Abstract
Background
Numerous statistical models have been developed to accurately predict outcomes in multiple trauma patients. However, such trauma scoring systems reflect the patient’s physiological condition, which can only be determined to a limited extent, and are difficult to use when performing a rapid initial assessment. We studied the predictive ability of the systemic inflammatory response syndrome (SIRS) score compared to other scoring systems.
Methods
We retrospectively reviewed 229 patients with multiple trauma combined with chest injury from January 2006 to June 2011. A SIRS score was calculated for patients based on their presentation to the emergency room. The patients were divided into two groups: those with an SIRS score of two points or above and those with an SIRS score of one or zero. Then, the outcomes between the two groups were compared. Furthermore, the ability of the SIRS score and other injury severity scoring systems to predict mortality was compared.
Results
Hospital death occurred in 12 patients (5.2%). There were no significant differences in the general characteristics of patients, but the trauma severity scores were significantly different between the two groups. The SIRS scores, number of complications, and mortality rate were significantly higher in those with a SIRS score of two or above (p<0.001). In the multivariant analysis, the SIRS score was the only independent factor related to mortality.
Conclusion
The SIRS score is easily calculated on admission and may accurately predict mortality in patients with multiple traumas.
Keywords: Trauma, Mortality, Systemic inflammatory response syndrome
INTRODUCTION
Trauma is an important health problem in modern society and a leading cause of death, particularly in younger adults [1]. Mortality rates range from 7% to 45%, depending on injury severity, the presence of shock or brain injury, and physiologic reserve [2,3]. Variations in trauma outcomes might result from a number of factors including injury severity and comorbidities along with individual and trauma center-specific management systems. Many scoring systems for assessing injury severity have been developed over the past few decades. The need to improve the quality of trauma care has led researchers to develop more accurate scoring models that allow traumatologists to predict the outcomes of injured patients, such as the Injury Severity Score (ISS), New Injury Severity Score (NISS), International Classification of Disease Ninth Revision-Based Injury Severity Score, Revised Trauma Score (RTS), Glasgow Coma Scale, Trauma and Injury Severity Score (TRISS), and the systemic inflammatory response syndrome (SIRS) score. The purpose of this study was to compare the accuracy of the SIRS score with other injury severity scoring systems in predicting mortality in trauma patients.
METHODS
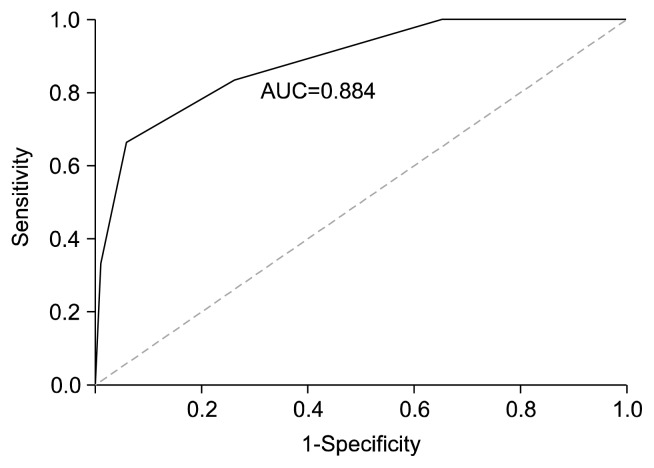
We retrospectively reviewed data on 229 patients who were hospitalized with multiple trauma combined with chest injury from January 2006 to June 2011. A SIRS score was calculated based on their presentation upon admission. One point was given for each of the following: temperature >38°C or <36°C, heart rate >90 beats per minute, respiratory rate > 20 breaths per minute, neutrophil count >12,000 cells/mcl or <4,000 cells/mcl. We used the receiver-operating characteristic analysis to determine an adequate cut-off value for the SIRS score that had a good ability to predict mortality. The receiver-operating characteristic curve showed an area under the curve of 0.884, and the best-discriminating SIRS score was between 1.5 (sensitivity=0.833, specificity=0.742) and 2.5 (sensitivity=0.667, specificity=0.94) (Fig. 1). Thus, we divided the patients into two groups based on this analysis: those with a SIRS score of two points or above (the S2OA group) and those with a score one or zero (the S1OZ group). We also calculated results for each patient using other scoring systems including the ISS, NISS, RTS, and TRISS. Patients with severe neurologic injuries were excluded. We compared the complications and mortality rates between the two groups and the ability of the SIRS score compared to other injury severity scores to predict mortality in trauma patients. All statistical analyses were performed using SPSS ver. 10.2 (SPSS Inc., Chicago, IL, USA). Differences were considered to be statistically significant if p<0.05.
