Abstract
Background
Few studies have examined the association between the food environment and adiposity in early childhood, a critical time for obesity prevention. The objective of this study was to examine the longitudinal association between neighborhood food environment and adiposity among low-income preschool-aged children in a major metropolitan region in the United States.
Methods
The study sample was 32,172 low-income preschool-aged children in Los Angeles County who had repeated weight and height measurements collected between ages 2 and 5 years through a federal nutrition assistance program. We conducted multilevel longitudinal analyses to examine how spatial densities of healthy and unhealthy retail food outlets in the children’s neighborhoods were related to adiposity, as measured by weight-for-height z-score (WHZ), while controlling for neighborhood-level income and education, family income, maternal education, and child’s gender and race/ethnicity.
Results
Density of healthy food outlets was associated with mean WHZ at age 3 in a non-linear fashion, with mean WHZ being lowest for those exposed to approximately 0.7 healthy food outlets per square mile and higher for lesser and greater densities. Density of unhealthy food outlets was not associated with child WHZ.
Conclusions
We found a non-linear relationship between WHZ and density of healthy food outlets. Research aiming to understand the socio-behavioral mechanisms by which the retail food environment influences early childhood obesity development is complex and must consider contextual settings.
Keywords: Food environment, childhood obesity, Los Angeles County
INTRODUCTION
The built environment influences healthy food accessibility and opportunities for exercise, and has been linked to obesity risk among adults.[1-3] However, its role in obesity development among children has been less studied. Findings from the few studies reporting associations between the food-related aspects of the built environment (“food environment”) and child obesity are inconsistent.[4-11] Among school-aged children, several cross-sectional[4, 5] and longitudinal[9, 10] studies have found no associations between the food environment and adiposity, while others have found the availability of supermarkets and convenience stores to be associated with lower and higher body mass index (BMI), respectively.[6, 7] Among preschool-aged children, even less is known about the role of the food environment in obesity development. To our knowledge, only three studies have looked at this association for preschool-aged children; all were cross-sectional and reported inconsistent findings.[8, 11, 12]
It could be argued that the family environment may be more important in influencing the food behaviors of children than the built environment, and that child obesity prevention efforts should focus on developing family interventions. However, it could also be argued that the neighborhood environment may influence what parents feed their young children. Given the unclear role of the built environment in influencing child obesity risk and the increasing recognition of the need to prevent obesity early in life, the aim of this study was to assess the contribution of the food environment to obesity development among preschool-aged children. Our study population was over 30,000 low-income children aged 2 to 5 years in Los Angeles County (LAC), one of the most populated and diverse regions in the United States, whose mothers had all received nutrition education from the Special Supplemental Nutrition Program for Women, Infants and Children (WIC), the second largest federal nutrition assistance program in the U.S. WIC participation reduced variation in parental nutrition education and repeated adiposity measurements on the children over time permitted longitudinal analysis.
METHODS
Child data
WIC provides food assistance and nutrition education to low-income pregnant and postpartum women and children up to age five. Our study sample was children born in the U.S. in 2003 who participated in WIC in LAC between their 2nd and 5th birthdays (2005-2008), had at least 3 weight and height measurements, and lived in census tracts (CTs) with at least 5 WIC-enrolled children (N=32,172 children, or 96,888 observations). This cohort was chosen because the children turned age 5 and therefore left the program before 2009 when a major change in the WIC program[13] that may have altered family behaviors and the neighborhood food environment occurred.[14, 15].
Child data were obtained from the WIC Data Mining Project[16], which has archived sociodemographic and anthropometric information on all children enrolled in WIC in LAC since 2002. Weight and height were measured for each child by WIC staff during recertification visits. A previous validation study comparing weight/height measurements collected by WIC staff in LAC to those collected by trained research staff found intraclass correlation coefficients of 0.93-0.99.[17] Socio-demographic information available for each child included age, gender, race/ethnicity (non-Hispanic White, Black, Asian, Hispanic), maternal language preference (English, Spanish, other), maternal educational level (less than high school, high school graduate or above), family size, and family monthly income. WIC oversaw the geocoding of participant addresses and provided the authors with participant’s residential CT rather than address to protect confidentiality. The outcome variable was weight-for-height z-score (WHZ), which was calculated from weight and height using age- and gender-specific CDC growth curves.[18] BMI (expressed as percentiles or z-scores), a commonly used adiposity indicator, is problematic for studying children’s longitudinal adiposity since BMI is correlated with height/length in children and dependent on body proportions, which change as a child grows.[19] In contrast, WHZ is independent of height at all ages and is therefore more appropriate for assessing adiposity trajectories in growing children.[20] Children with improbable WHZ (<-5 or >5) or health conditions that may have affected feeding practices were excluded from analyses (N=395).
