Abstract
Pseudoaneurysm of the right ventricular outflow tract (RVOT) has been reported as a rare complication of RVOT reconstruction performed using conduit replacement or patch repair. Rarely, it may present alongside symptoms secondary to the compression of adjoining mediastinal structures. We report the case of a patient who developed a symptomatic RVOT pseudoaneurysm one month after a total correction of tetralogy of Fallot. In the present case, superior vena cava syndrome was caused by compression of the superior vena cava, which was a very unusual presentation.
Keywords: Congenital heart disease (CHD); Tetralogy of Fallot; Aneurysm, false; Superior vena cava syndrome
CASE REPORT
A 12-month-old girl underwent a complete repair of tetralogy of Fallot that included a ventricular septal defect closure and right ventricular outflow tract (RVOT) reconstruction. On the preoperative echocardiogram, the pulmonary annular Z score was -4.5. RVOT reconstruction was performed with an infundibulectomy, infundibular patch enlargement, pulmonary valvotomy, and pulmonary angioplasty. A thin walled Gore-Tex (W.L. Gore and Associates, Flagstaff, AZ, USA) vascular graft was used as the material for an infundibular patch, which was attached to the RVOT with a continuous 6-0 poly-propylene (Surgipro; Covidien, Mansfield, MA, USA) running suture.
On intraoperative transesophageal echocardiography, the pulmonary valve residual pressure gradient was 49 mmHg and systolic pressure ratio between the right and left ventricles was 0.8 mmHG. However, we could not place a trans-annular patch because the patient had an anomalous coronary artery crossing the RVOT. The left anterior descending artery originated from the right coronary artery crossing the RVOT (Fig. 1). Therefore, we did not continue the procedure and treated the patient with a beta-blocker. Her postoperative course was uneventful, and she was discharged on postoperative day six.
Fig. 1.
An abnormal coronary artery is shown crossing the right ventricular outflow tract.
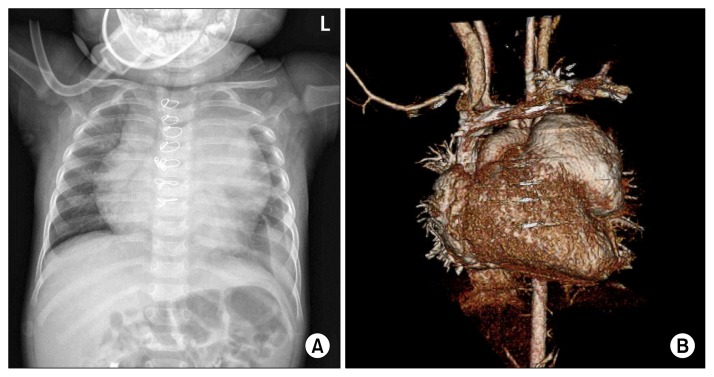
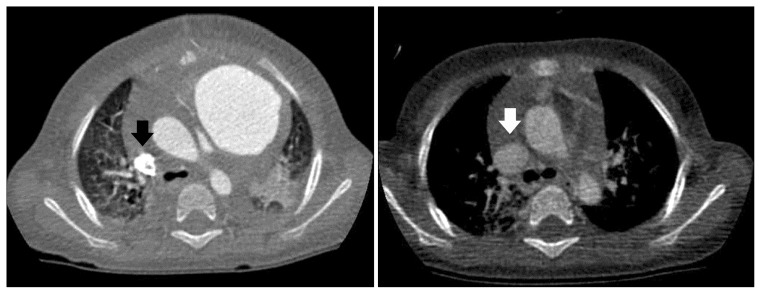
One month later, the patient was readmitted to Kyungpook National University Hospital complaining of cough, shortness of breath, and facial and upper extremity oedema over the previous three days. Chest radiography revealed enlargement of the left upper cardiac border with a left pleural effusion (Fig. 2A). In addition, transthoracic echocardiography showed a large aneurysmal dilatation of the RVOT with narrowing of the superior vena cava and main pulmonary artery, secondary to compression by the aneurysm. Colour Doppler images revealed decreased blood flow in the superior vena cava. Computed tomography (CT) showed a narrow communication between the RVOT and an aneurysmal sac. Through these findings, we confirmed an RVOT pseudoaneurysm measuring 55×51×45 mm (Fig. 2B). The superior vena cava was narrow compared to previous CT imaging (Fig. 3).
Fig. 2.
(A) Chest radiography revealed enlargement of the left upper cardiac border with left pleural effusion. (B) Computed tomography showed a right ventricular outflow tract pseudoaneurysm measuring 55×51×45 mm.
Fig. 3.
Computed tomography showed a narrowed superior vena cava compared with the previous image.
