempting to speculate that introduction of overt financial incentives for donation may also be beneficial in avoiding fluctuations in donation, it is unclear whether this would minimize or aggravate the income disparities we describe in living donation. The merits of financial incentives, therefore, cannot be determined in the absence of a study trialing this.
The association of income with longitudinal changes in living donation varied by the relationship between the donor and recipient: LRDs, which include donation from siblings, parents, and adult children to their parents, declined the most between 2005 and 2010, but neither the increase in LRDs between 1999 and 2004 nor the decrease in LRDs between 2005 and 2010 varied significantly by income quintile. For sibling donations, the decline may, in part, be related to an aging ESRD population,6 leading to recipients having fewer medically eligible potential sibling donors. The decline in parental donations may be partly attributed to changes in organ allocation policy that made it easier for pediatric patients with renal failure to obtain a deceased-donor transplant.17 The number of adult children donating to their parents has declined since 2006,6 which may reflect reluctance among older patients with ESRD to accept donations from their children or a shift in clinical practice away from acceptance of younger potential donors.6
Spousal donation was largely stable during the study period. However, changes in spousal donation after 2005 were more closely related to income than were changes in LRDs: Spousal donations decreased in lower-income populations (Q1, Q2) but remained stable in higher-income groups (Q3, Q4) and increased in the highest-income group (Q5). Because spouses probably reside in the same household, longitudinal changes in spousal donations may be the most prone to changes in economic stability compared with live donations between family members who may not reside in the same household.
In contrast to donations within families (i.e., LRDs or spousal donations), LURDs retracted the least, with continued overall growth after 2005. Whereas familial donors may in part be motivated by the fact that restoring health to the recipient may improve the financial status of the family unit, unrelated donors would not be motivated by such considerations. We therefore anticipated that LURDs would be most vulnerable to economic volatility and were surprised to find that they were less susceptible to economic changes over time. These findings suggest that compared with LRDs, LURDs may be less affected by economic uncertainty, perhaps because they are separated from the financial stressor related to ESRD in the recipient household.
The strengths of this analysis are that it includes all living donors in the United States with a valid zip code and directly examined longitudinal changes in living donor transplantation from the donor perspective, after adjustment for age, sex, race, and geographic differences in ESRD. All analyses were conducted at the population level and may not apply to individual donors. Zip codes are frequently used to determine median household income, and this approach assumes the same income for individuals living in a given zip code. This assumption may be incorrect, especially in metropolitan areas. Median household income is only one indicator of socioeconomic status and may not directly relate to the financial status of an individual. However, when we examined other metrics at the zip code level, such as education, we found that these were colinear with median household income. Because we examined median household income as a categorical variable rather than a continuous variable, we were unable to account for the variability in income within each income quintile and how this relates to living donation.
Data from the 2000 US Census were used to assign median household income and determine population figures. The intent of the study was to define the income groups close to the beginning of the study period and follow longitudinal trends in these rates during follow-up. Importantly, population demographic characteristics, such as zip code income level, age, race, and sex distributions between the 2000 and 2010 US Census were relatively consistent (data not shown). It is important to note that the lack of individual-level data limits our ability to account for changes in median household income over time, particularly during periods of economic stress. A total of 5717 donors were excluded from the analysis because of missing zip code data. Missing donors included a smaller proportion of white donors compared with the donors included in the analysis, and we were unable to reliably capture other surrogates for income in these donors. Therefore, it is possible that these missing donors may have been skewed in terms of median household income.
In summary, we found that changes in living donation varied between income groups and that the disparity in living donation between low- and high-income populations has increased during recent years against the backdrop of an economic crisis. These findings suggest that the financial implications of living donation have a greater impact on low-income populations and that policies to remove financial disincentives to living donation may be important in maximizing the potential for living donation, particularly during periods of economic stability and maintaining living donation during periods of economic uncertainty. Such policies may be particularly important for donations between donors and recipients living in the same household (i.e., spousal donations or other living arrangements), in which financial resources and living costs are shared.
Concise Methods
This study was performed with the approval of our local hospital research ethics board.
Definitions
LRDs included all donations from a biologic relative, including sibling donations, parental donations, and donations from adult children. LURDs included all nonspousal, non–biologically related donors.
Data Source and Study Population
Data from the Organ Procurement Transplant Network/United Network of Organ Sharing were used to identify all living kidney donors in the United States between 1999 and 2010. After the exclusion of 5717 donors for whom income could not be determined because of missing residential zip code data, 71,882 living kidney donors were identified for study inclusion. Data from the 2000 US Census were used to define zip code quintiles based on median household income.
The characteristics of living donors were examined between 1999–2004 and 2005–2010 within each income quintile. These time frames were defined a priori on the basis of observed periods of growth and retraction in living kidney donation.6 Continuous variables were reported as mean±SD or medians (25th, 75th percentiles), while categorical variables were described using proportions. Group differences were determined using t tests, ANOVA, or the chi-squared test as appropriate.
The rate of living kidney donation per million population was determined within each income quintile by year, after adjustment for age and sex using the direct method as previously described.1,4 Living donor rates were also calculated by the type of relationship between the donor and recipient (i.e., LRDs, spousal donors, and LURDs).