Neighborhood data
Neighborhoods were defined by CT boundaries. While not a perfect definition of neighborhood, CTs are useful for research purposes as they can be linked to census data on socioeconomic characteristics.[21] We used median annual household income and percent of high school graduates from the American Community Survey (ACS) 2005-2009 to characterize neighborhoods.[22]
Food environment data were obtained from business listings in the National Establishment Time-Series (NETS) from Walls & Associates[23], which provided Standard Industrial Classification (SIC) codes, years the business was active, and CT where the business was located. From this information we derived counts and densities (counts per square mile) of stores per CT per year for supermarkets, chain convenience stores, fruit and vegetable markets, liquor stores (which may sell convenience foods in addition to alcohol), and fast food outlets (including pizza establishments and sweets stores selling doughnuts, candy, nuts or confectionary items). In addition, to account for people travelling outside their CTs to purchase food, we created 0.5 and 1.0 mile buffers around the boundaries of each CT and obtained counts and densities per buffer per year for each establishment type. Supermarkets and fruit and vegetable markets were considered to be healthy food outlets because they carry significant amounts of fresh fruits and vegetables. Fast food outlets, liquor stores, and chain convenience stores were considered to be unhealthy food outlets because they mostly carry non-perishable processed food.[24] Children’s neighborhood food environment was then characterized by the density of healthy and unhealthy food outlets that operated during the years 2005-2008 in the CTs where the children lived and in the expanded areas. Densities of healthy and unhealthy food outlets were allowed to be time-varying (which accounted for changes in the food environment due to families moving or store openings and closures) and were top-coded to the 95th percentile to avoid unusual CTs from influencing results.
This study was approved by the UCLA Office of the Human Research Protection Program.
Statistical analyses
Analyses were conducted using SAS 9.2. Cross-sectional associations between WHZ and covariates at baseline (first measurement taken by WIC in 2005-2008) were examined using general linear models, adjusting for age. The longitudinal WHZ measurements were analyzed using a multilevel linear growth model.[25] WHZ for child i at time t is modeled as
where α1i is the growth rate for child i and represents change in WHZ per year, α0i is the WHZ of child i at age 3 years, and eti is random error. The WHZ growth-rate parameters were modeled as a function of individual- and neighborhood-level covariates:
where x1i, … , xki are covariates affecting mean WHZ at age 3, w1i, … , wli are covariates affecting change in WHZ per year, and r0i and r1i are random effects allowing each individual to have variation around the mean growth curve. This model gives two sets of parameter estimates: β1, … , βk estimate the effects of covariates on age-three WHZ, γ1, … , γl and estimate the effects of covariates on change in WHZ per year. This model is sometimes called an intercepts- and slopes-as-outcomes model.[25] We centered age at 3 years so that intercept terms could be interpreted as effect on mean WHZ at age 3 (mWHZ3). A random intercept was also included for CTs. Covariates for mWHZ3 and change in WHZ per year included child’s age, gender, and race/ethnicity; maternal education and language preference; and family monthly income, neighborhood income and education, and densities of healthy and unhealthy food outlets. Family and neighborhood income were categorized as low (<25th percentile), middle (between the 25th-75th percentile), and high (>75th percentile).
Separate models were fit for each geographical operationalization (CT, CT plus 0.5 and 1.0 mile buffers). Density of both healthy and unhealthy food outlets were included in models to estimate the effect of each controlling for the other. The potential for a non-linear association between adiposity and the food environment was assessed by fitting quadratic terms for healthy and unhealthy food outlets; quadratic terms found to be significant were included in the final models. Given the large sample size, a p-value < .01 was considered statistically significant.
RESULTS
The sample had similar proportions of boys and girls and was predominantly Hispanic (Table 1). Most mothers had less than high school education and preferred to speak Spanish. Average family size was 4 with a mean monthly income of $1,406. The median neighborhood annual income averaged $50,326; on average, 69% of residents in these CTs had at least a high school diploma. The prevalence of obesity at baseline was 17%.
Table 1.