Fig. 1.
Receiver-operating characteristic analysis of the systemic inflammatory response syndrome score and mortality. The area under the curve (AUC) is 0.884 with discrimination between 1.5 (sensitivity=0.833, specificity=0.742) and 2.5 (sensitivity=0.667, specificity=0.94).
RESULTS
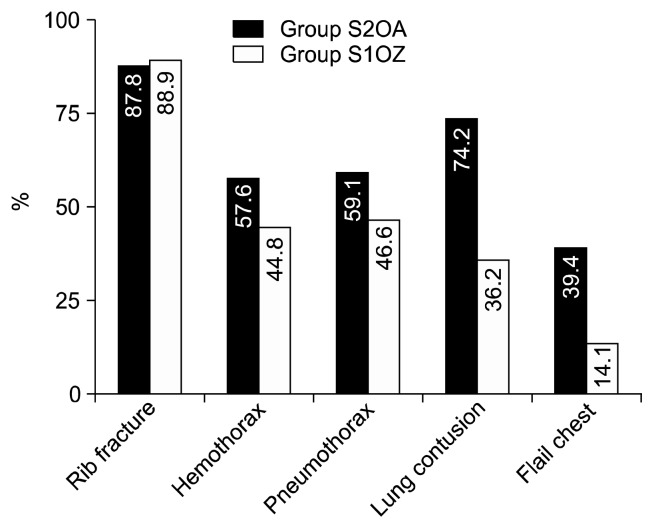
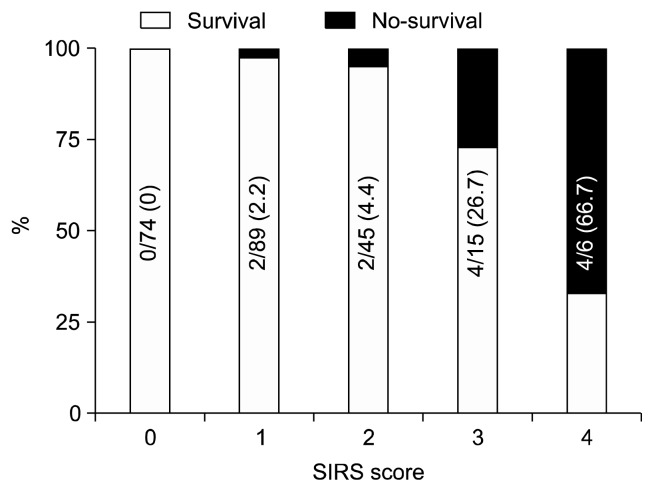
In total, 229 trauma patients presented between January 2006 and June 2011. Traffic accidents were the most common cause of trauma in both groups, and there was no overall difference across the types of trauma between the two groups (Table 1). In total, 173 patients were male (75.5%), 56 were female (24.5%), and complications occurred in 50 cases (21.8%). There were 12 deaths, resulting in a mortality rate of 5.2%. Trauma severity scores and general characteristics of all patients are shown in Table 2. The S2OA group had 66 patients (57 males and 9 females), and the S1OZ group had 163 patients (116 males and 47 females). There were no significant differences in the age, gender, past medical history, or length of emergency room stay between the S2OA and S1OZ group (Table 3). The trauma severity scores were significantly different between the two groups (Table 4). The complication and mortality rates were significantly higher for the S2OA group than for the S1OZ group (p<0.001). Lung contusions and flail chest were significantly more common in the S2OA group: 74.2% of the S2OA group had lung contusions compared to 36.2% of the S1OZ group (p<0.001), and 39.4% of the S2OA group had flail chest compared to 14.1% of the S1OZ group (p<0.001) (Fig. 2). Moreover, the SIRS score was positively correlated with mortality rate (Fig. 3). In the multivariant analysis that included the ISS, NISS, RTS, and SIRS scores, the SIRS score was the only independent factor for predicting mortality (Table 5).