Within each income quintile, multilevel linear regression models were used to determine the adjusted annualized change in the incidence of living kidney donation while living donation was increasing (i.e., between January 1, 1999, and December 31, 2004) and while living donation was declining (i.e., between January 1, 2005, and December 31, 2010). The models adjusted for donor- and population-level differences in age, sex, and race. To account for the possibility that differences in ESRD may affect living donation, we also adjusted for ESRD rate standardized for age and sex.4 Finally, to account for geographic factors that may affect the likelihood of living donation, all analyses were clustered by state of residence and adjusted for population density within each zip code using rural-urban commuting area (RUCA) codes.18,19 RUCA codes were classified into the following groups: metropolitan (cities with population of >50,000 and their associated suburban areas, RUCA codes 1.0–3.9); micropolitan (towns or cities with population of 10,000–50,000, RUCA codes 4.0–6.0); and rural (towns with a population <10,000, RUCA code >6.0).
Combined multilevel linear regression models was used to calculate the relative change in living donation in Q2, Q3, Q4, and Q5 compared with the lowest income quintile (Q1, where the change in living donation was assigned a value of zero) between 1999–2004 and 2005–2010.
Similar analyses were conducted for the outcomes of living-related donation, living-unrelated donation, and spousal donation. All analyses were performed using Stata MP 13 (StataCorp., College Station, TX).
Disclosures
None.
Supplementary Material
Acknowledgments
The data reported here have been supplied by the United Network of Organ Sharing as the contractor for the Organ Procurement and Transplantation Network, as well as the US Renal Data System. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the Organ Procurement Transplant Network or the US Government.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2014010113/-/DCSupplemental.
References
- 1.USRDS : Annual Data Report: Atlas of End Stage Renal Disease in the United States, Bethesda, MD, National Institute of Health, National Institute of Diabetes and Digestive and Kidney Disease, 2010 [Google Scholar]
- 2.Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, Klarenbach S, Gill J: Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 11: 2093–2109, 2011 [DOI] [PubMed] [Google Scholar]
- 3.National Data Report: United Network for Organ Sharing (UNOS). Available at: http://www.unos.org. Accessed March 14, 2012
- 4.Gill J, Dong J, Rose C, Johnston O, Landsberg D, Gill J: The effect of race and income on living kidney donation in the United States. J Am Soc Nephrol 24: 1872–1879, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klarenbach S, Garg AX, Vlaicu S: Living organ donors face financial barriers: A national reimbursement policy is needed. CMAJ 174: 797–798, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodrigue JR, Schold JD, Mandelbrot DA: The decline in living kidney donation in the United States: Random variation or cause for concern? Transplantation 96: 767–773, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boulware LE, Troll MU, Plantinga LC, Powe NR: The association of state and national legislation with living kidney donation rates in the United States: A national study. Am J Transplant 8: 1451–1470, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akil L, Ahmad HA: Effects of socioeconomic factors on obesity rates in four southern states and Colorado. Ethn Dis 21: 58–62, 2011 [PMC free article] [PubMed] [Google Scholar]
- 9.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A: Socioeconomic status and cardiovascular disease: Risks and implications for care. Nat Rev Cardiol 6: 712–722, 2009 [DOI] [PubMed] [Google Scholar]
- 10.Hudson CG: Socioeconomic status and mental illness: Tests of the social causation and selection hypotheses. Am J Orthopsychiatry 75: 3–18, 2005 [DOI] [PubMed] [Google Scholar]
- 11.Patzer RE, McClellan WM: Influence of race, ethnicity and socioeconomic status on kidney disease. Nat Rev Nephrol 8: 533–541, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reid JL, Hammond D, Driezen P: Socio-economic status and smoking in Canada, 1999-2006: Has there been any progress on disparities in tobacco use? Can J Public Health 101: 73–78, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sobal J, Stunkard AJ: Socioeconomic status and obesity: A review of the literature. Psychol Bull 105: 260–275, 1989 [DOI] [PubMed] [Google Scholar]
- 14.Williams CT, Latkin CA: Neighborhood socioeconomic status, personal network attributes, and use of heroin and cocaine. Am J Prev Med 32[Suppl]: S203–S210, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR: The prevalence of limited health literacy. J Gen Intern Med 20: 175–184, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gill JS, Gill J, Barnieh L, Dong J, Rose C, Johnston O, Tonelli M, Klarenbach S: Income of living kidney donors and the income difference between living kidney donors and their recipients in the United States. Am J Transplant 12: 3111–3118, 2012 [DOI] [PubMed] [Google Scholar]
- 17.Amaral S, Patzer RE, Kutner N, McClellan W: Racial disparities in access to pediatric kidney transplantation since share 35. J Am Soc Nephrol 23: 1069–1077, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Axelrod DA, Guidinger MK, Finlayson S, Schaubel DE, Goodman DC, Chobanian M, Merion RM: Rates of solid-organ wait-listing, transplantation, and survival among residents of rural and urban areas. JAMA 299: 202–207, 2008 [DOI] [PubMed] [Google Scholar]
- 19.Tonelli M, Klarenbach S, Rose C, Wiebe N, Gill J: Access to kidney transplantation among remote- and rural-dwelling patients with kidney failure in the United States. JAMA 301: 1681–1690, 2009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.