Characteristics of the study sample of children at their first WIC measurement (N=32,172)
| Variable | % | Mean (SD) |
|---|---|---|
| CHILD (INDIVIDUAL) CHARACTERISTICS | ||
| Child’s gender | ||
| Male | 51.4 | |
| Female | 48.6 | |
| Child’s race/ethnicity | ||
| Asian | 3.8 | |
| Black/African American | 5.2 | |
| Hispanic | 87.6 | |
| White | 3.2 | |
| Other | 0.2 | |
| Obese (BMI-for-age > 95th percentile) | 16.7 | |
| Maternal education | ||
| Less than high school | 61.6 | |
| High school education or higher | 38.4 | |
| Maternal language of preference | ||
| English | 34.8 | |
| Spanish | 63.2 | |
| Other | 2.0 | |
| Age (years) | 2.4 (0.3) | |
| Family size | 4.2 (1.4) | |
| WHZ | 0.7 (1.2) | |
| Family monthly income ($) | 1,406 (718) | |
|
| ||
| NEIGHBORHOOD CHARACTERISTICS | ||
| Annual median household income ($) | 50,326 (19,097) | |
| High school graduates (%) | 68.6 (18.0) | |
| Density of healthy food outlets (count/sq. mile) 1 | 1.2 (1.9) | |
| Density of unhealthy food outlets (count/sq. mile) 2 | 7.5 (6.4) | |
WIC = Special Supplemental Nutrition Program for Women, Infants and Children
Healthy food outlets include supermarkets and fruit and vegetable markets
Unhealthy food outlets include fast food outlets, chain convenience stores, and liquor stores
The food environment in the 1,634 CTs where the WIC families lived during the years 2005-2008 was dominated by fast food outlets (annual average for 2005-2008= 2762 outlets); the least common food outlets were fruit and vegetable markets (annual average 2005-2008 = 370 markets). On average, children lived in neighborhoods with 1.2 and 7.5 healthy and unhealthy food outlets per square mile, respectively (Table 1).
In cross-sectional associations at baseline, boys and Hispanic children had higher WHZ than girls and children of other ethnicities, respectively (Table 2). Children whose mothers did not graduate from high school were heavier than their counterparts. WHZ at baseline was negatively associated with family and neighborhood income and with neighborhood education, and not associated with density of healthy or unhealthy food outlets (Table 2).
Table 2.
Cross-sectional associations between weight-for-height z-score (WHZ)1 and individual- and neighborhood-level variables (adjusted for age; N=32,172 children)
| WHZ at 1st measurement | ||||
|---|---|---|---|---|
| Adjusted means (SE)2 |
p-value | Regression Estimates (SE) |
p-value3 | |
| Child’s gender | <.0001 | |||
| Female | 0.660 (0.010) | |||
| Male | 0.772 (0.009) | |||
| Child’s race/ethnicity | <.0001 | |||
| Asian | 0.370 (0.034)a | |||
| Black/African American | 0.438 (0.290)b | |||
| Hispanic | 0.759 (0.007)a,b,c | |||
| Non-Hispanic White | 0.470 (0.037)c | |||
| Maternal language of preference | <.0001 | |||
| English | 0.685 (0.011)a | |||
| Spanish | 0.746 (0.008)a | |||
| Other | 0.386 (0.046)a | |||
| Maternal education | <.0001 | |||
| Less than high school | 0.753 (0.008) | |||
| High school graduate or higher | 0.661 (0.011) | |||
| Family size | 0.002 (0.005) | 0.7326 | ||
| Family monthly income | −0.040 (0.009) | <.0001 | ||
| Neighborhood median income | −0.004 (0.001) | <.0001 | ||
|
Neighborhood %high school
graduates |
−0.008 (0.001) | <.0001 | ||
|
Density of healthy outlets
(stores per square mile) |
0.006 (0.003) | 0.0469 | ||
|
Density of unhealthy outlets
(stores per square mile) |
−0.001 (0.001) | 0.1541 | ||
First measurement recorded by WIC, 2005-2008
Same superscripts means that groups are significantly different from each other (Tukey’s test, p<.0001)
p-values obtained using separate general linear models for each variable, adjusting for age.
In longitudinal analyses, when neighborhood food environment was operationalized as density of food outlets in the child’s CT, the food environment was not significantly associated with mWHZ3 or WHZ slope (change in WHZ with age; Table 3). Quadratic terms for density of healthy and unhealthy food outlets were not significant and were omitted from the final model.