Because of the risk of a spontaneous rupture, we elected to perform emergency surgery. A careful median resternotomy was performed. A large serous pericardial and pleural effusion was present around the RVOT. Under cardiopulmonary bypass, the aneurysmal sac was opened, revealing patch dehiscence at the proximal suture line between the infundibular patch and the ventriculotomy site. Communication between the RVOT and the pseudoaneurysm was confirmed, and the previous infundibular patch and all aneurysmal tissue were excised. Another RVOT reconstruction was performed using the same method and type of infundibular patch. However, in this procedure, the infundibular patch was attached to the RVOT with multiple interrupted pledgeted mattress sutures as well as full-thickness bites in the suturing of the right ventricular wall. Intraoperative transesophageal echocardiography showed residual pulmonary stenosis (pressure gradient, 36 mmHg) and normal right ventricular systolic function. The patient’s postoperative course was uneventful, and both her facial and upper extremity oedema improved. She was discharged on postoperative day 10. Postoperative transthoracic echocardiography, performed eight months after the reoperation, showed residual pulmonary stenosis (pressure gradient, 36 mmHg) without any indication of the development of an aneurysm.
DISCUSSION
Pseudoaneurysm of the RVOT is an infrequent complication of cardiovascular surgical procedures that involve both a right ventriculotomy and RVOT reconstruction with patch repair or conduit replacement [1–3]. The pathogenesis and aetiology of pseudoaneurysms have been described as related either to obstructive RVOT or to elevated right ventricular systolic pressure, leading to mechanical strain at the proximal suture line. However, other contributing factors such as pulmonary insufficiency, suture material and technique, trauma, complete heart block, and infection have also been implicated [1–3]. Regardless of the aetiology, a pseudoaneurysm arises from the small dehiscence of a portion of the reconstructed RVOT, permitting blood leakage into the surrounding space and resulting in a pericardial haematoma [1–4]. In this case, the pseudoaneurysm may have been caused by residual RVOT obstruction, especially because of inappropriate suture techniques, such as continuous running sutures and partial-thickness sutures in the right ventricular wall. Follow-up transthoracic echocardiography, performed eight months after reoperation, showed no aneurysmal changes in the RVOT.
Pseudoaneurysms may remain asymptomatic and are found incidentally during regular follow-up examinations [2,3]. However, pseudoaneurysms progressively increase in size and may present, albeit rarely, alongside symptoms secondary to the compression of adjoining mediastinal structures, rupture, thromboembolism, and infection [1–4]. In the present case, superior vena cava syndrome was caused by compression of the superior vena cava, which was a very unusual presentation.
Transthoracic echocardiography has been reported as a reliable method for diagnosing pseudoaneurysms [1–4]. However, it does not provide detailed information about the anatomical relationship between the pseudoaneurysm and surrounding structures. We found CT to be very helpful in evaluating the location and size of the pseudoaneurysm and determining its anatomical relationships. CT was also useful in evaluating the safety of performing another sternotomy in light of the possible need for femoral or neck vessel cannulation before another sternotomy. Preoperative magnetic resonance imaging may also provide information helpful in choosing the best surgical approach [5]. However, magnetic resonance imaging is more time-consuming than CT, and is difficult to perform in haemodynamically unstable patients.
Compared to true aneurysms, pseudoaneurysms pose an increased risk of rupture because of the absence of myocardial tissue in their walls [3]. Therefore, they are potentially life threatening if not treated. Once diagnosed, pseudoaneurysms require either reoperation or another intervention.
In conclusion, a pseudoaneurysm in a surgically reconstructed RVOT is a rare but potentially fatal complication. It should always be suspected in patients with the relevant symptoms, and such patients must be followed up closely. Precise and careful preoperative assessment, using echocardiography and CT, is important for ensuring the safety of surgery performed on these patients. Reoperation can be performed safely, with low risk of mortality or morbidity.
ACKNOWLEDGMENTS
This research was sponsored by Kyungpook National University Research Fund, 2012.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Sah S, Berdjis F, Valdez S, Gates R. Pseudoaneurysm of surgically reconstructed right ventricular outflow tract. World J Pediatr Congenit Heart Surg. 2013;4:116–9. doi: 10.1177/2150135112458696. [DOI] [PubMed] [Google Scholar]
- 2.Pillai SK, Reddy HP, Kulkarni S, Murthy KS, Cherian KM. Pseudoaneurysm of homograft placed in right ventricular outflow tract. Ann Thorac Surg. 2004;78:1068–70. doi: 10.1016/S0003-4975(03)01583-2. [DOI] [PubMed] [Google Scholar]
- 3.Antal AD, Cikirikcioglu M, Myers PO, Didier D, Kalangos A. Respiratory distress after surgery of RVOT pathologies: a word of caution on pseudoaneurysm development. Thorac Cardiovasc Surg. 2010;58:356–8. doi: 10.1055/s-0029-1185883. [DOI] [PubMed] [Google Scholar]
- 4.Calabro R, Santoro G, Pisacane C, Pacileo G, Russo MG, Vosa C. Repeat syncopal attacks due to postsurgical right ventricular pseudoaneurysm. Ann Thorac Surg. 1999;68:252–4. doi: 10.1016/s0003-4975(99)00497-x. [DOI] [PubMed] [Google Scholar]
- 5.Murashita T, Hatta E, Imamura M, Yasuda K. Giant pseudoaneurysm of the right ventricular outflow tract after repair of truncus arteriosus: evaluation by MR imaging and surgical approach. Eur J Cardiothorac Surg. 2002;22:849–51. doi: 10.1016/s1010-7940(02)00446-3. [DOI] [PubMed] [Google Scholar]