Table 1.
Types of trauma presented
| Type of trauma | S2OAa) group | S1OZb) group | Total cases |
|---|---|---|---|
| Traffic accident | 51 | 106 | 157 |
| Fall | 11 | 29 | 40 |
| Slip | 2 | 9 | 11 |
| Penetrating injury | 0 | 7 | 7 |
| Assault injury | 1 | 8 | 9 |
| Compression | 1 | 4 | 5 |
| Total | 66 | 163 | 229 |
Values are presented as number.
Patients with a systemic inflammatory response syndrome score of two or above.
Patients with a systemic inflammatory response syndrome score of one or zero.
Table 2.
General characteristics of all patients
| Variable | Value |
|---|---|
| Gender (male/female) | 173/56 |
| Age (yr) | 54.2±17.6 |
| Emergency room stay (min) | 810.0±774.1 |
| Injury Severity Score | 20.7±10.5 |
| New Injury Severity Score | 27.8±11.0 |
| Revised Trauma Score | 7.78±1.34 |
| Trauma and Injury Severity Score | 8.35±11.2 |
| Systemic inflammatory response syndrome score | 1.08±1.01 |
| Complications (cases) | 50 (21.8) |
| Mortality (cases) | 12 (5.2) |
| Hospital stay (day) | 18.2±24.7 |
Values are presented as number, mean±standard deviation, or number (%).
Table 3.
| Variable | S2OA group | S1OZ group | p-value |
|---|---|---|---|
| Age (yr) | 50.8±20.5 | 55.6±16.2 | NS |
| Gender (cases) | 0.017 | ||
| Male | 57 | 116 | |
| Female | 9 | 47 | |
| Past medical history (cases) | |||
| Pulmonary tuberculosis | 4 (6.1) | 14 (8.6) | NS |
| Diabetes mellitus | 6 (9.1) | 16 (9.8) | NS |
| Hypertension | 14 (21.2) | 33 (20.2) | NS |
| Chronic obstructive pulmonary disease | 4 (6.1) | 4 (2.5) | NS |
| Emergency room stay (min) | 760.8±919.5 | 830.2±708.2 | NS |
| Ventilator care (cases) | 46 (69.7) | 40 (24.5) | <0.001 |
| Intensive care unit care | 48 (72.7) | 54 (33.1) | <0.001 |
Values are presented as mean±standard deviation, number, or number (%).
NS, not significant.
Patients with a systemic inflammatory response syndrome score of two or above.
Patients with a systemic inflammatory response syndrome score of one or zero.
Table 4.
| Variable | S2OA group | S1OZ group | p-value |
|---|---|---|---|
| Injury Severity Score | 25.2±11.2 | 18.9±9.68 | <0.001 |
| New Injury Severity Score | 33.4±11.3 | 25.5±10.0 | <0.001 |
| Revised Trauma Score | 7.42±0.60 | 7.91±1.51 | 0.01 |
| Trauma and Injury Severity Score | 13.3±14.4 | 6.34±8.93 | <0.001 |
| Systemic inflammatory response syndrome score | 2.41±0.66 | 0.55±0.49 | <0.001 |
| Complications (cases) | 32 (48.5) | 18 (11.0) | <0.001 |
| Mortality (cases) | 10 (15.2) | 2 (1.2) | <0.001 |
| Hospital stay (day) | 27.5±38.1 | 14.4±14.9 | 0.009 |
Values are presented as mean±standard deviation or number (%).
Patients with a systemic inflammatory response syndrome score of two or above.
Patients with a systemic inflammatory response syndrome score of one or zero.
Fig. 2.