Table 3.
Multilevel longitudinal growth models predicting mean weight-for-height z-score (WHZ) at age 3 (intercept) and change in WHZ (slope) among preschool-aged children participating in WIC in Los Angeles County (N=32,172 children)
| Variable | Census tract | CT + 0.5 mile buffer | CT + 1 mile buffer | |||
|---|---|---|---|---|---|---|
| B | p-value | B | p-value | B | p-value | |
| PREDICTORS OF MEAN WHZ AT AGE 3 | ||||||
| Child’s gender (ref = male) | −0.119 | <.0001 | −0.118 | <.0001 | −0.118 | <.0001 |
| Child’s race/ethnicity (ref=White) | ||||||
| Asian | −0.083 | 0.0518 | −0.084 | 0.0489 | −0.087 | 0.0419 |
| Black/African American | −0.078 | 0.0398 | −0.073 | 0.0555 | −0.072 | 0.0565 |
| Hispanic | 0.234 | <.0001 | 0.236 | <.0001 | 0.236 | <.0001 |
| Maternal language preference (ref=English) | ||||||
| Spanish | −0.020 | 0.1160 | −0.022 | 0.0906 | −0.022 | 0.0853 |
| Other | −0.060 | 0.1997 | −0.063 | 0.1777 | −0.065 | 0.1631 |
| Maternal schooling (ref=≥high school) | 0.030 | 0.0086 | 0.030 | 0.0083 | 0.030 | 0.0090 |
| Family monthly income (ref = high [>$1,800]) | ||||||
| Low (<$958) | 0.035 | 0.0002 | 0.035 | 0.0002 | 0.034 | 0.0002 |
| Middle ($958-1,800) | 0.016 | 0.0246 | 0.016 | 0.0280 | 0.016 | 0.0284 |
| Neighborhood median income (ref = high[>$50,557]) | ||||||
| Low (<$32,460) | 0.044 | 0.0226 | 0.026 | 0.1827 | 0.024 | 0.2094 |
| Middle ($32,460-50,557) | 0.019 | 0.2122 | 0.009 | 0.5516 | 0.011 | 0.4806 |
| % high school graduates in neighborhood | −0.002 | 0.0003 | −0.002 | 0.0002 | −0.002 | 0.0001 |
| Density of healthy food outlets 1 | 0.002 | 0.4187 | −0.026 | 0.1141 | −0.030 | 0.2746 |
| Squared density of healthy food outlets | 0.021 | 0.0014 | 0.045 | 0.0014 | ||
| Density of unhealthy outlets 2 | −0.001 | 0.1047 | 0.001 | 0.6552 | −0.001 | 0.8458 |
| PREDICTORS OF CHANGE IN WHZ WITH AGE (SLOPE) | ||||||
| Child’s age (years) | −0.007 | 0.7607 | 0.003 | 0.8968 | 0.003 | 0.8902 |
| Gender (ref=male) | −0.001 | 0.8763 | −0.001 | 0.8636 | −0.001 | 0.8729 |
| Race/ethnicity (ref=White) | ||||||
| Asian | −0.028 | 0.1966 | −0.027 | 0.2078 | −0.026 | 0.2168 |
| Black/African American | −0.002 | 0.9183 | −0.005 | 0.7991 | −0.005 | 0.8010 |
| Hispanic | −0.041 | 0.0124 | −0.042 | 0.0095 | −0.042 | 0.0106 |
| Maternal language (ref=English) | ||||||
| Spanish | 0.041 | <.0001 | 0.041 | <.0001 | 0.041 | <.0001 |
| Other | 0.018 | 0.4302 | 0.021 | 0.3645 | 0.023 | 0.3247 |
| Maternal schooling (ref=≥high school) | −0.005 | 0.3848 | −0.005 | 0.3742 | −0.005 | 0.3817 |
| Family monthly income (ref = high [>$1,800]) | ||||||
| Low (<$958) | −0.023 | 0.0045 | −0.023 | 0.0051 | −0.023 | 0.0054 |
| Middle ($958-1,800) | −0.009 | 0.1821 | −0.008 | 0.2088 | −0.009 | 0.1998 |
| Neighborhood median income (ref = high[<$50,557]) | ||||||
| Low (<$32,460) | −0.003 | 0.7697 | 0.004 | 0.6649 | 0.002 | 0.8097 |
| Middle ($32,460-50,557) | −0.021 | 0.0067 | −0.016 | 0.0419 | −0.016 | 0.0326 |
| % high school graduates in neighborhood | <0.001 | 0.1077 | <0.001 | 0.1034 | <0.001 | 0.0842 |
| Density healthy food outlets | <0.001 | 0.9767 | −0.014 | 0.0035 | −0.022 | 0.0102 |
| Density unhealthy food outlets | 0.001 | 0.1592 | <0.001 | 0.8841 | <0.001 | 0.9052 |
Healthy outlets include supermarkets and fruit and vegetable markets
Unhealthy outlets include fast food outlets, chain convenience stores, and liquor stores
When food environment was operationalized as food outlets in the CT plus 0.5-mile and 1-mile buffers, associations between the food environment and adiposity emerged. In these models, the quadratic term for density of healthy food outlets on the intercept (mWHZ3) was significant and included in the final models. As shown in Table 3, the association was non-linear: at lower densities, the association between density of healthy food outlets and mWHZ3 was negative; however, at higher densities, the association became positive. The point at which the relationship became positive is approximately 0.7 healthy food outlets/square mile (Figures 1-2). In addition, density of healthy food outlets was negatively associated with WHZ slope in the CT plus 0.5-mile model. There was no significant association between the density of unhealthy food outlets and mWHZ3 or WHZ slope.
Figure 1.
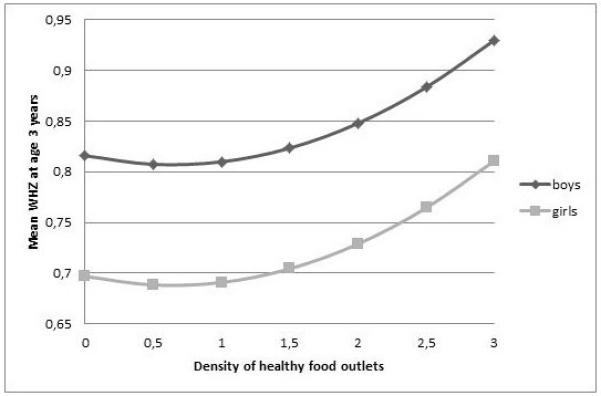
Relationship between mean WHZ at age 3 years and density of healthy food outlets in a 0.5-mile buffer around the borders of the census tracts where the child lived (2005-2008)1
WHZ = weight-for-height z-scores
1Equation estimated for Hispanic children (when compared to white children) whose mothers speak Spanish, have at least a high school education, have an average family income ($1402), and live in an average neighborhood (neighborhood annual income = $50,326; % high school graduates = 69%; density of unhealthy food outlets = 7.5)
Figure 2.
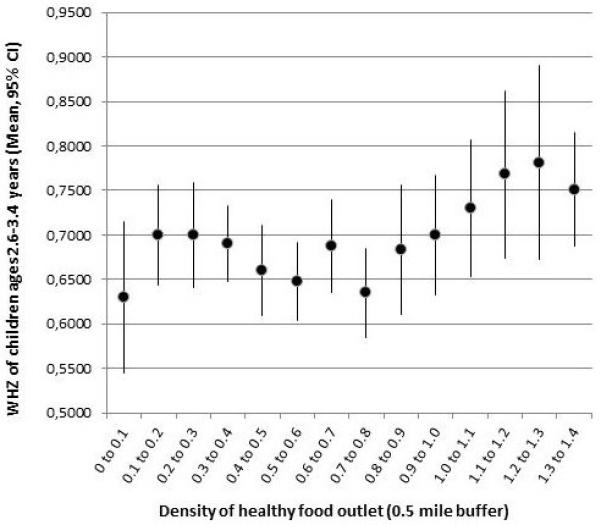
Means and 95% confidence intervals for WHZ for children around age 3 years (ages 2.6-3.4 years) by density of healthy food outlets in the census tract plus 0.5-mile buffer
WHZ = weight-for-height z-scores
DISCUSSION
In this study of largely Hispanic, low income preschool-aged children participating in WIC in LAC, the food environment, and in particular the density of healthy food outlets in the child’s neighborhood, was associated with adiposity. The association appeared when our broader definition of neighborhood (census tract plus 0.5 or 1 mile buffer) was used, and indicated a non-linear association of mean WHZ at age 3 with density of healthy food outlets.