Comparison of the systemic inflammatory response syndrome scores among those with a score of two or above (S2OA group) and those with a score of one or zero (S1OZ group) according to the type of chest trauma. Lung contusion and flail chest were significantly more frequent in the S2OA group.
Fig. 3.
Mortality rate according to the systemic inflammatory response syndrome (SIRS) score, which was positively correlated with mortality. Values are presented as number (%).
Table 5.
Comparison of trauma scores for mortality prediction
| System | Beta-value | Standard error | Hazard ratio | p-value |
|---|---|---|---|---|
| Injury Severity Score | 0.003 | 0.065 | 1.003 (0.883–1.138) | 0.966 |
| New Injury Severity Score | 0.020 | 0.055 | 1.020 (0.915–1.137) | 0.722 |
| Revised Trauma Score | 1.255 | 0.850 | 3.507 (0.662–18.567) | 0.140 |
| Trauma and Injury Severity Score | 0.035 | 0.033 | 1.036 (0.970–1.106) | 0.293 |
| Systemic inflammatory response syndrome score | 1.648 | 0.434 | 5.196 (2.221–12.154) | <0.001 |
DISCUSSION
Reported mortality rates for injured patients range from 7% to 45%, depending on injury severity, the presence of shock or brain injury, and physiological reserve [2,3]. Variations in trauma outcomes might be the result of a number of factors, including injury severity and comorbidities, the management of trauma by an individual practitioner, and the systems of trauma management specific to trauma centers. A number of prognostic tools and scoring models have been proposed for multiple trauma patients at risk of mortality and can be divided into three categories: those based on anatomic injury patterns, physiologic data, or a combination of anatomic and physiologic variables. Scoring systems based on anatomic injuries include the ISS, NISS, and Ninth Revision-based Injury Severity Score [4–8]. These scoring systems can be difficult to apply during the initial patient assessment. Scoring systems based on physiologic data such as the RTS and Glasgow Coma Scale are easier to use and have been widely applied to assessments in the pre-hospital setting [9,10]. Scoring systems combining anatomic and physiologic data have also been described. For instance, the TRISS combines the ISS and RTS [11–13]. However, the SIRS score is easily calculated at the patient bedside on admission and reflects the patient’s physiologic condition. The prediction of outcomes after injury has traditionally incorporated anatomic measures of injury severity, but many studies have documented that inclusion of physiologic and shock measures can improve the accuracy of anatomic-based models [14]. Trauma induces a major systemic inflammatory response immediately after injury. The physiologic course after an acute trauma is a dynamic process that is not accounted for in anatomic-based scoring systems [14]. In particular, tissue hypoperfusion after acute injury can have a tremendous impact on survival. An early retrospective investigation of trauma patients admitted for more than 48 hours found a markedly higher incidence of SIRS in trauma patients with multi-organ dysfunction syndrome than that in those without multi-organ dysfunction syndrome [15]. The variables of the SIRS scoring system are fever or hypothermia, tachycardia, tachypnea, and an abnormal white blood cell count [16]. The use of the SIRS score to determine illness severity has been investigated in several patient populations. The Physiologic Trauma Score was introduced in 2002 and incorporated the SIRS score, RTS, and Glasgow Coma Scale into a simple bedside calculation to predict mortality at the time of trauma admission [17]. The SIRS score is also easily calculated on admission. A previous study by Napolitano et al. [18] analyzed 4,887 consecutive trauma patients admitted to a level-1 trauma center and determined the presence of SIRS, as indicated by a SIRS score of two or greater, to be an independent predictor of mortality, controlling for age and ISS. We sought to examine the predictive value of the SIRS score for trauma mortality. Our results demonstrate a predictive relationship between the SIRS score and mortality in multiple trauma patients.
In conclusion, our single-institution study has provided validation of the SIRS score as a mortality predictor in multiple trauma patients, documenting comparable predictive ability to other trauma score systems. The mortality rate and number of complications were significantly higher in the S2OA group. In our multivariant analysis, the SIRS score was the only significant independent factor for mortality prediction. Therefore, the SIRS score is a useful tool for predicting outcomes in multiple trauma patients.