While a large proportion of studies looking at food environments and obesity define neighborhood based on CT boundaries, our findings support the results of other studies suggesting that a less circumscribed definition should be considered.[26-28] For example, Hillier et al.[26] studied shopping patterns among WIC recipients in Northern Philadelphia and found that, on average, participants traveled 1.0-1.6 miles for their food shopping, with only 1.5% of participants conducting most food shopping within their own CT. It is difficult to make comparisons between studies as there is substantial heterogeneity between different geographic areas. However, an effort should be made to develop food environment measures that are conceptually and empirically valid.[29] Given our findings, we suggest that CTs may be too small of an area to determine an effect of the food environment on children’s adiposity. On the other hand, it may be less convenient for families with very small children to travel outside of their immediate neighborhoods.
Two recent longitudinal, nationally representative studies among school-aged children found null associations between the food environment and BMI, regardless of the food environment measure used.[9, 10] Their use of CTs to define food environment may have contributed to the null findings. In addition, these studies used BMI, which is a problematic measure of adiposity for growing children.[20]
To our knowledge, no published study to-date has examined the longitudinal association between the food environment and adiposity in preschool-aged children. Cross-sectional findings, however, partially agree with ours. Burdette and Whitaker[8] reported no associations between BMI z-score and distance to fast food restaurants among 3-5 year old WIC participants in Ohio. We also found no associations between WHZ and density of unhealthy food outlets. Fiechtner et al.[12] found a positive association between BMI and living ≤1 mile from a large supermarket (vs. those living >2 miles away) in a small convenience sample of already overweight/obese preschool-aged children in Boston. Our study suggests that density of healthy food outlets is positively associated with mean WHZ but only at higher densities of healthy food outlets; at lower densities the association is negative, as hypothesized.
Our finding of a non-linear association between adiposity and density of healthy food outlets should be further explored. Even though we, as others before us, classified supermarkets as “healthy outlets,” supermarkets also carry a large variety of high-fat, high-sugar foods and drinks in addition to fresh produce. Miller et al.[30] reported that when compared to convenience and other small food stores in New Orleans, supermarkets had a much greater display of energy-dense snack foods and these were always within a meter of the cash registries. In contrast, fruit and vegetable displays (which were also greater in supermarkets when compared to convenience stores) were never within a meter of the cash register.[30] Therefore, referring to supermarkets as the “best” food outlet for healthy food purchases may be misleading. Our results suggest that there may be a threshold effect in which ~0.7 healthy stores per square mile is associated with lowest mean adiposity. We speculate that a lower density of healthy stores may translate into a lack of access to fresh healthy foods but >0.7 stores per square mile may increase the availability of both healthy and unhealthy foods. In this population of low-income families receiving nutrition education through the second largest federally funded nutrition assistance program, it is likely that the lack of neighborhood access to healthy fresh foods would have influenced food purchasing decisions. It is also possible that the positive association observed between WHZ and the density of healthy food outlets is spurious – neighborhoods that attract several supermarkets may be more urbanized and differ in other environmental aspects that may increase child obesity risk, such as having more traffic and fewer parks, affecting physical activity. Our study did not have access to data on traffic patterns or parks year by year. However, a separate analysis of land use data for LAC obtained for 2000 showed minimal variation in the percent of land that is occupied by green space (an indicator of park availability) in lower income census tracts (personal communication, Kara MacLeod, 2014).
This study demonstrates the complexity involved in studying the relationship between the food environment and obesity risk, with results varying depending on the definition of neighborhood boundaries (i.e. census tracts vs. buffers surrounding census tracts), the measure of food environment used (“unhealthy” vs “healthy” food outlets), the contextual setting (e.g. urban vs. suburban vs. rural) and the outcome examined (adiposity vs. change in adiposity with age).
Strengths of this study include its longitudinal nature and large sample size; exposure of all WIC families to nutrition education which reduces the likelihood that effects of the food environment are confounded by lack of parental nutrition knowledge; and high validity of its weight and height measurements.[17] A limitation, which is common to most studies using food store data, is the lack of assessment of the validity of the classification of food stores as healthy or unhealthy. In addition, using census tracts to define neighborhoods may be problematic since they are solely administrative units with no real-life significance for residents. Using such artificial boundaries could result into some misclassification bias, which we believe we have minimized by the use of the 0.5 and 1-mile buffers. Finally, our results are not necessarily representative of low-income preschool-aged children nor of all WIC participants as children included in this study were different from those excluded (those with 1 or 2 weight/height measures only), with those included more likely to be younger Hispanic children with Spanish speaking mothers and overall less advantaged (not shown). This is reflective of the fact that Spanish-speaking Hispanics are more likely to stay in WIC longer and, therefore, more likely to have been included in this longitudinal analysis. If we restrict our analyses to Hispanic children only, our non-linear relationship between mWHZ3 and density of healthy food outlets in our buffer models remain. However, a negative association between density of unhealthy food outlets and mWHZ3 surfaces in the CT-only model, again suggesting that the association between the food environment and adiposity needs to be interpreted within specific contexts and with consideration for the measures used.
Conclusion
Despite the latest evidence showing a slowing down of the obesity epidemic in preschool-aged children in the US,[31] there is an ongoing need to prevent obesity early in life. Our study contributes to our understanding of the role of the food environment in obesity development among preschool-aged children. To our knowledge, this is the first study to document a non-linear relationship between adiposity and the density of healthy food outlets, and one of just a few to longitudinally examine the contribution of the food environment to obesity early in life. This non-linear relationship suggests a threshold effect which warrants further investigation. Understanding the impact of the neighborhood food environment on obesity development has important implications for social and economic policies.
What is already known on this subject?
The food environment is associated with obesity risk among adults. However, little is known about this association among pre-school aged children.
What this study adds?
We found a non-linear association between child adiposity and neighborhood density of healthy food outlets; lowest adiposity was observed at ~0.7 healthy food outlets per square mile. This threshold effect warrants further research and may have important implications for social and economic research and policy.
ACKNOWLEDGMENTS
The authors wish to acknowledge Eloise Jenks and Armando Jimenez for assistance with data acquisition, all WIC staff for assistance with data collection, and Jennifer Arias, Vivian Alfonso, and Hannah Husby for their assistance with literature reviews and data management.
FUNDING STATEMENT
This study was supported by the American Heart Association (#09GRN2230167, PI: Wang), and First 5 LA. Crespi was also supported by National Institutes of Health UL1TR000124.
Footnotes
COMPETING INTEREST
Competing Interest: None to declare.
CONTRIBUTORSHIP STATEMENT
MPC participated in the design of the study, carried out the data management and analysis, and drafted the manuscript. SW participated in the design of the study, was in charge of data collection, and edited the manuscript. CMC participated in the design of the study, supervised the statistical analyses and edited the manuscript. MK aided in data collection and management and edited the manuscript. TZN aided in data management and analysis and edited the manuscript. ES aided in data collection and management and edited the manuscript. MCW participated in the design of the study, aided in data management and analyses, and edited the manuscript.
REFERENCES
- 1.Edwards KL, Clarke GP, Ransley JK, et al. The neighbourhood matters: Studying exposures relevant to childhood obesity and the policy implications in Leeds, UK. J Epidemiol Community Health. 2010;64:194–201. doi: 10.1136/jech.2009.088906. [DOI] [PubMed] [Google Scholar]
- 2.Black JL, Macinko J. Neighborhoods and obesity. Nutr Rev. 2008;66(1):2–20. doi: 10.1111/j.1753-4887.2007.00001.x. [DOI] [PubMed] [Google Scholar]
- 3.Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Affairs. 2010;29(3):503–12. doi: 10.1377/hlthaff.2009.0730. [DOI] [PubMed] [Google Scholar]
- 4.Oreskovic NM, Winickoff JP, Kuhlthau KA, et al. Obesity and the built environment among Massachusetts children. Clin Pediatr (Phila) 2009;48(9):904–12. doi: 10.1177/0009922809336073. [DOI] [PubMed] [Google Scholar]
- 5.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health Nutr. 2005;119(12):1059–68. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Galvez MP, Hong L, Choi E, et al. Childhood obesity and neighborhood food-store availability in an inner-city community. Acad Pediatr. 2009;9:339–43. doi: 10.1016/j.acap.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Powell LM, Auld MC, Chaloupka FJ, et al. Associations between access to food stores and adolescent body mass index. Am J Prev Med. 2007;33(4S):S301–S7. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: Relationships to overweight in low-income preschool children. Prev Med. 2004;38:57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 9.Shier V, An R, Sturm R. Is there a robust relationship between neighbourhood food environment and childhood obesity in the USA? Public Health. 2012;126(9):723–30. doi: 10.1016/j.puhe.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee H. The role of local food availability in explaining obesity risk among young school-aged children. Soc Sci Med. 2012;74:1193–203. doi: 10.1016/j.socscimed.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 11.Koleilat M, Whaley SE, Afifi A, et al. Understanding the relationship between RFEI and early childhood obesity among WIC participants in Los Angeles County using GeoDa spatial statistics software. Online J Public Health Inform. 2012;4(1) doi: 10.5210/ojphi.v4i1.3936. pii: ojphi.v4i1.3936. doi: 10.5210/ojphi.v4i1.3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiechtner L, Block J, Duncan DT, et al. Proximity to supermarkets associated with higher body mass index among overweight and obese preschool-age children. Prev Med. 2013;56(3-4):218–21. doi: 10.1016/j.ypmed.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Agriculture, Food and Nutrition Service Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Revisions in the WIC food packages; Interim Rule. 2007 cited 2013 March. Available from: http://www.fns.usda.gov/wic/regspublished/wicfoodpkginterimrulepdf.pdf.