ACKNOWLEDGMENTS
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan) (Fund No.KTCS04-012).
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Trunkey DD. Trauma: accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease: among the prescribed remedies are improved preventive efforts, speedier surgery and further research. Sci Am. 1983;249:28–35. [PubMed] [Google Scholar]
- 2.Baxt WG, Moody P. The differential survival of trauma patients. J Trauma. 1987;27:602–6. doi: 10.1097/00005373-198706000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Chawda MN, Hildebrand F, Pape HC, Giannoudis PV. Predicting outcome after multiple trauma: which scoring system? Injury. 2004;35:347–58. doi: 10.1016/S0020-1383(03)00140-2. [DOI] [PubMed] [Google Scholar]
- 4.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 5.Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma. 1988;28:69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43:922–5. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Brenneman FD, Boulanger BR, McLellan BA, Redelmeier DA. Measuring injury severity: time for a change? J Trauma. 1998;44:580–2. doi: 10.1097/00005373-199804000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Balogh Z, Offner PJ, Moore EE, Biffl WL. NISS predicts postinjury multiple organ failure better than the ISS. J Trauma. 2000;48:624–7. doi: 10.1097/00005373-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the Trauma Score. J Trauma. 1989;29:623–9. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Langfitt TW. Measuring the outcome from head injuries. J Neurosurg. 1978;48:673–8. doi: 10.3171/jns.1978.48.5.0673. [DOI] [PubMed] [Google Scholar]
- 11.Rutledge R, Osler T, Emery S, Kromhout-Schiro S. The end of the Injury Severity Score (ISS) and the Trauma and Injury Severity Score (TRISS): ICISS, an International Classification of Diseases, ninth revision-based prediction tool, outperforms both ISS and TRISS as predictors of trauma patient survival, hospital charges, and hospital length of stay. J Trauma. 1998;44:41–9. doi: 10.1097/00005373-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Hannan EL, Farrell LS, Gorthy SF, et al. Predictors of mortality in adult patients with blunt injuries in New York State: a comparison of the Trauma and Injury Severity Score (TRISS) and the International Classification of Disease, Ninth Revision-based Injury Severity Score (ICISS) J Trauma. 1999;47:8–14. doi: 10.1097/00005373-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Bouillon B, Lefering R, Vorweg M, Tiling T, Neugebauer E, Troidl H. Trauma score systems: Cologne Validation Study. J Trauma. 1997;42:652–8. doi: 10.1097/00005373-199704000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Guzzo JL, Bochicchio GV, Napolitano LM, Malone DL, Meyer W, Scalea TM. Prediction of outcomes in trauma: anatomic or physiologic parameters? J Am Coll Surg. 2005;201:891–7. doi: 10.1016/j.jamcollsurg.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 15.Smail N, Messiah A, Edouard A, et al. Role of systemic inflammatory response syndrome and infection in the occurrence of early multiple organ dysfunction syndrome following severe trauma. Intensive Care Med. 1995;21:813–6. doi: 10.1007/BF01700964. [DOI] [PubMed] [Google Scholar]
- 16.Knaus W, Wagner D, Draper E. APACHE III study design: analytic plan for evaluation of severity and outcome in intensive care unit patients: development of APACHE. Crit Care Med. 1989;17(12 Pt 2):S181–5. [PubMed] [Google Scholar]
- 17.Kuhls DA, Malone DL, McCarter RJ, Napolitano LM. Predictors of mortality in adult trauma patients: the physiologic trauma score is equivalent to the Trauma and Injury Severity Score. J Am Coll Surg. 2002;194:695–704. doi: 10.1016/s1072-7515(02)01211-5. [DOI] [PubMed] [Google Scholar]
- 18.Napolitano LM, Ferrer T, McCarter RJ, Jr, Scalea TM. Systemic inflammatory response syndrome score at admission independently predicts mortality and length of stay in trauma patients. J Trauma. 2000;49:647–52. doi: 10.1097/00005373-200010000-00011. [DOI] [PubMed] [Google Scholar]