- 14.Hillier A, McLaughlin J, Cannuscio CC, et al. The impact of WIC food package changes on access to healthful food in 2 low-income urban neighborhoods. J Nutr Educ Behav. 2012;44(3):210–6. doi: 10.1016/j.jneb.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Andreyeva T, Luedicke J, Middleton AE, et al. Changes in access to healthy foods after implementation of the WIC food packages revisions: Rudd Center for Food Policy and Obesity. Yale University; 2011. cited 2014 Feb. Available from: http://yaleruddcenter.org/resources/upload/docs/what/economics/AccessChangesWICRevisions_USDA-ERS_4.11.pdf. [Google Scholar]
- 16.PHFE WIC Program Data Mining Project. n.d. [cited 2013 March 20] Available from: http://www.phfewic.org/projects/DataMining.aspx.
- 17.Crespi CM, Alfonso VH, Whaley SE, et al. Validity of child anthropometric measurements in the Special Supplemental Nutrition Program for Women, Infants, and Children. Pediatr Res. 2012;71(3):286–92. doi: 10.1038/pr.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 19.Garn SM, Leonard WR, Hawthorne VM. Three limitations of the body mass index. Am J Clin Nutr. 1986;44:996–7. doi: 10.1093/ajcn/44.6.996. [DOI] [PubMed] [Google Scholar]
- 20.Jones A, Charadika M, Falaschetti E, et al. Adipose and height growth through childhood and blood pressure status in a large prospective cohort study. Hypertension. 2012;59:919–25. doi: 10.1161/HYPERTENSIONAHA.111.187716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Ann Rev Pub Health. 1997;18:341–78. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Census Bureau . American Community Survey; 2014. cited 2014 Apr 30. Available from: www.census.gov/acs/www. [Google Scholar]
- 23.Walls & Associates . NETS database by Walls & Associates. Oakland, CA: 2011. cited 2011 Dec. Available from: http://www.youreconomy.org/nets/?region=walls. [Google Scholar]
- 24.Farley TA, Rice J, Bodor JN, et al. Measuring the food environment: Shelf space of fruits, vegetables, and snack foods in stores. J Urban Health. 2009;86:672–82. doi: 10.1007/s11524-009-9390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raudenbush SW, Bryk AS. Hierarchical Linear Models. 2nd edition Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- 26.Hillier A, Cannuscio CC, Karpyn A, et al. How far do low-income parents travel to shop for food? Empirical evidence from two urban neighborhoods. Urban Geogr. 2011;35:712–29. [Google Scholar]
- 27.Hirsch JA, Hillier A. Exploring the role of the food environment on food shopping patterns in Philadelphia, PA, USA: A semiquantitative comparison of two matched neighborhood groups. Int J Environ Res Public Health. 2013;10:295–313. doi: 10.3390/ijerph10010295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.LeDoux TF, Vojnovic I. Going outside the neighborhood: The shopping patterns and adaptations of disadvantaged consumers living in the lower eastside neighborhoods of Detroit, Michigan. Health Place. 2013;19:1–14. doi: 10.1016/j.healthplace.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Caspi CE, Sorensen G, Subramanian SV, et al. The local food environment and diet: A systematic review. Health Place. 2012;18(5):1172–87. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller C, Bodor JN, Rose D. Measuring the food environment: A systematic technique for characterizing food stores using display counts. J Environ Public Health. 2012;2012 doi: 10.1155/2012/707860. doi: 10.1155/2012/707860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]


